
Michigan
Consumer Guide
to Health Insurance


Table of Contents
Employer Group Coverage .......................... 3
Individual Coverage ................................ 7
Costs for Individual Health Plans ................... 12
Types of Health Plans ............................. 16
Filing a Complaint With DIFS ....................... 19
Appealing a Decision Made by Your Health Insurer ... 20
Addional Resources .............................. 23
Glossary of Health Coverage and Medical Terms ... 23
Important Contact Informaon ................... 26

2 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
This guide provides consumers with health insurance basics to assist Michigan
residents in making informed decisions regarding their health coverage.
About DIFS
The mission of the Michigan Department of Insurance and Financial Services is to
ensure access to safe and secure insurance and nancial services fundamental for the
opportunity, security and success of Michigan residents, while fostering economic
growth and sustainability in both industries.
Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 3
Employer Group Coverage
The Employer Is the Policyholder
The employer is the master policyholder and the employees are cercate holders in an employer
group health plan. The master policyholder:
• Negoates the terms of the group policy with the health insurer.
• May reduce or change the plan’s benets.
• May increase the employees’ premium contribuon.
• Is permied to switch health insurers.
• May allow the employees to choose from more than one plan.
• Can stop providing coverage enrely.
Coverage and rates may change annually. The employee contribuon – what you pay – is
determined by your employer.
Employers with 50 or more employees are
required to provide health coverage to
employees and their dependents. Failure
to oer aordable coverage may subject
an employer to a tax penalty and allow
the employee to obtain a tax credit in the
Health Insurance Marketplace.
Employers with fewer than 50 employees
are not required to provide health
coverage. However, if they choose to oer
health coverage, they may be eligible for a
small business health care tax credit.
The Employer Is the Policyholder
The employer is the master policyholder and the employees are cercate holders in an employer
group health plan. The master policyholder:
• Negoates the terms of the group policy with the health insurer.
• May reduce or change the plan’s benets.
• May increase the employees’ premium contribuon.
• Is permied to switch health insurers.
• May allow the employees to choose from more than one plan.
• Can stop providing coverage enrely.
EMPLOYEE PREMIUMS

4 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Employer Group Coverage
Enrollment
Employees should be aware of the employer’s
group health coverage enrollment policies and
deadlines. Employers can require up to a 90-
day waing period before new employees are
eligible to enroll in coverage.
Employers have an annual open enrollment
period for employees to apply, change or
disenroll in coverage. Any benet changes or
premium adjustments in the group plan are
communicated to employees during the annual
open enrollment period.
Special enrollment periods (SEPs) are allowed
when certain life events occur (i.e., birth/
adopon, marriage/divorce). Check with the
employer’s human resources department for
more informaon about SEPs.
Benets of Employer Group
Health Plans
Employer group health plans typically oer:
• Limits on out-of-pocket maximums.
• No annual or lifeme dollar limits
on essenal health benets.
• Free prevenve services.
• Dependent coverage to age 26.
• Specic minimum benets required
by Michigan law.
Small Business Requirement
Employers with 50 or fewer employees are not
required to provide health coverage; however,
they are required to provide informaon about
the Marketplace to their employees, whether
they oer health coverage or not. If they oer
health coverage to their employees, they must
oer it to all eligible employees within 90 days of
their employment start date.
Small business employers can explore oering
health and/or dental insurance to their employees
through the Small Business Health Opons
Program (SHOP). An employer purchasing SHOP
coverage may be eligible for a small business
health care tax credit. To review plans and enroll
in coverage, contact an insurer or an insurance
agent licensed with DIFS and registered with
SHOP. SHOP health plans can be reviewed at
www.healthcare.gov/Small-Businesses or by
contacng the SHOP Call Center at 800-706-7893.
Wellness Plans
Employers may oer wellness plans to encourage
employee parcipaon in a healthy behavior,
maintenance or improvement program. If a health
insurer bases their health insurance rates on
tobacco use, they must oer a wellness program for
any group policy. For parcipaon in the wellness
plan, the insurer may provide the employees with:
• A rebate or reducon in premium.
• A reducon in co-payments,
co-insurance and deducbles.
• A combinaon of these incenves.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 5
A self-funded plan will not use
the term “insurance” in its
benet informaon package.
Instead, the word “plan” or
“summary plan descripon”
will be used.
Self-Funded Health Plans
If you work for a large employer or a
government agency, there is a good chance your
health plan is self-funded or self-insured. Self-
funded plans may work best for employers that
are large enough to oer substanal coverage
and pay expensive claims for medical services.
As long as claims are being paid, you may not
noce whether your employer has provided
coverage through a self-funded plan.
Employers may contract with insurance compa-
nies and third-party administrators to manage a
self-funded health plan.
DIFS does not have authority over employers
or self-funded plans. DIFS may, however, have
authority over the administrator of a self-funded
plan. Self-funded plans fall under the authority
of the United States Department of Labor’s
Employee Benet Security Administraon. They
can be reached at www.dol.gov/Agencies/EBSA
or 866-444-3272.
Losing Employer
Group Coverage
If you lose group health coverage through your
employer, you may have federal COBRA rights,
be eligible for Medicaid or the Healthy Michigan
Plan or be able to purchase health insurance
through a special enrollment period.
The following opons are available to those
losing employer group coverage:
• Temporarily connue the same group
health plan under COBRA. COBRA is
available to health plans of employers
with more than 20 employees.
• Purchase individual coverage through the
Health Insurance Marketplace, from a
licensed insurance agent or health insurer.
You can sll go to the Marketplace and
check to see if the rates oered there are
more suited for your needs even if your
employer has more than 20 employees.
You may be eligible for a subsidy.
• Enroll in another group health plan
you may be eligible for through a
new employer or a spouse’s plan.
• Purchase a short-term limited duraon plan
to bridge the gap between coverage during
a period of transion. See page 17 for more
informaon regarding short-term plans.
• Enroll in Medicare, Medicaid or the
Healthy Michigan Plan if you are eligible.

6 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Employer Group Coverage
The federal Health Insurance Portability and
Accountability Act (HIPAA) applies when you are
covered by an employer’s group health plan and
you move to a dierent employer also oering
health coverage.
If the new employer’s group health plan oers
dependent coverage, it must oer coverage to
your dependents who were covered under your
previous plan.
The new employer’s group health plan may cost
more and provide dierent coverage. If the new
employer health plan oers dependent cover-
age, it must have a special enrollment period
to add a dependent because of marriage, birth,
adopon or loss of other coverage. As with
individual health plans, group health plans may
not impose pre-exisng condion exclusions.
Employers with 20 or more employees must comply with COBRA, except health
plans sponsored by the federal government and some church-related organizaons.
Consolidated Omnibus
Reconciliaon Act (COBRA)
COBRA is a federal law that allows you the right
to connue employer group health coverage
on a temporary basis aer you, your spouse or
your parent leaves an employer with 20 or more
employees.
The employer must nofy the former employee
of their COBRA rights within 30 days aer
employment has ended. Once noed, the
former employee has 60 days to apply for
COBRA coverage and is responsible for paying
the enre premium, including any part the
employer paid, plus up to an addional 2% for
administrave expenses.
COBRA Coverage Is Available For:
• 18 months.
• 29 months if you became eligible for
Social Security disability during the
rst 60 days of COBRA coverage.
• 36 months if you were insured through
a spouse’s or parent’s employer and
the spouse or parent has become
eligible for Medicare, died, divorced or
separated or if the dependent child has
reached the age beyond eligibility.
COBRA is complicated! The employer’s human
resources oce should have a booklet explain-
ing the details. Addional quesons can be
addressed by the U.S. Department of Labor,
Employee Benets Security Administraon at
866-444-3272 or www.dol.gov/Agencies/EBSA.
Moving From One Employer
Group Plan to Another
Employer Group Plan

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 7
Individual Coverage
The monthly premium is the cost for your
health plan and depends on the following:
• The type of plan chosen.
• Your age.
• Where you live.
• The number of eligible dependents
covered under your plan.
• Tobacco use.
Premiums may increase each plan year to
reect the increasing cost of health care.
If you are a Michigan resident without access
to a group health plan and are ineligible for the
Healthy Michigan Plan, Medicaid or Medicare,
you may purchase an individual major medical
health plan through a licensed agent, directly
from a health insurer or through the Health
Insurance Marketplace (Marketplace).
You are the policyholder on an individual health
plan. The plan can cover you and your eligible
dependents and cannot deny coverage based
on pre-exisng condions.
The annual open enrollment period provides
an opportunity for you to enroll in an individual
health plan. Plans may be purchased outside of
open enrollment through a special enrollment
period under certain qualifying events.
To nd out which opons may be available to
you, call DIFS at 877-999-6442 or visit
www.michigan.gov/HICAP
Individual policies must include specic
minimum health care benets required by
Michigan and federal law. More informaon
regarding these requirements can be found at
www.michigan.gov/HICAP.
Open Enrollment
Required Benets
Premiums

8 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Healthy Michigan Plan
If you are uninsured and looking for coverage, you may be eligible for the Healthy
Michigan Plan. Individuals may be eligible for the Healthy Michigan Plan if they:
• Are age 19-64 years.
• Do not qualify for Medicaid.
• Are ineligible for or enrolled in Medicare.
• Are not pregnant when applying for the Healthy Michigan Plan.
• Earn up to 133% of the federal poverty level (adjusted annually).
• Are residents of Michigan.
Individual Coverage
Visit www.healthymichiganplan.org or call 855-789-5610 for more informaon.
Healthy Michigan Plan
If you are uninsured and looking for coverage, you may be eligible for the Healthy
Michigan Plan. Individuals may be eligible for the Healthy Michigan Plan if they:
• Are age 19-64 years.
• Do not qualify for Medicaid.
• Are ineligible for or enrolled in Medicare.
• Are not pregnant when applying for the Healthy Michigan Plan.
• Earn up to 133% of the federal poverty level (adjusted annually).
• Are residents of Michigan.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 9
Health Insurance
Marketplace
Health Insurance Marketplace (Marketplace)
is a federally operated insurance marketplace
where individuals and families can purchase
and compare health plans. The Marketplace is
primarily accessed at www.healthcare.gov or by
telephone at 800-318-2596.
An individual health plan may be purchased for
you and your family during the annual open
enrollment period with the Marketplace.
For informaon on how to purchase a health
plan outside of the Marketplace, please refer to
www.michigan.gov/HICAP.
CSRs allow you to save money when you
receive health care services. A health plan
with a CSR includes lower out-of-pocket costs,
such as a lower deducble, co-payment, co-
insurance and out-of-pocket maximum. To
qualify for a CSR, you must purchase a silver
level health plan on the Marketplace and
have a household income between 100%
to 250% of the federal poverty level. The
federal poverty level is adjusted annually.
• Advance premium tax credits
• Cost-sharing reducons
• Marketplace parcipaon
Advance Premium
Tax Credits (APTC)
An APTC is a federal tax credit that is used
to lower the monthly cost of a Marketplace
health plan. Eligibility for an APTC is
available for those with a household income
between 100% to 400% of the federal
poverty level. The federal poverty level is
adjusted annually. The Marketplace will
determine your eligibility for an APTC.
Cost-Sharing Reducons (CSR)When purchasing health coverage
through the Marketplace, it’s benecial
to understand the following:
Marketplace Parcipaon
Not all health insurers choose to parcipate in
the federal Marketplace. Prior to selling plans
on the Marketplace, an insurer’s qualied
health plan and rates must be cered
by DIFS and the federal government.

10 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Types of Qualied Health Plans
(QHP) on the Marketplace
QHPs are divided into ve metal levels. Each metal level represents how the cost for
health care services are split between you and the health plan.
The ve metal levels are: planum, gold, silver, bronze, and expanded bronze. Insurers
selling health plans on the Marketplace are not required to oer plans in every metal
level, or in all counes.
• Planum Level – These plans must cover 90% of expected health care costs
and you are nancially responsible for the remaining 10%.
• Gold Level – These plans must cover 80% of expected health care costs and
you are nancially responsible for the remaining 20%.
• Silver Level – These plans must cover 70% of expected health care costs and
you are nancially responsible for the remaining 30%.
• Bronze Level – These plans must cover 60% of expected health care costs and
you are nancially responsible for the remaining 40%.
• Expanded Bronze Level – These plans must cover between 56% and 62% of
expected health care costs.
If an expanded bronze plan covers and pays for at least one major
service, other than prevenve services, before the deducble or meets the
requirements to be a high deducble health plan, it must cover between 56%
and 65% of expected health care costs.
Qualied Health Plan (QHP): a health plan
that’s cered by the Health Insurance
Marketplace and DIFS. QHPs provide essenal
health benets, follow established limits on
cost-sharing (i.e., deducbles, co-payments,
and out-of-pocket maximum amounts), and
meet other requirements under the ACA.
Individual Coverage
Types of Qualied Health Plans
(QHP) on the Marketplace
QHPs are divided into ve metal levels. Each metal level represents how the cost for
health care services are split between you and the health plan.
The ve metal levels are: planum, gold, silver, bronze, and expanded bronze. Insurers
selling health plans on the Marketplace are not required to oer plans in every metal
level, or in all counes.
• Planum Level – These plans must cover 90% of expected health care costs
and you are nancially responsible for the remaining 10%.
• Gold Level – These plans must cover 80% of expected health care costs and
you are nancially responsible for the remaining 20%.
• Silver Level – These plans must cover 70% of expected health care costs and
you are nancially responsible for the remaining 30%.
• Bronze Level – These plans must cover 60% of expected health care costs and
you are nancially responsible for the remaining 40%.
• Expanded Bronze Level – These plans must cover between 56% and 62% of
expected health care costs.
If an expanded bronze plan covers and pays for at least one major
service, other than prevenve services, before the deducble or meets the
requirements to be a high deducble health plan, it must cover between 56%
and 65% of expected health care costs.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 11
Catastrophic Health Plans
In addion to the metal level plans described, catastrophic health plans are also
available on the Marketplace. However, these plans are available only to those
under age 30 or of any age who have received certain hardship exempons
through the Marketplace. Eligibility for a hardship exempon can be obtained
through www.healthcare.gov.
Catastrophic plans purchased through the Marketplace generally:
• Have lower premiums and higher deducbles.
• Cover three annual primary care visits prior to the deducble being met.
• Cover prevenve services at no cost.
• Are not eligible for federal tax credits.

12 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Costs for Individual Health Plans
There is more to shopping for health insurance
than just nding the lowest premium.
Considering your nancial status and family
needs, the boom line on your health insurance
may not be the monthly premium you pay.
A policy with a lower monthly premium may
seem like a beer deal, but a lower monthly
premium could mean you’ll have less coverage
– or that you’ll pay more out-of-pocket when
you need health care services.
Premiums for individual health plans on and
o the Marketplace are rated based on:
• Type of plan chosen
• Age
• Gender
• Geographic locaon
• Family size
• Tobacco use
Each year, DIFS publishes the names of the
insurers selling on the Marketplace, along with
their rates and changes in the rates. To view the
health plans available in your area and review
ancipated costs, visit www.michigan.gov/DIFS.
By compleng an applicaon through the
Marketplace, you can review plans and rates
available to you. Assistance signing up for a
Marketplace plan is available from navigators,
cered applicaon assisters and licensed
health insurance agents who have completed
training and registraon with the Marketplace.
Health insurance agents must also be licensed
with DIFS. These individuals cannot charge you
for their assistance. Visit localhelp.healthcare.
gov to nd assistance in your area. You may
also visit www.michigan.gov/DIFS to locate a
licensed agent.
DIFS’ role in the Health Insurance Marketplace
includes reviewing health plan rates and poli-
cies prior to the policies being available to sell
in the Marketplace.
Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 13
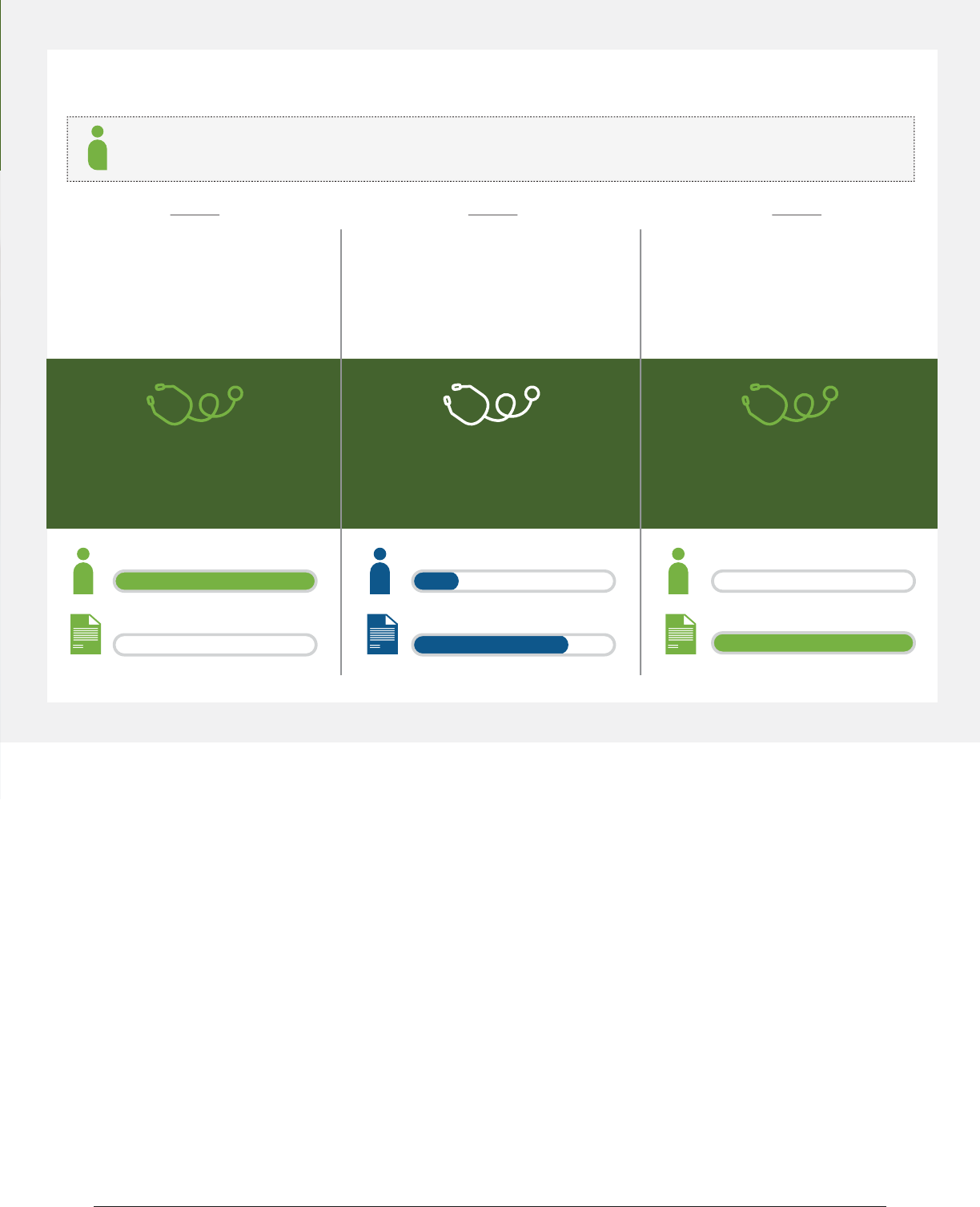
Example: How You and Your Insurer Share Costs Annually
Your Plan Deducble: $1,500 | Co-insurance: 20% | Out-of-Pocket Limit: $5,000
You have not reached your
$1,500 deducble yet.
Your plan does not pay
any of the costs.
You pay 100%
Your plan pays 0%
Office visit cost: $125
You pay: $125
Your plan pays: $0
You have reached your
$5,000 out-of-pocket limit.
You have seen the doctor oen and
paid $5,000 total. Your plan pays the
full cost of your covered health care
services for the rest of the year.
You pay 0%
Your plan pays 100%
Office visit cost: $200
You pay: $0
Your plan pays: $200
You have reached your $1,500
deducble; co-insurance begins.
You have seen a doctor several mes
and paid $1,500 total. Your plan pays
some of the costs of your next visit.
You pay 20%
Your plan pays 80%
Office visit cost: $75
You pay: 20% of $75 = $15
Your plan pays: 80% of $75 = $60
Plan year starng Jan. 1 and ending Dec. 31
1 2 3
What’s Covered
Health insurance helps pay for provider visits, hospital services and medicaons.
But remember, insurance isn’t just for when you get sick – it can also help you stay
healthy. Most plans cover prevenve services like immunizaons, annual visits,
screenings and more for free.
For more informaon on what your plan covers, review the “Summary of Benets
and Coverage.” If you don’t have one, ask your insurance company for a copy. The
Summary of Benets and Coverage explains the plan’s key features like:
• Covered health care services.
• Your share of the costs for a covered service.
• Health care services the plan does not cover.

14 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Costs for Coverage
Paying Medical Bills
Both the insured and insurer share the nancial
responsibility of health care services covered by a
health plan, otherwise known as cost-sharing. The
health plan explains exactly who pays for what.
It is the insured’s responsibility to understand
the benets of the health plan and how the plan
works. Contact the insurer’s customer service
department if there are quesons about the
plan’s benets. The insurer’s customer service
number can be located on the back of the
insurance card.
To beer understand the basics of health insur-
ance, review the following example of how an
insured would use their health plan:
• The insured person gives their insurance
card to the provider at the me
health care services are received.
• The co-payment is paid to the provider at
the me health care services are received.
• Usually, the provider submits a claim to
the health plan to receive payment for
the health care services. The insured
is responsible for subming the claim
if the provider doesn’t do it. This
typically occurs if services are received
from an out-of-network provider.
• The insurer sends an Explanaon of
Benets (EOB) to the insured if there
is a nancial responsibility for the
treatment received. The EOB lists the
date of service, the amount the provider
charged, the amount the insurer will
pay for the service(s) and your nancial
responsibility (deducble, co-payment,
co-insurance, non-covered benet).
The individual is responsible for their poron of
the bill when an invoice is received from the pro-
vider. It is important to keep a copy of the EOB
from the insurer to compare what the EOB says
you owe and what the provider is billing you.
Paying Medical Bills
Both the insured and insurer share the nancial
responsibility of health care services covered by a
health plan, otherwise known as cost-sharing. The
health plan explains exactly who pays for what.
It is the insured’s responsibility to understand
the benets of the health plan and how the plan
works. Contact the insurer’s customer service
department if there are quesons about the
plan’s benets. The insurer’s customer service
number can be located on the back of the
insurance card.
To beer understand the basics of health insur-
ance, review the following example of how an
insured would use their health plan:
• The insured person gives their insurance
card to the provider at the me
health care services are received.
• The co-payment is paid to the provider at
the me health care services are received.
• Usually, the provider submits a claim to
the health plan to receive payment for
the health care services. The insured
is responsible for subming the claim
if the provider doesn’t do it. This
typically occurs if services are received
from an out-of-network provider.
• The insurer sends an Explanaon of
Benets (EOB) to the insured if there
is a nancial responsibility for the
treatment received. The EOB lists the
date of service, the amount the provider
charged, the amount the insurer will
pay for the service(s) and your nancial
responsibility (deducble, co-payment,
co-insurance, non-covered benet).
The individual is responsible for their poron of
the bill when an invoice is received from the pro-
vider. It is important to keep a copy of the EOB
from the insurer to compare what the EOB says
you owe and what the provider is billing you.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 15
Specic quesons about coordinaon of benets may be directed to
DIFS at 877-999-6442.
Coordinaon of Benets (COB)
If you are covered by two or more
comprehensive health insurance policies, you
may be familiar with the term “coordinaon
of benets” (COB). Comprehensive health
insurance was designed to help cover the cost
of health care treatment; however, it was never
intended to pay more than 100% of that cost.
For this reason, COB rules were established to
address situaons where an individual has more
than one health plan and makes sure insurance
companies don’t duplicate or pay benets that
exceed 100% of the cost for treatment.
For policies issued In Michigan, the
COB Act of 1984 species how benets are
to be coordinated.
How Does COB Work?
The most common queson when two
or more comprehensive health insurance
policies are involved is “Who pays rst?” The
COB Act provides guidelines for the general
order by which the primary plan, the plan
that pays rst, and the secondary plan, the
plan that pays second, is determined.
The primary plan pays its share of the costs
rst, then the secondary plan pays up to
100% of the total cost of care. The plans
will not duplicate benets or pay more
than 100% of the cost for treatment.
It is important to note that COB rules for an
employee/subscriber/member dier from the
rules for dependent children.
The most common queson when two
or more comprehensive health insurance
policies are involved is “Who pays rst?” The
COB Act provides guidelines for the general
order by which the primary plan, the plan
that pays rst, and the secondary plan, the
plan that pays second, is determined.
The primary plan pays its share of the costs
rst, then the secondary plan pays up to
100% of the total cost of care. The plans
will not duplicate benets or pay more
than 100% of the cost for treatment.
It is important to note that COB rules for an
employee/subscriber/member dier from the
rules for dependent children.
How Does COB Work?

16 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Types of Health Plans
It is important to know the dierent types
of health plans to make the best use of your
benets and money.
Not all plans oer Minimum Essenal Coverage
(MEC), as dened under the Aordable Care
Act. MEC may be an individual or group health
plan, Medicaid, the Healthy Michigan Plan and
Medicare. The most common major medical
plans providing MEC are described below.
For more informaon related to MEC health
plans, visit www.healthcare.gov.
Health Plans
Minimum Essenal Coverage
• Health Maintenance Organizaon (HMO)
An HMO is a type of health plan that usually
limits coverage to their network of providers.
It generally won’t cover out-of-network care
except in an emergency. An HMO may require
you to live or work in the service area to be
eligible for coverage. All care is coordinated
through the member’s primary care physician
(PCP); therefore, you must designate a PCP.
• HMO Point-of-Service Plan
An HMO Point-of-Service plan oers in-network
and out-of-network benets. There may be
higher out-of-pocket costs for health care
services received outside the HMO’s network.
• Preferred Provider Organizaon (PPO)
A PPO is a contract between an insurer and
a network of providers agreeing to provide
health care services at a negoated rate. PPOs
may be less restricve than HMOs because
they do not require a referral to see other
providers. There are also out-of-network
benets with a higher nancial responsibility.
• Preferred Provider Arrangement (PPA)
A PPA is an oponal feature of a health plan.
The plan includes a network of parcipang
providers available to the insured to
obtain cost-eecve medical services.
• High Deducble Plans
These major medical plans are oen sold in
conjuncon with Health Savings Accounts.
They pay the cost of inpaent hospital
care and outpaent medical bills with high
deducbles. The nancial responsibility under
these plans changes annually and is paid from
a federally tax-exempt Health Savings Account.
Visit www.michigan.gov/HICAP for more infor-
maon on the annual limits under this plan.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 17
Health Plans
Limited Benets
• Short-Term Limited Duraon Plan
In Michigan, short-term limited duraon
plans are limited to a coverage period of
185 days out of any 365-day period. These
policies are not required to cover pre-exisng
condions, cannot be renewed or extended
for more than 185 days and do not sasfy
the requirement to have health insurance.
They also do not have to comply with
Aordable Care Act protecons, including
prohibions on annual or lifeme limits,
essenal health benets, protecons against
rescissions and cost-sharing limitaons.
• Limited Benet Plans
Limited benet plans provide reduced benets
intended to supplement comprehensive
health insurance, not to be an alternave
to them. These types of plans limit the
amount of coverage the company will
pay per episode of injury or illness.
» Accident Only
Accident only plans provide a cash
payment in the event of injury or death
resulng from a covered accident. For
example, the policy may pay a $200 benet
for each covered accident.
» Hospital Indemnity
Hospital indemnity plans pay a cash benet
in the event of hospitalizaon and/or surgery
resulng from a covered illness or injury. For
example, the policy may pay a $100 per-day
benet while the insured is hospitalized.
• Specied (Dread) Disease Plan
A specied disease plan provides benets
for specied causes of illness, disease or
injury, such as a heart aack, stroke or
cancer diagnosis. For example, the policy
may pay a $30,000 benet for an inial
cancer diagnosis while the policy is in force.
• Incidental Policies
Individual policies for dental and/or vision
benets pay for care not covered by typical
comprehensive health insurance and may be
available on a limited basis. Stand-alone dental
plans can be purchased through the Health
Insurance Marketplace during open enrollment
and o the Marketplace directly from an
insurer at any me throughout the year.

18 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Types of Health Plans
Health Plans
Medical Expense Reimbursement
• Health Savings Account (HSA)
HSAs are tax-exempt accounts set up by
an employer or individual to pay expenses
including deducbles, co-payments and other
out-of-pocket prescribed medical expenses.
An HSA must be established with a high
deducble health plan. The HSA is used to
pay roune expenses and the health plan is
used to pay more signicant expenses. HSAs
allow employers and consumers to set aside
funds on a tax-free basis to pay health care
expenses, including expenses that may not
be covered by tradional health coverage.
For example, HSAs may be used for vision and
dental services, prescripon drugs, over-the-
counter drugs (if you have a prescripon for
them), long-term care services and certain
health insurance premiums during rerement.
• Health Reimbursement Account (HRA)
HRAs are employer-funded group health
plans from which employees are reimbursed
tax-free for qualied medical expenses up
to a xed dollar amount per year. Unused
amounts may be rolled over to be used in
subsequent years. The employer funds and
owns the account. Health Reimbursement
Accounts are somemes called Health
Reimbursement Arrangements.
• Individual Coverage Health
Reimbursement Account (ICHRA)
Eecve January 1, 2020, employers can
begin oering employer funded ICHRAs as
an alternave to tradional group health
plan coverage. ICHRAs are arrangements
under which employees are reimbursed
tax-free for qualied medical care expenses
and premiums paid for individual health
insurance you’ve chosen, up to a certain
dollar amount for the plan year. Unused
funds can be rolled over to be used in
subsequent years. If you enroll in an ICHRA,
you must also be enrolled in an individual
health insurance plan purchased on or o the
Exchange, or Medicare (Part A and B, or C)
for each month you’re enrolled in the ICHRA.
• Excepted Benet Health
Reimbursement Account (EBHRA)
Eecve January 1, 2020, employers can
begin oering employer-funded EBHRAs
in conjuncon with a tradional group
health plan. The annual EBHRA employer
contribuon is limited to $1,800 (indexed for
inaon beginning in 2021). Employees may
enroll in the EBHRA even if they do not enroll
in the tradional group health plan or any
other coverage. EBHRAs are arrangements
under which employees are reimbursed
tax-free for qualied medical care expenses
and premiums paid for excepted benets,
such as dental and vision coverage, as well
as for short-term limited duraon insurance
(STDLI). EBHRAs cannot be used to reimburse
individual health insurance premiums, group
health plan premiums (other than COBRA),
or Medicare premiums. Unused funds can be
rolled over to be used in subsequent years.
For more informaon on HSAs and HRAs,
visit www.irs.gov.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 19
Filing a Complaint With DIFS
DIFS regulates the business of insurance
transacted in Michigan. Our authority pertains
to contracts issued in Michigan. DIFS accepts
complaints from pares involved in the contract,
such as the insured, policyholder or cercate
holder. Because a health care provider is usually
not a party to the health plan, DIFS generally
does not accept complaints from providers.
There are some excepons to this rule.
DIFS will pursue appropriate complaints from
providers acng as the authorized representave
of a paent; however, wrien authorizaon from
the paent or their legal representave must be
included with the complaint.
DIFS will accept complaints from providers
having problems with receiving timely
payment for submitted claims without any
errors or other issues. These claims are
referred to as “clean claims” and must be paid
within 45 days after they are received by the
health plan. For more information on clean
claims and to obtain the Clean Claim Report
form, visit www.michigan.gov/DIFS.
If you have a provider-related billing dispute,
these complaints can be submied to the
Michigan Aorney General Consumer Protecon
Division for review. The oce
can be reached toll-free at 877-765-8388 or
www.michigan.gov/AG.
You do not always need an aorney to resolve most
claim disputes with an insurer. Start with contacng
the insurer’s customer service department. Most
insurers have toll-free telephone numbers located
on the back of your insurance card.
If a sasfactory resoluon is not received, ask
about the insurer’s appeal process or le a
wrien complaint with the Michigan Department
of Insurance and Financial Services (DIFS).
DIFS will send the insurer a copy of the
complaint and ask them to explain its posion.
Insurers are required by law to respond to
DIFS. We will review the facts to ensure the
health insurer has complied with your contract
language and all rules and regulaons.
How to File a Complaint With DIFS
Complaints can be submied as follows:
• Online: www.michigan.gov/DIFScomplaints
• Email: DIFSc[email protected]
• Fax: 517-284-8837 or 517-284-8853
• Mail: The Department of Insurance
and Financial Services
Oce of Consumer Services
PO Box 30220
Lansing, MI 48909
• Contact DIFS toll-free at
877-999-6442 to request a complaint
form be sent to you via mail, email or fax.
Health Care Provider Complaints

20 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Michigan law provides you the right to le an
internal appeal if you disagree with your health
Appealing a Decision
Made by Your Health Insurer
Internal Grievance Process
If you disagree with a decision your health
insurer made regarding your health care claim,
you have the right to appeal the decision. There
are two levels of appeal – an internal appeal
with your health insurer and an external review
with the Department of Insurance and Financial
Services (DIFS).
The external review process should be
iniated only if:
1. The covered person has exhausted the
health carrier’s internal grievance process.
2. The health carrier fails to provide
a determinaon within the
meframe dictated by law.
Internal Appeal Process
insurer’s claim determinaon, also known as an
adverse determinaon.
An adverse determinaon means that an admis-
sion, availability of care, connued stay or other
health care service that is a covered benet has
been denied, reduced, or terminated. Failure
to respond in a mely manner to a request
for a claim determinaon is also an adverse
determinaon.
When you receive an adverse determinaon
noce, you must nofy your health insurer in
wring that you want to appeal its decision.
The adverse determinaon noce will provide
the meframe in which you are required to
submit your wrien appeal. Once you le an
appeal, the health insurer is required to com-
plete the internal grievance process within:
• 30 calendar days for a pre-service denial.
• 60 calendar days for a post-service denial.

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 21
You have the right to request an expedited
external review in situaons where the normal
PRIRA review meframe would seriously
jeopardize your life, health, or ability to regain
maximum funcon. An expedited external
review is conducted within 72 hours and
requires your treang physician to verify, orally
or in wring, the necessity of an expedited
review. You are not eligible for an expedited
external review if it concerns a health care
service that has already been received.
External Review Process
If you do not agree with the health insurer’s
nal adverse determinaon, you have 127 days
to le an external review under the Paent’s
Right to Independent Review Act (PRIRA).
To request an external review, you or your
authorized representave must complete the
Health Care Appeals-Request for External Review
form. In addion to the form, the external review
request should include a copy of the nal adverse
determinaon from your health insurer, the
reason(s) why you are appealing the decision and
any documentaon to support your posion.
If the external review concerns a denial based on
an experimental and/or invesgaonal service,
your treang provider must complete the
Treang Provider Cercaon for Experimental/
Invesgaonal Denials form and submit it with
your request.
For addional informaon related to DIFS’ external
review process and to access the required forms,
visit www.michigan.gov/DIFS or contact DIFS at
877-999-6442. Upon receipt, DIFS will examine
your external review request to determine if it
meets the requirements under PRIRA.
If your request is accepted and involves a
contractual dispute, the external review is
conducted by DIFS. If your request is accepted
and involves issues of medical necessity or
clinical review, it is referred for review to an
independent review organizaon. In both
instances, the Director of DIFS will issue an order
with the decision of the review.
Appointment of Authorized
Representave
Expedited External Review
You may authorize in wring any person, such
as a doctor, aorney, parent or spouse, to
represent you in the internal grievance process
and/or the PRIRA external review process.
In the PRIRA external review process, this
person is called an authorized representave.
The Health Care Appeals-Request for External
Review form provides space to authorize a
representave, who will be DIFS’ sole contact in
the PRIRA external review process.

22 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Appeal process is complete. If you or the health insurer disagrees with DIFS’ order,
an appeal can be filed in circuit court in Ingham County or the county in which you reside.
Send your appeal in
wring to health insurer
The health insurer agrees
to reverse its decision
Does your health insurer
have a second-level appeal?
File external review with DIFS
Director’s order is issued
The service or payment is
provided to you
Iniate second-level appeal
Do you sll disagree with the
health insurer’s decision?
The health insurer agrees
to reverse its decision
YES
YES
YES
Appeal Process Flow Chart
Receive adverse
determinaon
NO
NO
NO
!!!
22 • Michigan Consumer Guide to Health Insurance • michigan.gov/DIFS

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 23
This glossary has many commonly used terms but isn’t a full list. These glossary terms and denions are
intended to be educaonal and may be dierent from the terms and denions in your plan. Some of these
terms also might not have the same meaning when used in your policy or plan and, in any such case, the policy
or plan governs. (See your Summary of Benets and Coverage for informaon on how to get a copy of your
policy or plan documents.)
Allowed Amount
Maximum amount on which
payment is based for covered
health care services. This may
be called “eligible expense,”
“payment allowance” or
“negoated rate.” If your provider
charges more than the allowed
amount, you may have to pay the
dierence (see Balance Billing).
Appeal
A request for your health
insurer or plan to review a
decision or a grievance again.
Balance Billing
When a provider bills you for
charges not paid by your health
insurance because the charges are
higher than the allowed amount.
For example, if the provider's
charge is $100 and the allowed
amount is $70, the provider may
bill you the $30 dierence.
Co-Insurance
Your share of the costs of a
covered health care service,
calculated as a percent (for
example, 20%) of the allowed
amount for the service. You pay
co-insurance plus any deducbles
you owe. For example, if the
health insurance or plan’s allowed
amount for an oce visit is $100
and you’ve met your deducble,
your co-insurance payment of
20% would be $20. The health
insurance or plan pays the
rest of the allowed amount.
Complicaons of Pregnancy
Condions due to pregnancy,
labor, and delivery that require
medical care to prevent serious
harm to the health of the
mother or the fetus. Morning
sickness and non-emergency
caesarean secon aren’t
complicaons of pregnancy.
Co-Payment
A xed amount (for example,
$15) you pay for a covered
health care service, usually when
you receive the service. The
amount can vary by the type of
covered health care service.
Deducble
The amount you owe for covered
health care services before
your health insurance or plan
begins to pay. For example,
if your deducble is $1,000,
your plan won’t pay anything
unl you’ve met your $1,000
deducble for covered health
care services. The deducble
may not apply to all services.
Durable Medical
Equipment (DME)
Equipment and supplies ordered
by a health care provider
for everyday or extended
use. Coverage for DME may
include oxygen equipment,
wheelchairs, crutches or blood
tesng strips for diabecs.
Emergency Medical Condion
An illness, injury, symptom,
or condion so serious
that a reasonable person
would seek care right away
to avoid severe harm.
Emergency Medical
Transportaon
Ambulance service for an
emergency medical condion.
Emergency Room Care
Treatment you receive in
an emergency room.
Emergency Services
Evaluaon of an emergency
medical condion and
treatment to keep the condion
from geng worse.
Addional Resources
Glossary of Health Coverage
and Medical Terms

24 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Excluded Services
Health care services that
your health insurance or plan
doesn’t pay for or cover.
Grievance
A complaint that you communicate
to your health insurer or plan.
Habilitave Services
Health care services that help a
person keep, learn or improve skills
and funconing for daily living.
Examples include therapy for a child
who isn’t walking or talking at the
expected age. These services may
include physical and occupaonal
therapy, speech-language pathology
and other services for people with
disabilies in a variety of inpaent
and/or outpaent sengs.
Health Insurance
A contract that requires your
health insurer to pay some or
all of your health care costs in
exchange for a premium.
Home Health Care
Health care services a
person receives at home.
Hospice Services
Service to provide comfort
and support for persons in
the last stages of a terminal
illness and their families.
Hospitalizaon
Care in a hospital that requires
admission as an inpaent and
usually requires an overnight stay.
An overnight stay for observaon
could be outpaent care.
Hospital Outpaent Care
Treatment in a hospital that usually
doesn’t require an overnight stay.
In-Network Co-Insurance
The percent (for example, 20%)
you pay of the allowed amount
for covered health care services
to providers who contract
with your health insurance or
plan. In-network co-insurance
usually costs you less than out-
of-network co-insurance.
In-Network Co-Payment
A xed amount (for example,
$15) you pay for covered health
care services to providers
who contract with your health
insurance or plan. In-network
co-payments usually are less than
out-of-network co-payments.
Medically Necessary
Health care services or
supplies needed to prevent,
diagnose, or treat an illness,
injury, condion, disease or
its symptoms and that meet
accepted standards of medicine.
Network
The facilies, providers and
suppliers your health insurer
or plan has contracted with to
provide health care services.
Non-Preferred Provider
A provider who doesn’t have a
contract with your health insurer
or plan to provide services to
you. You’ll pay more to see a
non-preferred provider. [Check
your policy to see if you can
go to all providers who have
contracted with your health
insurance or plan or if your
health insurance or plan has a
“ered” network and you must
pay extra to see some providers.]
Out-of-Network Co-Insurance
The percent (for example, 40%)
you pay of the allowed amount
for covered health care services
to providers who do not contract
with your health insurance or
plan. Out-of-network co-insurance
usually costs you more than
in-network co-insurance.
Out-of-Network Co-Payment
The xed amount (for example,
$30) you pay for covered health
care services from providers who
do not contract with your health
insurance or plan. Out-of-network
co-payments usually are more
than in-network co-payments.
Out-of-Pocket Limit
The most you pay during a policy
period (usually a year) before your
health insurance or plan begins to
pay 100% of the allowed amount.
This limit never includes your
premium, balance-billed charges or
health care your health insurance
or plan doesn’t cover. Some health
insurance or plans don’t count all
of your co-payments, deducbles,
co-insurance payments, out-
of-network payments or other
expenses toward this limit.
Physician Services
Health care services a licensed
medical physician (M.D. – doctor
of medicine or D.O. – doctor
of osteopathic medicine)
provides or coordinates.
Plan
A benet your employer,
union or other group sponsor
provides to you to pay for
your health care services.
Addional Resources

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 25
Preauthorizaon
A decision by your health insurer
or plan that a health care service,
treatment plan, prescripon drug,
or durable medical equipment is
medically necessary. Somemes
called prior authorizaon, prior
approval, or precercaon.
Your health insurance or plan
may require preauthorizaon
for certain services before you
receive them, except in an
emergency. Preauthorizaon isn’t
a promise your health insurance
or plan will cover the cost.
Preferred Provider
A provider who has a contract
with your health insurer or
plan to provide services to
you at a discount. Check your
policy to see if you can see all
preferred providers or if your
health insurance or plan has a
“ered” network and you must
pay extra to see some providers.
Your health insurance or plan
may have preferred providers
who are also “parcipang”
providers. Parcipang providers
also contract with your health
insurer or plan, but the discount
may not be as great, and you
may have to pay more.
Premium
The amount that must be paid for
your health insurance or plan. You
and/or your employer usually pay
it monthly, quarterly or yearly.
Prescripon Drug Coverage
A health insurance benet
that helps pay for prescripon
drugs and medicaons.
Prescripon Drugs
A drug that by law requires
a medical prescripon.
Primary Care Physician
A physician (M.D. – doctor of
medicine or D.O. – doctor of
osteopathic medicine) who directly
provides or coordinates a range of
health care services for a paent.
Primary Care Provider
A physician (M.D. – doctor of
medicine or D.O. – doctor of
osteopathic medicine), nurse
praconer, clinical nurse
specialist or physician assistant,
as allowed under state law,
who provides, coordinates or
helps a paent access a range
of health care services.
Provider
A physician (M.D. – doctor of
medicine or D.O. – doctor of
osteopathic medicine), health care
professional or health care facility
licensed, cered or accredited
as required by state law.
Reconstrucve Surgery
Surgery and follow-up treatment
needed to correct or improve
a part of the body because
of birth defects, accidents,
injuries or medical condion.
Rehabilitaon Services
Health care services that help a
person keep, get back or improve
skills and funconing for daily
living that have been lost or
impaired because a person was
sick, hurt or disabled. These
services may include physical
and occupaonal therapy,
speech-language pathology
and psychiatric rehabilitaon
services in a variety of inpaent
and/or outpaent sengs.
Skilled Nursing Care
Services from licensed nurses
in your own home or in a
nursing home. Skilled care
services are from technicians
and therapists in your own
home or in a nursing home.
Specialist
A physician specialist focuses on
a specic area of medicine or a
group of paents to diagnose,
manage, prevent or treat certain
types of symptoms and condions.
A non-physician specialist is a
provider who has more training
in a specic area of health care.
UCR (Usual, Customary and
Reasonable)
The amount paid for a medical
service in a geographic area based
on what providers in the area
usually charge for the same or
similar medical service. The UCR
amount somemes is used to
determine the allowed amount.
Urgent Care
Treatment for an illness, injury
or condion that is serious
enough that a reasonable
person would seek care right
away but not so severe as to
require emergency room care.
Addional Resources

Updated Contact Information 6/2022
Important Contact Information
Michigan Department of Insurance and Financial
Services (DIFS)
• Michigan.gov/DIFS
• Phone: 877-999-6442
______________________________________
Health Insurance Marketplace
• Healthcare.gov
• Phone: 800-318-2596
______________________________________
SHOP Marketplace
The Small Business Health Options Program
(SHOP) Marketplace is a federally operated
insurance marketplace where small businesses
may shop for and compare group health coverage.
• Healthcare.gov/Small-Business
• Phone: 800-706-7893
______________________________________
Michigan Department of Health & Human
Services (MDHHS)
Apply for Michigan health care programs like
Medicaid, Healthy Michigan Plan and MiChild at:
• Michigan.gov/MiBridges
• Phone: 855-276-4627
• Michigan.gov/MDHHS
• Phone: 855-789-5610
• Michigan.gov/HealthyMiPlan
• Phone: 855-789-5610
Free Health Clinics
Free Clinics of Michigan (FCOM) is a network of
volunteer-staffed free clinics that provide health
care services to the uninsured or medically
underserved in Michigan.
• FCOMi.org
• Phone 248-635-8695
______________________________________
U.S. Department of Labor – Employee Benefits
Security Administration (USDOL)
The USDOL regulates self-funded health plans and
the Consolidated Omnibus Budget Reconciliation
Act (COBRA).
• DOL.gov/Agencies/EBSA
• Phone: 866-444-3272
______________________________________
Michigan Attorney General – Consumer
Protection
Handles complaints and answers questions
regarding provider billing issues.
• Michigan.gov/AG
• Phone: 877-765-8388

Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS • 27

28 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
Don’t Know Where to Turn?
Health Insurance Consumer Assistance Program (HICAP)
The Health Insurance Consumer Assistance Program is operated by the
Department of Insurance and Financial Services to help Michigan consumers with
health insurance issues
• www.michigan.gov/HICAP
• Telephone: 877-999-6442
Medicare
Medicare provides health insurance for people age 65 or older, some under age 65 with
disabilies, and those experiencing kidney failure.
• www.medicare.gov
• Telephone: 800-MEDICARE (800-633-4227)
Michigan Medicare/Medicaid Assistance Program (MMAP)
MMAP provides free educaon and personalized assistance to people with Medicare
and Medicaid, their families and caregivers.
• www.mmapinc.org
• Telephone: 800-803-7174
MMAP provides free educaon and personalized assistance to people with Medicare
and Medicaid, their families and caregivers.
• www.mmapinc.org
• Telephone: 800-803-7174


30 • Michigan Consumer Guide to Health Insurance • www.michigan.gov/DIFS
www.michigan.gov/DIFS
This Consumer Guide was created by the State of Michigan, Department of Insurance and
Financial Services (DIFS) and supported by Funding Opportunity Number
PR-PRP-18-001 from the U.S. Department of Health & Human Services, Centers for
Medicare & Medicaid Services. The contents provided are solely the responsibility of the
authors and do not necessarily represent the ocial views of HHS or any of its agencies.
