
PEBB Retiree Medicare Benefits
Engrossed Substitute Senate Bill 5187; Section 212(6); Chapter 475; Laws of 2023.
December 1, 2023
Employees and Retirees Benefits Division
P.O. Box 45502
Olympia, WA 98504
Phone: (360) 725-1612
Fax: (360) 586-9551
hca.wa.gov

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 2
Acknowledgement
HCA is appreciative of the participation of the PEBB members as well as the Stakeholders Medicare
Coalition in providing feedback on the retiree experience.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 3
Table of contents
Executive summary ............................................................................................................................................................................. 4
Background ............................................................................................................................................................................................ 5
PEBB Program overview .............................................................................................................................................................. 5
PEBB Medicare retirees – enrollment trends ................................................................................................................ 6
Overview of PEBB Medicare plans .................................................................................................................................. 13
Overview of CMS Medicare Advantage Program .................................................................................................... 26
Benefit of remaining in PEBB Medicare plans ........................................................................................................... 29
HCA survey of PEBB retirees ............................................................................................................................................. 30
2022 Proposal to consider closing UMP Classic Medicare Plan ....................................................................... 31
Findings ................................................................................................................................................................................................ 33
2023 PEBB retiree listening sessions ............................................................................................................................. 33
50 State comparison of state-sponsored health benefits for public sector Medicare retirees report
........................................................................................................................................................................................................ 50
Options and considerations to reduce UMP Medicare premiums .................................................................. 58
Conclusion ........................................................................................................................................................................................... 69
Appendix .............................................................................................................................................................................................. 72

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 4
Executive summary
Engrossed Substitute Senate Bill 5187 (2023) requires the Health Care Authority (HCA) to gather member
feedback about Public Employee Benefits Board (PEBB) retiree Medicare benefits and provide a final
report to the legislature with the intent to inform future health care plan selections.
By December 1, 2023, the authority must report to the legislature with its findings,
including an analysis of government self-insured plans with benefits that are equal to
or richer, and with more affordable premiums, than Uniform Medical Plan Classic
Medicare. (Sec. 212(6))
HCA invited PEBB retiree members to participate in listening sessions (held from February through May
2023) to assess retiree satisfaction with the current plan offerings. One hundred and ninety-three retirees
participated. Most had positive things to say about their plan and identified one or more challenges.
Feedback for each of the four PEBB Medicare health plan carriers includes:
• Kaiser members report their plan offers good coverage for an affordable price, although some
feel provider availability is limited and wait times to see a provider can be long.
• Premera plan members appreciate the coverage and the affordability of the plan, but wish the
plan covered additional benefits such as gym memberships, hearing aids, and naturopathy.
• UnitedHealthcare (UHC) members like the affordability of the premiums, and the additional
benefits such as massage and gym membership, but express frustration with UHC’s customer
service and the pharmacy coinsurance costs.
• Uniform Medical Plan (UMP) members speak highly about the quality of coverage and customer
service, but feel the plan is too costly, although some maintain the cost is worth it.
HCA completed an analysis of all 50 states’ government plan offerings to find examples of how to
maintain the quality and benefits UMP Classic Medicare offers, while reducing costs. The analysis found
Medicare supplement plans varied by state. No other state was found to have benefits equal to or richer
than UMP Classic Medicare with lower premiums. There are several pharmacy and medical coverage
alternatives for UMP Classic Medicare that could result in significant retiree monthly premium savings:
• The greatest savings would come from converting the UMP Medicare pharmacy benefit to a self-
funded Part D Employer Group Waiver Plan (EGWP), which would take advantage of federal
subsidies and drug discounts. Additionally, an EGWP could be customized to provide pharmacy
coverage that is like the current coverage offered through UMP. This would limit the impact to
retirees’ out-of-pocket costs, although there could be some disruption due to differences in how
the pharmacy benefit would be administered under Part D.
• Premiums could be lowered by changing the UMP coordination provisions when Medicare pays
primary. This would shift retiree costs from premium to out-of-pocket spending (deductible and
cost-share).
Finally, the pharmacy and medical options could be combined for even greater premium relief. For
example, changing the UMP coordination provisions to a carve out with no coordination of benefits
(COB) savings bank, combined with a standard self-funded Part D EGWP, could result in additional
savings. Milliman’s full report provides projected savings for each of these coverage combinations.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 5
Background
PEBB Program overview
HCA purchases and manages health care and other insurance benefits for more than 385,000 eligible
public employees, retirees, continuation coverage members, and their dependents through the PEBB
Program and over 273,000 eligible school employees and their dependents through the School
Employees Benefits Board (SEBB) Program. SEBB members are eligible for PEBB retiree benefits upon
retirement from school employment. Employers who access PEBB Program coverage include state
agencies, institutions of higher education, and a variety of public agencies who contract with HCA for
these benefits (e.g., counties, municipalities, tribal governments, and political subdivisions). The PEBB
Program in its current form dates to the 1980s. Before that, state employee and higher education
employee benefits were provided through the Department of Personnel and the State Employee
Insurance Board.
The PEBB Program is overseen by the PEB Board, which is comprised of 8 members appointed by the
Governor. Each Board member serves two-year terms; one of the Board members serves in a non-voting
capacity. The Board meets from January to July each year to authorize employee and retiree health care
benefits
1
, and each year approves the benefit design and premium rates that will be offered to employees
and retirees in the following year. The PEBB Program’s plan year for benefits coverage begins in January
and annual open enrollment occurs November of each year.
Proposals for new or enhanced benefits come from many sources including Federal and state regulatory
sources, the state Legislature, the PEB Board, HCA customer service, payers, and through monitoring of
trends in industry benefits. The timeline for consideration of a benefit enhancement can run from 12
months to 36 months, and is constrained by the calendar year plan design, competitive procurement
requirements, HCA staff workloads, and, in some cases, legislative action or input.
Figure 1 - PEBB Program benefit planning cycle
1
RCW 41.05.065 describes the duties of the PEB Board and establishes the level of benefits for employees
and retirees: RCW 41.05.065 (2) “The public employees' benefits board shall develop employee benefit
plans that include comprehensive health care benefits for employees.” (3) “To maintain the
comprehensive nature of employee health care benefits, benefits provided to employees shall be
substantially equivalent to the state employees' health benefit plan in effect on January 1, 1993.” (4)
“Except if bargained for under chapter 41.80 RCW, the public employees' benefits board shall design
benefits and determine the terms and conditions of employee and retired or disabled school employee
participation and coverage, including establishment of eligibility criteria...”

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 6
As shown in the above example, a decision in July 2023 (by the PEB Board or at the end of a legislative
session) may not be implemented until January 2025, and could be later if it involves a complex
procurement, or encounters complications or delays.
PEBB Medicare retirees – enrollment trends
As of June 2023, 76,547 PEBB Medicare retiree subscribers, and 30,229 spouses and dependents were
enrolled in one of the Medicare plans offered through the PEBB Program for a total of 106,776 PEBB
Medicare retiree members.
As shown in Chart 1 below, since 2018, the total number of PEBB Medicare subscribers has increased an
average of 2.9 percent per year increasing from 66,206 in 2018 to 76,547 subscribers in 2023.
Chart 1: PEBB Medicare retiree subscribers 2018 to 2023
Every year, approximately 5,400 PEBB and SEBB active employees retire from employment. During the
period from 2018 to 2022, an average of 2,890 PEBB subscribers and 2,525 SEBB subscribers changed to
retiree status each year. Some employees retire before reaching age 65 and are not eligible for the PEBB
Medicare plans upon retirement, but they may be able to continue with their PEBB or SEBB plans through
COBRA , choose a non-Medicare retiree plan, or defer PEBB coverage until they reach age 65.
2
An average of 8,184 PEBB and SEBB subscribers enrolled for the first time in one of the PEBB Medicare
health plans during each of the years 2021 and 2022.
As shown in Table 1 below, the proportion of Medicare retiree members (including spouses and
dependents) within PEBB compared to other PEBB & SEBB members (including active employees, retirees
2
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers the right to choose to
continue their group health benefits for limited periods of time after a job loss.
66,206
68,752
70,715
72,605
74,809
76,547
60,000
62,000
64,000
66,000
68,000
70,000
72,000
74,000
76,000
78,000
2018 2019 2020 2021 2022 2023
Subscribers
PEBB Medicare Retiree Subscribers
June 2023

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 7
who are not yet on Medicare, and spouses and dependents) has remained relatively stable since 2020. As
of June 2023, PEBB Medicare retiree membership (including spouses and dependents) comprised 16
percent of overall PEBB and SEBB membership; a proportion that has trended slightly upward since 2020.
Table 1: PEBB Medicare retiree members compared with total
2020
2021
2022
2023
PEBB Medicare Re�ree Members
98,942
101,743
104,815
106,776
Other PEBB & SEBB Members
540,803
546,214
549,516
558,348
Total PEBB & SEBB Members
639,745
647,957
654,331
665,124
Enrollment by plan
As of June 2023, approximately 42 percent of PEBB Medicare subscribers (32,455) were enrolled in
Uniform Medical Plan (UMP) Classic Medicare; 25 percent were enrolled in one of the Kaiser plans
(18,971); 20 percent were enrolled in Premera Plan F or G (14,894); and 13 percent were enrolled in one of
the UnitedHealthcare (UHC) plans (10,227).
Chart 2: PEBB Medicare subscribers by plan
During the period from 2021 to 2023, the Kaiser and UMP plans lost enrollment, while Premera and UHC
each gained enrollment in their plans. UHC added 7,221 new subscribers in 2023 and Premera gained
32,455
18,971
14,894
10,227
-
5,000
10,000
15,000
20,000
25,000
30,000
35,000
UMP Kaiser Premera UHC
Subscribers
PEBB Medicare Subscribers

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 8
1,003 new subscribers. This jump in enrollment for both UHC and Premera in 2023 coincided with a large
increase in premium costs in 2023 for the UMP Classic Medicare plan.
Table 2: Medicare subscriber enrollment by plan– 2021 to 2023
2021 2022 2023
Change
2021 - 2023
Pct. Change
2021 - 2023
UMP
38,965
38,784
32,455
(6,510)
-16.7%
Kaiser
19,425
19,128
18,971
(454)
-2.3%
Premera
13,036
13,891
14,894
1,858
14.3%
UHC
1,179
3,006
10,227
9,048
767.4%
Chart 3: PEBB Medicare subscriber enrollment by plan
-
5,000
10,000
15,000
20,000
25,000
30,000
35,000
40,000
45,000
UMP Kaiser Premera UHC
Subscribers
Medicare Subscriber Enrollment by Plan
2021 2022 2023

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 9
Chart 4: PEBB Medicare retiree Subscribers by age group 65 and older
Half (37,867) of all PEBB Medicare retiree subscribers are aged 65 to 74. Another 37 percent (28,574) are
aged 75 to 84; 12 percent (8,822) are age 85 to 94; and 1 percent (863) are age 95 or older.
Chart 5: 2023 PEBB Medicare Subscribers by plan and by age
13,056
8851
9,298
6,662
14,165
7643
3,737
3,029
4,567
2,184
1,616
455
420
221
201
21
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
UMP Kaiser Premera UHC
2023 Medicare Subscribers by Plan and by Age
65-74 75-84 85-94 95+

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 10
As of 2023, UMP had the oldest subscriber membership, with only 41 percent of UMP subscribers in the
age 65 to 74 group (compared with 50% in that age group for the PEBB Medicare population overall).
Forty-seven percent of Kaiser subscribers were in the 65 to 74 age group. UHC and Premera had the
youngest subscriber membership, 66 percent in UHC and 63 percent in Premera were in the 65 to 74 age
group.
Chart 6 below shows the aging trend for UMP since 2018. Those in the 65 to 74 age group have been
leaving the plan since 2018 with a steep drop from 2022 to 2023, again coinciding with large premium
increases for those last two years.
Chart 6: UMP subscribers by age 2018 to 2023

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 11
PEBB Medicare subscribers by state
Ninety-two percent of PEBB Medicare subscribers receive their benefits in Washington state, and the rest
are in every state in the US, plus Washington, D.C. The table below shows the top ten states (after
Washington) where PEBB Medicare subscribers receive their benefits, and the map on the following page
shows additional states where there are PEBB Medicare retirees. A full list of the number of subscribers by
state is shown in Appendix 1.
Table 3: PEBB Medicare retiree subscribers by state – Washington plus top 10
State
Subscribers
WA
70,375
AZ
1,243
ID
1,077
OR
1,007
CA
536
MT
269
TX
265
FL
249
NV
189
UT
124
CO
114

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 12
Figure 2: Map of PEBB Medicare subscribers by state
June 2023

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 13
Overview of PEBB Medicare plans
PEBB Medicare retiree risk pool and plan offerings
Under RCW 41.05.080, eligible state and school employees may continue their participation in PEBB
medical plans after retirement or disablement. The premium rates for those who are eligible for and enroll
in Medicare Part A and Part B are calculated separately from the non-Medicare risk pool, which includes
employees and non-Medicare retirees.
Since January 2021, the PEBB Program has offered four different Medicare plan types and eight distinct
plans to eligible retirees and their dependents who are enrolled in Medicare.
Figure 3: PEBB Program Medicare Plan Types
UMP Classic Medicare has the same benefits as UMP Classic offered to PEBB employees, but coordinates
coverage with Medicare for medical services covered by Medicare Part A and Part B
3
. This means that
Medicare is the primary payer (i.e., pays first) for these medical services, and UMP is the secondary payer
(pays after Medicare). UMP Classic Medicare also includes the same prescription drug benefits that
3
Medicare Part A covers inpatient care in hospitals, skilled nursing facility care, hospice care, and home
health care. Medicare Part B helps cover services from doctors and other health care providers.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 14
employees receive, but the plan is the only payer for these pharmacy claims. Original Medicare (Part A
and Part B) does not cover prescription drugs with the exception that some infusions and vaccines are
covered under Part B. The UMP Classic Medicare prescription drug benefit is creditable drug coverage,
not a Part D product, and does not receive several sources of federal funding that are only available to
Part D prescription drug plans.
The Kaiser Washington Original Medicare plan is only intended for PEBB Medicare retirees who are
outside of the Kaiser Washington Medicare Advantage (MA) service area. The premiums for this plan are
calculated independently and then blended with the Kaiser Washington MA plan premium based on
enrollment. Retirees who enroll in either plan pay the same blended premium.
The United HealthCare Medicare Advantage plus Part D (MA-PD) plans are the only plans in the PEBB
Medicare risk pool that offer prescription drug coverage through Part D. The Medicare Modernization Act
(MMA) of 2003 created Medicare Part D, which covers prescription drugs for Medicare enrollees through
private insurance plans. Part D plans may be offered through an employer, on the individual market, or
they may be integrated with medical coverage under an MA-PD plan.
• Employers - Part D Prescription Drug Plans (PDPs) can be offered exclusively by an employer to its
eligible retirees via an Employer Group Waiver Plan (EGWP).
• Individual Market - Part D Prescription Drug Plans (PDP) are available to all Medicare enrollees.
• Integrated - Medicare Advantage plans may also offer Part D prescription drug coverage. MA-PD
plans may be offered by employers or available to all Medicare enrollees on the individual market.
A plan’s list of covered drugs is called a “formulary,” and each plan has its own unique formulary. Plans
typically place drugs into different levels, called “tiers,” that have an associated patient cost-share. All
Medicare Part D drug plans must cover a wide range of prescription drugs including most drugs in
protected classes like cancer drugs, antivirals to treat HIV/AIDS, antipsychotics, and antidepressants.
Commercial prescription drug plans, such as that offered through UMP, and Medicare Part D drug plans
also have coverage rules for managing utilization, such as:
• Prior Authorization - the prescriber must contact the plan before covering certain prescriptions.
The prescriber may need to show that the drug is medically necessary for the plan to cover it.
• Quantity limits – for safety or cost reasons, plans may limit the amount of prescription drugs they
cover over a certain period. Some plans have an administrative process for requesting an
exception to the quantity limits.
• Step therapy –a type of prior authorization where the subscriber needs to try certain, less
expensive drugs on the plan’s formulary that are considered effective for most people with the
condition before they can move up a “step” to the requested drug.
PEBB Medicare subsidies
There are several different subsidies related to PEBB Medicare retiree coverage, as described in the table
below.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 15
Figure 4: Types of PEBB Medicare Subsidies
To the plan To retirees To the State
Federal Medicare subsidies
for Part C (Medicare
Advantage) and Part D
(Prescription Drug) plans
Washington State “Medicare
Explicit Subsidy”
Federal Retiree Drug Subsidy
(RDS)
•Provided by Centers for
Medicare and Medicaid
Services (CMS) to the plan to
reimburse for Medicare-
covered services and a large
portion of prescription drug
costs (for Part D Plans).
•Reduces overall plan costs and
the amount members pay in
premiums.
•Risk-adjusted and varies by
plan, but typically covers 100%
of Medicare-covered medical
services and ~74.5% of
pharmacy costs based on the
Standard Defined Part D
benefit.
•Described in the state budget.
•Subsidizes a portion of the
member’s monthly premium
(In 2024, $183 or 50% of the
carrier’s final bid rate,
whichever is less).
•Premiums approved by the
PEB Board have the subsidy
applied.
•A subsidy received by the state
and deposited into the
General Fund each year for
offering prescription drug
coverage to retirees that is at
least as generous as Medicare
Part D.
•Historically, the annual RDS
equals ~$22-$26M. This is
intended to offset the cost to
the employer of offering
prescription drug coverage.
Within UMP, the subsidy is a
small percentage of plan
spending on prescription
drugs.
•Not directly applied to
member premiums.
Federal Medicare subsidies for Part C (Medicare Advantage) and D (Prescription Drug) plans. Direct
and indirect funding for Part C and Part D plans is described in more detail in the following section.
Washington State “Medicare Explicit Subsidy”
This is described in RCW 41.05.085 and is provided to retirees via a reduction to monthly PEBB Medicare
health plan premiums. The amount of the premium reduction is established by the PEB Board and shall
not be more than fifty percent of the premium. The maximum value of the subsidy is set by the
Legislature in the state budget. For 2024 it is $183 or 50 percent of the plan’s premium, whichever is less.
The premiums approved by the Board have the maximum value of the subsidy applied. HCA collects the

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 16
subsidized (lower) premiums from the retiree and pays the health plans the full premiums (i.e., the “bid
rate”).
4
Federal Retiree Drug Subsidy (RDS)
The state also receives a subsidy for providing creditable prescription drug coverage through UMP Classic
Medicare, Kaiser Permanente Washington (Kaiser Permanente WA) Original Medicare and Medicare
Advantage, and Kaiser Permanente Northwest (Kaiser Permanente NW) Senior Advantage. To be eligible
for this subsidy, called the Retiree Drug Subsidy or RDS, prescription drug coverage must be at least as
rich as the standard Part D benefit. The total value of the subsidy is historically around $22-$26M but
varies based on enrollment and drug expenditures. It is deposited into the General Fund – State. Table 4,
below, shows how the maximum dollar limit of the subsidy has changed from 2016 to 2023.
Table 4: Medicare Explicit Subsidy maximum dollar limit, 2016 to 2024
2016
2017
2018
2019
2020
2021
2022
2023
2024
$150
$150
$150
$168
$183
$183
$183
$183
$183
MA and Medicare Part D subsidies
CMS pays a per beneficiary capitated payment to MA plans based on average spending under traditional
fee-for-service (FFS) Medicare, adjusted for the MA plan’s service area. This establishes the benchmark
that MA plans bid against based on their projected costs. Plans with bids above the benchmark have
higher premiums. Most plans bid below the benchmark and can use the resulting rebate to lower out-of-
pocket costs and/or cover supplemental benefits.
Medicare Part D plans and MA-PD plans receive federal funding to reimburse a portion of prescription
drug costs. This revenue reduces the plans’ overall costs and therefore the amount that is passed to
members as a monthly premium. The payments are adjusted based on the reported risk of the population
and cover about 74.5 percent of pharmacy costs based on the standard Part D benefit. This funding is
provided directly from CMS and indirectly through drug manufacturer discounts:
• A per beneficiary capitated payment from CMS, or direct subsidy, calculated as a share of the
adjusted national average of plan bids.
• Individual reinsurance through which CMS pays 80 percent per enrollee of drug spending above
the standard Part D out-of-pocket threshold.
• Manufacturer discount program, or drug manufacturer discounts for brand name drugs in the
Part D coverage gap.
Medicare also pays all or most of the premium for low-income beneficiaries up to a threshold that is
established based on the enrollment-weighted average premium per Part D region.
4
UMP Classic Medicare is a self-insured plan that pays its own claims; HCA does not pay a monthly
premium to Regence, the third-party administrator.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 17
Retiree Drug Subsidy Program
Congress enacted the Retiree Drug Subsidy (RDS) Program in December 2003 to reimburse plan sponsors
for a portion of their covered retirees' qualifying costs for prescription drugs. Through the subsidy, CMS
reduces employers’ financial obligation for offering non-Part D prescription drug coverage by reimbursing
the equivalent of 28 percent of each retiree’s allowable drug expenses that fall between the federally
designated cost threshold amount and the cost limit. The amount up to the cost threshold is not eligible
for subsidy, and the amount exceeding the cost limit is not eligible for subsidy. These amounts are
adjusted annually by CMS.
Table 5 5: RDS cost threshold and cost limit by plan year
Plan Year Ending
Cost Threshold
Cost Limit
2020
$435
$8,950
2021
$445
$9,200
2022
$480
$9,850
2023
$505
$10,350
2024
$545
$11,200
To qualify for the subsidy, a plan sponsor, in this case HCA, must show that its eligible plans’ drug
coverage is “actuarially equivalent” to, or at least as generous as, the defined standard Medicare Part D
benefit. This test looks at a plan’s spending on prescription drugs and the amount that enrollees pay for
premiums and cost-shares (copays/coinsurance and deductibles) compared to what they would pay under
the standard Part D benefit. It also factors in the value of employer financing of drug coverage, such as
the Medicare Explicit Subsidy.
RCW 41.05.068 authorizes HCA to participate as an employer-sponsored program to receive the RDS “for
continuing to provide retired employee health coverage, including a pharmacy benefit” and “any
employer subsidy moneys received from participation in the federal employer incentive program shall be
deposited in the state general fund.”
The HCA has qualified for the RDS since 2006 for UMP Classic Medicare, Kaiser Permanente WA Original
Medicare and Medicare Advantage, and Kaiser Permanente NW Senior Advantage plans. However, as
retiree premiums have increased, particularly for UMP Classic Medicare, the HCA may eventually no
longer meet the actuarial equivalence test to qualify for the RDS. The Medicare Explicit Subsidy is a key
component for PEBB to qualify for the RDS. If the explicit subsidy is fixed at a certain dollar amount,
eventually the plans’ increasing pharmacy costs will lower the value of the pharmacy benefit below the
standard Part D benefit. In other words, the plans will not pass the required actuarial equivalence test for
“net value” after the explicit subsidy is applied.
For 2024 the Legislature set the monthly retiree subsidy at a maximum of $183 per member per month.
Based on pharmacy claims costs through part of 2022 and pharmacy trend assumptions, HCA is projected

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 18
to retain eligibility for the RDS through 2025. However, this timeline may be earlier if pharmacy costs rise
more swiftly, or if changes are made to the pharmacy benefits offered by the plans.
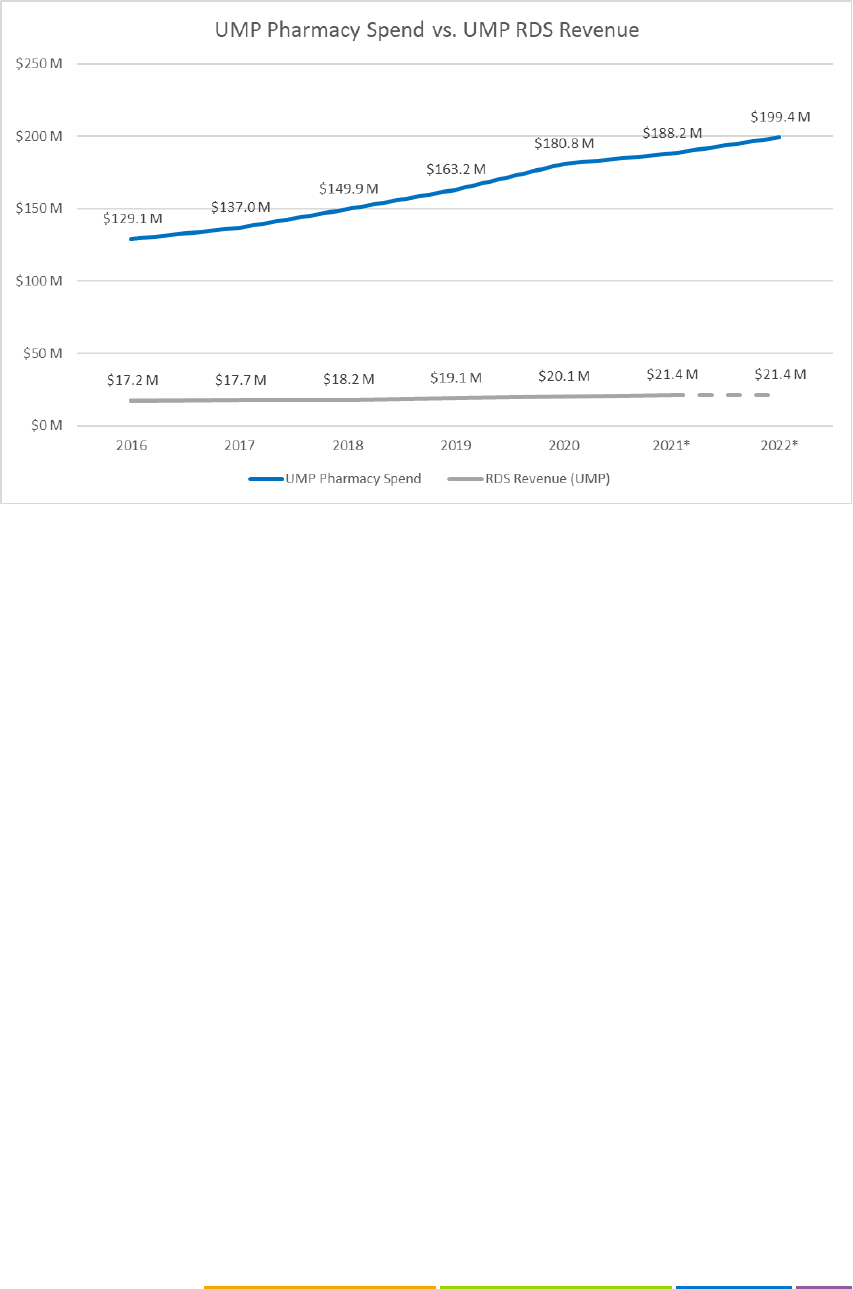
While the RDS provides revenue to the state, it is a small amount relative to what is spent on the Medicare
Explicit Subsidy and as a percentage of overall prescription drug spending. The line graphs below show: 1)
RDS revenue for all eligible plans (UMP Classic Medicare, Kaiser Permanente WA Medicare Advantage and
Original Medicare, and Kaiser Permanente NW Senior Advantage) compared to total state expenditure on
the Medicare Explicit Subsidy; and 2) RDS revenue attributed to UMP Classic Medicare from 2016 through
2021, which is the last reconciled year, compared to prescription drug spending by the plan gross of
rebates. Furthermore, the value of the RDS contributes indirectly to the explicit subsidy as a deposit into
the General Fund but is not directly factored into PEBB Medicare retiree premiums. If RDS revenue came
directly to HCA, the reduction to premiums would likely be minimal given the value compared to the
plan’s total drug costs. This would also represent an increase to the state’s investment in PEBB Medicare
premiums (i.e., the explicit subsidy).
Chart 7: Medicare Explicit Subsidy expenditures vs. RDS revenue,
2010 to 2022 (projected)
PEBB Retiree Medicare Benefits
December 1, 2023
Page | 19
Chart 8: UMP Classic Medicare Prescription Drug Cost (Gross of Rebates) vs. RDS
Revenue, 2016 to 2021
UMP Classic Medicare
UMP Classic Medicare is a self-insured coordination of benefits (COB) plan with creditable (non-Part D)
prescription drug coverage. Due to this structure, and because the plan is not eligible for several sources
of federal funding only available to Part D plans, UMP’s premium is significantly higher than other PEBB
Medicare plans. Without structural changes to UMP Classic Medicare, this trend of steadily increasing
premiums that are higher than other plans will continue.
Coordination of Benefits & COB Savings Bank
There are several ways that plans can design coordination provisions for retirees who have Medicare as
their primary medical coverage (Original Medicare Part A and Part B):
• Carve-out: the plan calculates what it would pay toward the claim (the “normal benefit”), then
reduces its payment by the amount that Medicare pays. Any remaining amount is the member’s
cost-share.
• Maintenance of benefits (MOB): the plan subtracts Medicare payments from the total allowed
amount, then applies the plan’s benefit limits and cost sharing to whatever amount remains. Any
remaining amount is the member’s cost-share.
• Coordination of benefits (COB): Medicare is treated as the primary carrier and plans pay all
amounts not covered by Medicare up to the amount that would be paid in the absence of
Medicare. This typically results in no member cost-share for Medicare-covered services.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 20
UMP Classic Medicare uses a COB approach to pay secondary to Medicare for services covered by
Medicare Part A and Part B. This means that when UMP pays secondary to Medicare, the plan covers any
member cost-sharing. If the service is not covered at all by Medicare, UMP is the primary, or only, payer.
5
COB plans have the most generous coverage levels, followed by MOB and carve-out. The table below
provides a hypothetical illustration of how member cost-share is calculated under each of these types of
coordination provisions.
Table 6: Types of coordination plans - illustration
In this hypothetical scenario a provider bills $200 for a service. The plan allowed amount, which is also the
Medicare allowed amount, is $100. In each case, the member pays a 15 percent coinsurance, and the plan
pays the remaining 85 percent. If the plan were primary, it would pay $85 of the $100 allowed amount.
But Medicare is the primary payer, and covers 80 percent, or $80 of the $100.
Under a carve-out design, the plan calculates what it would pay toward the claim, which is $85, and
reduces its payment by the amount that Medicare pays, which is $80. The plan then pays $5, and the
retiree pays the remaining $15.
Under a maintenance of benefits design, the plan subtracts the Medicare payment ($80) from the total
allowed amount ($100) and applies the plan’s benefit limits and cost-sharing to the amount that remains.
In this case $20 remains, so the plan covers 85 percent of $20, or $17. The retiree then pays the remaining
example $3 for services.
Under a coordination of benefits design, Medicare pays first ($80), and the plan pays the rest of the
allowed amount ($20). The retiree pays $0. UMP Classic Medicare also has a unique feature that allows
members to use savings accrued in their “COB Savings Bank” to cover out-of-pocket costs for the UMP
deductible or services not covered by Medicare. The COB Savings Bank transfers the plan’s savings
(resulting from Medicare primary coverage) to the member, up to the amount of the member’s out-of-
pocket spending. In other words, the COB Savings Bank gives back to retirees the amount that the plan
5
In addition to medical services and prescription drugs, UMP Classic Medicare covers benefits not
covered by Original Medicare such as massage therapy, hearing aids, routine hearing exams, and vision
care. See the 2023 UMP Classic (PEBB) Certificate of Coverage for a full listing of benefits.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 21
saves with Medicare as the primary payer for Part A- and Part B-covered services. For services not covered
by Medicare Part A and Part B, such as massage therapy, hearing aids, or vision hardware, the amount of
COB savings is typically enough to cover any out-of-pocket costs for those services plus some or all the
UMP Classic Medicare deductible.
Below is an example of how COB savings are accrued after a retiree meets the $250 UMP medical
deductible:
Table 7: Illustration of how COB Savings are acrued
In 2022, more than 95 percent of UMP Classic Medicare members accrued COB savings. Regence as third-
party administrator (TPA) tracks how much members have paid out of pocket during the year, and the
amount of COB savings accrued. They send a check to pay back out-of-pocket expenses, such as the
medical deductible or retiree cost-share, for services not covered by Medicare. Members only receive a
COB Savings Bank check for non-Medicare covered services that they have paid for out-of-pocket; UMP
Classic Medicare does not reimburse members for more than they have paid. Members who use more
Medicare-covered services accrue greater COB savings which can be used to pay for non-Medicare
benefits. The COB Savings Bank lowers or eliminates cost-sharing for members who use non-Medicare
covered services but increases overall plan costs and therefore monthly premiums.
Rate development
UMP Classic Medicare is a self-insured plan
6
that coordinates coverage with traditional Medicare and is
administered by Regence BlueShield. As the TPA, Regence provides full claims services, manages the
provider network, performs utilization management, administers specialized benefit programs, and
provides member services including customer service, plan materials, and other resources. The HCA sets
6
In a self-insured, or self-funded plan, the sponsor (typically an employer or union) pays the health claims
of the members enrolled in the plan. This is in contrast with a fully insured plan, where the sponsor pays a
per member monthly premium to the health insurance company.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 22
UMP rates each year in consultation with contracted actuaries at Milliman. The goal of this annual process
is to set rates based upon projected costs to pay claims (including statutorily mandated reserves) and
administer the plan. UMP rates do not include a profit margin.
The bid rate reflects the total average price per member, per month, to enroll in a plan. The premium is
the amount that retirees pay per month for coverage and is calculated as the bid rate minus the Medicare
explicit subsidy, plus the HCA administrative fee. The value of the Medicare Explicit Subsidy is calculated
according to each plan’s final accepted bid rate, as illustrated in the example below.
Figure 5: Illustration of PEBB Medicare premium calculation
The UMP Classic Medicare bid rate is comprised of projected pharmacy and medical costs. While UMP
coordinates payment of Medicare-covered medical services with CMS, UMP is the only payer for
pharmacy; there is no coordination with Medicare for incurred pharmacy costs. Therefore, pharmacy costs
are a significant contributor to UMP Medicare’s annual bid rate development and represent more than
60% of plan spending, as reflected in Figure 6, below.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 23
Figure 6: UMP Classic Medicare percentage of total spend by major service
categories, 2018 -– 2022
Additionally, UMP Classic Medicare covers supplemental benefits such as vision and hearing instruments
that Medicare does not cover. For these medical services, UMP does not coordinate payment with
Medicare. UMP Classic Medicare’s unique COB Savings Bank, discussed earlier, is often applied to cover
out-of-pocket retiree costs for the UMP deductible and services not covered by Medicare. The COB
Savings Bank transfers the plan’s savings resulting from Medicare primary coverage to the member, up to
the member’s out-of-pocket spending, leaving most retirees with $0 out-of-pocket medical costs. If these
savings were to remain with the plan instead of being passed to the individual member, the premium for
all members would be reduced while most members’ out-of-pocket costs would increase. This is
discussed later in the Options and Considerations section of this report.
The UMP Medicare rate is significantly higher than other plans in the risk pool due to a combination of
the cost of prescription drug coverage (which is not offset by federal subsidies available to Part D plans),
coverage for many non-Medicare covered services, and low or no member cost-sharing for non-Medicare
covered medical services through the COB savings bank. The figure below captures this dynamic (all
numbers are for illustrative purposes only).

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 24
Figure 7: Illustration of impact of Medicare subsidies on premiums
For UMP Classic Medicare, the total average cost is $1,350 per member for monthly medical and
pharmacy claims. Medicare pays primary on the portion of the medical claims that are covered by
Medicare ($700). The medical cost ($250) and pharmacy cost ($400) are not covered by Medicare but are
covered by UMP and represent the total bid rate of $650. The bid rate is discounted by the state-applied
$183 Medicare Explicit Subsidy, leaving $467 to be paid by the retiree as a monthly premium.
For the MA-PD plan, the total average is $1,000 per member for monthly medical and pharmacy claims.
The Part C medical portion ($650) and the Part D pharmacy portion ($150) of the member’s costs is
covered by Medicare, for a total bid rate of $200. The total bid rate represents the cost of non-Medicare
covered benefits (supplemental benefits) and lower member cost-sharing compared to Original Medicare.
This amount is discounted by the $100 Medicare Explicit Subsidy, leaving $100 to be paid by the retiree as
a monthly premium.
Despite paying secondary to Medicare on most medical claims, UMP total plan costs and member
premiums are higher than the MA-PD plans. This is because UMP provides full coverage for certain non-
Medicare covered medical services, reimburses members through the COB savings bank, and does not
benefit from risk-adjusted CMS Part D subsidies and Part D pharmacy discounts. Part D plans are
significantly advantaged over creditable drug coverage plans because there are several different sources
of federal funding, as described earlier in this report (Risk-adjusted direct subsidy, Federal reinsurance, and
Coverage gap/manufacturer drug discount program) that cover a large portion of drug costs and keep
premiums low.
Chart 9 shows that even before the introduction of MA-PD plans in the PEBB Medicare risk pool, UMP
Medicare had historically higher bid rates than the other plan offerings. High annual rate increases for
UMP Medicare are expected to continue in future years, particularly if members continue to shift to the
other plans.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 25
Chart 9: PEBB Medicare bid rates, 2013 – 2024
In 2023 there was a large outflow of members from UMP Medicare when the monthly premium increased
by 20 percent, or $73. As described earlier, the UMP Medicare bid rate is the projected average per
member, per month cost for the members expected to be enrolled in the plan. For the 2024 UMP Classic
Medicare bid rate development, HCA’s contracted actuaries at Milliman used a clinical risk grouping tool
to determine the relative health status and cost of members who stayed in UMP following the large
enrollment shift in 2023. The analysis found that in 2023 relative to 2022, a greater proportion of less
healthy members, that is, those who use more benefits, were retained in UMP Classic Medicare, which
resulted in increased average projected per-member cost. As future UMP Classic Medicare rate increases
are realized, additional loss of members from UMP is expected. This phenomenon is likely to continue to
intensify future UMP Classic Medicare premium increases.
2018 Medicare portfolio expansion project
As a result of high and increasing UMP Classic Medicare premiums during the 2017 rate setting process
for 2018 plan year premiums, the Legislature provided funding in the 2018 supplemental budget and
directed HCA to analyze options for stabilizing costs in the Medicare portfolio. From mid-2018 through
the end of 2019, HCA researched options to provide greater choice and value to PEBB Medicare retirees.
The goal was to identify benefit options that would allow for lower retiree premiums and out-of-pocket
costs, while maintaining comprehensive benefits with coverage levels like that of UMP. This led to an 18
month-long competitive procurement to contract with one or more MA-PD plans. There were two
apparently successful bidders, and although contracts with both bidders were possible HCA was able to
complete negotiations and reach an agreement with only one bidder for the 2021 plan year. Two
UnitedHealthcare (UHC) MA-PD plans were then authorized by the PEB Board and added to the PEBB
Medicare portfolio beginning January 2021.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 26
Overview of CMS Medicare Advantage Program
MA plans are offered by private companies approved by Medicare, and they provide a member’s Part A
and Part B benefits. In addition, the plan may cover things that Original Medicare doesn’t cover, like gym
memberships, vision, hearing, and dental services.
This type of risk-based plan within Medicare had its beginnings in the 1980s and was introduced with the
goal of reducing costs, improving choice, and enhancing quality, but MA plans have undergone significant
policy changes since their beginnings.
7
Over the last decade, enrollment in MA plans has grown considerably and in 2022 more than 28 million
Medicare beneficiaries were enrolled in an MA plan (nearly half of the Medicare population).
8
In total,
3,998 MA plans were available nationwide for individual enrollment in 2023, 228 more plans than were
offered in 2022 and the largest number of plans offered since 2010. About 5 million beneficiaries were
enrolled in Employer Group Waiver Plans (EGWP) through their employers or unions, comprising about 29
percent of total MA plan enrollment in 2021.
9
Medicare Advantage enrollment is projected to increase to
60 percent of eligible Medicare beneficiaries by 2031.
10
7
Patel, Yash M., and Guterman, Stuart, The Evolution of Private Plans in Medicare, The Commonwealth
Fund, December 8, 2017. The Evolution of Private Plans in Medicare (commonwealthfund.org)
8
Freed, Meredith, Biniek, Jeannie Fuglesten, Damico, Anthony and Neuman, Tricia. Medicare Advantage
2023 Spotlight: First Look. KFF, November 10, 2022. Medicare Advantage 2023 Spotlight: First Look | KFF
9
Better Medicare Alliance, March 21, 2022, Separating Fact from Fiction on Medicare Advantage EGWPs.
Separating Fact from Fiction on Medicare Advantage EGWPs - Better Medicare Alliance
10
Medicare - May 2022 Baseline (cbo.gov)

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 27
Chart 10: MA enrollment 1990 to 2030 (projected)
Most MA plans (89 percent) include prescription drug coverage (MA-PDs), and in 2022, 69 percent of
enrollees in MA-PD plans paid no premium other than the Medicare Part B premium. (KFF). MA plans are
allowed to provide extra benefits that are not available in traditional Medicare and can use federal
subsidies to help cover the cost of these extra benefits such as vision, hearing, gym memberships,
telehealth, or dental benefits. Other extra benefits include over-the-counter items such as bandages, meal
delivery, transportation, massage, and adult day health services. (KFF)
During the last five years, concerns about “widespread and persistent problems related to inappropriate
denials of services and payments”
11
,
12
have led CMS to issue new rules aimed at addressing some of
these concerns. The new rules, issued by CMS on April 5, 2023, are intended to ensure timely access to
care through utilization management requirements, protect Medicare beneficiaries from confusing and
11
Medicare Advantage Plans Often Deny Needed Care, Federal Report Finds - The New York Times
(nytimes.com)
12
Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns
About Beneficiary Access to Medically Necessary Care" (OEI-09-18-00260) (hhs.gov)

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 28
potentially misleading marketing, strengthen the Quality Star Ratings Program, advance health equity, and
improve access to behavioral health care.
13
Historical and projected Medicare spending
According to the Medicare Trustees report (April 2022), Medicare spending on Part A, Part B, and Part D
benefits in 2021 totaled $829 billion, up from $541 billion in 2011.
14
Projected spending growth for
Medicare is due in part to growing enrollment in Medicare due to the aging of the US population,
increased use of services and intensity of care, and rising health care costs. (KFF). Spending on benefits in
each part of Medicare (A, B, and D) increased in dollar terms between 2011 and 2021, but the distribution
of payments by Part has changed over time. Spending on Part B benefits, including physician services,
hospital outpatient services, physician-administered drugs, and other outpatient services now accounts for
the largest share of total spending on Medicare benefits. (KFF) Spending on Part D prescription drug
benefits has stayed roughly constant since the drug benefit began in 2006 and is expected to remain
constant through 2031 as shown in Chart 11 below.
Chart 11: Spending on Medicare services by Part A, B, and D
History of Medicare Advantage plans within PEBB
Group Health Cooperative of Puget Sound (GHC) was one of the earliest staff model HMOs (where the
HMO hires its own physicians) in the US and was offered as a Part C plan choice to state employees prior
13
2024 Medicare Advantage and Part D Final Rule (CMS-4201-F) | CMS
14
What to Know about Medicare Spending and Financing | KFF

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 29
to the creation of the PEBB Program. In 2003, GHC converted its Medicare+Choice plan to a MA plan with
the establishment of the Medicare Modernization Act of 2003. In 2017, GHC was acquired by Kaiser
Foundation Health plan of Washington and the plan was renamed “Kaiser Washington Medicare
Advantage” and as of May 2023 had 23,294 total members. The Kaiser Medicare Advantage plan includes
creditable coverage for prescription drugs, meaning that the plan offers prescription drug coverage at
least as generous as a Part D plan, but with a formulary that is not governed by CMS rules.
15
Kaiser Permanente NW has offered a managed care plan to PEBB members since the 1990s in counties
along the Columbia River that weren’t covered by Group Health. In 2003 when GHC adopted the Medicare
Advantage plan, Kaiser Permanente NW did the same, naming it the “Senior Advantage” plan. Today, the
Kaiser Permanente NW Senior Advantage plan is offered in Washington counties not covered by Kaiser
Permanente WA and select counties in Oregon. This plan also includes creditable drug coverage and as of
May 2023 total membership in this plan was 2,343.
In 2021 UnitedHealthcare began offering two MA-PD plans within the PEBB portfolio after negotiating the
benefit design with HCA and gaining PEBB Board approval in July 2020. The plan was designed to mirror
UMP benefits as closely as possible. The pandemic limited HCA’s ability to provide the kind of outreach it
would have liked to provide when introducing a new plan (e.g., there were no in-person benefits fairs),
and enrollment in the first year was low. As of May 2023, total membership in the two plans was 14,903.
Benefit of remaining in PEBB Medicare plans
As discussed above, SEBB and PEBB members have the opportunity, when they retire, to continue to
receive medical benefits through the PEBB Program either through COBRA or, if they are eligible, through
a PEBB Medicare plan. Because enrolling in Medicare can be a confusing process (as described in the
findings from the listening sessions, discussed later in this report), and there are many options available to
Medicare members in the individual market, the benefit of remaining in one of the plans offered through
PEBB may not be evident to PEBB members. Nevertheless, these can be substantial and include the
following:
• PEBB retirees have access to the state’s Medicare Explicit Subsidy that subsidizes a portion of their
monthly premium as described in RCW 41.05.085.
• PEBB retiree insurance coverage has less restrictive enrollment rules compared to individual
MA/Medigap products. PEBB retirees can choose any retiree plan that is available, whereas a
Medigap plan in the commercial market may deny their applications based on health status if
they apply outside of their guaranteed issued periods.
• PEBB retirees will be covered if they meet the eligibility and enrollment requirements.
In addition, there are differences in the MA-PD and Medicare Supplemental Plans offed through PEBB
versus in the individual market, including:
15
An MA-PD plan is required to offer a formulary governed by CMS’ formulary rules.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 30
MA-PD Plan:
• The PEBB MA-PD plan offerings are stable, unlike individual MA-PD plans which may terminate
after the end of a plan year.
• Some rural counties in Washington have limited access to individual MA-PD plans. PEBB members
who live in Klickitat, Pend Oreille, Lincoln, Skamania, Garfield, and Whitman counties each only
have one MA-PD plan available to them through the individual market.
• There is no enrollment limitation penalty within PEBB as there is in the individual market.
• Although some of the MA-PD plans in the individual market have $0 or low premiums, their
maximum out-of-pocket costs can be as high as $8,300. The PEBB MA-PD plan maximum out-of-
pocket costs are no more than $2,000.
• The UHC plans are rated 4.5/5 stars (a measure of quality). The individual MA-PD plans in
Washington State are rated between 2.5 and 4.5 stars.
• PEBB offers both local HMO and extended PPO plans (nation-wide coverage) whereas the
individual MA-PD plans offered in Washington State are either local HMO or local PPO.
• The Part D drug coverage offered by individual MA-PD plans has up to a $505 deductible; the
UHC plan offered through PEBB which has a $100 deductible amount.
Premera Medicare Supplement Plan F/G:
• PEBB Premera Plan G has no health screening or pre-existing condition waiting period. An
applicant who applies for a Medicare supplement plan in the individual market may be subject to
a 90-day pre-existing condition waiting period with a 90-day look back period if they apply
outside of their guaranteed issued period, such as during their Medicare initial enrollment period.
• The PEBB Medicare Supplement Plan G is one of the most affordable Plan G Supplement plans in
the market.
HCA survey of PEBB retirees
In 2020, HCA surveyed PEBB retirees to gain a better understanding of their needs. The survey was made
available on the HCA website over a three-week period in August 2020. To promote the survey HCA sent
emails to PEBB retirees through the GovDelivery system and promoted it through stakeholders. The
purpose of the survey was to hear what retirees’ priorities were when it came to their PEBB health
coverage, and to help HCA determine which areas to focus on to improve retirees’ experience with the
PEBB Program.
Responses were collected from 7,364 members, although not every member answered every question.
More than 4,500 members provided narratives, which were reviewed and analyzed by HCA staff. The
following is a summary of the survey responses.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 31
The question “How could we improve your experience as a PEBB Retiree?” had 4,212 respondents with-
34% reporting being satisfied, 29% feeling that improvements could be made to the cost of their benefits,
19% wanting improvements to coverage, and 18% listing improved customer service.
By far, the main concern of members responding to the survey was the cost of PEBB benefits, including
the monthly premiums and the out-of-pocket costs. Out of 6,766 responses: 4,397 chose “Affordable
monthly premiums”; 3,817 selected “Comprehensive benefits” including coverage for prescription drugs;
and 3,583 selected “Affordable costs” (deductibles coinsurance and copays), as the top three priorities.
(Respondents were allowed to select more than one priority.)
When asked to provide more detail, 929 members responded wanting better coverage for gym
memberships (23%), prescription drugs (20%), vision (19%), dental (12%), and hearing aids (7%).
There were 767 responses identifying the types of customer service support they felt would improve their
experience, with 30% identifying live customer service, 19% HCA communications, (15%) web customer
service, 12% outreach/other, 11% enrollment, 9% plan communications, and 4% payment options.
16
HCA has incorporated these responses into annual planning cycles and has begun to implement several
improvements which are detailed later in this report.
2022 Proposal to consider closing UMP Classic Medicare Plan
UMP Classic Medicare’s premium increases had become an issue as early as 2016 when retirees, who are
often on fixed incomes and particularly vulnerable to cost increases, began to raise concerns in public
comment at PEBB Board meetings. In 2021, HCA staff began hearing anecdotally that in some cases the
monthly premium for UMP Classic Medicare had exceeded the retiree’s monthly pension income.
Given retirees’ concerns about the cost of UMP, and projected increases in UMP premiums, in June 2022
HCA made a recommendation to the PEB Board to consider an orderly closing of the UMP Classic
Medicare plan at the end of the 2023 plan year. After many PEBB members and stakeholders voiced their
concerns with the possible closing of UMP, the PEB Board instead passed a resolution to “postpone action
on closure of the UMP Classic Medicare plan until at least January 2024 to allow staff to interact in earnest
with stakeholders.”
In September 2022, HCA began working with the Stakeholders Medicare Coalition,
17
to conduct a series of
statewide listening sessions with PEBB retirees regarding their health benefits. Although the initial request
16
Source: PEB Board meeting Briefing Book January 27, 2021 (wa.gov) Tab 6. The high response rate
requesting live customer service may have been a result of the pandemic, as such customer service
delivery methods had been suspended for months prior to the survey.
17
The Stakeholders' Medicare Coalition is made up of representatives from Retired Public Employees
Council, Washington Education Association Retirees, Puget Sound Advocates for Retirement Action,
Health Care as a Human Right, Washington State Alliance for Retired Americans, Washington State Senior
Citizens Lobby, Social Security Works Washington, the Washington Federation of State Employees, and the
Washington American Federation of Teachers. This Coalition includes a wide range of organizations who

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 32
was to offer six listening sessions with PEBB retirees, HCA ended up conducting 24 sessions. The Coalition
and HCA developed a joint statement that read:
“The UMP Classic Medicare is not closing and there is no recommendation, proposal, or intended action
by current HCA Leadership for the foreseeable future, demonstrating HCA listens to and respects the
voices of PEBB members.”
represent a significant number of the PEBB Program’s enrolled retiree population, there are also a
significant number of PEBB retirees who are represented by organizations that are not part of the
Coalition (such as Washington State School Retirees Association (WSSRA), University of Washington
Retiree Association, and Washington State University – Emeritus) and PEBB retirees who do not belong to
any formal retiree organization.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 33
Findings
2023 PEBB retiree listening sessions
From February 28 to May 31, 2023, HCA conducted 24 listening sessions with PEBB retirees to hear how
the portfolio of PEBB Medicare plans might better meet members’ needs. The sessions were facilitated by
a consultant from Ernst and Young. Twenty of the sessions were conducted virtually, and four were
conducted in person. Members were recruited largely through the Stakeholders Medicare Coalition and
were able to sign up for their preferred session via the HCA website. Participants were sent a list of
questions in advance that included what members liked about their current plan, what could be better,
and how they like to receive communication from HCA.
Participation in listening sessions
Two hundred and sixty-eight PEBB members registered for the sessions, and 193 participated. After the
initial five listening sessions, HCA researched the reasons why those who signed up may not have
ultimately participated and learned:
• The sign-up process limited the number of attendees for each group, unlike other Zoom meetings
that don’t have a capped number of attendees. Although most of the registrants were able to
access the meeting for which they had registered, it created some confusion and even impacted
the observers from the Coalition and HCA for the first few meetings. The issue was identified, and
participation instructions better clarified how to attend the meetings, which resolved the issue for
the rest of the listening sessions.
• HCA determined that users were having trouble finding the original confirmation email that they
had been sent, which has a unique login link. This was addressed by HCA resending the
confirmation email with the unique link the day before the event.
• HCA attempted to contact anyone who had registered but hadn’t logged in by the start of the
listening session to help with technical issues. These contacts were made either by email or by

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 34
phone, when possible. HCA also offered to help users sign up for a different session if they were
no longer able to attend the one they had signed up for.
• In some cases, HCA learned that a registered attendee had changed their mind and didn’t cancel
their registration. Reasons included not feeling well, needing to focus on home repairs, or
thinking that what they signed up for was a webinar. Some registrants never responded to the
day of outreach. HCA was able to change the Zoom confirmation language to highlight how to
cancel the registration if the attendee’s plans changed.
• Some registrants had technical challenges that could not be resolved. In those few cases, HCA
encouraged attending an in-person session if possible.
After discussion with the Coalition regarding recruitment efforts, HCA began connecting with retiree
organizations such as Washington State School Retirees Association (WSSRA), University of Washington
Retiree Association, and Washington State University – Emeritus (entities who are not part of the
Stakeholders Medicare Coalition) to encourage attendance. HCA staff also reached out to Eastern
Washington University, Central Washington University, and Evergreen State College to encourage retiree
participation in the in-person sessions near those campuses, as well as in the online sessions. In addition,
HCA created a script for the HCA customer service staff to use at the end of retiree phone calls and in-
person lobby visits.
While most participants were in Washington, there were members with experience accessing PEBB
Medicare benefits from Arizona, California, Florida, Idaho, Oklahoma, and Oregon. The ability to travel
while maintaining coverage was often cited as one of the benefits of several of the plans. Although an
effort was made to ensure broad participation from members in each plan, UMP and UHC members were
slightly over-represented in the listening sessions, while Kaiser and Premera members were
underrepresented. Of the 193 members participating in the listening sessions, 88 were in UMP, 46 in UHC,
32 in Kaiser, 15 were in Premera, and the balance was made up of participants who had not yet retired but
were interested in learning what other members were saying about their plans in anticipation of signing
up for Medicare.
18
Members’ experience with their plans ranged from as little as four months to as long as
40 years.
18
UMP membership is 42 percent of total PEBB members compared with 49 percent participation in the
listening sessions. UHC membership is 13 percent of total PEBB members compared with 25 percent
participation. Kaiser members are 23 percent of total PEBB membership compared with 18 percent
participation. Premera is 20 percent of PEBB membership but only 8 percent of participation in the
listening sessions.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 35
Chart 12: Listening session participation by plan
Limitations
While the number of listening sessions offered many opportunities for members to participate, it should
be noted that the opinions expressed through the listening sessions may not be fully representative of the
PEBB membership overall. Recruitment efforts for attendees prioritized retirees from the Coalition’s
organizations, which worked with HCA over a series of months to create the format and content of the
listening sessions. Members who are unaffiliated with the Stakeholders Medicare Coalition participating
retiree associations may not have been aware of the sessions and so were less likely to participate. In
addition, although most of the sessions were held online, which provided access to members regardless
of where they lived, it limited participation to members who have access to a computer and who are
comfortable using Zoom technology. The in-person sessions were held in four locations across the state
to allow face-to-face participation from members in different regions, however, lack of transportation may
have been an issue for some participants. In addition, the UHC enrollees had at most two years with the
plan (and many had only four months of experience), so comments, both negative and positive, may
reflect limited experience with that plan.
Qualitative analysis - themes from the listening sessions and public forums
Comments from the listening sessions were categorized into themes using the affinity diagram
methodology, where comments are organized into groups or themes based on their relationships.
Representative quotes from participants are included to demonstrate member feedback on their needs,
expectations, understandings, and desires for improvement. The full set of summary notes from the
listening sessions, including additional comments from the Coalition, is included in the appendices.
Summary comments and themes from the listening sessions are shown below first, by health plan, and
then, by overall theme.
0
20
40
60
80
100
UMP UHC Kaiser Premera
Participants
Participation by Plan

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 36
Health Plans
Kaiser
Positive Comments: Members reported that the plan offered good coverage and felt they paid very little
out-of-pocket even though they had received very expensive treatments. They felt the prescription drug
cost was affordable and liked the fact that they only had copays when seeking specialty care. One person
described it as a “self-contained system” with all the coordination between providers done internally
rather than the individual having to do it. Members liked the coordination and that they can get their lab
tests, x-rays, and prescriptions done in one place.
Negative Comments: A few members reported having been with Group Health previously and when it
was acquired by Kaiser, they felt that the quality of care had declined. Members commented on limited
provider availability and reported that wait times to see a doctor or get a response can be long,
sometimes as long as one or two months to get an appointment, and there is no guarantee that you can
see your primary care physician. Seeing a new doctor who is unfamiliar with your needs for each
appointment is a concern.
Some members felt that decisions were not made locally but with Kaiser in California. Several members
expressed disappointment that they were unable to have the same coverage in other states, even though
Kaiser has a presence there, and there was some confusion about the difference between Kaiser Original
Medicare and Kaiser Medicare Advantage plans.
Members in rural areas expressed frustration with the mail order prescription service known as “First Fill”
and worry that they can’t talk to their local pharmacy as they once could.
19
19
Kaiser Permanente WA’s First Fill Program was designed to be safer and more cost effective for
members by requiring that maintenance drugs—those for long-term use—would be filled via mail order.
The policy stated that members could fill their first prescription at any in-network pharmacy, where
pharmacists could review the prescription to ensure members avoided negative drug interactions and
other risks, but subsequent refills must be filled via mail order or at a Kaiser Permanente retail pharmacy.
This allowed the use of generic drugs when medically appropriate and allowed Kaiser Permanente
Washington to negotiate better drug prices. The program was removed for the 2024 plan year because of
member dissatisfaction and the inherent risks of delivery via mail for rural members without secure mail
drop points.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 37
Premera Plan F/G
Positive Comments:
Members felt that the plan had good coverage, and liked the fact that there are no
deductibles, you never have to worry about copays, and it is affordable. They liked the flexibility the plan
offers in seeing physicians, and several reported that they haven’t had any issues. Members liked that it
was a “traditional Medicare” plan. One person reported having a rotator cuff injury and was able to go
straight to an orthopedic surgeon without seeing their family doctor first. They were able to get an MRI
within two days. Another participant noted that the lower cost of premiums made the cost of eyewear
more affordable.
One of the members felt that “Plan G does not get adequate exposure (i.e., positive promotion); after the
deductible it pays everything…PEBB needs to do a better job getting information out about Plan G.”
Negative Comments: Several members felt that the “benefits were skinny,” and wished the plan covered
things such as hearing, vision, a gym membership, and naturopathy.
Members did not like having to wait for approval to get a referral, and although they liked being on
“Original Medicare” they did not like the fact that they must sign up for a separate Part D plan, which is
not available through PEBB, and a separate dental plan. They felt that signing up for those additional
plans and then managing multiple bills is challenging.
Uniform Medical Plan
Positive Comments: Members liked the dependability of the plan and the fact that it can be used
anywhere. They felt secure that any health care needs will be taken care of.
• “You don’t need to worry about what will be paid or not. Health is stressful enough.”
There is no delay in treatment. They felt that it provided excellent access to providers, with a minimum of
pre-authorizations, denials, and appeals. Several stated that it had been important to have UMP as they or
their spouses experienced serious health concerns. They liked that it offered a seamless transition
between coverage as an employee and coverage as a retiree, and coverage includes benefits that
Medicare does not cover, including chiropractic, massage, acupuncture,
20
vision, and hearing aids.
Participants felt that the travel coverage was good, and several mentioned that their physicians are happy
that they have UMP coverage since Regence is known to pay physicians promptly.
The UMP members felt that the drug coverage was good, and at least one member indicated that they
were on a medication that is effective for them and that only UMP covers it. For the most part, members
reported receiving good customer service when they called the plan, and they appreciated the relative
ease of getting reimbursement for services such as naturopathy, and physical therapy. Participants liked
20
Starting in January 2020, Medicare began covering acupuncture for low back pain. Acupuncture
coverage (medicare.gov)

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 38
the fact that UMP is a state-sponsored plan, and not operated by a private, for-profit company because
they are concerned about what they see as an increase in the privatization of Medicare. Finally,
participants liked that UMP is “traditional Medicare” and does not have the incentives that some MA plans
are perceived to have to deny coverage.
Negative Comments: Many UMP members reported that they felt that the cost of premiums was high,
although some members felt that the value they received was worth the cost. A few members said they
want the best coverage they can buy, even if they must pay more. As one member put it, when asked
what could be better about UMP: “The cost, but I wouldn’t trade benefits in order to lower costs.”
A few wondered why UMP was so expensive and if it was worth the cost. Some said that the increasing
cost of the premiums had driven them to try out another plan, even if only temporarily. Many of the
participants attributed the cost of the premiums to the fact that UMP does not receive the same federal
subsidies that the Medicare Advantage plans enjoy and would like to see HCA and their legislators work
to try to fix what they see as an unfair playing field. They objected to what they see as the privatization of
a federal program and were concerned that this was the direction that Medicare was taking.
A few members had concerns about the length of time to get an appointment, although acknowledging
that this may be due to provider shortages. In a related comment, one member said that there were no
massage therapists in their area who would take UMP because the provider payment is so low, and
another felt that UMP requirements for mental health counselors to continue to qualify made it more
difficult for their provider.
One member was unhappy with the process they had to go through to get the right medication but felt
this might be an issue that needs to be addressed at the federal level.
Some said that they would like to see an improved vision benefit, that dental services should be offered,
and they wished that the plan offered a gym membership.
United Healthcare
Positive Comments: Although most members had relatively little experience with this plan since it has
only been offered since 2021, many reported positive experiences with the plan. They liked the lower
premiums, that they could keep their same doctors, and coordinating services is easy. They liked the $0
copays, the massage benefits, and the gym benefits. As this was a new plan, several members said they
had worked hard to understand what would be different from their previous plan, and what they would be
missing by not being on UMP. One member indicated that so far, they have been able to see any doctor
that they would have seen on UMP.
Several members expressed appreciation for the state offering an MA plan.
• “The state has done a great job of negotiating an MA plan to give us some good benefits. Some of
them are better than UMP.”
One member said they were grateful that the state was offering the MA plans, since the costs are lower
than what is available in the general market. But some members felt that they did not completely

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 39
understand what was in these offerings. Also, since the plan is so new, there was some skepticism that the
plan would turn out to be as good as it initially appeared.
• “The power of a very large group and the negotiation power has been great. So far so good. Check
back with me at the end of year. “
One member said they always had UMP but switched in January to UHC and had no adverse issues with
the plan. The cost is much lower than UMP and all their doctors are in network. Another member said they
had a lot of referrals for tests with no denials from UHC. One member who “almost exclusively used
alternative health care providers” said that they were “thrilled that UHC covers chiropractic, acupuncture
and naturopathy pretty completely.” Another member said that they wished they had switched to UHC
when the plan first became available.
• “It has been a godsend because my wife and I had serious health issues, and the coverage was
phenomenal.”
Negative Comments: Members expressed frustration with UHC customer service and criticized the fact
that there was not a dedicated phone line as they had anticipated. Some said that the customer service
representative had no special knowledge about the plan and couldn’t answer questions and that it was
hard to get information about prescriptions. Several members had negative experiences with the Optum
mail order through UHC. They described errors in filling the prescriptions and mailing them to the
members, although they have used mail order successfully in the past. Although some members reported
satisfaction with the coverage, and reimbursement process for services such as massage and naturopathy,
others cited it as a frustrating experience with reimbursement taking a long time.
Some members said they were uncomfortable with the fact that UHC is a for-profit insurance company
and that they were in essence giving money to a private company. A few members noticed that their
medication copays were higher than when they were on UMP.
One participant said they were not happy with the plan as the gym membership was not useful to them.
They were told that the plan would reimburse them for physical therapy with massage but then they were
reimbursed for less than what they paid, which felt like a “bait and switch.”
A few participants said they felt overwhelmed with the amount of information from UHC in the form of
calls, emails, and mail. These included requests to check in to make sure medications were being taken,
and requests to send out a doctor and a nurse for an in-home visit.
Additional themes from the listening sessions
Assistance in plan selection
One common theme throughout the listening sessions was the desire to have more information
to compare plans, and more assistance in understanding which plan to select. It is worth noting
that the in-person benefit fairs, that are normally held in October and November of each year,
were suspended for two years during the pandemic emergency and retirees, who normally attend
these to learn more about the plans, had to find other ways to get assistance in plan selection.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 40
Also, PEBB has a policy of passive enrollment, i.e., if you do nothing during open enrollment your
plan choices remain the same. Until members were faced with a steep increase in UMP premiums
for 2022, they were less inclined to want to consider changing plans and weren’t seeking
information on the plans either from HCA or other sources. Finally, retirees who were considering
changing plans were unfamiliar with the new UHC plans and required more assistance before
deciding if this would be a good choice for them.
Members wondered about the differences between HMOs and the other plans and wanted help
in understanding how the prior authorization process worked. A few members wondered why
they should stay with a PEBB plan and not use a market-based plan, particularly since they are
told that if they leave PEBB they can never come back into it. The SHIBA Program, the WEA and
RPEC were all mentioned by participants as valuable and trusted sources of information when
deciding what plans to choose. At least one former SEBB member recalled having an interactive
plan selection tool available when SEBB was initially launched and suggested that something
similar might be helpful for PEBB retirees. A few participants had the inaccurate perception that if
they changed from UMP to another plan, they could never re-enroll with UMP.
• “When the UHC plan came out in 2022, I was trying to figure out how the two plans (UHC/UMP)
could be so comparable and such a difference in cost. I couldn’t find anyone to talk to and PEBB
didn’t have any guidance either. So that was a concern.”
Members said that open enrollment was a confusing time; it is difficult to change plans and the
timing is bad because of the conflict with the federal Medicare open enrollment and the holidays.
It is frustrating that there are only twenty working days in November and the forms must be
received by the last day of the month. They appreciated the Zoom webinars that are presented to
retirees and being able to attend an in-person benefit fair.
• “The open enrollment period is very short, and I would like to have more time to consider options.
Alerting people to something earlier would be a good idea. HCA should provide something three
months in advance that compares plans.”
One participant said that they appreciated dealing with the HCA customer service and found that
dealing with a live person was more helpful than just having the online forms. However, some
said that the wait times to speak with an HCA representative are very long.
• “It’s a foregone conclusion that you are going to be on hold with PEBB because there are not
enough people to answer questions.”
• “I had to call PEBB with some questions when I was first retiring, and I was on hold for 1.5 hours. A
call back system would be great.”
Medicare Enrollment
A common theme among participants was that the process of retiring and signing up for
Medicare with the federal government and separately with the state for the PEBB health plans was
confusing and overwhelming. Members were sometimes surprised that they were now writing
several checks for their coverage to Medicare, HCA, and for their life insurance. The process of

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 41
retiring and signing up for Medicare left many participants feeling confused and anxious. As one
participant said: “Lots of effort is made to try to prepare people and [provide] options but [HCA]
should provide an overall sense that it’s not going to be like it was, [it’s] going to be really
different, so people are not so shocked with the complexity.” Another member felt that “the sign-
up process with PEBB is a complete and total labyrinth.”
• “It’s the signing up for me. I was panicking with the wording on how to sign up for insurance. I
wish I just got a postcard that said, ‘this will be seamless, you had Medicare before, and you will
still be on UMP.’”
• “I retired from teaching in September 2022, and I found it to be one of the most confusing
processes. Especially the health insurance part. I thought I would be eligible for Medicare, and I
would need to purchase additional insurance. I don’t understand the Medicare Advantage.
Deductions are taken out from Medicare and my health care premiums. I understand that MA is
Medicare. It’s Medicare Part C so it covers drugs and throws in some other things like glasses and
maybe dental. I’m not clear what I’m buying.”
Communications
In addition to wanting to understand the plans and have better comparisons of the plans,
members said they were surprised to find out that HCA was planning on closing the UMP Classic
Medicare plan and only found out through their retiree association. They were surprised that the
information on discontinuing UMP was not in the PEBB quarterly newsletter.
Multiple attendees stated that they preferred email communications, but there seemed to be a
consensus that mail was important too, since they like to retain the hard-copy information that
HCA sends out so they can refer to it later. Emails tend to get lost.
• “Having something arrive in the mail, I pay attention to that. But I also appreciate getting email
reminders.”
While some felt the website was helpful, others felt it was cumbersome and difficult to use.
• “The HCA website is hard to manage and not very user-friendly. It is hard to get to where you
want to go; hard to find things.”
Participants felt that significant changes in plans or rates should be communicated via mail.
• “Retirees have more medical issues and have a bigger stake in these decisions. If there’s
something really important that people need to know (rates or plan no longer available) it should
be in a letter not email.”
• “I’m a tech person but I like paper, I don’t like backing things up to the cloud. I appreciate hard
copies, but I don’t have to have them.”
• “I am a Luddite. I feel that way about most electronics. It doesn’t mean it shouldn’t be used. Most
things I get that I want to keep, I print it.”
• “Emails with very clear subject lines would be helpful.”
• “Every person’s needs are different. What I think would work is a good website to start with. A lot
of specificity so you can drill down into a subject as far as you want.”

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 42
Medicare Advantage plans
Some participants expressed the desire to have a health plan that is “consumer oriented rather
than profit centered” and are concerned that Medicare is forcing people into MA plans without
their knowledge. One member expressed concern about what they saw as an increase in the ACO
REACH program
21
and the fear that “Wall Street taking over Medicare would result in higher
costs.” Several members who attended the listening sessions expressed the concern that
Medicare seems to be headed toward more privatization.
• “When you are part of an MA plan, the money is going into private pockets and not back into the
system and I don’t like that. I don’t want to go back to what it was before the Affordable Care Act
when it was all private.”
One member said that they wanted “traditional Medicare run by a not-for-profit company that is
more in line” with their values. Several members cited newspaper articles indicating that UHC and
other MA plans were under investigation for incorrect charges and billing practices. One member
said they were concerned that the low rates currently charged by UHC were a loss-leader to grow
their membership within PEBB and that they will increase their premiums later.
• “I don’t trust United. The media is full of stories about the company not being trustworthy. I am
concerned that if UMP goes away, UHC will be more expensive and less trustworthy. I want the
state to do whatever they can to advocate for subsidies from the federal government for UMP.“
• “We need to be equal with the private sector. They shouldn’t get a handout that we don’t get.”
Provider availability
Many participants shared their challenges related to the healthcare system in general. These
comments were not attributable to a specific health plan but seemed to be a common theme
across all the plans. Access to providers can be challenging in certain communities, but especially
in rural areas where it can be hard to find a physical therapist. A few members expressed concern
that providers aren’t available for people on Medicare because Medicare doesn’t pay doctors
enough.
• “There is a dearth of doctors and providers; there is a loss of specialists. You need to take care of
yourself. How about the people who are incapacitated; how are they dealing with this, if I am
having issues?”
21
The Accountable Care Organizations Realizing Equity, Access and Community Health model, (ACO
REACH), encourages health care providers to form an Accountable Care Organization to improve care and
manage costs for patients. In this model, participating providers accept Medicare claims reductions and
agree to receive at least some compensation from their ACO. The model puts a strong emphasis on health
equity and ACOs have to develop a plan for health equity. Beneficiaries in ACO REACH keep all of their
rights, coverage and benefits and can see any willing Medicare provider. ACO REACH Brings Next Era of
Medicare Payment Models (ajmc.com)

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 43
Preserving UMP
Members expressed concern about the possibility that the plan they had always relied on would
not be available in the future and they want to preserve it.
• “I was distraught when I thought UMP wouldn’t be available. It is a godsend, and I don’t want it to
go away.”
A few members said that, although the UMP Plan was more expensive, they were willing to pay
more for quality care. A few members suggested using higher drug copays to help keep costs
lower in the UMP plan.
• “I chose to work for the state because of the medical and retirement package; enjoyed state
service but it was part of the tradeoff for lower salary to have better retirement benefits.”
• “Cost is my biggest concern. I have worked since I was 15 years old and I saved and I contributed
to my savings plans, I paid for myself to get through school. I’ve been fiscally responsible and
even with that, is the money that we’ve saved going to last?”
There was a sense that the subsidies received by the MA plans presented an unfair advantage and
the belief that the state-sponsored plan should receive those same subsidies.
Listening sessions
Several participants said that they appreciated the opportunity to provide feedback directly to
HCA via the listening sessions, and wondered how the listening session feedback would be used
to improve services and address their concerns.
• “Thanks for being receptive to the concerns about losing UMP and doing these sessions and
getting feedback.”
• “I appreciate the listening sessions and because I am in Kentucky and can’t participate in person it
gave me a chance to give my input.”
• “I debated if I knew enough to participate in the listening session and I was anxious and not sure
what I was going to say, getting all the materials, etc. But I really appreciate the process and I’ve
learned a lot.”
• “I do appreciate how thorough PEBB is to keep in touch. There is a sincere desire to know how we
feel about the plans. And I feel like I am being heard. I don’t expect miracles, I do expect to be
treated with respect and I am getting that.”
Public forum comments
HCA held a series of three public forums in April and May 2023. Like the listening sessions, participants
were recruited largely through efforts by the Stakeholders Medicare Coalition and participants could sign
up through the HCA website. The forums were not as well attended as the listening sessions: out of 90
open slots, 17 members participated in the forums. The format of the meetings differed from the listening
sessions in that, although the Public Forums were held using Zoom, the sessions were not facilitated and
allowed the speaker three minutes to deliver any message of their choosing. Nevertheless, many of the
themes were like those in the listening sessions.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 44
Assistance with plan selection
• “We want more information about the ways to change from one plan to another, and what points
to consider before changing.”
• “We need people on the phone and in person, as well as the web to provide information about
these changes that people are trying to make.”
• “HCA could provide more information about prior authorization and provide links to prior
authorization policy for different plans in the newsletters on the rates. They should include the
denial rates for claims for each insurer.”
• “Overall, my ask is that HCA provide more information that is clear and complete to make
appropriate health care choices.”
• “We need better education about plan choices.”
• “The good thing about HCA is if you are placed on hold or have trouble with the website, you can
go down to their headquarters and see someone face to face. I got my questions cleared up right
away.”
Medicare Enrollment
• “It was challenging, and the premiums are much higher than were paid as an active employee”.
• “There needs to be more clarity for people who plan to continue working…I have an MBA and I
want to cry sometimes with how complex and difficult it is. I wonder how many people out there
just give up.”
• “We need better education for those near retirement to choose the best plan based on lifestyle,
such as traveling or living in two states.”
• “It was never explained to me that as a retiree I now pay about four times as much as I paid in
premiums as an active employee.”
Medicare Advantage
• “It is a fact that Medicare Advantage plans are profit driven. UHC only adds to the confusion;
several friends thought Medicare Advantage was real Medicare.”
• “What is being done to educate the Washington federal congressional delegation about the fact
that UMP Classic Medicare can’t get the same subsidies given to Medicare Advantage plans?”
• “Private equity is destroying the health system in this country.”
Preserving UMP
• “UMP premiums are the highest, but don’t let that scare you. It has worked for my wife and
I…coordination with original Medicare works seamlessly.”
• “I would like to see UMP cost less.”
• “I like what I have, and I want to keep it. I have friends who switched to the United Healthcare
plan, and they will live with it for a year and then tell me what to think about it.”
• “A COB plan should always be part of the portfolio.”

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 45
Concern about costs
• “I am paying so much [for the Kaiser plan] but it is not clear to me what I am getting for that
money compared to the marketplace plans.”
• “What steps are being taken by HCA to decouple the pharmacy benefit from UMP?”
• “Are a small group of people taking very expensive drugs, driving up the cost?”
UHC
• “The process for establishing naturopathic doctor claims reimbursement has to be fixed; it is
totally broken…Naturopaths won’t bill United directly, so you have to pay and get
reimbursement.”
• “I have specific concerns about United’s customer service…They should have specially trained
agents for PEBB Complete and PEBB Balance.”
• “It seems very patient centered. There are more resources like gyms and home health visits…I
have never had an issue with accessing the plan and I have seen specialists. All of my providers
are covered. I never had one who didn’t accept the plan.”
Listening Sessions
• “It is a disservice to not have the listening sessions recorded or notes not taken by an unbiased
professional notetaker or scribe”.
Quantitative Analysis
Each comment in the final version of the summary notes from each of the listening sessions was
categorized in several ways: Plan Type, Statement Type, and Message Category. Plan Type aligned
statements with the relevant plan type or category of question from the listening session. The options
included UMP, UHC, Kaiser, Premera, General, Communication, and Motivation. The Statement Type
categorized statements based on whether it was Positive, Negative, or Neutral. Message Category
involved sorting statements into options, such as "High plan cost" or "I like my plan." After the
categorizing of all the statements, results were tabulated, and charts created to highlight the most
frequently mentioned messages received from the participants.
It is important to note that these charts display the messages with the highest frequency of mentions, not
necessarily the number of participants who mentioned it. This limitation, along with those mentioned at the
beginning of this section related to participant self-selection, should be considered when drawing
conclusions from the data. While not statistically significant, the data in these charts is nevertheless both
representative of the responses from the participants in the listening sessions and is consistent with the
themes from the qualitative analysis.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 46
Chart 13: UMP top mentions
UMP members feel their plan is costly but want to keep it as an option. They feel that the coverage is
good, they like the plan, and feel that UMP is worth the cost. They like the provider availability but feel
that UMP has an unfair disadvantage compared to the MA plans because it is unable to receive the
federal subsidies that they receive. Members like the travel coverage. They feel that the overall cost of
prescriptions is driving up the cost of the premiums.
Chart 14: UHC top mentions
0 10 20 30 40 50 60 70 80
Travel coverage good
Drug coverage needs improvement
Subsidy, advocacy members/HCA
Provider availability, good
Like my plan
UMP worth the cost
Keep UMP option
Coverage, good
High plan cost
UMP Top Mentions
0 10 20 30 40 50 60 70 80
Mail order drugs needs improvement
Switched from UMP due to cost
Plan ok so far
Need plan information
Coverage, good
Concerns with Medicare Adv. Plans
Improve customer service
Like my plan
Low cost
Drug coverage needs improvement
UHC Top Mentions

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 47
UHC members felt that the drug coverage was more costly than they expected (coinsurance vs. copays)
22
and were unhappy with the Optum Rx administration. They liked the low cost of the plan, and in general,
said they liked their plan. They would like UHC to improve its customer service, but felt the coverage was
good and that the plan is okay, although their experience with the plan is short. Participants had concerns
about MA plans in general and felt that UHC had a little too much outreach. A number mentioned that
they switched from UMP due to cost.
Chart 15: Kaiser top mentions
Kaiser members felt that their coverage was good, and they said they liked their plan because of the
coordination and quality of care, and the low cost. They had concerns about provider availability and the
coverage and felt that appointment scheduling was challenging with long wait times for appointments.
22
UHC pharmacy benefit design initially included coinsurance, where the member pays a percentage of
the cost of the drug. This was changed to a copay, where the member pays a set amount for the drug,
e.g., a $5 copay, to provide members with greater certainty about their out-of-pocket costs.
0 10 20 30 40 50 60 70 80
Long wait times for appointments
Coverage, needs improvement
Low cost
Care quality, good
Coordinated care, good
Provider availability, limited
Like my plan
Coverage, good
Kaiser Top Mentions

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 48
Chart 16: Premera top mentions
Premera participants liked their plan overall, felt that the coverage was good, the plan is low cost, and the
provider availability was good. They don’t particularly like the fact that they must separately purchase a
Part D drug plan. A number had switched recently from UMP and felt that given the short time they had
been on the plan, they felt it was okay.
Chart 17: General themes
Participants mentioned that they had concerns about MA plans, which they see as a move toward the
privatization of Medicare. They would like to have better communication, more information to be able to
0 10 20 30 40 50 60 70 80
Plan ok so far
Switched from UMP due to cost
Plan comparisons
Drug coverage/cost, needs improvement
Provider availability, good
Low cost
Need plan information
Drug coverage good
Like my plan
Coverage, good
Premera Top Mentions
0 10 20 30 40 50 60
Long wait times for appointments
Profit focus/privatized
Appreciate/like HCA listening sessions
Customer service, needs improvement
Improve communication
Open Enrollment help selecting plans
Concerns with Medicare Adv. Plans
Plan comparisons
Need plan information
General Comments (Not plan specific)

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 49
compare the different plans and would like to have help during OE in selecting or changing plans. They
appreciated the listening sessions and appreciated that HCA and PEBB had negotiated better plans than
they could get on the individual market.
Chart 18: Motivation for listening session participation
Participants mentioned that they appreciated the listening sessions and being able to provide input to
HCA. They were not happy about the proposal to close UMP and appreciated that their retiree
associations were able to share information with them. They felt strongly about the impact that health
care has on their lives and would like to see members and HCA work together to improve
communications and improve the plans.
Chart 19: Communications preferences
0 2 4 6 8 10 12 14 16 18
Like my plan
Want to hear from other retirees
HCA/PEBB, thanks for good plans
Healthcare impacts us
Need plan information
Members not happy about recommendation
Retiree associations help share info
Get retiree input
Want to provide input
Appreciate/like HCA listening sessions
Motivation for Participation
0 20 40 60 80 100 120
Lobby
Text
Zoom/Webinar
Website
Benefit Fairs
Email
Mail/Paper
Communication Preferences

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 50
Many participants indicated they appreciated all the different ways that HCA communicates with
members, including paper/mail, emails, website, videos, the HCA lobby, in-person events (e.g., benefit
fairs), and online events (webinars). They want HCA to continue using all these communication methods.
Most participants indicated a preference for receiving communications through both paper and email.
Some participants felt it was important to bring to HCA's attention that there are retirees who do not use
computers or access the internet. For this group, receiving information through paper communications
was deemed crucial and valuable.
Participants also identified some areas for improvement, including:
• Emails should include HCA in the subject, so that member knows the email is from HCA.
• Emails should provide links to where to find additional information on the HCA website.
• Communications material should be plan-specific.
• All newsletters should include retiree-specific information.
• Improve website navigation.
• Improve plan comparison information.
• Improve open enrollment processes, communications, and support.
• Improve customer service (i.e., HCA and plans).
50 State comparison of state-sponsored health benefits for public
sector Medicare retirees report
The budget proviso requires HCA to “conduct an analysis of government self-insured plans with benefits
that are equal to or richer, and with more affordable premiums, than Uniform Medical Plan Classic
Medicare.” HCA received assistance on this analysis from its contracted actuaries at Milliman, who
maintain a proprietary data library with information on state-offered health plans in all 50 states. The full
report is available in Appendix 3. The slide deck of the report that was presented to the PEB Board in June
2023 is included as Appendix 4.
Milliman researched how other states provide health benefits to state government/public sector retirees
who are enrolled in Medicare, including the types of plans that are offered, the benefits that are covered,
premiums, and whether and how states provide subsidies. At a high level, the report found that there is
great variability in employer-sponsored supplementary Medicare coverage for state retirees. Few states
offer self-insured COB plans, and none have benefits equal to or richer than UMP Classic Medicare with
lower premiums. Washington is unique in that it is the only state offering every type of employer-
sponsored Medicare plan identified in this analysis.
Employer sponsored health benefit options for Medicare retirees
Employers have several options for offering health benefits to retirees who are enrolled in Medicare.
Medical
• Coordination of coverage plans pay secondary to Medicare for services covered by Original
Medicare, which includes Part A and Part B. Part A covers hospital care and Part B covers doctor
visits (as well as durable medical equipment, vaccines, and infusion therapies). These plans often,
but not always, mirror coverage provided to employees and may also include pharmacy coverage.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 51
• MA plans cover all services under Parts A and B of Medicare. They usually include additional, non-
Medicare benefits and often also include pharmacy coverage under Part D.
• Medicare Supplement plans cover some degree of member cost-sharing under Original Medicare
and do not include pharmacy coverage.
Pharmacy
• States may offer medical plans with or without prescription coverage, or standalone prescription
drug plans under Medicare Part D.
• States can provide pharmacy coverage through a self-insured or fully-insured Part D prescription
drug plan, which has a standard benefit design defined by CMS with the option of enhanced
coverage. Part D plans can be standalone or integrated with medical coverage and are
administered by private insurance companies or pharmacy benefit managers.
• States can also provide pharmacy coverage that is not through Part D and that is integrated with
medical coverage. If the prescription drug coverage is at least as rich as the standard Part D
benefit it is considered creditable and may be eligible for the RDS.
The map shows the distribution of Medicare retiree plan types by state. Twenty-nine states have MA
plans, twenty states have Medicare Supplement plans, and twelve states have coordination plans. Of the
six states without plan options for Medicare retirees, three offer a subsidy through a Health
Reimbursement Account (HRA) that retirees can use to purchase coverage through the individual market.
For states that offer retiree plans, the average number of plans is approximately four, but the range is one
to twenty. Washington’s offerings are slightly higher than the average (excluding the Kaiser WA Original
Medicare plan and the grandfathered Medicare Supplement Plan F, which is not open to new enrollment).
Greater plan choice appears to correlate with larger retiree populations and/or regional availability of
plans.
Many states choose to offer plans that are fully-insured. MA plans are always fully-insured, but Medicare
Supplement plans may be fully-insured or self-insured. Twenty states have only fully-insured plans and
eleven states have both fully-insured and self-insured plans. Thirteen states have only self-insured plans
that are coordination plans or Medicare Supplement plans. As stated previously, there are six states that
do not offer any plans to Medicare eligible retirees. Fifteen states offer only an MA plan to their retirees,
and fourteen states offer a Medicare Advantage plan along with another type of plan (either Medicare
Supplement or coordination plan[s]). Washington is the only state that offers all three types of plans to its
retirees: MA, Medicare Supplement, and coordination with Medicare (COB).

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 52
Figure 8: Summary of Plan Options by State

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 53
Benefits and premiums
The study found that benefit provisions vary widely according to factors such as whether a plan has a
narrow or broad network; the cost-share structure, including deductibles, out-of-pocket limits, and
coinsurance or copays; and the services that are covered. As mentioned, some states do not offer any
plans to public retirees.
23
In addition, there is wide variation in the amount of premium charged to public retirees. The total
premium is the entire monthly amount charged by the insurance carrier or set by an employer for a self-
insured plan; the retiree premium is the monthly amount charged to retirees who enroll in the plan. These
may be the same or they may be different if an employer offers a contribution toward the premium. State
subsidies, if available, may take the form of a fixed dollar or fixed percentage of total premium regardless
of what plan a member selects, or may vary based on the cost of the plan, the type of plan, a retiree’s
years of service, or other factors. The fixed contribution approach is the most common, and this is how the
explicit subsidy is set by the Legislature in Washington.
The median total premium for all MA plans was $200 with a minimum of $0 and a maximum of $625. For
Medicare Supplement plans the median total premium was $411 with a minimum of $96 and a maximum
of $660. Coordination plans had a median total premium of $462 with a minimum of $213 and a
maximum of $699. The lowest cost coordination plan with a $213 total premium does not include
prescription drug coverage.
Table 8: Summary of total 2023 monthly premium by state
(before employer contribution, if any)
Medicare Advantage
Medicare Supplement
Coordination with
Medicare
Median
$200
$411
$462
Minimum
$0
$96
$213*
Maximum
$625
$660
$699
Note: total premium costs were unavailable for NY, PA, and GA. Benefit coverage levels varied across states and
plans significantly.
*Lowest cost plan does not include prescription drug coverage
Overall, this shows that the MA plans have the lowest premiums, the Medicare Supplement Plans are in
the middle, and the Coordination plans have the highest premiums. While it can be helpful to do this type
of summary comparison, costs do not necessarily reflect the richness of benefits for each plan. Benefit
coverage levels vary significantly, and premium costs are influenced by a multitude of factors including
23
Among all large firms offering health benefits to current workers, only 13 percent offer retiree health
benefits to Medicare-age retirees. Section 11: Retiree Health Benefits – 10020 | KFF

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 54
federal subsidies, relative cost of health care, negotiated allowed amounts, population demographics, and
more.
States with coordination plans
Twelve states have at least one plan that coordinates benefits with Medicare through Coordination of
Benefits (COB), Maintenance of Benefits (MOB), or carve-out provisions: Alaska, Florida, Iowa, Maryland,
Mississippi, Montana, New York, North Carolina, Vermont, Virginia, Washington, and Wyoming. All these
plans are self-insured. Only six states have COB plans as defined earlier in this report: Florida, Mississippi,
Montana, Virginia, Washington, and Wyoming.
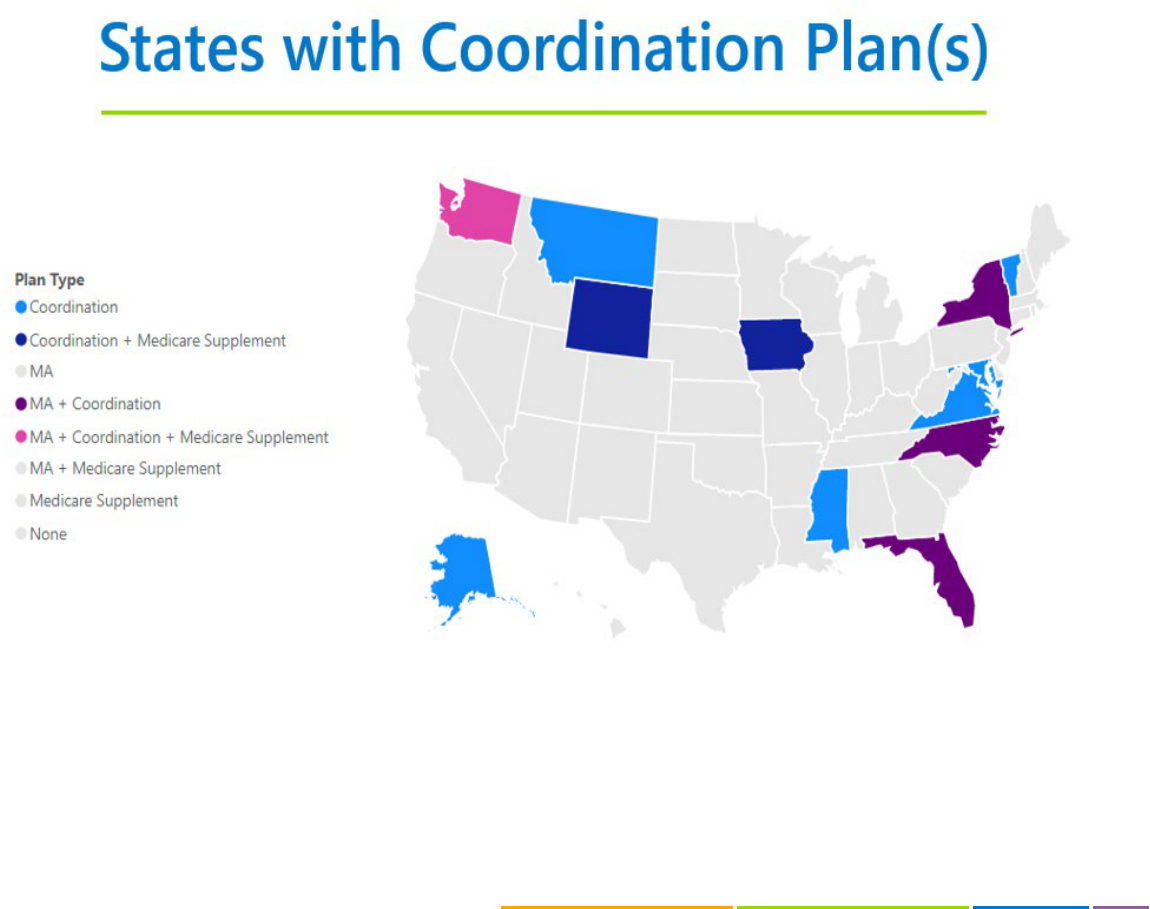
PEBB Retiree Medicare Benefits
December 1, 2023
Page | 55
Figure 9: States with Coordination Plans

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 56
An exact comparison of benefits provided by the COB plans in these states presents a challenge because
of the many differences in COB provisions and how the plans are administered. For example, the COB
savings bank is a unique feature of UMP that typically results in a full reimbursement of the UMP
deductible and zero out-of-pocket costs. This is not reflected in the plan benefit design. Pharmacy is
another area where benefits are difficult to compare because of the different tier structures and cost-
shares. The following chart shows the 2023 total premiums for the six states that offer Medicare COB
plans, broken down by retiree premium in lighter blue and state contribution in darker blue, where
applicable. Only Washington and Wyoming have state contributions toward premiums.
Chart 20: 2023 COB premium comparison
Total monthly premiums for these COB plans range from the lowest at $213 (Mississippi) to the highest at
$699 (Wyoming). The state with the lowest premium (Mississippi) does not include prescription drug
coverage, and the state with the highest premium (Wyoming) has significantly higher deductibles than
UMP Classic Medicare. Of the three states with COB plan premiums that are lower than UMP, Florida’s
plan is a high-deductible plan without vision or hearing coverage, Mississippi offers a plan with no
pharmacy coverage, and Virginia’s COB plan has Part D drug coverage but does not cover routine vision
or hardware.
24
24
Virginia’s COB plan “Advantage 65 PPO”, is not an MA plan. It is a self-insured COB plan and although
the name of the plan is “Advantage 65” it is not a Medicare Advantage plan.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 57
Table 9: COB benefits comparison
In summary, HCA conducted an analysis of state government self-insured plans across all fifty states and
found that there is wide variability in retiree health coverage. Most states offer at least one health plan for
retirees who are enrolled in Medicare. Washington is the only state that offers all plan types and is one of
only six states that has a COB plan. There is a broad range of cost-shares and supplemental benefits
across state plans. Compared to other states with COB plans, UMP has more comprehensive benefits and
this contributes to a higher premium. About two thirds of states subsidize retiree premiums, but only two
of the six states that have COB plans provide any subsidy, Washington being one of these states. In short,
this study found that there are no other states offering self-insured plans with benefits that are equal to
or richer, and with more affordable premiums, than UMP Classic Medicare. Those that have lower
premiums than UMP Classic Medicare either have benefits that are not as comprehensive as UMP, or they
do not provide a subsidy. In the next section of this report, HCA will explore several options that, if
adopted, could potentially reduce UMP Classic Medicare premiums going forward.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 58
Options and considerations to reduce UMP Medicare premiums
HCA, with help from Milliman, analyzed several options to reduce UMP Classic Medicare premiums while
retaining the program’s self-insured status and coordination with Original Medicare. Some of these
options result in a reduction in benefit coverage levels, such as through increased member cost-sharing at
the aggregate level or changes to prescription drug formulary and tiers. Others represent changes to how
certain benefits are administered but could be actuarially equivalent to current UMP Classic Medicare
coverage. The options have been organized by changes to pharmacy benefits versus medical benefits,
although they could be combined for greater retiree premium savings.
The results of Milliman’s analyses, summarized below and available in full in Appendices 5 and 8, are
projections based on a set of assumptions outlined in their reports and subject to change according to
actual experience and federal law or guidance. HCA’s annual procurement cycle and rate setting which
takes place each spring, and projected premiums as contained in this report, or its attachments, should
not be relied upon for future budgets or rate setting periods.
Changes to pharmacy coverage
Option 1: Changes to UMP Classic Medicare pharmacy benefit design
Following the 2023 premium increase for UMP Classic Medicare, HCA received stakeholder feedback
regarding the need to reduce retiree premiums. Much of this feedback included suggestions for changing
the pharmacy benefit, which contributes to more than 60 percent of plan costs. HCA worked with
Milliman to analyze the impact of different pharmacy benefit design scenarios on total pharmacy costs
and retiree out-of-pocket cost (prescription cost-share). This analysis was presented to the PEB Board on
March 9, 2023. The full report is available in Appendix 8.
For this analysis, Milliman modeled what each member’s cost-sharing and plan paid amounts would have
been under each scenario based on actual 2019 through 2021 spending and utilization. These modeled
amounts were compared with actual spending for this period to estimate the total claims savings. The
results indicate there are potential pharmacy claims savings, or plan savings, for UMP Classic Medicare
under alternative pharmacy benefit designs that could result in lower monthly premiums. However, these
savings are generated by increased out-of-pocket costs for most members when they fill prescriptions at
the pharmacy.
The benefit design scenarios were variations on the following:
• Change from member paid coinsurance, which is a percentage of the allowed cost of the drug, to
a predictable copay amount.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 59
• Increase the pharmacy maximum out-of-pocket limit; currently set at $2,000 for a single
subscriber.
25
• Create a separate coverage tier for high-cost specialty drugs.
It is important to note that because the study was based on historical data, findings do not account for
future changes to enrollment, the drug formulary, member behavior and health status, drug prices and
the practice patterns of medical providers and drug suppliers.
Co-insurance to copay
These scenarios tested the impact of moving from a co-insurance payment to a defined copay. Currently,
in UMP Classic Medicare, members pay 5% of the allowed cost of prescriptions up to a cap of $10 for the
Value Tier. Tier 1 is 10% up to a cap of $25, and Tier 2 is 30% up to a cap of $75. The maximum that
members pay out of pocket is $2,000 per member up to $4,000 maximum for a family of two or more.
Under a different benefit structure, members would instead pay a copay, and for the Value Tier they
would pay up to $5 (if the prescription cost is less than $5, they would pay the actual price). Tier 1 would
have up to $10 copay and Tier 2 would have up to a $75 copay. Specialty drugs would be covered under
Tiers 1 or 2 as they are today.
Table 10: Scenario 1-Co-insurance to copay
Total pharmacy claims impact:
Cost vs. current, as shown in the last line in Table 10 above, represents the estimated average difference in
paid claims between the current UMP Classic Medicare pharmacy benefit and the modeled scenario for
claims incurred from 2019 – 2021. In other words, this is what the plan actually paid for pharmacy claims
versus what the plan would have paid for the same claims under the modeled benefit design. The
modeled copay benefit design resulted in about a 3.3% reduction in pharmacy claims spending for this
historical period. Milliman also modeled the same copay structure with higher maximum out-of-pocket
(MOOP) amounts of $3,000 and $4,000. The $3,000 limit resulted in an additional 0.1% in estimated claims
25
Note: The Inflation Reduction Act includes a yearly cap ($2,000 in 2025) on out-of-pocket prescription
drugs in Medicare. HCA has not yet received guidance on whether this would apply to creditable coverage
plans, such as UMP.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 60
savings, or 3.4% total. There was no additional incremental savings to premiums from increasing the
MOOP to $4,000.
Retiree cost-share impact:
In aggregate, more than 95% of members would have paid on average about $122 more per year in
prescription drug cost-share under a copay benefit design compared to the current coinsurance structure.
Only about 1.8% of members would have paid, on average, about $30 less out-of-pocket, and about 3%
would have had no change in their out-of-pocket pharmacy costs. This scenario was estimated to result in
a monthly premium savings of around $11.
Table 11: Scenario 1a – Annual member cost-share impacts
Specialty Tier
Total pharmacy claims impact
The second set of scenarios analyzed the impact of creating a separate tier for high-cost specialty drugs.
These scenarios resulted in minimal plan savings. The estimated average difference in paid claims
between the current benefit and the modeled scenarios ranged from -0.1% for a Specialty Tier with a $100
maximum copay to -0.5% for a Specialty Tier with a $300 maximum copay.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 61
Table 12: Scenario 2 - Specialty Tier
Retiree cost-share impact
For the period analyzed, HCA found that most members, on average, would not have experienced a
difference in their out-of-pocket prescription drug costs under these Specialty Tier scenarios. Almost 98%
of members would have averaged the same amount of out-of-pocket costs for the year on covered
prescription drugs. This is because most members do not use drugs that would fall into the new Specialty
Tier. However approximately 2% of members who do use specialty drugs would have paid more. Under
Scenario 2a, which caps the member’s cost-share at $100 for the Specialty Tier, these members would
have paid about $200 more per year. Under Scenario 2b, which caps the member’s cost-share at $300, this
same group of members would have paid about $860 more per year for their specialty prescriptions.
Table 13: Scenario 2 – Annual member cost-share impacts
Copay plus Specialty Tier
This scenario is a hybrid of the copay and Specialty Tier scenarios described above. It shifts the Value Tier,
Tier 1, and Tier 2 from coinsurance to a set copay and creates a separate tier for high-cost specialty drugs.
It also models the impact of a Specialty Tier cap of $100 vs. $300. Under these scenarios, HCA found that
the potential claims savings are slightly higher than the switch to copays alone. This is because both
changes shift more cost to members who use the prescription drug benefit. The estimated average
difference in paid claims between these modeled scenarios and actual claims for 2019 – 2021 is -3.4% for
Scenario 3a and -3.7% for Scenario 3b, outlined in Table 14. The scenarios described here do not include a
change to the pharmacy MOOP, but additional details are available in Milliman’s report in the appendices.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 62
Table 14: Scenario 3 – Copay + Specialty Tier
At the population level, under Scenario 3 95% of members would have paid between $125 and $40 more
on average per year. This is very similar to Scenario 1 but claims savings and member out-of-pocket costs
are slightly higher.
Table 15: Scenario 3 – Annual member cost-share impacts
Summary of Option 1 findings
While there are potential cost savings for UMP Classic Medicare under different pharmacy benefit designs,
all the scenarios in this study showed an increase to out-of-pocket pharmacy costs to members. The
estimated potential premium savings under Scenario 1 could have been as much as $11 per month. But,
since most members would spend on average $122 more per year on their prescription drugs under this
benefit design, the potential reduction in premiums would be offset by greater out-of-pocket spending.
Option 2: Transition UMP Classic Medicare pharmacy coverage to Part D Self-funded
EGWP
HCA also considered structural changes to the UMP Classic Medicare pharmacy benefit to address high
pharmacy costs; specifically, converting coverage to Medicare Part D through an Employer Group Waiver
Plan. As mentioned earlier, Part D plans receive subsidies and discounts that are not available to plans
with creditable drug coverage, which results in significantly lower premiums. EGWPs are exclusively
offered to retirees under a group policy, may be self-funded or fully-insured, and often have enhanced
benefits over individual Part D plans.
HCA worked with Milliman to analyze the potential retiree premium savings if the UMP Medicare
pharmacy benefit converted to a self-funded or fully-insured Part D EGWP (either with enhanced

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 63
coverage
26
or Defined Standard
27
coverage). This summary will only cover results for the self-funded
EGWP options. Details on the fully-insured costs can be found in the full report.
28
Self-funded EGWP
The study found that compared to current UMP Classic Medicare creditable drug coverage, converting the
pharmacy benefit to a self-funded EGWP (SF EGWP) could reduce prescription drug spending and
resulting retiree premiums significantly. The following table reflects projected UMP pharmacy spending
and retiree monthly premiums for 2025. All modeling assumes ongoing authorization and use of a state
explicit subsidy amount of $183 or 50% of premium, whichever is less.
Table 16: Projected 2025 UMP Classic Medicare total pharmacy costs and retiree
premiums (per adult unit per month, “PAUPM”),
status quo versus self-funded EGWP
As shown, UMP Classic Medicare could save up to one hundred and six million dollars in projected 2025
pharmacy spending, or approximately $243 off monthly retiree premiums, under a self-funded EGWP with
Defined Standard Part D coverage. These savings are driven by leaner pharmacy coverage (i.e., through
higher member cost-shares) and the Manufacturer Discount Program (MDP), federal reinsurance, and
direct subsidy for Part D plans. Under an enhanced EGWP with wrap coverage (like the current UMP
Classic Medicare pharmacy benefit) retirees could potentially save over $200 on their monthly premium.
The primary advantages and disadvantages of status quo versus an EGWP are discussed in Table 17.
26
Plan Sponsors may offer enhanced Part D coverage, typically lower member cost sharing and coverage
for over-the-counter drugs via a “wrap” benefit.
27
The standard Part D benefit defined by CMS, including deductible and cost-share amounts by coverage
phase.
28
Attached in Appendix 5
Status Quo
(Creditable Drug
Coverage)
SF EGWP
(Enhanced)
SF EGWP
(Standard)
Total Annual Rx Costs*
$223.7 $132.4 $118.0
Total Annual Rx (Savings)*
N/A $91.3 $105.7
Medical Claims + Administration
$286.61 $286.61 $286.61
Rx Claims + Administration
$514.57 $304.6 $271.5
Explicit Subsidy
$183 $183 $183
Retiree Monthly Premium
$618.18 $408.22 $375.06
Retiree Monthly Premium Costs/(Savings)
N/A ($209.96) ($243.12)
*in Millions

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 64
Table 17: Advantages and disadvantages of creditable drug coverage compared
with EGWP for UMP Classic Medicare
Option
Advantages
Disadvantages
Creditable drug coverage
(status quo)
•
Maintains current benefits.
• More formulary flexibility.
• Highest level of program
control within HCA.
•
Does not receive federal
subsidies and discounts for
Part D plans, resulting in
significantly higher premiums.
• Will require eventual increases
in the explicit subsidy to
continue receiving RDS.
Employer Group Waiver
Plan
•
Significantly lower premiums
compared to creditable drug
coverage, with the option to
customize benefits to retain
similar coverage to status
quo.
• Provides protection against
catastrophic (very high) drug
costs, as defined by CMS.
• Lowers administrative burden
in the long term after the
initial setup.
•
Introduces members to
disruption through changes to
the benefit design and
formulary.
• Can require education to help
members understand their
benefit.
• Some members may pay
more out-of-pocket for
prescriptions depending on
the plan’s formulary and cost-
shares.
• Subjects HCA to increased
regulatory uncertainty.
• Increases administrative costs.
• Additional resources will be
needed to implement and to
educate members about their
new benefits.
• Longer implementation
timeline. Transition would
need to begin in late 2023 to
early 2024 for an effective
date of January 2025.
Changes to medical coverage
Option 3: Changes to UMP’s Medicare coordination provisions
To explore all options for addressing UMP Classic Medicare premium affordability, HCA also elicited
analysis from Milliman on possible changes to the medical benefit that would retain the plan’s self-funded
status and coordination with Original Medicare. Specifically, these would be changes to the plan’s
Medicare coordination provisions that would lower premiums but shift more cost-sharing to members at
the point-of-service. UMP Classic Medicare’s covered benefits and visit limits would not change; however,

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 65
members would pay more for some or all medical services depending on how the plan coordinates
coverage when Medicare pays primary.
Table 20 describes these alternative medical benefit options and how they impact retirees’ out-of-pocket
costs.
Table 18: UMP Classic Medicare optional medical benefit changes
Status Quo
Eliminate COB
Savings Bank
Eliminate COB
Savings Bank,
Increase
Deductible
Maintenance
of Benefits
Carve-out
Deductible
$250, but
usually
reimbursed
with COB
Savings Bank
$250
$500
$250
$250
Medical out-
of-pocket
maximum
$2,000
$2,000
$2,250
$2,000
$2,000
Cost-sharing
$0 for
Medicare-
covered
services;
typically, $0
for
supplemental
benefits with
COB Savings
Bank
$0 for
Medicare-
covered
services; 15%
(or $15 copay)
for
supplemental
benefits
$0 for
Medicare-
covered
services; 15%
(or $15 copay)
for
supplemental
benefits
15% of the
difference
between the
Medicare
allowed amount
and Medicare
paid amount;
15% (or $15
copay) for
supplemental
benefits
15% of the
Medicare
allowed
amount; 15%
(or $15 copay)
for
supplemental
benefits
As shown below, based on 2025 projected costs these alternative medical coverage provisions could save
retirees approximately $27 to $104 in monthly premium compared to the status quo. These premium
savings are offset by increased cost-sharing at the aggregate level, and members who use more benefits
would incur greater out-of-pocket costs. Modeling did not assume any change to the pharmacy benefit or
explicit subsidy of $183 or 50% of the premium, whichever is less.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 66
Table 19: Projected 2025 UMP Classic Medicare retiree premium cost/(savings) per
adult unit per month (“PAUPM”), status quo versus medical coverage alternatives
Summary of pharmacy and coverage alternatives for UMP Classic Medicare
There are several pharmacy and medical coverage alternatives for UMP Classic Medicare that could result
in retiree monthly premium savings. The greatest savings would be gained from converting the UMP
Classic Medicare pharmacy benefit to a self-funded Part D EGWP, which would take advantage of federal
subsidies and drug discounts to reduce total plan spending and retiree premiums. Additionally, an
enhanced EGWP could be customized to offer similar pharmacy coverage to the status quo. This would
limit the impact to retirees’ out-of-pocket costs, although there would be some disruption due to
differences in how the pharmacy benefit would be administered under Part D. Premiums could also be
lowered by changing the UMP coordination provisions when Medicare pays primary. This would shift
retiree costs from premium to out-of-pocket spending (deductible and cost-share). Finally, the pharmacy
and medical options could be combined for even greater premium relief. Milliman’s full report provides
projected savings for each of these coverage combinations.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 67
Addressing feedback from the listening sessions
HCA is appreciative of the participation of the PEBB members as well as the Stakeholders Medicare
Coalition in providing feedback on the retiree experience and is in the process of developing
improvements in processes and communications materials to address the challenges and concerns of the
members. Below is a partial listing of these ongoing process improvement projects.
Table 20: PEBB Medicare Retiree Process Improvement Projects
Member Challenge
Response
Assistance in understanding plan
comparisons and plan selection
Changes to communications materials, improvements to
benefits fairs.
Additional time to work on enrollment
change (OE) forms
HCA is planning to have the Open Enrollment change form
available earlier in October so members can begin
completing it earlier.
Access to information
Benefits fairs are being restructured to allow for more time
for retirees to meet with plan representatives as well as
HCA representatives. More benefits fairs are being offered
compared to those offered in Fall 2022.
Retiree-specific information will be available in one location
on the website so members can quickly identify the issues
that are specific to them. Added Medicare FAQs and
Medicare Myth Busters documents to website as a
response to listening session feedback.
Tools for retirees
HCA is streamlining the Open Enrollment form to allow
members to only complete the relevant portions of the
form. The Open Enrollment form tutorial will be made more
accessible.
Assistance in enrolling or changing
plans
See benefits fairs improvements, one-on-one support.
HCA will be mailing to members a customized letter
showing what plans they currently have and providing a
premium comparison with other plans that are available.
Advocacy for subsidies to UMP
HCA has written a letter to this effect to the state
congressional delegation, available in the appendices to
this report. HCA leadership also met and discussed this
issue with the CMS Administrator in February 2023.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 68
Opportunities for one-on-one support
HCA is working on establishing a scheduling system for
members wanting one-on-one support at the HCA office.
HCA is also exploring the ability to do virtual appointments
(most likely via Zoom) and establishing a scheduling
system.
Better communication regarding
significant changes in benefits or
plans
Benefits 24/7 is a new online portal for PEBB subscribers,
including retirees. This will allow members, including
retirees, to provide their emails which will facilitate faster
and more widespread communication of benefits changes
or plan changes that will be of interest to members.
Changes in the readability of the retiree guide.
Ability to upload documents
Benefits 24/7 will allow members to upload documents
directly into the system and provide feedback regarding
whether HCA has received them. Members can already
provide documents electronically through the HCA Support
Portal.
Support for Secure Access Washington
sign-ups
Providing a toll-free number for members to reach out for
technical support help if needed.
Improved OE communications
See benefits fairs, Open Enrollment forms improvements
and tools for retirees.
Decreasing wait times for customer
service during open enrollment
HCA requested additional Medicare support positions in a
supplemental budget decision package
Additional opportunities to provide
direct feedback
HCA is planned a focus group of retirees to design the
Benefits 24/7 wizard tool prior to its go-live in 2024.
HCA will be offering listening sessions on an ongoing basis
after determining the best time of year in terms of the
balancing timely responsiveness to feedback with the
cyclical work of the Legislature, PEB Board, and agency.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 69
Conclusion
During the spring of 2023 HCA conducted a series of listening sessions with PEBB members to gather
feedback regarding their health plan needs. This feedback is included in summary form in this report. In
addition, HCA conducted a study to determine if there were other states with similar, but more affordable,
plan options and found none. Finally, HCA studied three potential changes to the current UMP pharmacy
and medical benefits to determine their likely impact on member premiums.
Summary of listening session feedback
From February 28 to May 31, 2023, HCA held 24 listening sessions and three public forums to gather
feedback from PEBB Medicare retirees about their current health plan options available through the PEBB
Program. One hundred and ninety-three retirees participated in the listening sessions and 17 retirees
participated in the Public Forums. Participants provided feedback on what they liked and didn’t like about
their current health plans and offered additional insights into challenges they encountered while selecting
health plans.
• Kaiser members felt that their coverage was good, and they said they liked their plan because of
the coordination and quality of care, and the low cost. They had concerns about provider
availability and the coverage and felt that appointment scheduling was challenging with long wait
times for appointments.
• Premera participants liked their plan overall, felt that the coverage and provider availability was
good, and the plan is low cost. They don’t particularly like the fact that they must purchase a
Medicare Part D drug plan. A number had switched recently from UMP and felt that given the
short time they had been on the plan, they felt it was okay.
• UHC members felt that the drug coverage was more costly than they expected due to the use of
a copay rather than coinsurance and were unhappy with the Optum administration. They liked the
low cost of the plan, and in general, said they liked their plan. They would like UHC to improve its
customer service, but felt the coverage was good and felt that the plan is okay, although their
experience with the plan is short. Participants had concerns about MA plans in general and felt
that UHC had too many communications. A number mentioned that they switched from UMP due
to cost.
• UMP members feel their plan is costly but want to keep it as an option. They feel that the
coverage is good, like the plan, and feel that UMP is worth the cost. They like the provider
availability but feel that UMP has an unfair disadvantage with the MA plans because it is unable to
receive the federal subsidies that they receive. They like the travel coverage but feel that the
overall cost of prescriptions is driving up the cost of the premiums.
Participants provided insights into their communications preferences, indicating that they would like HCA
to continue to use the existing methods including paper/mail, emails, website, videos, the HCA lobby, in-
person events (e.g., benefit fairs), and online events (webinars).
In addition, participants mentioned that they had concerns about MA plans, which they see as a move
toward the increased privatization of Medicare. They would like to have better communication, more
information to be able to compare the different plans and would like to have help during Open

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 70
Enrollment in selecting or changing plans. They appreciated that HCA and PEBB had negotiated better
plans than they could get on the individual market.
Finally, participants mentioned that they valued the listening sessions and being able to provide input to
HCA. They were not happy about the 2022 proposal to close UMP Classic Medicare and were glad that
their retiree associations were able to share information with them about it. They felt strongly about the
impact that healthcare has on their lives and would like to see members and HCA work together to
improve communications and improve the plans.
Summary of 50 state comparison of state-sponsored Health Benefits for Public Sector
Medicare Retirees
An analysis of other government self-insured plans with comparable but more affordable benefits found
great variability in employer sponsored supplementary Medicare coverage for state retirees. Few states
offer self-insured COB plans, and none have benefits equal to or richer than UMP Classic Medicare with
lower premiums. Washington is unique in that it is the only state offering every type of employer
sponsored Medicare plan identified in the analysis.
Recognizing that lower UMP premiums can only be attained through changes in the plan itself, HCA
studied several options that might serve to reduce retiree premiums while still maintaining the plan’s self-
insured status and coordination with Original Medicare. These are discussed below.
Summary of options and considerations to reduce UMP Classic Medicare premiums
HCA, with help from Milliman, analyzed several options to reduce UMP Classic Medicare premiums, while
retaining the program’s self-insured status and coordination with Original Medicare. These options
included changes to pharmacy benefits and/or medical benefits.
• Option 1: Pharmacy – changes in pharmacy benefit designs
While there are potential premium savings for UMP Classic Medicare under different pharmacy
benefit designs, all the scenarios in this study showed an increase in out-of-pocket pharmacy
costs to members. The potential premium savings that could have been achieved under Option 1
could have been as much as $11 per month. But, since most members would spend on average
$122 more per year on their prescription drugs under this benefit design, the potential reduction
in premiums would be offset by greater out-of-pocket spending.
• Option 2: Pharmacy – transition UMP Classic Medicare pharmacy coverage to Part D
The greatest premium savings to members, while maintaining a pharmacy benefit that could
potentially be like that of UMP, would be gained from converting the UMP Medicare pharmacy
benefit to a self-funded Part D EGWP. This option would take advantage of federal subsidies and
drug discounts to reduce total plan spending and retiree premiums compared to creditable drug
coverage.
Additionally, an EGWP could be “enhanced” to offer pharmacy coverage that is like that currently
offered through UMP Classic Medicare. This would limit changes to the drug formulary and cost-
sharing, although there would be some disruption due to differences in how the pharmacy
benefit would be administered under Part D.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 71
• Option 3: Medical – changes to UMP Classic Medicare’s coordination of benefits provisions
Retiree premiums could be lowered by changing the UMP coordination provisions when Medicare
pays primary. This would shift retiree costs from premium to out-of-pocket spending (deductible
and cost-share).
Finally, the pharmacy and medical options outlined in the Milliman report could be combined for
even greater premium relief. For example, changing the UMP coordination provisions to a carve
out with no COB Savings Bank, combined with a standard self-funded Part D EGWP, could result
in additional savings. Milliman’s full report provides projected savings for each of these coverage
combinations.

PEBB Retiree Medicare Benefits
December 1, 2023
Page | 72
Appendix
1. Medicare Subscribers by State
2. Medicare Listening Sessions Summary Notes
3. Milliman Report - Medicare Benefits 50 States
4. June 2023 - PEB Board Coordination of Benefits State Analysis
5. UMP Pharmacy Benefit Change Impact Analysis
6. Milliman Report - UMP Medicare Analysis
7. Congressional Delegation Letter - Medicare subsidies
8. Evolution of private plans in Medicare
9. PEB Board Proposed Resolution - UMP Medicare Closure
10. PEB Board Resolution - Postpone Closure of UMP
11. December 19, 2022 HCA and Coalition agreement
12. June 12, 2023 - PEB Board Benefit Cycle
13. Listening Sessions Guide
