

Publishing Manager: Inta Izols
Development Editor: Karen Gilmour
Project Manager: Peggy Fagen
Design Manager: Mark Bernard
Design: Sheilah Barrett Design
CLINICAL AROMATHERAPY 2e ISBN 0-443-07236-1
Copyright 2003, Elsevier Science.
All rights reserved. No part of this publication may be reproduced in any form or by any means, elec-
tronic or mechanical, including photocopy, recording, or any information storage and retrieval system,
without permission of the publisher (Churchill Livingstone,The Curtis Center, Independence Square
West, Philadelphia, PA 19106).
Churchill Livingstone and the sailboat design are registered trademarks.
NOTICE
Complementary and alternative medicine is an ever-changing field. Standard safety precautions must
be followed, but as new research and clinical experience broaden our knowledge, change in treatment
and drug therapy may become necessary as appropriate. Readers are advised to check the most cur-
rent product information provided by the manufacturer of each drug to be administered to verify the
recommended dose, the method and duration of administration, and contraindications. It is the re-
sponsibility of the licensed prescriber, relying on experience and knowledge of the patient, to deter-
mine dosages and the best treatment for each individual patient. Neither the publisher nor the editors
assume any liability for any injury and/or damage to persons or property arising from this publication.
Library of Congress Cataloging in Publication Data
Buckle, Jane, RGN, MA, BPhil, Cert Ed, MISPA, MIScB.
Clinical aromatherapy / Jane Buckle.—2nd ed.
p. ; cm.
Rev. ed. of: Clinical aromatherapy in nursing / Jane Buckle. c1997.
Includes bibliographical references and index.
ISBN 0-443-07236-1
1. Aromatherapy. 2. Nursing. I. Buckle, Jane, RGN, MA, BPhil, Cert Ed, MISPA,
MIScB. Clinical aromatherapy. II. Title.
[DNLM: 1. Aromatherapy—methods. WB 925 B924ca 2003]
RM666.A68B83 2003
615⬘.321—dc21 2003043823
Printed in the United States of America.
Last digit is the print number: 9 8 7 6 5 4 3 2 1
CHURCHILL
LIVINGSTONE
An Imprint of Elsevier Science

This book is for all those who walk the path with me.
Thank you.

A
romatherapy is possibly the most simple of all complementary therapies
to integrate because when we inhale air, we inhale aroma, although we
are usually unaware of it. However, aromatherapy is rarely presented in a
cogent, scientific way; as a result, it has been difficult for physicians and nurses to
take the field seriously, or to understand how we could use it in our practice. Here
is a book from a health professional who writes about aromatherapy in a way that
we can understand and apply.
As a small boy growing up in Turkey, I had my own special paradise—my
grandfather’s walled garden—where I became aware of the power of the senses;
in particular, how the fragrance of plants made me feel good. Now, as a cardio-
vascular surgeon, I work on repairing the heart. I know the heart is perceived by
many to be more than a pump, the epicenter of emotion, and I continue to be
aware of how important our senses are to our well being, and how feeling good can
help recovery. The very smell of many hospitals is unpleasant, alien, or distressing
to our patients. Patients feel at their most vulnerable in a hospital’s high-tech sur-
roundings, so a familiar and comforting smell can do much to put them at their
ease. In common with several forward-thinking hospitals in the United States, we
now use aromatherapy at Columbia Presbyterian, and we have been working with
Jane Buckle on research since 1995.
Our sense of smell is located in the catacombs of the most primitive area of
the brain and is extremely powerful. Smell can produce all sorts of physical reac-
tions ranging from nausea to napping. The amygdala, the brain’s emotional cen-
ter, is located in the limbic system and is directly connected to the olfactory bulb.
Rage and fear are processed in the amygdala and both contribute to heart disease.
Our studies at Columbia have found that diluted essential oils rubbed on the feet
affected some volunteer’s autonomic nervous system within minutes.
Clinical Aromatherapy is presented logically, with considerable background
information given at the outset. I expect many readers will go straight to the clin-
ical section and look at their own specialty. In each specialty, a few symptoms or
problems have been explored, and the way in which aromatherapy might help
treat those symptoms or problems is clearly outlined. The information will be of
particular interest to readers working in that clinical specialty. However, I think
the book will also be of great interest to those who want to know what aro-
matherapy really is, and how it can be used in a scientific way.
Jane Buckle is well qualified to write this ground-breaking book. She brings
a wealth of knowledge and clinical experience acquired over 25 years in the field.
W
Foreword
vii

With a PhD in health service management, a background in critical care nursing,
a teaching degree and a fistful of degrees from the world of alternative medicine,
she writes authoritatively, and she speaks from the heart. Jane was a co-presenter
with me at The World Economic Forum in Davos, Switzerland, a few years ago.
We were invited to talk about the economics of alternative medicine and its im-
pact on globalization. I was impressed by Jane’s passion, as she also hosted four
different events that helped bridge the divide between big business, alternative
medicine, pharmaceutical organizations, and political leaders. An underlying
question permeated all her presentations: What can we do to get the caring back
into healthcare? When Jane speaks, people listen.
Jane Buckle is a pioneer and she uses writing, researching, and teaching to
get her message across. Her message is one of holism and she inspires those in
healthcare to evaluate how they use simple things like smell and touch to help
people heal. In the United States, many hospitals are beginning to integrate clin-
ical aromatherapy and use Jane’s program. She is involved in numerous hospital
research programs (apart from our own) and has been a reviewer for NIH grants.
Under her guidance, hundreds of students have carried out small pilot stud-
ies in American hospitals. She has written templates for aromatherapy policies
and protocols that are being used by hospitals. More than any other person, Jane
Buckle has labored to integrate clinical aromatherapy into hospitals, not as a pos-
sible add-on but as a legitimate part of holistic care. That achievement alone is
remarkable. But, she has another string to her bow. She has pioneered a registered
method of touch, called the “m” technique. This technique was tested in our lab-
oratory at Columbia Presbyterian on the legs of students and found to have a
pronounced parasympathetic response in some. The technique is very relaxing (I
have experienced it myself!) and eminently suitable for hospital patients (with or
without the use of essential oils), so I am delighted to see a section on the “m”
technique in this book.
Essential oils offer extraordinary potential from a purely medicinal stand-
point, and the recent studies on MRSA and human subjects show just how pow-
erful they can be. That an essential oil can be effective against resistant organisms
is medicine indeed and I think the chapter on infection will be of great interest
to pharmacists as well as those involved in infection control. When nausea is re-
lieved through the inhalation of peppermint and insomnia is alleviated through
the inhalation of lavender or rose, we are witnessing clinical results—not just the
“feel-good” factor. The studies on alopecia and topically applied essential oils, or
Candida albicans and teatree, show that aromatherapy can work at a clinically sig-
nificant level. However the strength of clinical aromatherapy is that it offers care
as well as, in some instances, cure. This is of particular relevance in the field of
chronic pain where the perception of pain can be altered using smell and touch.
The subject of clinical aromatherapy is vast and will be of interest to nurses
and physicians, chiropractors and massage therapists, pharmacists and natur-
opaths, pharmaceutical companies and herbalists. I share a goal with Jane
Buckle—to enhance patient care and give the best of what we have to offer, what-
viii Foreword

ever that may be. As a physician, I believe clinical aromatherapy has an important
role to play in integrative medicine. Jane Buckle gives us a glimpse of the future,
and it smells good!
Mehmet Oz
Mehmet Oz, MD, is a cardiac surgeon. He is the Director of the Cardiovascular Institute
and Vice Chairman of the Department of Surgery at Columbia Presbyterian
Medical Center, New York, NY.
Foreword ix

T
his book is intended for health professionals in the United States want-
ing to use aromatherapy in a clinical way to enhance their practice. It
draws from Clinical Aromatherapy in Nursing (London: Arnold, 1997) but
is a different book as it is no longer written from a nursing perspective and has
been substantially expanded to meet the needs of all health professionals. Things
have changed since 1997. I have gained a PhD (which helped my thinking!) and
much has improved in the aromatherapy world. Several clinical studies have ap-
peared in peer-reviewed medical journals. Aromatherapy is finding its way into
wellness clinics, hospices, and hospitals, and courses are being taught at leading
universities. Aromatherapy has become part of everyday language. Despite this,
popular misconceptions abound. This book was written to try to correct those
misconceptions and to indicate the important role that essential oils could play in
future healthcare.
The book is laid out in a similar way to the first book but with several im-
portant differences.
1. The book is no longer written from a nursing perspective, although there
is a section on aromatherapy as part of nursing care.
2. The text has been reviewed and edited by experts in the field (see Ac-
knowledgments).
3. The text includes many new tables to help the reader assimilate the in-
formation.
4. The chemistry section has been expanded and improved and includes
molecular drawings.
5. There are new sections on psychology, psychiatry, and aromatic medicine
(which covers internal use). There are specific sections for the physician,
massage therapist, chiropractor, and naturopath.
6. The individual clinical sections have been updated and expanded, espe-
cially the part on immunology.
7. The book is intended for U.S. residents and so OSHA and JCAHO re-
quirements are covered and education in the United States is addressed.
8. The number of references has almost doubled.
9. The reference system has been changed to make it easier to identify the
references in the text.
10. There is an extensive index.
W
Preface
xi

The book is divided into two broad sections. These are Overview and Clin-
ical Use. The overview begins with a background section, which covers such top-
ics as historical use, where essential oils come from, how they are obtained, what
they consist of, how they work, and how they are absorbed into the body. Then
there is a short introduction to the psychology of smell. This is immediately fol-
lowed by contraindications, toxicology, and safety issues. After this broad intro-
duction, the book begins to become more specific, with sections on how aro-
matherapy could be used by nurses, massage therapists, and physical therapists, or
as part of prescriptive medicine used by physicians, chiropractors, and natur-
opaths. A general hospital section follows, addressing how the generic problems
of infection, pain, insomnia, nausea, and stress could be relieved by essential oils.
Finally the clinical section is divided into departments found in a medical setting,
and there is a discussion of how aromatherapy could alleviate some of the com-
mon problems found in each clinical section with reference to published research,
my own clinical experience, and that of my students.
I am greatly indebted to the many physicians, nurses, and other profession-
als who edited and reviewed these sections. At the end of the book there are ap-
pendixes covering OSHA and JCAHO requirements, training and education in
the United States, and some recommended reading, websites, and essential oil
companies.
This book has been a labor of love. I hope you enjoy reading it as much as I
enjoyed the journey. If one piece of good research is carried out because of this
book, all the hours will be have been well spent.
Jane Buckle
xii Preface

I
would like to acknowledge the following people who edited specific parts of
the book. Thank you for your generosity of spirit and your nurturing editor-
ship.
Ann Adams, RN, CMN
Elizabeth Barrett, RN, PhD
James Duke, PhD
Charlotte Eliopoulos, RN, PhD
Ben Evans, MSN
Claire Everson, MSN
Debbie Freund, RN, LMT
Howard Freund, PhD
Ron Guba
Diana Guthrie, RN, PhD
Sue Hageness, MSN
Bob Harris
Rhi Harris, RN
Dorothy Larkin, RN, PhD
Michael McCrary, MA
Lee McGunnigle, DC
Lori Mitchell, RN, MSN
Gayle Newsham, RN, PhD
Tom Numark
Mary Poolos, RN, PhD
Ganson Purcell, MD
Scottie Purol-Hershey, RN, PhD
Linda Scaz RN, PhD
Kurt Schaubelt, PhD
Paul Schulick
Neal Schultz, MD
Keith Shawe, PhD
Kay Soltis, MSN
Brenda Talley, RN, PhD
Mark Warner, MD
Acknowledgements
xiii

e
section
I
Overview

Chapter 1 Introduction
Chapter 2 The Nature of Aromatherapy
Chapter 3 Basic Plant Taxonomy, Chemistry, Extraction, Biosynthesis, and
Analysis
3.1 Basic Plant Taxonomy and Chemistry
3.2 Extraction, Biosynthesis, and Analysis
Chapter 4 Toxicity and Contraindications
4.1 Essential Oil Toxicity
4.2 Contraindications
Chapter 5 Psychology
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice
Chapter 7 Oral and Internal Use of Aromatherapy
Chapter 8 Manual Therapies
Introduction to Section 1
Section I is an overview covering the foundations of aromatherapy. This section
opens with an examination not only of the history of aromatic medicine and the
emergence of a new, complementary therapy in the 1940s but also of the “what,
how, why, and when” aspects of essential oil production from plant to bottle. Next
is a two-part chapter on toxicity and contraindications (the “when and why not”
aspects of aromatherapy). Following this is a chapter on the psychology of smell.
The next part of Section I covers the use of aromatherapy within the context of
specific healthcare fields—nursing and manual therapies—including a discussion
of the oral and internal uses of essential oils.
The author is grateful for the input of many reviewers in this section whose
help and advice was most appreciated. The reviewers include: Tony Balazs PhD;
Elizabeth Barrett, RN, PhD; James Duke, PhD; Howard Freund, PhD; Ron
Guba; Bob Harris; Dorothy Larkin, RN, PhD; Lee McGunnigle, DCh; Gayle
Newsham, RN, PhD; Tom Numark; Mary Poolos, RN, PhD; Scottie Purol-
Hershey, RN, PhD; Brenda Talley, RN, PhD; Kurt Schaubelt, PhD; Keith
Shawe, PhD; and Neal Schultz, MD.

W
3
1
Introduction
The scent organ was playing a delightfully refreshing Herbal Capriccio—rippling
arpeggios of thyme and lavender, of rosemary, basil, myrtle, tarragon; a series of
daring modulations through the spice keys into ambergris; and a slow return
through sandalwood, camphor, cedar and new-mown hay.
Aldous Huxley
Brave New World
O
FALLthe complementary therapies, aromatherapy is perhaps the most
misunderstood. It is maligned, misrepresented, and can be very confus-
ing. Even the name aromatherapy is a misnomer. Contrary to popular be-
lief, aromatherapy is not just about smells! It is little wonder that orthodoxy
ridicules what the perfume industry guards so well.
Despite the misunderstanding, aromatherapy has become very popular in the
United States ( Jacknin 2001) and was even part of the millennium celebrations
in Times Square, New York. Two million celebrants were each given a 4
1
⁄
2
-inch
square scent strip that bore a global bouquet representing the aromatic choice of
every nation—the culmination of 10 years work by Gayil Nalls, a New York artist
who works in multimedia. Her work was endorsed by the United Nations Edu-
cational, Scientific and Cultural Organization (Kyle 2000). The United States
chose pine, England chose sweet grass, and France chose lavender.
Aromatherapy is the fastest growing of all complementary therapies (Buckle
2001). Although not mentioned in David Eisenberg’s groundbreaking 1993 study
on alternative medicine, aromatherapy was clearly in the picture just 5 years later
when it was being used by 5.6% of the study cohort (Eisenberg 1998). Aro-
matherapy is now an all-time favorite with UK nurses (Thompson 2001) and
is becoming popular among nurses in the United States. In a recent survey of

certified nurse-midwives in North Carolina, 32.9% had recommended aro-
matherapy (Allaire et al 2000).
There are currently 761,000 web sites on aromatherapy. This is hardly sur-
prising. As Larry Dossey, MD, states in his editorial on the impact of smell
(2001), “Throughout history people have responded to aromas.” Clinical aro-
matherapy has been described as the “most exciting of all complementary thera-
pies” by Andrew Weil, MD (personal communication). At the Nurse Practitioner
Associates for Continuing Education conference in 2001, Tieraona Low Dog,
MD, stated, “If you think herbal medicine is exciting, wait for clinical aro-
matherapy!” Mehmet Oz, MD, cardiothoracic surgeon at Columbia Presbyterian
Medical Center and pioneer of the first complementary medicine center in New
York city wrote, “Aromatherapy appears to impact perceptions of pain” (Oz 1998);
chronic pain is big business.
The effect of complementary therapies in general, and aromatherapy in par-
ticular, is economic. I was one of the speakers at the World Economic Forum in
Davos, Switzerland, in January 1999. The economics of herbal medicine (in
which clinical aromatherapy has its roots) is exciting and global. Americans spend
an astonishing amount of money on health care, approximately $4000 per person
in 1997. Americans and others in the Western world are growing tired of phar-
maceuticals as the “cure all” and are yearning for a more holistic approach that
would enable them to use more natural products. “People’s perception of the
chemical industry is belching chimneys, acrid smells and toxic waste products, not
an enticing prospect” (Brooks 2001). The recent Fen-Phen debacle, involving
hundreds of thousands of people whose heart valves were damaged by the drug,
is more evidence of a pharmaceutical industry that is accused of seeing itself above
federal regulation (Mundy 2001). The 44,000 to 98,000 deaths that occur each
year because of medical error (Pear 1999) also are encouraging people to try com-
plementary therapies, or at least to be wary of hospital visits.
Despite aromatherapy’s popularity, some important questions remain. What
is aromatherapy? Does it work? Is it safe? Where is the research? Many licensed
health professionals (LHPs) have been using aromatherapy in clinical settings
without really knowing exactly what they are using on their patients (Buckle
1992). There are few specialized training courses for LHPs who want to use clin-
ical aromatherapy to enhance the care they provide. Most training programs are
intended for the lay public. Some universities have begun to bridge the void, in-
troducing a more academic voice. A discussion on the different types of training
available appears in Appendix I.
Some critics of clinical aromatherapy have cited the paucity of research
(Vickers 1996). This is a fair criticism. Until recently, research has been limited
mainly to studies of animals or in-vitro systems. However, in the last 3 years
many pilot studies have been carried out and published, as a search on the Na-
tional Library of Medicine’s journal search engine, PubMed, indicates. Many of
the studies on human subjects have been carried out by nurses, many of whom
were not trained in research and had little or no funding. Often, the patient
4 Section I Overview

population was small and the study modest. However, these studies demonstrate
that aromatherapy is being used clinically in many hospitals throughout the
world. The results of these studies also indicate that aromatherapy is safe, effica-
cious, and, most importantly to managed care, less expensive than orthodox drug
therapy.
Perhaps orthodox medicine might be more open to the published research
available if they were to look hard at their own research. A Canadian study eval-
uated 4000 medical papers, applying 28 basic criteria that should be met in sci-
entific papers; the researchers concluded that only 40 of the 4000 papers met all
of the criteria. This analysis went on to state that only 15% of medical interven-
tions are supported by reliable scientific evidence, that most therapies applied
daily in doctors’ offices have never been tested by the scientific method, and that
these therapies are not supported by any evidence at all (Smith 1992). Peter
Gotzsche, a Danish statistician, chose for his thesis in 1990 the title “Bias in
Double-Blind Trials.” Gotzsche is director of the Cochrane Collaboration, which
reviews clinical studies; he made headlines in 2001 with his suggestion that mam-
mograms did not show evidence of reducing the number of deaths resulting from
cancer (McNeil 2002).
Although aromatherapy has been ridiculed by some, a growing group of
practitioners believe that aromatherapy has a valid place in integrative medicine.
Integrative medicine includes complementary and alternative medicine (CAM).
CAM has been around much longer than Western medicine (Buckle 1999a).
However, the growth in CAM’s popularity has precipitated a power struggle be-
tween the believers in Western medicine and the believers in CAM. Both appear
to be entrenched in their philosophies, but share the idea that if one is correct, the
other one is wrong.
Orthodox medicine may save lives, but it does have considerable drawbacks:
expense, serious side effects, and a considerable loss of life. Orthodox medicine
prides itself on being reductionist. It treats everyone more or less the same re-
gardless of age, sex, ethnicity, diet, stress level, or weight. Orthodox medicine talks
about the “average” patient and claims to be rigorously scientific. However,
some well-promoted procedures such as appendectomies and tonsillectomies
have, over time, proven to be of little value. Even bone-marrow transplants, the
much-lauded treatment of the 1990s, received a major setback in 1998. Results
presented at a world conference in Atlanta, Georgia, indicated that in four out of
five major trials there was no difference between the survival rate of patients re-
ceiving chemotherapy and patients receiving chemotherapy plus bone-marrow
transplantation (Kolata & Eichenwald 1999).
Some orthodox treatments are invasive and some can go badly wrong. In the
United States in 1998 there were between 44,000 and 80,000 deaths caused by
the misuse of pharmaceutical drugs. This exceeds the number of people killed in
car accidents (44,500), who died from breast cancer (42,300), or who died from
HIV/AIDS (16,500) (Pear 1999). Success in orthodox medicine is measured by
how quickly patients return to work. Few follow-up audits of orthodox treatment
Chapter 1 Introduction 5

have taken place, and if a patient “breaks down” again, it is classified as a new oc-
currence rather than as a reoccurrence.
The rationale behind CAM, including aromatherapy, is quite different.
These therapies are multidimensional and are not aimed at one specific body
system. They are not usually invasive. CAM therapists are interested in the in-
dividuality of the patients and what has led each patient to his or her particu-
lar disease process or set of symptoms (Hildebrand 1994). CAM therapists feel
that when the patient is balanced, homeostasis can return and the disease will
be unable to survive. They believe that the world is full of viruses and bacteria
but that it is mainly individuals whose immunity is compromised because
of emotional, spiritual, or physical trauma who tend to succumb to disease
(Gasgoigne 1993). Thirty years of orthodox research into cancer, with relatively
little progress toward an overall cure, support this viewpoint (Beardsley 1994).
Currently, 3% of the US population (9 million people) is living with the diag-
nosis of cancer (Okie 2001).
Success in CAM therapies is based on a long-term view. Practitioners look
at the “patterning” of the disease process: how often a patient has been ill during
his or her lifetime, and whether the incidence and severity of the disease has in-
creased. All diseases are taken into account, not just those of the same system. Pa-
tients are warned that treatment may take time. Emphasis is placed on teaching
the patient preventative medicine to avoid a relapse and on providing support
during the healing process. The patient is encouraged to rest, and not to work,
while the repairing process is in progress. The old-fashioned idea of convalescing
is stressed.
Is it possible for the two opposite positions to merge? Possibly. Certainly, the
term integrative medicine, coined by Andrew Weil, MD, conveys that vision. Per-
haps CAM is the yin of medicine and orthodoxy is the yang. Together yin and
yang make a circle, each needing the other to complete a whole. Yin is often per-
ceived as intuitive, feminine, spiritual, and artistic. Yang is often seen as mascu-
line, dominant, invasive, and scientific. Together, there could be a strong symbi-
otic partnership between orthodox medicine and CAM, each bringing out the
best in the other. Acute illnesses and trauma could be treated with Western drugs
or surgery, and chronic illnesses (e.g., arthritis, insomnia, and irritable bowel syn-
drome) could be helped with CAM.
So what is the place of clinical aromatherapy? Clinical aromatherapy can be
used to encourage healing and promote relaxation, but it can also help fight in-
fection and chronic illness. Clearly it has a role to play in integrative medicine.
Angela Avis (1999), chair of the Complementary Therapies Forum of the Royal
College of Nurses (the largest union in the world with approximately 330,000
members), suggests that an aromatherapist (normally a lay person) is not “an aro-
matherapist” when essential oils are being used clinically within the parameters of
a recognized license. In other words, aromatherapy is a tool used by LHPs, and,
as such, requires more specialized training than most lay practitioners receive.
6 Section I Overview

Approaches to aromatherapy can be herbal or chemical. Aromatherapy is
rooted in herbal medicine. Many orthodox medicines also are derived from
herbs, for example, aspirin, atropine, codeine, curare, digitalis, ephedrine, er-
gometrine, ipecacuanha, morphine, papaveretum, podophyllum, quinine,
senna, theophylline, and vinblastine (Hollman 1991). Even the contraceptive
pill was originally derived from a plant, the Mexican yam (Ryman 1991).
Herbalists are vitalists; they believe in the synergy of plants (i.e., the whole is
more than the sum of its parts), and they also understand that plants are adap-
togens (i.e., that their therapeutic effects are affected by the “terrain” of the pa-
tient). Chemists believe that the chemistry of a plant indicates its therapeutic
properties. A chemist is more likely to have a reductionist viewpoint similar to
orthodox medicine: Eradicate the symptom and the patient will be cured. An
herbalist might have a broader and more holistic approach to the patient,
stressing the patient’s background and intrinsic make-up. Both approaches
have validity.
In the United Kingdom, aromatherapy has been closely associated with mas-
sage. Perhaps this confusion arose because aromatherapy emerged in England via
the beauty therapy industry. However, aromatherapy has become sufficiently ac-
cepted as a therapy in its own right and the massage element has become less im-
portant. Certainly, applications of essential oils in massage have their place, partic-
ularly in stress reduction, but there are many other ways essential oils can be used
in health care. It is troubling that the only systematic review of aromatherapy ex-
amined 12 studies targeting relaxation and combining essential oils with massage
(Cooke & Ernst 2000). Double-blind, randomized studies of essential oils used
topically, through inhalation, or orally, instead of in conjunction with massage,
were ignored.
In France, aromatherapy is seen in a different light. Essential oils are often
diluted in vegetable oil and given orally in a gelatin capsule by a medical or herbal
doctor. The oral use of essential oils is often called aromatic medicine; it can be
an effective treatment for gastrointestinal complaints or to combat an acute or
chronic infection. Essential oils can also be given rectally or vaginally; the essen-
tial oils are absorbed through the “internal skin” of the body. Dermatologist Neal
Schultz (2002) suggests that there is a clear difference between the modus
operandi of essential oils that are ingested and those that are absorbed through
external or internal skin. However they are used—topically, through inhalation,
or orally—the use of essential oils goes back several thousand years.
Because often only one or two drops of essential oil are used, aromatherapy
is known for its gentleness and is important in stress management (Buckle 1999).
Aromatherapy can produce tremendous relaxation in a relatively short period
(Mathers 1991). Many nurses use aromatherapy to help their patients relax.
However, aromatherapy is not just about relaxing patients, improving their com-
fort level, or reducing pain. Essential oils can also help fight infection, also an ac-
ceptable nursing diagnosis (Carpenito 1993).
Chapter 1 Introduction 7

Essential oils are multitalented, and it is possible to use the same essential oil
for relaxation and for infection. This can pose a problem: Is the essential oil cure
or care? Florence Nightingale once said “the cure is in the caring” (Dossey 2000).
(Nightingale was adamant that patients should be removed from malodorous
odors.) During illness and following surgery relaxation can be a vital key to
recovery (Nightingale 1859), and the ability to relax can be greatly enhanced by
aromatherapy. By helping patients relax and feel better, they may actually get bet-
ter. Shames (1993) suggests that “we need to put more caring back into curing so
we can create a less costly, healthier system that will empower us all.”
This book is not intended to be a substitute for training. I believe strongly in
education, preferably in a hands-on class. There is a need for a clinical focus; the
“recreational” issues can be left to the perfumers and soap makers. Safety con-
cerns, as listed by the US Department of Labor Occupational Safety and Health
Administration, need to be addressed. Health professionals need to be aware of
the position on aromatherapy taken by the Joint Commission on Accreditation of
Healthcare Organizations ( JCAHO). JCAHO is in favor of complementary
therapies that have a positive effect on pain and improve patient care. Protocols
and policies need to be written. With these guidelines in place, aromatherapy can
enhance patient care and reduce costs. This last point is important in a health care
business desirous of a rapid, reliable turnover.
This book is about aromatherapy in clinical settings. It describes the use of
essential oils in health care: as part of nursing care and as an aid in massage and
physical therapy. It also covers the oral use of essential oils for physicians, nurse
practitioners, pharmacists, and chiropractors. The chapter on the psychology of
smell will be of interest to clinical psychologists, neurologists, behaviorists, and
psychiatrists.
REFERENCES
Allaire A, Moos M, Wells S. 2000. Complementary and alternative medicine in preg-
nancy: a survey of North Carolina certified nurse-midwives. Obstetrics and Gynecol-
ogy. 95(1) 19-23.
Avis A. 1999. When is an aromatherapist not an aromatherapist? Complementary Ther-
apies in Medicine. 79(2) 53-124.
Beardsley T. 1994. Trends in cancer epidemiology: a war not won. Scientific American
270, 130-138.
Brooks M. 2001. Turning chemistry green. Worldlink. Accessed April, 2002, from
http://www.worldlink.co.uk/stories/story.
Buckle J. 1992. Which lavender? Nursing Times. 88, 54-55.
Buckle J. 1999a. Aromatherapy in perianesthesia nursing. Journal of Perianesthesia Nurs-
ing. 14(6) 336-344.
Buckle J. 2001. The role of aromatherapy in nursing care. The Nursing Clinics of North
America. 36(1) 57-73.
Carpenito, LJ. 1993. Nursing Diagnosis, 3rd ed. Philadelphia: J.B. Lippincott.
8 Section I Overview

Cooke B, Ernst E. 2000. Aromatherapy: a systematic review. British Journal of General
Practice. 50: 493-496.
Dossey B. 2000. Florence Nightingale: Mystic, Visionary, Healer. Springhouse, PA:
Springhouse.
Dossey L. 2001. Surfing the odornet: exploring the role of smell in life and healing. Al-
ternative Therapies in Health and Medicine. 7(2) 12-15, 100-107.
Eisenberg DM, Davis RG, Ettner SL et al. 1998. Trends in alternative medicine use in
the United States; 1990-1997. Journal of the American Medical Association. 280,
1569-1575.
Gasgoigne S. 1993. Manual of Orthodox Medicine for Alternative Practitioners. Rich-
mond: Jigme Press.
Hildebrand S. 1994. Aromatherapy. In Wells, R. (ed.), Supportive Therapies in Health-
care. London: Baillière Tindall, 124-125.
Hollman A. 1991. Plants in Medicine for the Chelsea Physic Garden. London: Chelsea
Physic Garden.
Jacknin J. 2001. Aromatherapy. In Smart Medicine for Your Skin: A Comprehensive
Guide to Understanding Conventional and Alternative Therapies to Heal Common
Skin Problems. New York: Avery Penguin Putnam, 73-79.
King. J. 1994. The scientific status of aromatherapy. Perspectives in Biology and Medi-
cine. 37(3) 409-415.
Kolata G, Eichenwald K. 1999. Business thrives on unproven care, leaving science be-
hind. The New York Times, Oct 3, 664.
Kyle L. 2000. World sensorium. National Association for Holistic Aromatherapy Aro-
matherapy Journal. 10(3) 41-42.
Mathers P. 1991. Learning to cope with the stress of palliative care. In Penson J, Fraser
R. (eds.), Palliative Care for People with Cancer. London: Edward Arnold, 260-261.
McNeil D. 2002. Scientist at work: confronting cancer. The New York Times. Tuesday
April 9, 202. F7.
Mundy A. 2001. Dispensing with the Truth. New York: St. Martins Press.
Nightingale F. 1859. Notes on Nursing: What It Is and What It Is Not. London: Harri-
son & Sons.
Okie S. 2001. Report faults priorities of cancer care in the US. Albany, NY Times
Union. June 20th. A5.
Oz M. 1998. Healing from the Heart. Dutton: New York.
Pear R. 1999. Medical mistakes kills tens of thousands annually. Albany, NY Times
Union. Nov 30th. A1.
Ryman D. 1991. Aromatherapy. London: Piatkus.
Shames K. 1993. The Nightingale Conspiracy. Montclair, NJ: Enlightenment Press.
Schultz N. 2002. Personal communication.
Smith R. 1992. The ethics of ignorance. Journal of Medical Ethics. Reprinted in
Newsletter of People’s Medical Society 12, 4-51.
Thompson C. 2001. Oil on troubled waters. Nursing Times 97(15) 24-26.
Vickers A. 1996. Massage and aromatherapy: a guide for health professionals. London:
Chapman and Hall.
Weil A. 2001. Personal communication.
Chapter 1 Introduction 9

W
10
2
The Nature
of Aromatherapy
When, from a long-distant past nothing subsists, after the people are dead, after the
things are broken and scattered; taste and smell alone, more fragile but more
enduring, more insubstantial, more persistent, more faithful, remain poised a long
time, like souls, remembering, waiting, hoping, amid the ruins of all the rest; and
bear unflinchingly, in the tiny and almost impalpable drop of their essence, the vast
structure of recollection.
Marcel Proust
Remembrance of Things Past
The Nature of Aromatherapy
C
ontrary to popular opinion, aromatherapy is not just about smelling
things. The true definition of aromatherapy is much more specific: the use
of essential oils for therapeutic or medical purposes. However, the way in
which those essential oils are used is not specified. English aromatherapist Shirley
Price defines aromatherapy as “the use of essential oils, all of which are derived
from plants” (Price & Price 1999). American aromatherapist Jeanne Rose
classifies aromatherapy as “the healing of essential oils through the sense of smell
by inhalation, and through other application of these therapeutic volatile sub-
stances” (Rose 1992). An aromatherapy school in the United Kingdom defines
aromatherapy as “a natural treatment which uses the concentrated essential oils
from plants in association with massage, friction, inhalation, compresses and
baths” (Kusmerik 1992). French physician Valnet (1990) writes that aromather-
apy involves essences obtained from plants that are generally given “in the form
of drops, or capsules.”
There are four different types of aromatherapy: clinical, stress management,
beauty therapy, and environmental fragrancing (Gilt 1992). British aromatherapy

pioneer Robert Tisserand classifies them as psychotherapeutic, esthetic, holistic,
and nursing and medical aromatherapy (Tisserand 1993a).
Without doubt, “nice smells” added to a massage in a beauty salon are some-
thing akin to flowers on the table at a restaurant; they are not specific ingredients
of the meal, but they certainly enhance it. This is a form of esthetic aromather-
apy. Beauty therapists do not usually treat disease. However, at the other end of
the aromatherapy spectrum, medical aromatherapy suggests that specific medical
conditions can be treated with essential oils. French medical aromatherapists
Franchomme, Penoel, Gattefosse, and Belaiche have each written books dedi-
cated to this subject. These two types of aromatherapy—esthetic and medical—
are very distinct. The misunderstandings that arise often concern the types of aro-
matherapy that fall in between and what they entail.
Holistic aromatherapy suggests the therapist is involved with all parts of the
patient—in other words, with mind, body, and spirit. Holistic aromatherapy in-
volves “supporting” a patient; this is consistent with Tisserand’s diagrammatic
outlines. It is a procedure often carried out by body workers who may or may not
know much about the chemistry of the essential oils or the pathologic conditions
for which they are appropriate. These therapists are not “treating” the patient so
much as supporting other treatments the patient may be receiving, which can be
either orthodox or alternative.
Esthetic aromatherapy is about pleasure. Choosing a smell because it is
pleasing is similar to studying a beautiful picture. The picture is treasured for the
pleasure it gives, not for its intrinsic molecular structure. To put it another way,
the use of perfumes, scented bath soaps, and incense sticks are the use of esthetic
aromatherapy, and the world would be a sadder place without them. When pa-
tients are nearing the end of their lives, the focus is on keeping them comfortable,
not prolonging life. At that stage, esthetic aromatherapy can give both pleasure
and comfort.
Psychoaromatherapy concerns the ways smells or odors affect our brains by
influencing the production of endorphins and noradrenaline. Whether we realize
it or not, our entire life is affected by smell. All forms of aromatherapy have been
around for hundreds of years. They are definitely not “New Age.” Despite the ex-
plosion of products on the market that include the word aromatherapy on their la-
bels, the use of essential oils in products is not new. Only the use of their synthetic
copies is a recent development.
History of Aromatherapy: An Outline
Ancient History
The use of aromatic plants (and thus aromatherapy) was originally part of herbal
medicine. Herbal medicine dates back thousands of years and is not confined to
any one geographical area. Almost every part of the world has some history of the
use of aromatics in its health care system.
Chapter 2 The Nature of Aromatherapy 11

Iraq
Perhaps the earliest use of aromatics was discovered only recently. In 1975, dur-
ing investigation of an archaeologic dig in Iraq, concentrated extracts of yarrow,
knapweed, grape hyacinth, mallow, and other plants were found near a Nean-
derthal skeleton dating back 60,000 years (Erichsen-Brown 1979). Of the eight
species of herbs discovered there, seven are still being used today in medicine
(Griggs 1981). Yarrow is an aromatic herb that produces an essential oil often
used in aromatherapy.
France
One of the earliest records of plant medicine is in the form of paintings drawn on
the walls of caves in Lascaux, Dordogne, in southern France (Ryman 1991).
These drawings show the use of medicinal plants and date back to 18,000
BC.
Much later, in the thirteenth century, a medieval religious sect called the Cathars
lived in the area around Languedoc and Montaillou in southern France (Le Roy
Ladurie 1984). Vegetarian and deeply spiritual, their priests (called parfaits) were
also highly skilled in herbal and aromatic medicine. Regarded as heretics by the
Catholic Church, they were tortured and murdered during the Inquisition. One
night, more than 100 Cathar men, women, and children were tied to stakes and
burned alive (Guirdham 1990).
Mesopotamia
The Sumerians, who lived in Mesopotamia around 5500 BC, were sophisticated
herbalists. In their matriarchal society women were the healers. They were either
shamans called Ashipu or herbalists called Asu (Lawless 1994). They left as their
legacy clay tablets bearing prescriptions, names of plants, methods of preparation,
and dosages for their treatments (Erichsen-Brown 1979). Aromatic medicine fig-
ured strongly in this early culture, and pots have been found that could have been
used in plant distillation. In the Epic of Gilgamesh, a Sumerian poet writes, “There
is a plant whose thorns will prick your hand like a rose. If your hands reach that
plant you will become a young man again” (Swerdlow 2000).
Egypt
One of the most famous manuscripts listing aromatic medicines is the Egyptian
Papyrus Ebers manuscript, found near Thebes in 1872. This document, written
during the reign of Khufu (around 2800
BC), was followed by another document,
written about 2000
BC, that mentions “fine oils and choice perfumes.” These
manuscripts, written while the Great Pyramid was still being built, reveal that
during the time of Moses, frankincense, myrtle, galbanum, and eaglewood were
used as medicines to cure symptoms of disease. There is also mention of myrrh
being used to treat hay fever.
When Tutankhamun’s tomb was opened in 1922, the boy-king’s floral collars
were still faintly aromatic. Thirty-five alabaster jars of perfume were found in his
12 Section I Overview

burial chamber, but all of them were broken or empty. Many had contained frank-
incense and myrrh, highly valued commodities and likely the first items to be
stolen from the tomb (Steele 1991). The ancient Egyptians also used aromatics in
their embalming process. They removed most of the internal body parts and re-
placed them with fragrant preparations such as cedar and myrrh. In the seven-
teenth century some of these mummies were sold and distilled to be used in med-
icines themselves (Levabre 1990).
China
The earliest known text containing written instructions on how to use herbs as
medicines was written by the Chinese in approximately 2800
BC. The Great
Herbal (Pen Ts’ao) is believed to have been written by Shen Nung. In it he lists
some 350 plants, many of which are still being used today. One of them is the
herb Ephedra sinica, which was among those found in the Neanderthal grave in
Iraq. The Great Herbal dates back to around 2800
BC. Another emperor, Huang
Ti, sometimes called the Yellow Emperor, wrote the Huang Ti Nei Ching Su Wen.
The English translation is called The Yellow Emperor’s Classic of Internal Medicine
(Rose 1992a). Today, a huge concrete statue of ginseng presides over the state-run
herbal market in Anguo, China (3 hours south of Beijing), indicating how im-
portant herbal medicine remains. The Chinese method of soaking a cloth in herbs
and resting it on the skin indicates how the Chinese have always accepted the ef-
ficacy of transdermal delivery—something Western medicine denied for many
years. There is a great similarity between Ayurvedic and Chinese medicine, prob-
ably dating back to when India and China first traded. As early as 1000 BC, the
Chinese were exchanging herbs with India (Swerdlow 2000).
India
Vedic medicine (the precursor to Ayurvedic medicine) has at its core the Vedas,
a series of texts that refer to plants as “supreme, a remedy for need and a bless-
ing for the heart.” The first Sanskrit medical treatises, Caraka Samhita and
Sushrata Sambita, date back to 2000
BC and describe the use of 700 plants, many
of them aromatics such as ginger, coriander, myrrh, cinnamon, and sandalwood
(Swerdlow 2000). Ayurvedic medicine was pushed underground by the Muslim
invasion of India in the eleventh and twelfth centuries and later by the British
occupation. The British prohibited the funding of Ayurvedic colleges and clin-
ics. India fought back in 1921 with a document presented to the British gov-
ernment in Madras, India, stating that no Western scientist should think of
criticizing Ayurveda until he had learned the Sanskrit language (Swerdlow
2000).
In the last few decades Ayurveda has become popular again, in part because
of the influence of Deepak Chopra, MD (Chopra 1991). Preparing an Ayurvedic
medicine can take many days of following the Sanskrit instructions. Ayurveda
has a strong spiritual base, and in northern India, Ayurvedic physicians are known
as holy men. Traditional Indian shamans were known as perfumeros and were
Chapter 2 The Nature of Aromatherapy 13

healers who used the scents of aromatic plants (Steele 1991). Today, aromatics re-
main an important part of Ayurvedic medicine.
Tibet
Tibetan medicine is thought to date back to pre-Buddhist times and is based on
the Four Tantras of Tibetan Medicine, written in the eighth century. This is a
whole medical system and is similar to Chinese medicine in that it focuses on the
person (or the society in which the person lives), rather than the disease. Tibetan
medicine has traditionally used aromatic herbs, often as inhalations. These herbs
are usually prescribed in complex remedies such as Aquilaria A, which contains
aromatics including clove, cardamom, sandalwood, and myrrh (Lawless 1992).
Greece
Theophrastus was a pupil of Aristotle and inherited the botanical garden at
Athens that Aristotle had planted (Stearn 1998). In 300
BC, Theophrastus wrote
Enquiry into Plants, in which he described specific uses for aromatics. At that
time doctors who used aromatic unctions were called latralyptes. One aromatic
formula, called Kyphi, contained 16 different ingredients. Kyphi was used as an
antiseptic and an antidote to poison; it was soothing to the skin and would also
“lull one to sleep, allay anxiety and brighten dreams.” It was Theophrastus, later
called the “father of botany” (Ryman 1991), who discovered the perfume of jas-
mine was stronger at night. Hippocrates (who lived around 460
BC) is recognized
as the father of medicine. He wrote “aromatic baths are useful in the treatment
of female disorders, and would often be useful for the other conditions too”
(Chadwick & Mann 1983). He understood the principles of psychosomatic dis-
orders, and his was possibly the first statement on holism: “In order to cure
the human body it is necessary to have knowledge of the whole” (Lawless 1994).
Hippocrates also knew aromatics could have important antibacterial properties,
and when an epidemic of plague broke out he urged the people to use aromatic
plants to protect themselves and stop the spread of the disease. He also wrote,
“the growth of plants forms an excellent parallel to the study of medicine”
(Chadwick & Mann 1983).
Greek army doctors traveled with large supplies of herbal remedies, and, in a
manual written for the Emperor Claudius in 43
AD, detailed instructions were
given on how to recognize plants abroad and how to pick and pack them. Every-
one seemed to be using aromatic medicine in some form. Even audiences watch-
ing competitive sports in the stadium at Daphne were sprinkled with rose water
to keep up their spirits and urge on the games. Helen of Troy was famed for her
use of aromatics in mood-enhancing potions.
The legendary Greek Pedanios Dioskurides (often spelled Dioscorides) lived
around 100
AD and wrote the famous De Materia Medica. This foundation of
Western herbal medicine lists and illustrates some 700 plants that were in use at
the time (Holmes 1993). Included are aromatics such as basil, verbena, car-
damom, rose, rosemary, and garlic. Each section of De Materia Medica begins
14 Section I Overview

with a drawing and description of a plant and the contraindications are carefully
listed (Griggs 1981). Dioscorides suggests that one of them, tarragon (Artemesia
dracunculus) might be useful in four different treatments: for cancer, for gangrene,
to produce abortions, and as protection against viper bites. Tarragon was later
used by Native Americans during difficult labor and to induce menstruation. Na-
tive Americans believed tarragon was such an important herb it was classified a
“chief medicine,” requiring the collector to pull it (pick it) and not dig it up out
of respect for its power.
When Claudios Galenos (known in English as Galen) was appointed per-
sonal physician to Emperor Marcus (130-200
AD) he continued the use of fra-
grant oils and referred to the fragrance of narcissus as the “food of the soul.”
Galen also introduced a system for identifying plants (Griggs 1981). In his fa-
mous work Peri, he listed not only different herbs but different grades of herbs
like cinnamon (Holmes 1993). Unfortunately, many of the 500 works he com-
piled were destroyed when his clinic in Rome burned down. However the sys-
tem introduced in his largest work (which consisted of 11 books) survived. By
describing a disease process in terms of temperature and moisture, Galen laid the
cornerstone of modern physiology (Lawless 1994). He also described a plant’s
energetic profile, which is similar to both Chinese and Ayurvedic approaches.
This approach is continued today with contemporary writers (Holmes 1993;
Mojay 2000). During the immediate pre-Christian era, Jewish women spiked
wine with myrrh and frankincense, which have anesthetic effects, and gave it to
those being tortured. The early Christian era considered aromatics to be pagan
because they could heighten sensual pleasure. In 529
AD, Pope Gregory the
Great passed a law banning all Materia Medica. This was the first hiccup in the
history of aromatherapy. The school of philosophy at Athens closed down, and
the works of Galen and Hippocrates were smuggled to Syria. There the works of
Galen, Hippocrates, and Dioscorides were translated into Arabic by Hunayn ibn
Ishaq al’Ibadi who was paid for his efforts with an amount of gold equal to his
weight.
Arabia
In the prologue to The Canterbury Tales, Chaucer describes four Arabic physi-
cians. Arabic doctors were regarded as the greatest medical authorities in the
fourteenth century. One of Chaucer’s physicians is an historical figure known as
Ibn Sina—later called Avicenna (Tschanz 1997). Arabia added a whole host of
new aromatics such as senna, camphor, tamarind, nutmeg, and cloves to the list
of medicinal plants, and began to play an important part in the development of
herbal and aromatic medicine. Arabs suggested rose and orange-blossom water to
make medicines taste more palatable, and they were familiar with the anesthetic
effect of inhaled henbane. Arabic physicians also used topical sugar to staunch
bleeding. Sugar promotes new cell growth by drying the bed of the wound and
dehydrating the bacteria there. This practice is still used today by some physicians
(Swerdlow 2000).
Chapter 2 The Nature of Aromatherapy 15

By the third century AD, the city of Alexandria had become a center for med-
icine, continuing the Greek tradition of the science of aromatics. At the start of
the ninth century, the first private apothecary shops opened in Baghdad. Medi-
cines were manufactured and distributed commercially to physicians and phar-
macists who dispensed them to the public as pills, tinctures, suppositories, and in-
halants.
Abd Allah ibn Sina (980-1037) was born in what is now called Bukhara
(present-day Uzbekistan). His name was later westernized into Avicenna. Ibn
Sina was to the Arabic world what Aristotle was to the Greeks. He was a child
prodigy: a scholar who at the age of 10 could recite the entire Koran and who
went on to excel in medicine, poetry, math, physics, and philosophy. At the age of
20 ibn Sina was appointed court physician and during his life he wrote more than
20 medical texts including the Canon of Medicine, which remained a standard
medical textbook until the sixteenth century (Lawless 1994). The Canon lists 760
medicinal plants and the drugs that can be derived from them. Ibn Sina also laid
out the basic rules of clinical drug trials, principles that are still followed today
(Tschanz 1997).
Ibn Sina is also credited with inventing a new kind of apparatus for distill-
ing essential oils, called an alembic. During the tenth century many classic texts
were translated from Arabic to Latin, and ibn Sina’s Canon of Medicine first ap-
peared in Europe in the twelfth century. It is interesting that Constantinus
Africus and Gerard of Cremorna, the two translators of this classical text, lived in
different towns and came from two different worlds—one Arabic and one Chris-
tian. This joint project was possible because the two scholars lived in towns close
to the border dividing the Arabic and Christian worlds at that time. Ibn Sina’s
portrait still hangs in the great hall of the School of Medicine at the University
of Paris, and Dante Alighieri held him in the same regard as Hippocrates and
Galen.
Europe
By the thirteenth century, “the perfumes of Arabia” mentioned by Shakespeare
had spread to Europe. Bad odors were thought to harbor disease (interestingly
malaria literally translated means bad air), and being surrounded by pleasant
odors was supposed to give protection against disease, especially the plague.
Physicians wore birdlike masks containing aromatics to protect themselves. They
also carried plague torches, fragrant herbs burned in a tiny brazier at the top of a
long stick, containing aromatic resins and sprinkled houses affected by disease
with aromatic waters like eau de cologne (Stoddart 1990).
Glovemakers in London became licensed to impregnate their wares with es-
sential oils, and legend has it this is why so many glovemakers and perfumers sur-
vived the Great Plague. Scent boxes and pomanders containing solid perfumes
(which originated in the East) became popular among the aristocracy. During this
time the Abbess of Bingen, St. Hildegarde, wrote four books on medicinal plants.
16 Section I Overview

By the sixteenth century, many Europeans had written their own collective
works on herbs and aromatics. With the Renaissance and subsequent world ex-
ploration, many spices were added to Europe’s knowledge of herbs. Cocoa (Theo-
broma cocao) was discovered in South America and tea tree was found in Australia.
During one expedition in the winter of 1535, French explorer Jacques Cartier dis-
covered a cure for scurvy from the Native Americans. Cartier’s ship was frozen in
the St. Lawrence River at St. Croix in Quebec, Canada. Most of the ship’s com-
pany had fallen ill and had purple blotches on their skin, swollen legs, joint pain,
and putrid gums. Several were dying. Cartier’s friend, a Native American called
Agaya, who had been very sick, suddenly appeared to be completely well. In-
trigued, Cartier investigated and discovered Agaya had drunk an extract made
from the tree Native Americans called Annedda.
Native Americans
Annedda is now thought to have been white spruce (Picea glauca), and this was
the first documentation of successful scurvy treatment (Erichsen-Brown 1979).
Native Americans were also adept at treating wounds, often with a tree gum like
Abies balsamea. They treated dysentery with cedar leaves, and they used sweat
lodges to promote healing. Native Americans also used narcotic plants such as
water hemlock in topical applications, vigorously scratching the skin until it bled
before applying the herb. Native-American medicine has produced many plant
remedies such as Black cohosh root (Cimicifuga racemosa) for musculoskeletal
pain and as an aid for labor and hormonal imbalances (Low Dog & Riley 2001)
and May apple resin (Podophyllum peltatum), originally used for warts and today
used to treat skin cancer. Only recently has Native American medicine become
respected for its depth, history, and sophistication (Erichsen-Brown 1979). One
of its advocates, Tieraona Low Dog, MD, is an eminent physician herself.
Fourteenth Century to Present
Paracelsus was born Philippus Aureolus Theophrastus Bombast von Hohenheim
in 1493 near Zurich, Switzerland. Although his father was a physician, it is un-
clear whether Paracelsus ever completed his medical training. He wandered from
university to university and was something of a rebel. His wanderings took him
to live with the Tartars in Asia from whom he learned herbal medicine. He also
learned anatomy from executioners. While he was on his travels he took the name
Paracelsus.
Paracelsus was the subject of many legends, some suggesting he had magic
powers and could conjure a hurricane with a twirl of his hat (Swerdlow 2000). He
was a controversial figure and angered the orthodox medical community of the
day by burning volumes of Avicenna’s work at a public bonfire in the marketplace
in Basel, Switzerland. Paracelsus was frustrated by what he felt were old princi-
ples and wanted to experience something innovative and new. He questioned
Galen’s work and thought the plethora of herbal manuals in circulation were
Chapter 2 The Nature of Aromatherapy 17

written by “quacks” who abused sick people’s lack of knowledge and were only af-
ter quick money.
Paracelsus believed the way forward was to isolate an active ingredient from
a plant. “What the eye perceives in herbs or stone or trees is not yet a remedy; the
eye sees only the dross. The remedy must be cleansed from the dross, then it is
there. This is alchemy” (Griggs 1981). Paracelsus believed isolating the active in-
gredient would enhance the medicine’s strength and increase its safeness. He was
associated with the revolution supporting mineral preparations, and he used mer-
cury, iron, sulfur, and antimony as well as herbs. Although Paracelsus remained
fascinated by alchemy all his life (Griggs 1981), he was also a strong believer in
the doctrine of signatures: that plants indicate the organ of the body they can help
either by their shape or by the place where they grow. It is obvious from his co-
pious writings (14 large volumes) that Paracelsus used herbs knowledgeably, and
he was very successful.
Although a specific action of a plant may appear to depend on a single chem-
ical constituent, isolating it may not make the effect more active or safer. Nature
is not a fool; plants have their own synergistic action that is irreplaceable. In the
plant world, the sum of the parts really does add up to more than the total (Mills
1991). If the most active constituent is removed and applied in isolation, it may
have a different effect or negative side effects. The ability of one part of a plant to
“switch off ” negative properties of another part is sometimes called quenching
(Watt 1991). For example, isolated citral (an aldehyde found in lemongrass) pro-
duces a more severe sensitization reaction at a lower concentration than does the
complete essential oil, which contains a higher percentage of citral.
This concept is further demonstrated by extracting and separating all the ac-
tive ingredients of an essential oil, then recombining them. They will not neces-
sarily produce the same effect as the complete essential oil (or herb). However,
this is how drug companies usually approach research of herbs: they isolate and
synthesize. To this day Paracelsus is regarded as the first medical pharmacologist,
the “patron saint” of drug companies.
When Rene Descartes (1596-1650) declared that man was a machine, the
next hiccup occurred for aromatherapy. Descartes’ philosophy, the basis of Carte-
sian thinking, is summed up in his own words, “cognito, ergo sum,” or “I think,
therefore I am” (Cook 1978). Descartes went on to say mind and body bore no
relationship to one another, and the concept of soul faded. The idea that an aro-
matic compound could have an effect on the body via the brain fell into disrepute.
Not until the eighteenth century when a physician named Gaub suggested that
“bodily diseases may often be more readily alleviated or cured by the mind, that
is by the emotions, than by corporeal remedies” did the idea of a connection be-
tween mind and body return (Lawless 1994). In 1763 Julien La Mettries wrote
an essay that said man was a machine. Gaub disagreed and wrote a response, sug-
gesting doctors should search for substances that affect the mind.Today it is grad-
ually becoming accepted that smell affects the mind. The mind is not an isolated,
18 Section I Overview

single organ, but is connected to every cell of our body. The way each cell feels in-
timately affects the way a person feels overall (Pert 1997).
United Kingdom
William Turner (1520-1568) was one of the earliest English herbalists. A
Cambridge graduate, he believed in the doctrine of signatures and gave many
plants, such as lungwort and liverwort, their common names to indicate their use.
At this time, qualifying to become a physician took up to 10 years. Interestingly,
Shakespeare’s son-in-law John Hall called himself a physician, although he had
only a Master of Arts degree. However, this did not stop him from purchasing
300 plants, “practicing” medicine, and leaving notes from 178 different cases. One
of his patients was the Earl of Compton who lived some 40 miles away, several
days’ journey by horseback (Swerdlow 2000).
During Shakespeare’s time the apothecaries, from whom physicians pur-
chased their medicines, were also prescribing. In 1512, in an attempt to control
the situation, the British Parliament introduced the first laws controlling the pre-
scription and sale of medicines. Six years later, the Royal College of Physicians of
London was established.
However, the seventeenth century is mainly remembered as the golden era
for herbal medicine. Nicholas Culpeper, who posthumously became one of the
more famous herbalists, published his Complete Herbal in 1660. During the 1700s
essential oils were widely used in “mainstream” medicine. In William Salmon’s
The Compleat English Physician oils of cinnamon, lavender, lemon, clove, and rue
are listed with others in a recipe to “cheer and comfort all the spirits, natural, vi-
tal and animal”(Tisserand 1979). In 1770 the British Parliament passed an act to
protect men from the “guiles of perfumed women” who might trick them into
matrimony as the “witchcraft of scent could manipulate their mind” (Watson
2000). The United States followed with a paper published in the New York Med-
ical Journal on the “connections of the sexual apparatus with the ear, nose and
throat” that suggested perfume was a conscious attempt to “stimulate lecherous
thoughts” (Dabney 1913).
The first scientific evaluation of essential oils occurred in the nineteenth cen-
tury, and many of the results were published in William Whitla’s Materia Medica
and Therapeutics in 1882. The industrial and scientific revolutions followed. Dur-
ing the next two centuries scores of essential oils were analyzed. It was thought
important to identify and isolate therapeutic components of plants (just as
Paracelsus had advocated). In the late 1890s specific components such as geran-
iol and citronellol were identified, and in 1868 William Henry Perkin announced
the synthesis of coumarin.
Modern Drug Development
Synthetic copies of perfumes and aromatics began to be appear, and the
era of modern drug development dawned—the third hiccup for aromatherapy.
Chapter 2 The Nature of Aromatherapy 19

Willow bark became aspirin, and foxglove became digitalis. Despite important re-
search on the therapeutic effects of many essential oils by Cadeac and Meunier in
France and Gatti and Cajola in Italy, essential oils and herbal medicine lost out
to the profits of synthetic drugs. With the 1930 partnership of Rockefeller in the
United States and Faben in Germany, the petrochemical pharmaceutical industry
became a major economic and political force.
Following the Flexner report on the nation’s medical schools in 1910 (which
was paid for by the Carnegie Foundation), almost all homeopathic and naturo-
pathic medical schools in the United States were squeezed out. Herbal medicine,
including the use of aromatics, was excluded from medical school curricula.
Petrochemical drug companies became the major underwriters of all medical col-
leges in the United States. More importantly they also became the major funders
of the American Medical Association and therefore 90% of all medical research
(Buckle 2001).
Renaissance of Aromatherapy
The modern renaissance of aromatherapy began in France with the work of a
chemist, a physician, and a nurse: Gattefosse, Valnet, and Maury.
Rene-Maurice Gattefosse, a chemist, lived in France from 1881 to 1950. He
was interested in both the psychologic and physiologic effects of aromatics and
mainly used topical application of essential oils. It was because of an accident that
Gattefosse was first drawn to aromatherapy. In 1910, while he was working in his
laboratory, an explosion occurred, covering him with burning substance. He rolled
on the grass to extinguish the flames. A few days later the wounds became in-
fected with gas gangrene but “one rinse of essential oil of [English] lavender (La-
vandula angustifolia) stopped the gassification of the tissue”(Tisserand 1993).
Impressed by the way his wounds had healed, Gattefosse dedicated his life to re-
searching essential oils. Many of his patients were soldiers wounded in the
trenches of World War I. Among the essential oils Gattefosse used were thyme,
chamomile, clove, and lemon. Until World War II, those essential oils were used
both as natural disinfectants for wounds, and to sterilize surgical instruments
(Ryman 1991).
Gattefosse was one of the first people to use the word aromatherapy. He dis-
covered essential oils take between 30 minutes and 12 hours to be absorbed com-
pletely by the body after being applied topically. His work Aromatherapie: The Es-
sential Oils — Vegetable Hormones (giving detailed medical case studies performed
by various physicians) was published in France in 1937. The manuscript was dis-
covered by Jeanne Rose, translated into English, edited by Robert Tisserand, and
published in English in 1993 (Tisserand 3).
Throughout World War II, French physicians used essential oils on infected
wounds and as a treatment for gangrene. Perhaps the course of aromatic medicine
would have been different if Alexander Fleming had not discovered a piece of
moldy bread that led to the manufacture of penicillin. With the emergence of
manufactured antibiotics—full of promise, profit, and easy availability—came the
20 Section I Overview

fourth hiccup in the history of aromatherapy, and its demise seemed certain.
However, during World War II, American nurses stationed at Pearl Harbor used
handkerchiefs infused with perfume to help cope with the nauseating aroma of
burned flesh (Sarnecky 2001). They also offered the scented handkerchiefs to
their patients. Fessler (1996) suggests this was an early example of modern aro-
matherapy.
Jean Valnet, MD, was born in the early 1900s and died only a few years ago.
A French army physician, he spent much of his life researching aromatherapy and
was interviewed in 1993 by Christine Scott for the International Journal of Aro-
matherapy (Scott 1993-1994). His publication Aromatherapie (Valnet 1937) was
the first “medical” publication on aromatherapy, full of case studies and citing nu-
merous references. Valnet wrote it “is not necessary to be a doctor to use aro-
matherapy. But one has to know the power of essential oils in order to avoid ac-
cidents and incidents” (Scott 1993-1994).
During his time in Indochina, when he was commander of an advanced sur-
gical unit, Valnet used essential oils with the full approval of his superiors. How-
ever, despite impressive results, when he returned to France he found the ortho-
dox medical community unhappy with his use of unconventional medicine and
they tried to strike him from the general medical list. Fortunately for aromather-
apy, some of his patients were high-ranking government officials, including the
Minister of Health, so this did not happen (Scott 1993-1994). Valnet’s book, The
Practice of Aromatherapy, possibly the classic on aromatherapy, has been translated
into German, Italian, Spanish, and Japanese, as well as English.
Marguerite Maury’s life was initially one of tragedy. Born in Austria, she mar-
ried very early and had her first child while still a teenager. Sadly her son died from
meningitis when he was only 2 years old. Shortly afterward, her husband was
killed in action, and his death was closely followed by her father’s suicide. Keen to
make a new start, Marguerite decided to move to France and train as a nurse.
While working in France as a surgical assistant, she met and married Dr. Maury.
He shared her love of the arts and her fascination with alternative approaches to
medicine, and together they formed a cohesive and inspirational team.
Marguerite Maury classified the use of essential oils into various clinical de-
partments: surgery, radiology, dermatology, gynecology, general medicine, psychi-
atry, spa treatment, physiotherapy, sports, and cosmetics. She won two interna-
tional prizes for her research on essential oils and the skin, and her book, Le
Capital Jeunesse, was published in 1961 and translated into English 3 years later.
She left a dedicated and now famous pupil, Daniele Ryman, to continue her
work (Maury 1964).
Gattefosse, Valnet, and Maury may have been the first pioneers of modern aro-
matherapy, but there were plenty of now-famous names waiting in the wings.
Tisserand and Price made aromatherapy a household word in England and sparked
the interest of the medical and nursing community. Many researchers—too many
to list—followed. Of particular note are Gildemeister in Germany, Guenther and
Lawrence in the United States, Leclerc and Belaiche in France, and Dodd, Deans,
Chapter 2 The Nature of Aromatherapy 21

and Svoboda in the United Kingdom, all of whom wrote extensively about the clin-
ical use of essential oils. Today, there is a wealth of information and sufficient evi-
dence to suggest the medicine of the future could be a sweet-smelling one.
How Essential Oils Work
The study of where essential oils go when they are absorbed and how they are ab-
sorbed and eliminated by the body is called pharmacokinetics. Essential oils are ab-
sorbed into the body through digestion, through the “internal skin” lining of ori-
fices (mouth, vagina, and anus), by olfaction, and through the external skin ( Jager
et al 1992).
There is fairly heated debate as to how aromatherapy should be used. Some
people believe the term aromatherapy means just that: inhalation. But, in many
parts of the world, aromatherapy is often combined with touch, as the absorption
of essential oils through the skin coupled with soothing touch (or warmth) may
enhance and prolong their therapeutic effects. Some believe the sublingual, rec-
tal, and vaginal routes of absorption are the most effective. Others believe essen-
tial oils are most useful when taken orally and digested. Clearly there is a differ-
ence in metabolism between a substance that is ingested and one that is applied
topically (to internal or external skin) or inhaled. Ingestion of essential oils is
more akin to Western medicine.
There is a substantial body of knowledge about the absorption of essential
oils through the shaved skin of animals or by injection into their peritoneal cavi-
ties, but published research on the absorption of essential oils through human
skin or by ingestion is limited. There is published research to show inhaled es-
sential oils affect the human brain, but clearly the use of aromatherapy in a clin-
ical setting is in its infancy. Patients say aromatherapy works, and the whole
movement of aromatherapy in health care appears to be led by patients as much
as practitioners.
Using aromatherapy in a clinical setting is still a bit like pioneer work. Nurses
using aromatherapy say they feel a little like modern-day Florence Nightingales.
Although it is impossible to provide evidence of efficacy without research, a pat-
tern of efficacy is emerging. Health professionals believe there is sufficient anec-
dotal evidence to show clinical aromatherapy is efficacious, cost effective, and
safe, but the information is scattered. A major collaborative effort is needed to
bring together all that information so the “pattern” becomes clear. That pattern
will be the basis for future research.
Routes of Absorption of Essential Oils
Essential oils contain many different components, and these components are ab-
sorbed by the body. Thus lavender is not found in the bloodstream, but linalyl ac-
etate and linalol, two of the major components found in lavender, are found in the
bloodstream after inhalation, topical (internal or external) application, or inges-
tion of lavender essential oil.
22 Section I Overview

There are four methods by which the components within essential oils can
be absorbed.
1. Topical: using external skin via touch, compress, or bath
2. Internal: using internal skin via mouthwashes, douches, pessaries, or sup-
positories
3. Oral: via gelatin capsules or diluted in honey, alcohol, or a dispersant (pur-
chasable from most good essential-oil companies)
4. Inhaled: directly or indirectly, with or without steam
Each method of application has its own physiologic process, advantages, and
disadvantages.
Topical Application
“A good name is like a precious ointment; it filleth all around about, and will not
easily away; for the odors of ointments are more durable than those of flowers.”
Francis Bacon, 1561-1626
The skin is a complex, multifaceted membrane, varying from a fraction of a mil-
limeter thick on the eyelid to approximately 3-mm thick on the back. The skin is
the largest organ in the body. For many years the skin was thought to be a bar-
rier, and it was believed drugs could not be absorbed through the skin. Women
were ridiculed for putting creams and lotions on their faces in an effort to pre-
serve their youthfulness. Now it is acknowledged that cosmetics not only pene-
trate the stratum corneum but are also absorbed into the viable epidermis (Zatz
1993). Autoradiography can be used to demonstrate the absorption of lipid-
soluble substances through the skin (Fig. 2-1) (Suzuki et al 1978).
Nicotine patches are common since the advent of patch therapy, and many
conventional drugs are now administered transdermally on a continuous basis.
Examples of such drugs are antianginals such as nitroglycerine, the female hor-
mones estradiol and progesterone, antihypertensives such as clonidine, narcotics
such as fentanyl, and antispasmodics and antiemetics such as scopolamine (Cleary
1993). Topical anesthetic lidocaine and cortisone dexamethasone have also been
introduced using a transdermal patch in combination with an electric current
(Zetzer et al 1991). Tests are currently in progress to establish how commercially
viable it will be to deliver beta-blockers timolol and bupranolol, antihistamines
tripolidine and azatadine, and testosterone via this method. Furthermore, the
New York Times reported that scientists may have found a way to avoid the sting
of vaccinations by spreading the vaccine on the skin. The vaccinations tested on
the mice were diphtheria, tetanus, and cholera (Associated Press 1998).
Not every substance is absorbed through the skin in the same amount.
Hotchkiss (1994) demonstrated that only 1% of Cypermethrin (a pesticide) was
absorbed, but 65% of benzoic acid (a fungicide) was absorbed through human
skin. Two processes are involved in topical absorption: penetration and perme-
ation (Reiger 1993). Penetration is the actual entry of a substance into and
through the skin, whereas permeation is the subsequent absorption of a substance
Chapter 2 The Nature of Aromatherapy 23

24 Section I Overview
Figure 2-1 Diagram to show drug absorption through skin. (From Zatz J. 1993. Factors affecting absorption of topically applied substances. In Zatz J
(ed.), Skin Permeation: Fundamentals and Applications. Wheaton, IL: Allured.)

into the body. Obviously the former is more important if the skin is being treated
and the latter if a systemic treatment is sought.
The process of diffusion and permeation are in part described by Fick’s laws
(Rieger 1993). These are a series of mathematical descriptions of diffusion
through membranes. More important than the actual concentration of the sub-
stance (in this case the essential oil), is its chemical activity or potency. Therefore
if an essential oil contains a small amount of a potent component (a phenol), its
chemical potential is greater than that of an essential oil containing a larger
amount of a less potent chemical (an alcohol).
If the essential oil is diluted in a substance with lower permeability, its
progress, or pharmacokinetics, are adversely influenced. In other words, essential
oils diluted in a fixed oil (carrier oil) are absorbed more slowly than undiluted es-
sential oils. The actual carrier medium can also affect (and to a certain extent in-
hibit) the concentration of the active ingredients of essential oils. For example, in
one study, the germicidal effects of phenol (a common constituent of essential
oils) could not be exerted when it was applied to the skin in a fatty base (Zatz
1993a). Heat appears to enhance penetration, and hot water may speed up the ab-
sorption of essential oils into the skin. Studies have shown that penetration of the
dermis is increased 100-fold if essential oils are dispersed in a bath (Buchbauer
1993a).
Essential oils are lipid soluble, and they can be absorbed through the skin
rapidly. Fuchs et al (1997) reported that carvone, a ketone component found in
essential oils, was found in the bloodstream of a human subject within 10 min-
utes of a massage. Carvone was also found in the subject’s urine. The subject, a
25-year-old woman, wore a mask to avoid inhaling the aroma. The exact time re-
quired for absorption depends on the weight of the molecule and certain physio-
chemical properties, such as polarity and optical activity (Jager et al 1992). In
simple terms, polarity refers to polar molecules, so called because they have a neg-
ative and positive “pole” which attract opposite charges (Bowles 2000). Optical
properties refers to the ability of molecules to rotate in polarized light (Williams
1996). In the case of lavender, most of the two main constituents, linalol and lina-
lyl acetate, were absorbed within 20 minutes and eliminated within 90 minutes.
The disadvantage of applying essential oils topically is not all of the essential oil
is absorbed unless an occlusive dressing is applied. Otherwise, much of the es-
sential oil evaporates because of its high volatility. Straehli, who researched the ki-
netics of essential oils in 1940, found that all the essential oils appear in the breath
following absorption through the skin, although the time interval differs with
each essential oil (Tisserand 1985).
The greater the percentage of skin covered, the greater the penetration by an
essential oil (Balacs 1993). Friction, caused by stroking or massage, encourages di-
lation of blood vessels in the dermis, which increases absorption of the essential
oils (Pratt & Mason 1981). Because the stratum corneum (the outer layer of the
epithelium) is partly hydrophilic and partly lipophilic, some water-based and
some oil-based components can pass through it (Riviere 1993). Essential oils are
Chapter 2 The Nature of Aromatherapy 25

lipid soluble so they gain rapid access to lipid-rich areas of the body (Buchbauer
1993), such as the myelin covering of medullated nerve fibers. This lipid solubil-
ity also enables the relatively small molecules of components within the essential
oils to cross the blood-brain barrier: the separation of neurons from capillary walls
by astrocytes (Anthony & Thibodeau 1983).
Although some areas of skin are more accessible, all areas of the skin are per-
meable. Clearly this indicates that it is not necessary, or sometimes even advis-
able, to give a patient a full-body treatment. Patients’ feet are usually easily acces-
sible, and they rarely have intravenous infusions attached to them. Treatment of
feet requires no removal of clothes apart from shoes and socks, and therefore the
feet are possibly the least embarrassing body part to have touched (except for the
hands). Another advantage of using the feet is they are not highly innervated ar-
eas like the face, nor are they areas of low innervation like the back (Weiss 1979).
Caution should be taken when applying essential oils to damaged skin, be-
cause damaged skin is more absorbent of outside chemicals. Moore et al (1980)
found twice as much lead was absorbed by abraded skin as undamaged skin. In a
clinical setting, damaged skin includes skin affected by systemic disease; derma-
tology problems; or dehydration caused by a cold, dry environment or the daily
use of strong detergents. Stress (either physical or emotional) results in vascular
shut-down, which produces cold hands and feet. Psychologic stress also perturbs
the epidermal permeability-barrier homeostasis (Garg et al 2001); in the case of
essential oils this means that less is absorbed. However, when a patient is sweat-
ing, the body is trying to get rid of heat and the blood vessels are dilated. But di-
lated blood vessels can increase penetration of essential oils. Older skin, because
it is thinner and its barrier function is diminished, tends to absorb essential oils
faster.
Topical absorption can be enhanced with an occlusive dressing (Fuchs et al
1997). This reduces the potential for evaporation. Fuchs et al (1997) found that
with an inclusive wrap, substantially more of the essential oil components were
absorbed. Bronaugh’s study (1990) showed that 75% of a fragrance was absorbed
when the skin was covered, and only 4% was absorbed when the skin was not cov-
ered. Covering the skin also increases its temperature and hydration and therefore
enhances penetration. Topically applying essential oils has several advantages:
they do not need to be digested, they are simple to use, and the essential oils are
excreted slowly. This is also the most direct way to treat topical issues such as skin
problems or muscle complaints. There are a few disadvantages. One disadvantage
is that the skin contains certain enzymes that can activate (or inactivate) toxic
chemicals (Tisserand & Balacs 1995). Another disadvantage of applying essential
oils topically is that some essential oils (those containing phenols) can be epider-
mal irritants and others (containing furocoumarins) may cause photosensitivity.
Epidermal absorption is still not fully understood, and pharmacokinetics is a
relatively new field. What is safe to put on the skin and in what concentration is
an ongoing dialogue between cosmetic manufacturers. For many years the most
commonly used hospital bactericide for hand washing and consumer products
26 Section I Overview

was hexachlorophane. At the time, it was thought to be completely safe. How-
ever, hexachlorophane was later demonstrated to be a potential neurotoxin
(Sherman & Leech 1973). Because of a manufacturing error in the 1970s, a baby
powder was manufactured that contained 10 times the intended concentration of
hexachlorophane. This resulted in the deaths of several babies in France. It is
thought that because the diapers acted as an occlusive dressing, the drug’s ab-
sorption was enhanced ( Jackson 1993). The use of hexachlorophane in medical
products such as Ster-Zac and Dermalex was halted in 1973 because of the toxic
effects it might produce when absorbed into the body (McFerran 1996).
Finally, a serious disadvantage is that many essential oils plants are still grown
with pesticides. While gas chromatography might indicate this, because it ana-
lyzes the different compounds in an essential oil, pesticides are not beneficial to
human skin and can also cause a reaction that has nothing to do with the essen-
tial oil. Expressed essential oils are most likely to have high levels of pesticides.
Topical application of essential oils can be used for the following:
Relieving localized trauma such as bruising, sprains, stings, or burns
Relaxing and warming specific muscles
Cooling specific areas
Relieving neuralgic conditions
As an antiinflammatory
As an antispasmodic
As a specific antiviral, antifungal, or antibacterial agent for skin infections
For systemic treatments including hormonal imbalance
As a general body relaxant
Topical applications can be given as follows:
In a carrier oil (cold-pressed vegetable oils)
In an ointment
In a gel
Undiluted (see Chapter 4)
In a bath (sitz, hand, foot, or full)
As a compress
In a wound irrigation
The amount of an essential oil absorbed through the skin depends (not in any specific or-
der) on the following:
Dilution used
Amount used
Amount of skin surface covered
Choice of essential oil
Choice of carrier (lotion, oil, cream, alcohol, water)
Part of the body used
Temperature of the skin
Integrity of the skin
Heat of the environment
Age of the skin
Chapter 2 The Nature of Aromatherapy 27

In an aromatherapy massage, or when the essential oil is applied using the
“m” technique, much of the essential oil evaporates into the room and is inhaled
by the patient. Therefore the benefit is likely to be a synergy of the topically ap-
plied and inhaled essential oils together. Both, mixed with gentle touch, allows
the patient to relax and breathe deeply. It is difficult to separate the two means of
entry, and it is suggested they could work synergistically. Currently there is no
body of comparative knowledge on the gastrointestinal and cutaneous absorption
of the same test material ( Jackson 1993).
Oral and Internal Administration
The oral route for administering essential oils is important and can be an excel-
lent way to treat gastrointestinal problems. Almost all other problems can be
helped using other methods. For those who have a license to prescribe, the oral
route (aromatic medicine) is very powerful. Aromatic medicine can produce im-
pressive results, especially with chronic or acute infections. In the United King-
dom the Aromatherapy Organization Council, the lead body for aromatherapy,
advises against the oral use of essential oils. The Royal College of Nursing accepts
all methods of aromatherapy as part of nursing care except the oral use of essen-
tial oils. However, the internal skin route (using the inner skin of the mouth, rec-
tum, and vagina) is an extension of the external skin route (Schultz 2002) and is
very relevant to nursing care.
Essential oils can be used in a mouthwash, which is excellent for mouth in-
fections, and are very important in dental care. Gargles can be very effective in
treating tracheitis. Essential oils can also be diluted in a douche or on a tampon
and are very effective for some vaginal infections. Essential oils can also be used
in both vaginal and rectal pessaries to treat infection and inflammation. Both rec-
tal and vaginal routes have a distinct advantage in the treatment of reproductive
or urinary conditions because the essential oils are absorbed directly into the sur-
rounding tissue. Recurrent cystitis responds well to this method of treatment.
In aromatic medicine, essential oils can be administered orally either in a
gelatin capsule, honey water, or alcohol (Valnet 1990). For more information,
please see Chapter 7. This is a highly specialized field that requires proper train-
ing and, in the United States, probably a license to prescribe. Despite the fact that
many essential oils are used in small amounts as flavoring agents in our food, pure
essential oils are concentrated and are not to be experimented with casually. Just
as a whole bottle of Tylenol can be lethal (although this drug is still sold over the
counter because the public is expected to take only one or two tablets at a time),
so a few essential oils can be lethal if several milliliters are ingested at once. Price
and Price (1999) suggest the maximum number of essential oil drops taken in-
ternally should be limited to 3 drops 3 times a day for a period of 3 weeks maxi-
mum. Brinker (2000) suggests up to 2
1
⁄
2
ml a day. (If there are 20 drops per mil-
liliter, this works out to be 50 drops a day, which does seem a little high.)
However, much depends on the essential oils and its chemical constituents.
28 Section I Overview

A safer option is to offer herbal teas. These are gentle and are sold over the
counter. Common herbal teas are chamomile, peppermint, ginger, and fennel.
Warning: Encouraging patients to take essential oils by mouth is not advised
unless the person advocating it is trained in this method.
Inhalation
“Smells are surer than sounds and sights to make your heartstrings crack.”
Rudyard Kipling (Birchall 1990)
Of all the methods for introducing essential oils into the human body, inhalation
is the simplest and fastest. It is also the oldest method, and the use of aromatics
in rituals is well documented. Perfume, as the name implies, began its existence
as a ritual source of odor spread by heat and smoke (Watson 2000). The Oxford
Dictionary defines perfume as “odorous fumes of burning substance,” and the
word is derived from the Latin fume, meaning smoke (Oxford Dictionaries 1964).
Inhalation may be the oldest method of drug use, but it is also turning out to be
one of the most current. The latest drug to be used via olfaction is insulin. In this
revolutionary method of treating diabetes, powdered or liquid insulin is inhaled
once a day (Epstein 2001). Inhalation takes the essential oils from the outside of
the body to deep inside the body in one easy step. The lungs have a huge surface
area that is intimately connected to the blood system via the alveoli. Jori et al
(1969) showed that inhaled cineole (an oxide found in eucalyptus and several
other essential oils) can have a measurable effect at very low concentrations.
Olfaction
The nose has two distinct functions: to warm and filter incoming air and to act as
the first part of the olfactory system. If inhalation was the same as olfaction, then
olfactory stimuli would be obvious each time a breath was taken, which is not the
case; taking a normal breath is different than sniffing an essential oil (Alexander
2001). However, aromas can have instant effects, and sometimes just thinking
about a smell can be as powerful as actually smelling it (Betts 1996). Odors have
psychologic and physiologic effects. Until very recently smelling salts were the
standard method for reviving someone who had fainted. A person knows imme-
diately if a smell is pleasant or unpleasant and what memories it evokes. Smell is
a chemical reaction; receptors in the brain respond to chemicals within the es-
sential oil. As a person breathes in, these chemicals move up behind the bridge of
the nose, just beneath the brain, where they attach themselves to millions of hair-
like receptors connected to the olfactory bulb. These receptors are extremely sen-
sitive and can be stimulated by very subtle scents. Different odors bind to distinct
arrays of receptors. This allows people to discriminate between more than 10,000
odors, even though there are only about 1000 odor receptors.
Because olfactory receptors are so sensitive, they are easily fatigued, which ex-
plains why smells seem less obvious as the body tires or adapts to them (Anthony
Chapter 2 The Nature of Aromatherapy 29

& Thibodeau 1983). Air flows through the nostrils at different rates because of
turbinate swelling. Every few hours, the nostril taking in more air switches from
left to right. In one study, odors breathed through one or the other nostril pro-
duced different effects; 17 out of 20 participants identified l-carvone differently,
depending on which nostril was dominant. However, there are no differences with
regard to the electrical changes in the brain between the left and right nostrils
(Walter et al 1964). Essential oils are highly complex and are made up of many dif-
ferent chemical components, or odor molecules. These molecules travel via the
nose to the olfactory bulb and on to the limbic system of the brain.
The limbic system (LS) is vital for normal human functioning and is the
oldest part of the human brain, supposedly having evolved first. (In lower verte-
brates it is called the smell brain, because these animals depend on their sense of
smell for survival.) The LS is a complex inner ring of brain structures below the
cerebral cortex, arranged into 53 regions and 35 associated tracts (Watts 1975).
The main structures in the limbic system are the amygdala, septum, hippocam-
pus, anterior thalamus, and hypothalamus. These structures are connected by a
number of complicated pathways (Anthony & Thibodeau 1983). Of these re-
gions, the amygdala and hippocampus are of particular importance in processing
aromas.
The amygdala is an almond-shaped group of subcortical nuclei located un-
der the surface of the front medial portion of the temporal lobe. It is thought to
play a pivotal role in processing emotion and in the formation of emotional mem-
ory, and it governs emotional response. The amygdala is known to affect survival
behavior and is intimately responsible for the sensation of fear. It is also thought
to play an important role in controlling aggression. Autism has been linked to a
change in the cells of the amygdala (Edelson 2001). Diazepam (Valium) is
thought to reduce the effect of external emotional stimuli by increasing gamma
aminobutyric acid (GABA)-containing inhibitory neurons in the amygdala
(LeDoux 1996). True lavender (Lavandula angustifolia) is thought to have a
similar effect on the amygdala, producing a sedative effect similar to diazepam
(Tisserand 1988). This is interesting because tricyclics or benzodiazepines, which
were commonly used by orthodox medicine to treat chronic pain, also inhibit the
action of nociceptor neurotransmitters. True lavender is a common essential oil
used topically for pain relief that also appears to enhance the effect of orthodox
pain medication.
The hippocampus is where the memory of smell is triggered, so this part of
the limbic system is concerned with the formation and retrieval of explicit mem-
ories (LeDoux 1996). It is also closely involved with the three types of memory:
semantic (facts and concepts), episodic (recollection of events), and spatial (recog-
nition). The hippocampus is thought to be the storage area for new experiences
before they become permanent memories that are then believed to be stored in
the cerebral cortex. The hippocampus is particularly vulnerable to ischemia,
Alzheimer’s disease, and epilepsy (Healing Arts 2001). A stroke can affect mem-
ory, but only if it causes bilateral damage to the hippocampus.
30 Section I Overview

As well as influencing the expression of emotions, instinctive behaviors, dri-
ves, and motivations, the limbic system plays an essential role in learning and
memory (Kirk-Smith 1993). Buchbauer (1993a) states the limbic system is re-
sponsible for sexual desires and feelings of wellness and harmony. The posterior,
superior part of the cingulate gyrus is related to sexual behavior and is linked to
obsessive-compulsive behavior (Diamond et al 1985).
The limbic system also receives most sensory input and passes it on to the
voluntary and involuntary motor centers. Gatti and Cajola (1923) noted that
odors produced an immediate effect on respiration, pulse, and blood pressure, and
therefore concluded that odors had produced, by a reflex action, a dramatic effect
on the functioning of the central nervous system. Singewald et al (2000), nearly
80 years later, found that the locus coeruleus played a pivotal role in conditioned
fear and inescapable shock.
The effect of odors on the brain has been “mapped” using computer-
generated tomographics. These brain electrical activity maps indicate how sub-
jects linked to an electroencephalogram psychometrically rate odors presented to
them (Van Toller et al 1992). Smells can have a psychologic effect even when the
aroma is below the level of human awareness. Lorig et al (1990) reported the ef-
fects of subliminal (below consciousness) smelling of vanilla. The scent of vanilla
was found to elicit positive mood change. Aromas can also have an effect while a
person is sleeping (Bardia et al 1990).
An electrical phenomenon discovered by Grey in 1964 called contingent
negative variation (CNV) showed the sedative effects of diazepam decreased
CNV, and the stimulant effect of caffeine increased CNV. When fragrances were
tested, these also caused different effects. Lavender produced a similar reaction to
diazepam, decreasing CNV, and jasmine had the reverse effect, increasing CNV
(Torii et al 1991). Rovesti and Columbo’s research (1973) showed that olfactory
receptors are also affected by nonvolatile molecules in aerosols. This was con-
firmed with research conducted by Vellmair et al in 1998.
Anosmia Certain genetic conditions, such as Kallman’s syndrome, pro-
duce anosmia (Bartoshuk & Beauchamp 1994), the lack of a sense of smell.
Sometimes there is specific anosmia, which means a certain aroma, such as an-
drostenone, is not smelled or is perceived differently. When the olfactory nerve
has been severed by trauma, aromas are unable to connect to the limbic part of
the brain. However essential oils can still enter the body through the lungs, skin,
or ingestion. When a person has a sinus infection or a heavy cold, some aromas
may get through; they tend to be the most penetrating, such as peppermint and
eucalyptus. Temporary loss of smell can also follow a severe shock or infection.
Smell is closely aligned to the sense of taste. Taste is divided into four categories:
salty, sour, sweet, and bitter. Salty and sour tastes involve ion channels in the cells
of receptor membranes, whereas sweet and bitter tastes bind to receptor proteins
(Bartoshuk & Beauchamp 1994).
Administration Via the Olfactory System Inhalation can be targeted di-
rectly to a single patient, in which case it is called direct inhalation, or it can be
Chapter 2 The Nature of Aromatherapy 31

used in a more general way, for example in a room of people. This second method
is called indirect inhalation. Indirect inhalation can use a selection of apparatus:
electrical, heat, or battery operated.
Direct Inhalation
1. Tissue or cotton ball: Put one to five drops of essential oil(s) on a facial
tissue or cotton ball and inhale for 5 to 10 minutes. Alternately, aroma rib-
bons can be attached to the bedclothes of children or adults for an easily
applied sleeping or comfort aroma. Cut off a 1-inch piece of ribbon and
attach it to the mattress or pillow with a diaper pin. Caution: Ensure that
the pin is secure and that a child cannot put the ribbon in his or her
mouth.
2. Steam: Add one to five drops of essential oil to a bowl of steaming water.
Place a towel over the patient’s head and ask him or her to inhale for 10
minutes. Remember to ask the patient to close his or her eyes and remove
spectacles. Because soft contact lenses can absorb some of the essential oil
and cause stinging, it is a good idea to remove lenses before steam inhala-
tion. Caution: Avoid this procedure with the elderly, confused, very
young, or infirm.
3. Hood: The hood is a new method of delivery, initially designed for a labo-
ratory experiments, that uses a controlled and measured supply of essential
oil and involves a stream of vaporized aroma combined with air and
pumped at a constant rate into an oxygen-therapy hood (Palmer et al 1999).
Indirect Inhalation
1. Room fresheners: Add one to five drops of essential oil to a bowl of hot
water and place in a safe space. The warmth of the water gradually allows
the essential oils to evaporate with the water. This is excellent in air-
conditioned facilities where the atmosphere may be dry.
2. Burners: Burners usually have a small candle that heats a container sus-
pended above. Float one to five drops of essential oil on top of water in
the container. The water stops the essential oil from burning and leaving
a yellow, sticky residue. Caution: Keep away from children and pets.
3. Fans: Fans can be battery or electrically operated and come with a num-
ber of small, absorbent pads. Add one to five drops to the pad, place in the
fan, and switch on. Inexpensive spare pads can be made by cutting incon-
tinence pads or pantyliners into the correct small, square size.
4. Humidifiers: Humidifiers can be purchased in most drug stores. Fill the
container with water. Place essential oils on a tissue and put the tissue in
the direct pathway of the exiting steam. Do not float the essential oil on
top of the water inside the humidifier because it will not come out with
the steam, but will remain floating on the water. This is an excellent
method for treating croup and asthma.
5. Diffusers: Diffusers can be multifaceted, with different compartments
timed for different hours, or a more simple apparatus. Gentle heat causes
the essential oil to evaporate.
32 Section I Overview

6. Nebulizers: Nebulizers are electrical units with small, glass attachments
into which drops of undiluted essential oil are placed. Microdroplets of
the essential oil are atomized into the air, often at timed intervals, ioniz-
ing the air. Most nebulizers use no heat. They can be expensive and frag-
ile, but they are most effective for large areas. Caution: Avoid overdosing
with essential oils.
7. Spritzer sprays (essential oils in water): Sprays are excellent for hot flashes
or fatigue. Caution: Avoid spraying on plants or flowers by mistake.
Benefits of Inhalation: Inhalation is effective for both physical and psy-
chologic complaints. It is a simple method, is fast acting, and is empowering for the
patient. Inhaled essential oils can be particularly useful for treating the following:
Upper and lower respiratory tract infections
Hay fever, sinusitis, and headache
Asthma
People who cannot be touched, for physical or psychologic reasons
Prevention of cross-infection
Depression or fatigue
Insomnia
Finally, the nose, as well as governing the smell system, contains a touch sys-
tem, which is often (wrongly) thought to be part of the smell system. This touch
system is the trigeminal system and forms part of the fifth cranial nerve. It can
detect aggressive odors such as acetic acid and ammonia and causes the head-
swiveling reflex (Van Toller & Dodd 1991).
REFERENCES
Alexander M. 2001. How Aromatherapy Works: Vol. I, Principle Mechanisms in Olfac-
tion. Odessa, FL: Whole Spectrum Arts and Publications.
Anthony C, Thibodeau G. 1983. Nervous System Cells in Anatomy and Physiology. St.
Louis: Mosby.
Associated Press. 1998. Scientists see vaccinations without sting. New York Times. Feb
26 A15.
Balacs T. 1993. Essential oils in the body. In Aroma 93 Conference Proceedings.
Brighton, UK: Aromatherapy Publications, 12-20.
Bardia P, Boecker M, Lammers W. 1990. Some effects of different olfactory stimuli on
sleep. Sleep Research. 19, 145.
Bartoshuk L, Beauchamp G. 1994. Chemical senses. Annual Review of Psychology. 45
419-449.
Betts T. 1996. The fragrant breeze: The role of aromatherapy in treating epilepsy. Aro-
matherapy Quarterly. 51(Winter) 25-27.
Birchall A. 1990. A whiff of happiness. New Scientist. 25(August) 44-47.
Brinker F. 2000. The Toxicology of Botanical Medicines, 3rd ed. Sandy, OR: Eclectic
Medical Publications.
Bowles J. 2000. The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Printers.
Chapter 2 The Nature of Aromatherapy 33

Bronaugh R. 1990. In vivo percutaneous absorption of fragrance ingredients in rhesus
monkeys and humans. Food and Chemical Toxicology. 28(5) 369-373.
Buchbauer G. 1993. Molecular interaction. International Journal of Aromatherapy. 5(1)
11-14.
Buchbauer G. 1993a. Biological effects of fragrances and essential oils. Perfumer and
Flavorist. 18(19) 19-24.
Buckle J. 2001. The ethic of plant v petrochemical medicine. International Journal of
Aromatherapy. 11(1) 8-17.
Chadwick J, Mann W (eds.). 1983. Hippocratic Writings. Harmondsworth, UK: Pen-
guin Books.
Chopra D. 1991. Perfect Health: The Complete Mind/Body Guide. New York: Har-
mony Books.
Cleary G. 1993. Transdermal drug delivery. In Zatz J (ed.), Skin Permeation: Funda-
mentals and Applications. Wheaton, IL: Allured Publishing, 207-238.
Cook C (ed). 1978. Pears Cyclopedia, 87th ed. London: Pelham, B19.
Dabney V. 1913. Connections of the sexual apparatus with the ear, nose and throat. New
York Journal of Medicine. 97, 533.
Diamond M, Schreibel B, Elson L. 1985. The Human Brain Coloring Book. New York:
Harper.
Edelson S. 2001. Autism and the limbic system. Retrieved January 2002 from
http://www.autism.org.
Epstein R. 2001. For some, insulin without needles. New York Times. July 17, F5.
Erichsen-Brown C. 1979. Medicinal and Other Uses of North American Plants. New
York: Dover Publications.
Fessler D. 1996. No Time For Fear: Voices of American Military Nurses in World War
II. Lansing, MI: Michigan State University Press.
Franchomme P, Penoel D. 1990. Phytoguide: Aromatherapy Advanced Therapy for In-
fectious Illnesses. International Phytomedical Foundation. Limoges, France: Jollois.
Fuchs N, Jager W, Lenhardt A et al. 1997. Systemic absorption of topically applied car-
vone: Influence of massage technique. Journal of the Society of Cosmetic Chemists.
48(6) 277-282.
Garg A, Chren M, Sands L et al. 2001. Psychological stress perturbs the epidermal per-
meability barrier homeostasis. Archives of Dermatology. 137(1) 53-59.
Gattefosse R. 1937. (Translated in 1993 by R. Tisserand.) Aromatherapie: Les Huile
Essentielles-Hormones Vegetales (Gattefosse’s Aromatherapy.) Saffron Walden, UK:
CW Daniels, 89.
Gatti G, Cajola R. 1923. L’Azione delle essenze sul sistema nervosa. Rivista Italiana
delle Essenze e Profumi. 5, 133-135.
Gilt A. 1992. Aromatherapy 2000 and beyond. Journal of Alternative and Complemen-
tary Medicine. 9, 19-20.
Griggs B. 1981. Green Pharmacy. London: Jill Norman & Hobhouse.
Guirdham A. 1990. The Cathars and Reincarnation. Saffron Walden, UK: CW Daniels.
Healing Arts. 2001. Medial temporal lobe (the limbic system). Retrieved January 2002
from http://www.healing-arts.org.
Holmes P. 1993. The Energetics of Western Herbs, Vols. 1 and 2. Berkley, CA: Nattrop
Publishing.
Hotchkiss S. 1994. How thin is your skin? New Scientist. Jan 29, 24-27.
34 Section I Overview

Jackson E. 1993. Toxicological aspects of percutaneous absorption. In Zatz J (ed.), Skin Per-
meation: Fundamentals and Applications. Wheaton, IL: Allured Publishing, 177-193.
Jager W, Buchbauer G, Jirovetz L et al. 1992. Percutaneous absorption of lavender oil
from a massage oil. Journal of the Society of Cosmetic Chemists. 43(1) 49-54.
Jori A, Bianchelli A, Prestini P. 1969. Effects of essential oils on drug metabolism. Bio-
chemical Pharmacology. 18(9) 2081-2095.
Kirk-Smith M. 1993. Human olfactory communication. In Aroma 93 Conference Pro-
ceedings. Brighton, UK: Aromatherapy Publications, 86-103.
Komori T, Fujiwara R, Tanida M et al. 1995. Effects of citrus fragrance on immune
function and depressive states. Neuroimmunomodulation. 2:174-180.
Kusmerik J. 1992. Aromatherapy for the Family. London: Institute of Classical Aro-
matherapy, Wigmore Publications.
Lawless J. 1992. The Encyclopedia of Essential Oils. Shaftesbury, UK: Element Books.
Lawless J. 1994. Aromatherapy and the Mind. London: Thorsons.
LeDoux J. 1996. The Emotional Brain. New York: Simon & Schuster, 170, 264.
LeRoy Ladurie E. Bray B, translator. 1984. Montaillou. London: Penguin Books.
Levabre M. 1990. Aromatherapy Workbook. Vermont: Healing Arts Press.
Lorig T, Herman K, Schwartz G et al. 1990. EEG activity during administration of low
concentration odors. Bulletin of the Psychonomic Society. 28, 405-408.
Low Dog T, Riley D. 2001. An integrative approach to menopause. Alternative Thera-
pies in Health and Medicine. 7(4) 45-55.
Maury M. Ryman D, translator. 1964. Le Capital Jeunesse (The Secrets of Life and
Youth). London: Macdonald.
McFerran T (ed.). 1996. A Dictionary of Nursing, 2nd ed. Oxford UK: Oxford Univer-
sity Press.
Mills S. 1991. Out of the Earth. London: Viking Arkana.
Moore M, Meredith P, Watson W et al.1980. The percutaneous absorption of lead-203
in humans from cosmetic preparations containing lead acetate, as assessed by whole-
body counting and other techniques. Cosmetic Toxiocology. 18:399-405.
Mojay G. 1996. Aromatherapy for Healing the Spirit. London: Giai Books, Ltd.
Oxford Dictionaries. 1964. Concise English Dictionary. Oxford, UK: Oxford University
Press.
Palmer B, Stough C, Patterson J. 1999. A delivery system for olfactory stimuli. Behavior
Research Methods, Instruments, & Computers. 31(4) 674-678.
Pert C. 1997. Molecules of Emotion. New York: Scribner, 304.
Pratt J, Mason A. 1981. The Caring Touch. London: Heyden.
Price S, Price L. 1999. Aromatherapy for Health Professionals. London: Churchill Liv-
ingstone, 93.
Proust M. 1981. Remembrance of Things Past, Vol 1. New York: Random House.
Reiger M. 1993. Factors affecting sorption of topically applied substances. In Zatz J
(ed.), Skin Permeation: Fundamentals and Applications. Wheaton, IL: Allured Pub-
lishing, 33-72.
Riviere J. 1993. Biological factors in absorption and permeation. In Zatz J (ed.), Skin Per-
meation: Fundamentals and Applications. Wheaton, IL: Allured Publishing, 113-125.
Rose J. 1992. The Aromatherapy Book. San Francisco: North Atlantic Books.
Rose J. 1992a. A history of herbs and herbalism. In Tierra M (ed.), American Herbal-
ism. Freedom, CA: Crossing Press, 3-32.
Chapter 2 The Nature of Aromatherapy 35

Rovesti P, Columbo E. 1973. Aromatherapy and aerosols. Soaps, Perfumery and Cos-
metics. 46:475-477.
Ryman D. 1991. Aromatherapy. London: Piatkus.
Sarnecky M. 2001. Nurses at Pearl Harbor: the real story. Reflections of Nursing Lead-
ership. 17-20, 51.
Schultz N. 2002. Personal communication.
Scott C. 1993-1994. In profile with Valnet. International Journal of Aromatherapy. 5(4)
10-13.
Sherman R, Leech R. 1973. Neuropathology in newborn infants bathed in hexa-
chlorophene. Morbidity and Mortality. 22, 93.
Singewald N, Kaehler S, Sinner C et al. 2000. Serotonin and amino acid release in the
locus coeruleus by conditioned fear and inescapable shock. 6th Internet World Con-
gress for Biomedical Sciences. Presentation #27.
Stearn W. 1998. Botanical Latin, 4th ed. Portland, OR: Timber Press.
Steele J. 1992. Anthropology of smell and scent in fragrance. In Van Toller S, Dodd G
(eds.), Fragrance: The Psychology and Biology of Perfume. London: Elsevier Applied
Science, 287-302.
Stoddart D. 1990. The Scented Ape. Cambridge, UK: Cambridge University Press, 5.
Suzuki M, Asaba K, Komatsu H et al. 1978. Autoradiographic study on percutaneous
absorption of oils useful in cosmetics. Journal of Society of Cosmetic Chemists. 29,
265-282.
Swerdlow J. 2000. Nature’s Medicine: Plants That Heal. Washington, DC: National Ge-
ographic Society.
Tisserand R. 1979. The Art of Aromatherapy. Saffron Walden, UK: CW Daniels.
Tisserand R. 1985. The Essential Oil Safety Data Manual. Brighton, UK: Tisserand
Aromatherapy Institute.
Tisserand R. 1988. Lavender beats benzodiazepines. International Journal of Aro-
matherapy. 1(2) 1-2.
Tisserand R. 1993a. Aspects of aromatherapy. In Aroma 93 Conference Proceedings.
Brighton, UK: Aromatherapy Publications, 1-9.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone, 30.
Torii S, Fukuda H, Kanemoto H et al. 1991. Contingent negative variation and the psy-
chological effects of odor. In Van Toller S, Dodd G (eds.), Perfumery: The Psychology
and Biology of Fragrance. London: Chapman and Hall, 107-118.
Tschanz D.1997. The Arab Roots of European Medicine. Aramco World. May/June
20-31.
Valnet J. 1937. Aromatherapie: Les huiles essentielles hormones vegetales. Paris: Girardot.
Valnet J.1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Van Toller S, Hotson S, Kendal-Reed M. 1992. The brain and the sense of smell. In Van
Toller S, Dodd G (eds.), Fragrance: The Psychology and Biology of Perfume. Lon-
don: Elsevier Applied Science, 195-217.
Van Toller S, Dodd G. 1991. Preface. In Van Toller S, Dodd G (eds.), Perfumery: The
Psychology and Biology of Fragrance. London: Chapman and Hall, xii-xv.
Vellmair D, Byrne M, Hotchkiss S et al. 1998. An experimental study of the dermal pen-
etration of aerosol particles. Journal of Aerosol Sciences. 28(supplement 1) 297-298.
Walter R, Cooper R, Aldridge V et al. 1964. Contingent negative variation: an electric
sign of sensorimotor association and expectancy in the human brain. Nature. 203,
380-384.
36 Section I Overview

Watson L. 2000. Jacobson’s Organ. New York: Norton.
Watt M. 1991. Plant Aromatics. Witham, UK: Watt.
Watts G. 1975. Dynamic Neuroscience: Its Application to Brain Disorders. New York:
Harper and Row.
Weiss S. 1979. The language of touch. Nursing Research. 28, 76-79.
Williams D. 1996. The Chemistry of Essential Oils. Weymouth, Dorset, England:
Michelle Press.
Zatz J. 1993. Factors affecting sorption of topically applied substances. In Zatz J (ed.),
Skin Permeation: Fundamentals and Applications. Wheaton, IL: Allured Publishing,
11-32.
Zatz J. 1993a. Modification of skin permeation by solvents. In Zatz J (ed.), Skin Perme-
ation: Fundamentals and Applications. Wheaton, IL: Allured Publishing, 127-162.
Zetzer L, Regalado M, Nichter L et al. 1991. Iontophoresis versus subcutaneous injec-
tion: a comparison of two methods of local anesthesia delivery in children. Pain.
44(91) 73.
Chapter 2 The Nature of Aromatherapy 37

W
38
3
Basic Plant Taxonomy,
Chemistry, Extraction,
Biosynthesis, and Analysis
The problem with wonder drugs is that they breed in the public mind a sense that
medicine can and always should work miracles, even with benign problems. What
gets forgotten is the price we always pay by tampering so totally with Mother
Nature
McTaggart (1996)
L
earning how and why a plant manufactures an essential oil is relevant to
understanding aromatherapy. The way plants make essential oils gives
some insight into their complexity. Traditionally, biochemists have stud-
ied primary metabolism and organic chemists have studied secondary metabo-
lism. In aromatherapy, it is of interest to have an overall picture of both meta-
bolic processes. Why some plants make essential oils is the subject of ongoing
scientific debate and is relevant to the therapeutic potential of the essential oil in
humans.
The process of extraction clarifies the need for unadulterated essential oils.
Unadulterated essential oils are required for clinical use, and the process of steam
distillation or expression can produce an essential oil with no residue. However,
there are new and exciting methods of obtaining extracts that may become part
of aromatherapy in the future. How essential oils are absorbed into the body is a
subject of heated discussion and is a topic I attempt to cover. There is no doubt
that new evidence will emerge after this book is published.
I am very appreciative of the help and advice given by the expert reviewers of
this section: James Duke, PhD; Howard Freund, PhD; Bob and Rhi Harris; Tom
Numark; Keith Shawe, PhD; and Neal Schultz, MD. I am also appreciative of the
published work of John Mann, PhD.

Part I: Basic Plant Taxonomy and Chemistry
The lovesick, the betrayed and the jealous all smell alike.
Colette
T
he Latin names of plants can seem a bit intimidating initially, but they are
the best way to be sure of what is in that bottle of essential oil, and they
are recognized the world over, from China to Peru. Latin has been used
for thousands of years in botany and was first used in this context by Pliny in
23
AD. However, it was Carl Linnaeus (1707-1778) who established the basis for
naming plants in Latin (Stearn 1998).
A plant only has one Latin name, but it may have many common names, and
those common names may also be used for completely different plants. Take for
example bergamot. In aromatherapy, bergamot refers to the oil extracted from
the peel of the citrus fruit, Citrus bergamia. This should not be confused with the
medicinal plant Monarda didyma, which is also known as bergamot. Similarly,
the word geranium refers to the species geranium for gardeners, but in the world
of aromatherapy it refers to Pelargonium graveolens.
Every plant has a unique name in Latin composed of two words. The first
word is the name of the genus, and the second is the name of the species—rather
like our first name and surname. Classification of plants is called taxonomy. All
plants can be grouped into categories. For plants to be properly identified they are
divided into division, class, order, family, genus, and species. This process takes
into account the number, shape, and position of leaves on the stem; the shape and
position of the flowers; the number and shape of the petals; whether the plant is
hairy, prickly, or smooth; whether the stem is ridged; and so on.
Life on earth began about 4 billion years ago with a single-celled organism that
did not have a nucleus. Many of these basic organisms, including algae and bacteria,
are still living in our world today. Through gradual evolution a vast range of aromatic
plants evolved that presently produces 30,000 known volatile oils (Elpel 1998).
Lavender
Lavender belongs to a plant family called Lamiaceae or Labiatae: the mint fam-
ily. This family includes many species used in aromatherapy. Plants in this family
usually have five united petals with two lobes on the top and three on the bottom
forming lips (labia). The leaves are usually directly opposite each other on the
stem, and often the stem is square. The Latin name for the lavender genus is
Lavandula. The most commonly used lavender is a hybrid, lavandin, which is a
widely used cross between two Lavandula species: L. angustifolia and L. latifolia.
Chapter 3 Basic Plant Taxonomy 39

There is also another species of lavender, L. stoechas, which can be used clinically.
See Table 3-1. However, as frequently happens in the plant kingdom, two of the
species also have other names. Lavandula angustifolia is sometimes called L. vera
or L. officinalis, although the correct name is L. angustifolia (Lawrence 1989). This
plant also has several common names: English lavender, French lavender, and true
lavender. Lavandula latifolia is sometimes called L. spica, and its common name
is spike lavender or spike. Spike is completely different from spikenard (Nar-
dostachys jatamansi), which is closely related to valerian and belongs to the family
Valerianaceae.
Lavandula angustifolia and Lavandula latifolia were listed in the British Phar-
macopoeia and supplied to hospitals in vats labeled simply “lavender.” However,
the two plants have very different therapeutic properties. L. angustifolia is a seda-
tive, relaxant, and hypotensor. L. latifolia is a stimulant and expectorant.
Chamomile
Chamomile can cause confusion to the newcomer, too. There are three main types
of chamomile used in aromatherapy: German, Roman, and Moroccan (Table
3-2). They are quite different and produce different-colored essential oils that
40 Section I Overview
Table 3-1 h Lavenders and Some of Their Properties
Latin Name Common Name Properties
Lavandula angustifolia True lavender Calming, sedative, good for
Lavandula vera burns, analgesic, antibacterial,
Lavandula officinalis immune-system enhancer
Lavandula latifolia Spike lavender Expectorant, mycolytic,
Lavandula spica possible stimulant
Lavandula stoechas Stoechas Useful against Pseudomonas
spp., high in ketones
Table 3-2 h Chamomiles and Some of Their Properties
Latin Name Common Name Properties
Matricaria recutita German chamomile Dark blue, useful for skin
complaints and inflammation
Chamaemelum nobile Roman chamomile Pale blue or yellow, sedative,
useful for spasms
Ormenis mixta Moroccan chamomile Mainly used by perfume in-
dustry, some antibacterial
activity

have different properties, but they all belong to the same family: Asteraceae or
Compositae—the daisy family.
German chamomile (Matricaria recutita) is a smoky smelling, dark-blue oil
that contains chamazulene. The oil’s color depends directly on the amount of
chamazulene present and the method of extraction. It should be noted that
chamazulene is not present in the fresh flower (or in its CO
2
extract) but is pro-
duced during distillation (Lawless 1992). It is possible to obtain a green or yellow
German chamomile oil that has less than 3% chamazulene, but the dark-blue va-
riety always has more than 7% (Svab & Sarkany 1975). The price of German
chamomile oil is usually related to the amount of chamazulene it contains.
Chamazulene is an antiinflammatory with a history of use in the treatment
of skin problems (Jakovlev et al 1983). German chamomile also contains a sec-
ond antiinflammatory compound called alpha-bisabolol, which is a monoterpenol
(Carle & Gomaa 1992). In addition, this species has antibiotic properties and is
effective against Staphylococcus aureus, hemolytic Streptococcus, and Proteus vul-
garis. Valnet, a French MD, claims that wound infections bathed with a solution
of 1 part German chamomile in 100,000 parts water have been healed (Valnet
1990). German chamomile is also thought to “stimulate liver regeneration and
subcutaneous treatments will initiate formation of new liver tissue”(Rose 1992).
CO
2
-extracted German chamomile is brown and almost solid at room tempera-
ture. It smells of sweet apples with an earthy undertone.
Roman chamomile (Chamaemelum nobile) is a colorless to pale blue oil that
turns yellow with storage. Listed in the British Herbal Pharmacopoeia, it contains
up to 80% esters. Esters have antispasmodic properties, and essential oil of Ro-
man chamomile is traditionally used as an antispasmodic and relaxant whereas
the herb is used as a carminative. Roman chamomile also has mild antiinflam-
matory properties (Franchomme & Penoel 1990), particularly if the oil is col-
lected from white-headed flowers instead of the classic yellow-headed flowers
(Rossi et al 1988).
Moroccan chamomile (Ormenis multicaulis or O. mixta) is a relative new-
comer to the aromatherapy field and is mainly used in the perfume industry. Lit-
tle is known about its clinical effects. In all respects it is different from the other
chamomiles and cannot be regarded as a substitute for either of them.
Different Parts
Occasionally, different parts of the same plant can produce different essential oils.
In the case of the bitter orange plant (Citrus x aurantium var. amara), three dif-
ferent types of essential oils can be obtained: Petitgrain from the stems and leaves,
Neroli from the petals, and bitter orange from the fruit. Neroli and petitgrain-
type essential oils can also be obtained from other citrus species. Bergamot es-
sential oil is obtained from the rind of a fruit that is a subspecies of the bitter-
sweet orange. The shorthand for Citrus aurantium subspp. bergamia (bergamot) is
Citrus bergamia (Guenther 1976).
Chapter 3 Basic Plant Taxonomy 41

Sometimes just the part of the plant is listed (for example, cinnamon bark or
cinnamon leaf ). Cinnamon bark contains approximately 50% eugenol (a phenol).
Cinnamon leaf contains 80 to 96% eugenol. Eugenol is strongly antimicrobial; it
can inhibit bacterial growth on food for 30 days (Moleyar & Narasimham 1992).
However, it is also dermacaustic and can dissolve metal, false teeth, and pearls
(Ryman 1991). Small amounts of cinnamon bark and cinnamon leaf are used by
the fragrance and pharmaceutical industries. Cinnamon is also one of the flavo-
rants of Coca-Cola (Lawless 1992).
Clones and Chemotypes
To complicate the situation still further, some plants have been cloned or culti-
vated to produce different chemotypes (Table 3-3). This means the essential oil
has a specific chemical profile that might make it more suitable for treating a par-
ticular ailment or safer to use. Common thyme (Thymus vulgaris) has several
chemotypes: linalol, geraniol, a-terpineol, thujanol-4, carvacrol, and thymol
(Vernet & Gouyon 1976). The first four are all safe to use on the skin, because
they are high in alcohols. However, thymol and carvacrol are phenols and can
cause skin irritation. Red thyme, which commonly grows in garden lawns, is a
phenol type.
Tea tree, eucalyptus, rosemary, and German chamomile are other essential
oils that have commercial chemotypes. Chemotypes will become more com-
mon as aromatic plants are grown on a more global level as cash crops (Franz
1993).
42 Section I Overview
Table 3-3 h Some Examples of Essential Oil Chemotypes
Latin Name Chemical Constituents Research Paper
Achillea millifolium Caryophyllene, farnasene, Hethelyi et al 1988
azulene-free Oswiecimska 1974
Artemesia dracunculus Methyl chavicol, sabinene Tucker & Maciarello
1987
Ocimum basilicum Linalool, methyl chavicol, Sobti et al 1978
eugenol
Matricaria recutita Bisabolone oxide, Frantz 1993
bisabolol, chamazulene,
chamazulene-free
Salvia officinalis - & -thujone, cineole, Tucker & Maciarello
thujone-free 1990

Chemistry of Essential Oils*
The chemical components that make up essential oils are produced during the
second stage of biosynthesis and are called secondary metabolites (Fig. 3-1). Ter-
penes make up the largest group of secondary metabolites with some 1000
monoterpenes and 3000 sesquiterpenes known (Harborne 1988). However, the
Chapter 3 Basic Plant Taxonomy 43
*I was greatly helped with revising this section by the following books: The Chemistry of Essential Oils
(Williams 1996), The Basic Chemistry of Aromatherapeutic Essential Oils (Bowles 2000), and Volatile Oil
Crops (Hay & Waterman 1993). These books are highly recommended for additional reading.
phenylalanine
NH
2
COOH
apiole
MeO
O
O
OMe
PA L
COOH
cinnamic acid
chavicol
HO
estragole
MeO
anethole
MeO
Figure 3-1 Biosynthesis of phenylpropanes. (Adapted from Waterman P. 1993. The Chem-
istry of volatile oils. In Hay R, Waterman P (eds.), Volatile Oil Crops: Their Biology, Biochemistry
and Production. Essex, UK: Longman Scientific and Technical, 47-61.)

number of phenylpropanes (which contain benzene rings) is much smaller—
approximately 50. Terpenes arise from the mevalonic pathway. Phenylpropanes
come from the shikimic pathway.
Mevalonic Pathway
This pathway depends on mevalonic acid, a chemical intermediate containing six
carbon atoms made by the plant and vital to its life (Waterman 1993). The plant
converts mevalonic acid to a 5-carbon structure (with the isoprene arrangement)
typical of all terpenes. This is then converted to geranyl pyrophosphate (GPP)—
the first recognizable 10-carbon molecule. This process can continue with an-
other enzyme catalyst to result in the first 15-carbon molecule, sesquiterpene
compound, farnesyl pyrophosphate (FPP). Once the plant has formed GPP, the
substance can be converted into alcohols or aldehydes.
Shikimic Pathway
This pathway utilizes an enzyme called phenylalanine ammonia lyase (PAL) to
produce phenolic compounds that include benzene rings (Waterman 1993). This
pathway also produces alkaloids such as morphine.
Terpenes, Isoprene Units
Terpenes make up the largest single class of compounds, although phenyl-
propenes tend to have the largest impact on the aroma (Waterman 1993). Ter-
penes found in essential oils are made up of the isoprene units (building blocks)
referred to previously. Each isoprene unit contains 5 carbon atoms, and some peo-
ple believe the shape resembles the skeletal profile of a dog in flight (Table 3-4)
(Williams 1996). One of the carbon atoms is attached by a double bond.
Monoterpenes have two isoprene units, sesquiterpenes have three, and diterpenes
have four. Because each isoprene unit has five carbon atoms, it is simple math to
work out the number of carbon atoms per molecule (Table 3-5).
Monoterpenes make up the largest number of terpenes and can be subdivided
into groups that indicate their structure. All terpenes end in -ene. They are light
molecules and evaporate quickly. Monoterpenes are often referred to as top notes.
They oxidize easily and combine with oxygen over time to become alcohols.
In aromatherapy, the term terpenoid is given to terpene molecules that in-
clude oxygen (Tisserand & Balacs 1995). Terpenoid is not a chemical term in a
44 Section I Overview
Table 3-4 h Structure of Terpenes
Molecular Structure Name Chemical Constituent
Chain, no ring acyclic -myrcene
One ring cyclic -limonene
Two rings bicyclic

strict sense, but it can be useful to distinguish between molecules that do not have
oxygen and those that do. All terpenes have antiseptic properties (Table 3-6).
Camphene, phellandrene, pinene, myrcene, and limonene are common examples
of monoterpenes. Limonene is thought to be antitumoral (Zheng et al 1992;
Gould 1997) and occurs in most citrus oils and in dill (Anethum graveolens).
Myrcene, found in lemongrass (Cymbopogon citratus), has analgesic properties
(Lorenzetti et al 1991)). Monoterpenes in general have a stimulating effect, but
they can become skin-sensitizing if used over time. Because they are insoluble in
water, the perfume industry frequently removes terpenes from an essential oil so
the oil can be used in toilet water. In this case the essential oil is said to be “ter-
peneless” (Guenther 1972).
Sesquiterpenes are less volatile but because they are larger structures, they
have a greater potential for stereochemical diversity (Waterman 1993). Sesquiter-
penes have stronger odors, are antiinflammatory and have bactericidal properties
(Table 3-7). As terpenes, they still oxidize over time into alcohols. In patchouli
Chapter 3 Basic Plant Taxonomy 45
Table 3-6 h Some Terpenes and Their Properties
-limonene found in many Antitumoral (Gould 1997)
citrus peel oils (60-90%) May dissolve gall stones (Igimi
et al 1991)
Myrcene found in Analgesic (Lorenzetti et al 1991)
Cymbopogon citratus,
Juniperus communis
Table 3-5 h Number of Carbon Atoms in Terpenes
Number of Number of
Chemical Constituent Isoprene Units Carbon Atoms
Monoterpene 2 isoprene units 10 carbon atoms
Sesquiterpene 3 isoprene units 15 carbon atoms
Diterpene 4 isoprene units 20 carbon atoms

oil this oxidation is thought to improve the odor. Chamazulene actually has 14
carbon atoms but is often included with sesquiterpenes. Chamazulene and
caryophyllene have antitumor activity (Mills 1991). Chamazulene is found in
German chamomile, bisabolene is found in black pepper, and caryophyllene is
found in ylang ylang (Cananga odorata).
The very few diterpenes found in essential oils tend to oxidize into alcohols.
This process produces sclareol in clary sage and viridiflorol in niaouli. However,
diterpenes may occur in solvent extracts. Taxol is a diterpene (Lewinsohn 2001).
Alcohols
Terpenic alcohols are found in many essential oils. Their names all end in -ol.
Structurally, they have a hydroxyl group attached to one of their carbon atoms
(Table 3-8). Monoterpenic alcohols (monoterpenols) are thought to be good an-
tiseptics with some antibacterial and antifungal properties. Isoborneol inhibits the
herpes virus (Armaka et al 1999). Some alcohols, such as terpinen-4-ol, are up-
lifting; others like linalool are thought to be sedatives. Usually essential oils with
a high percentage of monoterpenols are safe to use undiluted on the skin. Exam-
ples include geraniol in palmarosa (Cymbopogon martini) and citronellol in Euca-
lyptus citriodora (Lewis Walter & Elvin-Lewis Memory 1977). Isoborneol has an-
tiviral properties and is a potent inhibitor of herpes simplex virus type (Amarka
et al. 1999). Perillyl alcohol has been shown to regress pancreatic, mammary, and
liver tumors in animal studies and to revert tumor cells to a differentiated state
(Belanger 1998). However, in human studies, oral doses did not regress these tu-
mors. There have been no studies to date on topically applied or inhaled perillyl
alcohol that I could find.
Sesquiterpenols have 15 carbon atoms and a variety of therapeutic effects
(Table 3-9). When -eudesmol was injected directly into the spinal cords of rats,
it significantly reduced edematous effusion following brain injury (Asakura et al
46 Section I Overview
Table 3-7 h Some Sesquiterpenes and Their Properties
Chamazulene found in Antiinflammatory (Safayhi
Matricaria recutita et al 1994)
Sedative (Yamada et al 1996)
-caryophyllene found in Antiinflammatory
Cananga odorata (Tambe et al 1996)

Table 3-8 h Some Alcohols and Their Properties
Linalool in Lavandula Sedative (Buchbauer et al 1991;
angustifolia Re et al 2000)
Antispasmodic (Lis-Balchin &
Hart 1999)
Geraniol in Cymbopogon Antifungal (Carson &
martini Riley 1995)
Potentiates antiherpetic activity
of SON (Shoji et al 1998)
Terpinen-4-ol in Melaleuca Effective against Pseudomonas
alternifolia aeruginosa (Budhiraja et al
1999; Jedlickova et al 1992)
OH
OH
OH
Table 3-9 h Some Sesquiterpenols and Their Properties
Farnesol found in Effective against Trichomonas
vaginalis (Viollon et al
1996)
Hypotensor (Luft et al 1999)
-bisabolol found in Antiinflammatory ( Jakovlev
Matricaria recutita et al 1979)
Patchoulol found in Effective against bacteria that
patchouli cablin cause foot odor (Yang et al
1996)
OH
OH
OH

2000). It also appeared to reduce potassium- and electric shock-induced seizures
(Chio et al 1997). The anticonvulsant properties of -eudesmol were compared
to phenobarbitone in another study by Santos et al (1997). -eudesmol is found
in West Indian Sandalwood (Amyris balsamifera) and Psidium guyanensis.
Nerolidol, found in Melaleuca quinquenervia (a special chemotype of niaouli),
completely inhibited development of the malaria-bearing mosquito (Lopez et al
1999). The Amazonian Waiapi tribe treat malaria by inhaling the essential oil
from the leaf of Virola surinamensis (a rainforest tree that contains nerolidol). San-
talol found in sandalwood is an effective antiviral agent against early-stage cold
sores (Benencia & Courreges 1999) and was also found to work as a sedative in
mice (Okegawa et al 1995). Sclareol kills tumor cells in vitro (Dimas et al 1999)
and is used extensively for ambergris fragrance (Bauer et al 1990).
Phenols
A phenol is a hydroxyl group attached to a benzene ring (Table 3-10). Like alco-
hols, phenol names end in -ol, but this is where the similarity ends. There are only
four common phenols found in essential oils: thymol, carvacrol, eugenol, and
chavicol. There are two ethers from phenols: one from eugenol and one from
48 Section I Overview
Table 3-10 h Some Phenols and Their Properties
Thymol found in Thymus Antibacterial (Shapiro et al 1994)
vulgaris, Lippia sidoides Effective against Cryptococcus neo
formans (Voillon & Chaumont
1994)
Eugenol found in Syzygium Sedative & vasodilator
aromaticum (clove bud) (Hume 1983)
Carvacrol found in Anticonvulsant (Santos et al 1997)
Origanum vulgare Antibacterial (Consentino et al
1999) 1999)
OH
O
OH
CH
3
OH

chavicol. Benzene (aromatic) rings can easily be formed from aliphatic (nonben-
zene) rings, but the reverse reaction rarely occurs (Guenther 1972). Phenols need
to be treated with care because many of them are skin irritants. Most have very
strong antibacterial properties, and some have a stimulatory effect on both the
nervous system and the immune system. Thymol (from Thymus vulgaris) also has
anthelmintic properties. Eugenol is a powerful antiinflammatory (Sharma et al
1994) and decreases gut motility in diarrhea. It also inhibits prostaglandin syn-
thesis (Bennett et al 1988).
Aldehydes
An aldehyde has an oxygen atom double bonded to a carbon atom at the end of
a carbon chain (Table 3-11). The fourth bond is always a hydrogen atom (Bowles
2000). Aldehydes usually end in -al and often have sedative, calming effects, as
well as being important to the aroma of the plant. Examples include citral in
lemon balm (Melissa officinalis), citronellal in lemongrass (Cymbopogon citratus),
geranial in lemon eucalyptus (Eucalyptus citriodora), and neral in lemon verbena
(Aloysia triphylla). Geranial and neral are isomers, meaning they have the same
molecular make-up but the carboxyl molecule is in a different place. For a long
time they were thought to be so similar they were combined and called citral.
Chapter 3 Basic Plant Taxonomy 49
Table 3-11 h Some Aldehydes and Their Properties
Citronellal found in Antifungal (Hmamouchi et al 1990)
Eucalyptus citriodora Antilouse (Mumcouglu et al 1996)
Neral & geranial (citral) Antibacterial (Onawunmi 1989)
in Cymbopogon citratus
Cinnamaldehyde in Selective effect against pathogenic
Cinnamomum intestinal flora (Lee & Ahn
zeylanticum 1998)
O
H
O
H
O
H

Citral has strong antiseptic and antibacterial properties (Onawunmi & Oguniana
1981). Citronellal possesses antifungal properties (Hmamouchi et al 1990).
Esters
Esters are a combination of an acid and an alcohol and take their name from the
acid and alcohol (Table 3-12). Hence, acetic acid and linalool produce Linalyl ac-
etate. Acids do not occur in essential oils but can be found in floral waters. Esters
end in –ate, and have antispasmodic and calming properties. Some are also anti-
fungal. They often smell very fruity. Examples include Linalyl acetate found in
lavender (Lavandula angustifolia), clary sage (Salvia sclarea), bergamot (Citrus au-
rantium subsp. bergamia), and genaryl acetate found in sweet marjoram (Origanum
majorana). One essential oil with a very high ester content (85%) is Roman
chamomile (Chamaemelum/Anthemis nobilis), which includes angelic and tiglic esters
(Bauer et al 1990).
Ketones
A ketone is derived from an alcohol by oxygenation and has an oxygen atom dou-
ble bonded to a carbon atom, which is also bonded to two other carbon atoms
(Table 3-13) (Bowles 2000). Ketones end in -one with a single exception: cam-
phor. This substance has no relation to the plant camphor. Ketones should always
be treated with respect because certain ketones can produce convulsant effects
(usually when taken orally). Because ketones are resistant to metabolism, they can
build up in the liver. An easy way to remember that they are a potential problem
is to think of ketosis. Potentially toxic ketones include d-pulegone (found in pen-
nyroyal), which caused the death of a 23-year-old woman in 1897. It must be
stressed that this lady did drink a tablespoonful (15 ml) of undiluted essential
oil (Allen 1897). Pennyroyal tea caused the death of two infants. A child who
50 Section I Overview
Table 3-12 h Some Esters and Their Properties
Linalyl acetate found in Sedative (Buchbauer et al 1991)
Lavandula angustifolia Topical anesthetic (Ghelardini
et al 1999)
Geranyl acetate in Stimulates bile production
Cymbopogon martini (Trabace et al 1994)
O
O
O
O
O

developed hepatic malfunction and presented with severe epileptic encephalopa-
thy was tested for pulegone; results were positive (Bakerink et al 1996). Once
again large amounts of the essential oil had been ingested.
There are some nontoxic ketones. Most of these are good for the skin and for
scars, a view supported by Lavabre (1990). Safe ketones include jasmone in jas-
mine (Jasminum officinale) (International School of Aromatherapy 1993), fen-
chone in fennel (Foeniculum vulgare var. dulce), and isomenthone in geranium
(Pelargonium graveolens). A special diketone found in everlasting (Helicrysum
italicum) has antihematoma properties and reduces contusions with great speed.
Oxides
Oxides in organic chemistry typically involve an oxygen bridge between two
neighboring carbon atoms (Table 3-14). The use of the term oxide in aromather-
apy is a little more general because the carbons are not neighbors. In chemical
terminology, an oxide is called an ether or a peroxide. However, the term ether
might be confusing because there is another group of phenolic ethers that have
different properties. An oxide has an oxygen atom in a chain of carbons, which
forms a ring (but not a benzene ring). The most common oxide is cineole—a
strong expectorant. Both 1,4-cineole and 1,8-cineole occur in essential oils
(Tisserand & Balacs 1995). Sometimes called eucalyptol, 1,8-cineole is found in
blue gum (Eucalyptus globulus), rosemary (Rosmarinus officinalis CT cineole), and
bay laurel (Lauris nobilis). Other oxides are ascaridole found in wormseed
(Chenopodium ambrosioides var. anthelminticum) and rose oxide found in geranium
(Pelargonium graveolens) and rose (Rosa damascena). The freshly baked smell
Chapter 3 Basic Plant Taxonomy 51
Table 3-13 h A Ketone and Its Properties
Menthone in Mentha piperita Inhibition of platelet aggrega-
tion in decompression sick-
ness (Murauama & Kumaroo
1986)
O
Table 3-14 h An Oxide and Its Properties
1,8 cineole found in Antiinflammatory ( Juergens et al 1998)
Eucalyptus globulus Enhances pentobarbitol effects
(Santos & Rao 2000)
Expectorant (Duke 1992)
O
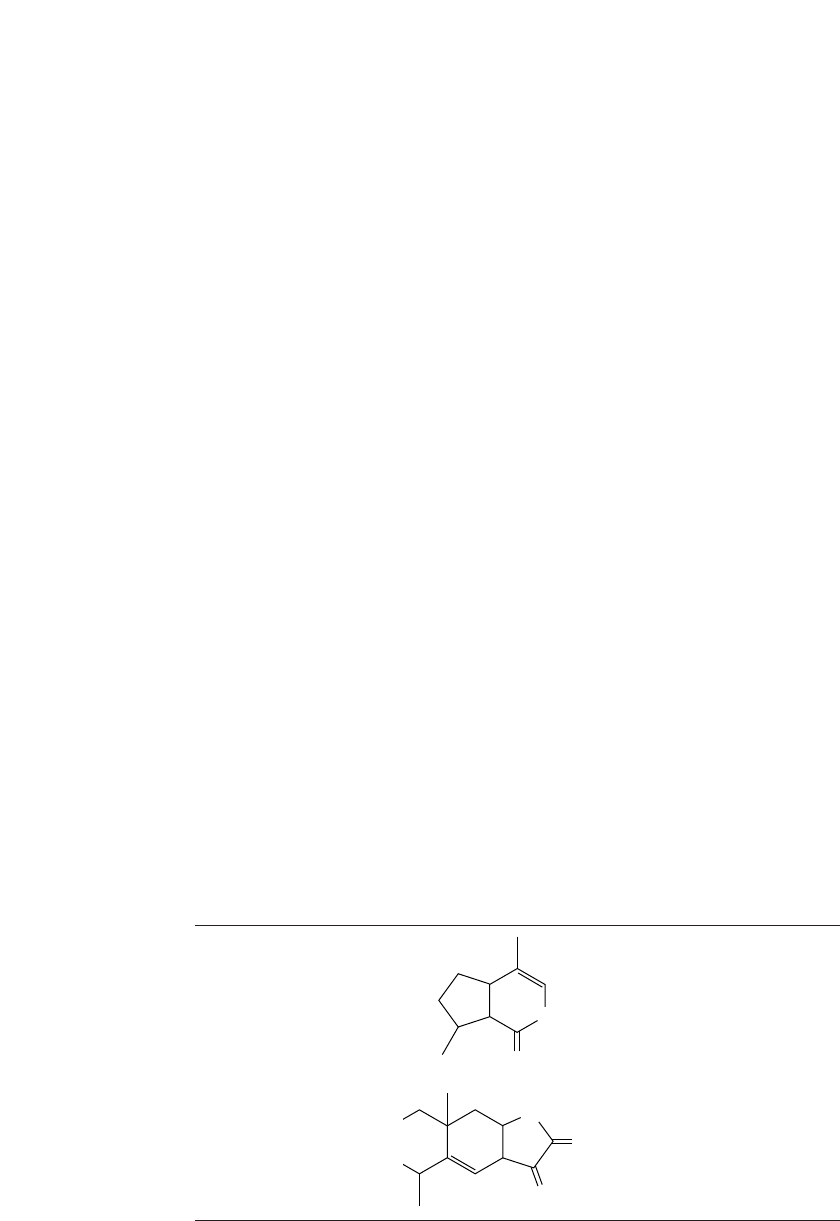
that wafts around bread counters in supermarkets is often due to an oxide called
2-furaldehyde (Bauer et al 1990).
Lactones
Lactones always have an oxygen atom double bonded to a carbon atom. The car-
bon atom is attached to another oxygen atom that is part of a closed ring (Table
3-15). Lactones are present in most expressed oils and tend to end in -lactone or
-ine. The percentage of lactones present may be low, but they play an important
role as expectorants and mucolytics. However, lactones tend to have the same
potential neurotoxic effects as ketones. Many essential oils belonging to the
Asteraceae family contain lactones that can also cause skin sensitivities (Gordon
1999).
Alantolactone is present in elecampane (Inula helenium) and is used to treat
purulent bronchitis (Rose 1994). Isolantolactone is found in sweet inule (Inula
graveolens) and is effective in treating bronchial congestion. Lactones that contain
15 carbon atoms seem to have distinctive antiinflammatory properties (Bowles
2000). Nepetalactone, found in catnip (Nepeta cataria), showed sedative and anal-
gesic effects in rats (Aydin et al 1998). A bicyclic lactone (a phthalide) is respon-
sible for the odor of celery root (Bauer et al 1990).
Coumarins
Coumarins are a type, or subgroup, of lactones. They have an oxygen atom dou-
ble-bonded to a carbon atom. That carbon atom is attached to another oxygen,
which is part of a closed ring, and they also have a benzene ring attached (Table
3-16). Coumarins usually end in -one (pronounced own), as in umbelliferone, or
with –in, as in coumarin. Coumarins may be present in small amounts, in essen-
tial oils but they are very potent. Franchomme states that coumarins augment the
antispasmodic effect of esters. Coumarins include khellin and visnagin, which are
52 Section I Overview
Table 3-15 h Some Lactones and Their Properties
Nepetalactone found in Analgesic & sedative (Aydin
Nepata caesarea (catnip) et al 1998)
Alantolactone found in Respiratory antiinflammatory
Inula graveolens (Mazor 2000)
O
O
O
O

strong vasodilators found in khella (Ammi visnaga) essential oil (Lewis Walter &
Elvin-Lewis Memory 1977). Khella is also a bronchodilator (Budavari et al
1996). Reconstituted compounds from Khella form the ingredients of the phar-
maceutical product Intal, an inhaled asthma medication (Rose 1992).
There is sometimes confusion regarding the chemical dicoumarol, which
forms the basis of warfarin, an anticoagulant drug (Mills 1991). Dicoumarol is
created naturally by the breakdown of sweet clover plant, but it is created syn-
thetically by drug companies (Budavari 1996). However, if you look at the chem-
ical drawing, you will find a coumarin group within it (see Table 3-16) (Bowles
2000), although coumarin-rich essential oils have not yet been shown to have a
measurable anticoagulant effect.
Small amounts of furanocoumarins (up to 2%) are present in citrus-peel oils
and a few other essential oils such as angelica (Angelica archangelica) root, cumin
(Cuminum cyminum), and rue (Ruta graveolens) (Tisserand & Balacs 1995). Vir-
ginian cedarwood (Juniperus virginiana) and lemon verbena (Lippia citriodora)
are also phototoxic (Price & Price 1999).
Furanocoumarins react in the presence of ultraviolet light and can have a
phototoxic effect, resulting in burns or erythema. Higher percentages are needed
to have a phototoxic effect on darker skin (Zaynoun et al 1977). A phototoxic ef-
fect was produced with a 2.4% concentration on pale skin and an average of a 15%
concentration on dark brown or black skin. On some skin the resulting pigmen-
tation can remain for life. Bergamottin, a furanocoumarin, was found to be anti-
tumoral in vitro (Miyake et al 1999).
Ethers
Ethers occur when a methyl or ethyl group is attached to a benzene ring via an
oxygen molecule (Table 3-17). Ethers are thought to be responsible for some of
the hallucinogenic properties of certain essential oils when taken orally. The hy-
pothesis is that estragole and anethole could be metabolized into 4-methoxy-
Chapter 3 Basic Plant Taxonomy 53
Table 3-16 h Structural Similarities between Coumarin and Warfarin
Coumarin Enhances antispasmodic effect of esters
(Franchomme & Penoel 1991)
Reduces lymphedema (Casley-Smith
1999)
Warfarin Anticoagulant (Budavari 1996)
O
O
O
O
OH
OH

amphetamine or the corresponding ketone (Benoni et al 1996). Unlike phenols,
ethers are not aggressive on the skin.
Apart from Chemistry
Some people believe there is more to an essential oil than the sum of its parts:
there is a synergy of all those parts working together. Many people also believe
there is an energy or vibration to an essential oil, and it may be this part that plays
the major role in healing. Some people think of essential oils as having yin- and
yang-like qualities. Oils with yanglike qualities are thought to tone the whole
body, stimulate immune growth, support the metabolic response, raise internal
temperature, and stimulate the nervous system. Oils with yinlike qualities are
thought to reduce temperature, decrease activity in the nervous system, and have
a calming effect. This process of attributing yin- and yang-like properties to es-
sential oils is key to the work of Peter Holmes (1989) and Gabriel Mojay (1996).
REFERENCES
Albert-Puleo M. 1980. Fennel and anise as estrogenic agents. Journal of Ethnopharma-
cology. 2(4) 337-344.
Allen W. 1897. Note on a case of supposed poisoning by pennyroyal. Lancet. 1:1022-1023.
Amarka M, Papanikolaou E, Sivropoulou A et al. 1999. Antiviral properties of isoborneol,
a potent inhibitor of herpes simplex virus type 1. Antiviral Research. 43(2) 79-92.
Asakura K, Matsuo Y, Oshima T et al. 2000. Omega-Agatoxin IVA sensitive Ca(2)
channel blocker, alpha-eudesmol, protects against brain injury after focal ischemia in
rats. European Journal of Pharmacology. 394(1) 57-65.
Aydin S, Beis R, Ozturk Y et al. 1998. Nepetalactone: A new opioid analgesic from
Nepeta caesarea Boiss. Journal of Pharmacy and Pharmacology. 50(7) 813-817.
Bakerink J, Gospe S, Dimand R et al. 1996. Multiple organ failure after ingestion of
pennyroyal oil from herbal tea in two infants. Pediatrics. 98(5) 944-947.
54 Section I Overview
Table 3-17 h An Ether and Its Property
Transanethole in Estrogenic activity (Albert-Puleo 1980)
Foeniculum vulgare
(fennel)
O
CH
3

Bauer K, Garbe D, Surburg H. 1990. Common Fragrance and Flavor Materials. Wein-
heim, Germany: VCH Publishing.
Belanger J. 1998. Perillyl alcohol: Applications in oncology. Alternative Medicine Re-
view. 3(6) 448-457.
Benencia F, Courreges M. 1999. Antiviral activity of sandalwood oil against herpes sim-
plex virus 1 and 2. Phytomedicine. 6(2) 119-123.
Bennett A, Stamford P, Tavares I. 1988. The biological activity of eugenol, a major con-
stituent of nutmeg (Myristica fragrans): Studies on prostaglandins, the intestine and
other tissues. Phytotherapy Research. 2:124-130.
Benoni H, Dallakian P, Taraz K. 1996. Studies of the essential oil from guarana.
Zeitschrift Lebensmittel-Untersuching und-forshung. 203(1) 95-98.
Bowles J. 2000. The Basic Chemistry of Chemotherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Printers.
Buchbauer G, Jirovetz L, Jager W et al. 1991. Aromatherapy: Evidence for sedative ef-
fects of the essential oil of lavender after inhalation. Zeitschrift fur Naturforschung.
46(11-12) 1067-1072.
Budavari, S, et al (eds.). 1996. The Merck Index, 12th ed. Whitehouse Station, NJ:
Merck & Co. Inc.
Budhiraja S, Cullum M, Sioutis S et al. 1999. Biological activity of Melaleuca alternifolia
(teatree) oil components, terpinen-4-ol in human hyelocytic cell line HL-60. Journal
of Manipulative Physiological Therapeutics. 22 (7) 47-53.
Carle R, Gomaa K. 1992. The medicinal use of Matricaria flos. British Journal of Phy-
totherapy. 2:147-153.
Carson C, Riley T. 1995. Antimicrobial activity of the major components of the essential
oil of Melaleuca alternifolia. Journal of Applied Bacteriology. 78(3) 264-269.
Casley-Smith J. 1999. Benzo-pyrones in the treatment of lymphedema. International
Journal of Angiology. 18(1) 31-41.
Chio L, Ling J, Chang C. 1997. Chinese herb constituent beta-eudesmol alleviated the
electroshock seizures in mice and electrographic seizures in rat hippocampal slices.
Neuroscience Letters. 231(1) 171-174.
Colette. 1975. “Break of Day.” Reprinted in Earthly Paradise, Robert Phelps Ed. New
York: Noonday Press.
Consentino S, Tuberoso C, Pisano B et al. 1999. In vitro antimicrobial activity and
chemical activity of Sardinian Thymus essential oils. Letters in Applied Microbiology.
29(2) 130-135.
Dimas K, Kokkinopoulos D, Demetzos C et al. 1999. The effect of schlareol on growth
and cell cycle progression of human leukemic cell lines. Leukemia Research. 23(3)
217-234.
Duke J. 1992. Handbook of Biologically Active Phytochemicals and Their Activities.
Boca Raton: CRC Press.
Elpel T. 1998. Botany in a Day. Pony, MT: Hollowtop Outdoor Primitive School, LLC.
Franchomme P, Penoel D. 1991. Aromatherapie Exactement. Limoges, France: Jollois.
Franz C. 1993. Genetics. In Hay R, Waterman P (eds.), Volatile Oil Crops: Their Biol-
ogy, Biochemistry and Production. Essex, UK: Longman Scientific and Technical,
63-96.
Ghelardini C, Galeotti N, Salvatore G et al. 1999. Local anesthetic activity of the essen-
tial oil of Lavandula angustifolia. Planta Medica. 65(8) 700-703.
Chapter 3 Basic Plant Taxonomy 55

Gordon L. 1999. Compositae dermatitis. Australasian Journal of Dermatology. 40(3)
123-128.
Gould M. 1997. Cancer chemoprevention and therapy by monoterpenes. Environmental
Health Perspectives. 105 (Suppl 4) 977-979.
Guenther E. 1972. The Essential Oils, Vol. I. Malabar, FL: Krieger.
Guenther E. 1976. The Essential Oils, Vol. III. Malaber, FL: Krieger.
Harborne J. 1988. Introduction to Ecological Biochemistry. London: Academic Press.
Hay R, Waterman P (eds.). 1993. Volatile Oil Crops: Their Biology, Biochemistry and
Production. Essex, UK: Longman Scientific and Technical.
Hethelyi E, Danos B, Tetenyi P. 1988. Investigation of the essential oils of the Achillea
genus. I. The essential oil composition of Achillea distans. Herba Hungarica. 27:35-42.
Hmamouchi M, Tantaoui EA, Es-Safi N et al. 1990. Elucidation of antibacterial and
antifungal properties of Eucalyptus essential oils. Plantes Medicale Phytotherapie.
24(4) 278-279.
Hume W. 1983. Effect of eugenol on constrictor response in blood vessels of rabbit ear.
Journal of Dental Research. 62(9) 1013-1015.
Igimi H, Tamura R, Yamamoto F et al. 1991. Medical dissolution of gallstones: Clinical
experience of d-limonene as a simple, safe and effective solvent. Digestive Diseases
and Sciences. 36(2) 200-208.
International School of Aromatherapy. 1993. A Safety Guide on the Use of Essential
Oils. London: Nature By Nature Oils.
Jakovlev V, Isaac O, Thiener K et al. 1979. Pharmacological investigations with com-
pounds of chamomile: New investigations on the antiphlogistic effects of (-)a-bis-
abolol and bisabolol oxides. Planta Medica. 35:125-140.
Jakovlev V, Isaac C, Flaskamp E. 1983. Pharmacological investigations with compounds
of chamomile. VI. Investigations on the antiphlogistic effects of chamazulene and ma-
tricin. Planta Medica. 49(2) 67-73.
Jedlickova Z, Mottl O, Sery V. 1992. Antibacterial properties of the Vietnamese Cajeput
oil and Ocimum oil in combination with antibacterial agents. Journal of Hygiene,
Epidemiology, Microbiology, and Immunology. 36(3) 303-309.
Juergens U, Stober M, Schmidt-Schilling L et al. 1998. Anti-inflammatory effects of eu-
calyptol (1,8-cineole) in bronchial asthma: inhibition of arachidonic acid metabolism
in human blood monocytes ex vivo. European Journal of Medical Research. 3(9)
407-412.
Lavabre M. 1990. Aromatherapy Workbook. Vermont: Healing Arts Press.
Lawless J. 1992. Encyclopedia of Essential Oils. Shaftesbury, UK: Element Books.
Lawrence B. 1989. Essential Oils: 1981-1987. Wheaton, IL: Allured Publishing.
Lee HS, Ahn YJ. 1998. Growth-inhibiting effects of Cinnamomum cassia bark-derived
materials on human intestinal bacteria. Journal of Agriculture, Food, and Chemistry.
46:8-12.
Lewinsohn E. 2001. The biosynthesis of essential oils. Notes from Essential Oils
Course, Rutgers University. August 12-16.
Lewis Walter H, Elvin-Lewis Memory R. 1977. Medical Botany. New York: John Wiley.
Lis-Balchin M, Hart S. 1999. Studies on the mode of action of the essential oil of laven-
der (Lavandula angustifolia). Physiotherapy Research 13(6) 540-542.
Lopez N, Kato M, Andrade E et al. 1999. Antimalarial use of volatile oil from the leaves
of Virola surinamensis by Waiapi Amazon Indians. Journal of Ethnopharmacology.
67(3) 313-319.
56 Section I Overview

Lorenzetti, Souza G, Sarti S et al. 1991. Myrcene mimics the peripheral analgesic activ-
ity of lemongrass tea. Journal of Ethnopharmacology. 34(1) 43-48.
Luft U, Bychkov R, Gollasch M et al. 1999. Farnseol blocks the L-types Ca2 channel
by targeting the alpha 1C subunit. Arteriosclerosis, Thrombosis & Vascular Biology.
19(4) 959-966.
Miyake Y, Murakami A, Sugiyama Y et al. 1999. Identification of coumarins from lemon
fruit (Citrus limon) as inhibitors of in vitro tumor promotion. Journal of Agriculture
and Food Chemistry. 47(8) 3151-3157.
Mills S. 1991. Out of the Earth. London: Viking Arkana, 295.
Moleyar V, Narasimham P. 1992. Antibacterial activity of essential oil components. In-
ternational Journal of Food Microbiology. 16:337-342.
Mumcuoglu K, Galun R, Bach U et al. 1996. Repellency of essential oils and their com-
ponents to the human body louse, Pediculus humanus. Entomologia Experimentale et
Applicata. 78(3) 309-314.
Okegawa H, Ueda R, Matsumoto K et al. 1995. Effect of a-santalol and b-santalol from
sandalwood on the central nervous system of rats. Phytomedicine. 2(2) 119-126.
Onawunmi G, Oguniana E. 1981. Antibacterial constituents in the essential oil of Cym-
bopogon citratus. Ethnopharmacology. 24:64-68.
Onawunmi G. 1989. Evaluation of the antimicrobial activity of citral. Letters in Applied
Microbiology. 9:105-108.
Oswiecimska M. 1974. Korrelation zwischen Chromosomenzahl und Prochamazulenen
in Achillea von osteuropa. Translated. Correlation between number of chromatosomes
and prochamazulene in Easteurapean Achillea. Planta Medica. 25(4) 389-395.
Price S, Price L. 1999. Aromatherapy for Health Professionals, 2nd ed. London:
Churchill Livingstone, 51.
Re L, Barocci S, Sonnino S et al. 2000. Linalool modifies the nicotinic receptor-ion
channel kinetics at the mouse neuromuscular junction. Pharmacological Research.
42(2) 177-182.
Rose J. 1992. The Aromatherapy Book. San Francisco: North Atlantic Books.
Rose J. 1994. Guide to Essential Oils. San Francisco: Jeanne Rose Aromatherapy.
Rossi T, Melegari M, Bianchi A et al. 1988. Sedative, anti-inflammatory and anti-
diuretic effects induced in rats by essential oils of varieties of Anthemis nobilis: a com-
parative study. Pharmacological Research Communications. 20(Suppl 5) 71-74.
Ryman D. 1991. Aromatherapy. London: Piatkus.
Safayhi H, Sabieraj J, Sailer E et al. 1994. Chamazulene an antioxidant type inhibitor of
leukotriene B4 formation. Planta Medica 60(5) 410-413.
Santos F, Rao V, Silveira E. 1997. The leaf essential oil of Psidium guyanensis offers pro-
tection against pentylenetetrazole-induced seizures. Planta Medica. 63:133-135.
Santos F, Rao V. 2000. Anti-inflammatory and antinociceptive effects of 1,8 cineole, a
terpenoid oxide present in many plant essential oils. Physiotherapy Research. 14(4)
240-241.
Shapiro S, Meir A, Guggenheim B. 1994.The antimicrobial activity of essential oil com-
ponents towards oral bacteria. Oral Microbiology and Immunology. 9:202-208.
Sharma J, Srivastava K, Gan E. 1994. Suppressive effects of eugenol and ginger oil on
arthritic rats. Pharmacology. 49:314-318.
Shoji Y, Ishige H, Tamura N et al. 1998. Enhancement of anti-herpetic activity of anti-
sense phosphorothioate oligonucleotides 5 with geraniol. Journal of Drug Targeting.
5(4) 261-273.
Chapter 3 Basic Plant Taxonomy 57

Sobti S, Pushpangadan P, Thapa R et al. 1978. Chemical and genetic investigations in
essential oils of some Ocimum species, their FI hybrids and synthesized allopoly-
ploids. Lloydia 4:50-55.
Stearn W. 1998. Botanical Latin, 4th ed. Portland, OR: Timber Press.
Svab J, El-Din-Awaad C, Fahmy T. 1967. The influence of highly different ecological
effects on the volatile oil content and composition in the chamomile. Herba Hungar-
ica. 6(2) 177-188.
Tambe Y, Ysujiuchi H, Honda G et al. 1996. Gastric cytoprotection of the non-steroidal
anti-inflammatory sesquiterpene, beta-carylophyllene. Planta Medica. 62(5)
469-470.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Trabace L, Avato P, Nazzoccoli M et al. 1994. Choleretic activity of Phapsia Chem 1,
11, 111 in rats: Comparison with terpenoid constituents and peppermint oil. Phy-
totherapy Research. 8(5) 305-307.
Tucker A, Maciarello M. 1987. Plant identification. In Simon J, Grant L (eds.), Pro-
ceedings of the First National Herb Growing and Marketing Conference. West
Lafayette, IN: Purdue University Press, 341-372.
Tucker A, Maciarello M. 1990. Essential oils of cultivars of Dalmation sage (Salvia offic-
inalis). Journal of Essential Oil Research. 2:139-144.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Vernet P, Gouyon D. 1976. Le polymorphisme chimique de Thymus vulgaris. Parfums,
Cosmetiques, Aromes. 30:31-45.
Viollon C, Mandin D, Chaumont J. 1996. Antagonistic activities, in vitro, of some es-
sential oils and natural volatile compounds in relation to the growth of Trichomonas
vaginalis. Fitoterapia. 67(3) 279-281.
Waterman P. 1993. The chemistry of volatile oils. In Hay R, Waterman P (eds.), Volatile
Oil Crops: Their Biology, Biochemistry and Production. Essex, UK: Longman Scien-
tific and Technical, 47-61.
Williams D. 1996. The Chemistry of Essential Oils. Dorset, UK: Michelle Press, 40.
Yamada K, Miura T, Mimaki Y et al. 1996. Effect of inhalation of chamomile oil vapor
on plasma ACTH level in ovariectomized rat under restriction stress. Biological &
Pharmaceutical Bulletin. 19(9) 1244-1246.
Yang D, Michel D, Mandin D et al. 1996. Antifungal and antibacterial properties in
vitro of three Patchouli essential oils from different origins. Acta Botanica Gallica.
143(1) 29-35.
Zaynoun S, Johnson B, Frain-Bell W. 1977. A study of bergamot and its importance as a
phototoxic agent. Contact Dermatitis. 3:225-239.
Zheng GQ, Kenney P, Luke T. 1992. Anethofuran, carvone and limonene: potential can-
cer chemopreventive agents from dill weed oil and caraway oil. Planta Medica. 58:
338-341.
58 Section I Overview

Part II: Extraction, Biosynthesis, and Analysis
“It looked totally innocent, like a light tea—and yet contained, in addition
to the four-fifths alcohol, one fifth of a mysterious mixture that could set
a whole city trembling with excitement.”
Suskind P. 1986.
Perfume: The Story of a Murderer. London: Penguin Books, 62.
Essential Oils and Extracts from Aromatic Plants
There are several ways of extracting the volatile components from plants. Some
methods produce essential oils, and other methods produce extracts rather than
essential oils. See Figure 3-2 and Table 3-18 for comparisons of the extraction
procedures used for aromatic extracts and essential oils. Traditionally aromather-
apy has specified the use of essential oils, but some other methods of extraction
and the products they yield are becoming more acceptable.
Extraction of Essential Oils
Essential oils are either distilled or expressed (Arctander 1960). Distillation can
mean water distillation, water-and-steam distillation, steam distillation, or steam-
and-vacuum distillation (Arctander 1960).
Water distillation
Material from the plant is in direct contact with boiling water. Arctander (1960)
suggests that such direct heating methods may produce a burnt note to the es-
sential oil. Most water distillation stills have a grid. This protects the plant mate-
rial from the heating elements, and the process is similar to that of water-and-
steam distillation.
Water-and-steam distillation
In water-and-steam distillation, steam is blown into the mixture of water and
plant material.
Steam distillation
This method formerly involved a copper still, but now the still is more likely to
be made of stainless steel. The aromatic plant material is placed on a grid through
which steam passes, usually at a temperature not above 100°C (Bowles 2000). See
Chapter 3 Basic Plant Taxonomy 59

60 Section I Overview
Extracts vs. essential oils
Essential oils
obtained by
Aromatic extracts
obtained by
Distillation Expression
Distilled
essential oils
Citrus peel oils
Maceration with alcohol
Tinctures
Solvent extraction Enfleurage
Pomades
Enfleurage
absolutes
Concretes Resinoids
Absolutes
Figure 3-2 Extracts vs. essential oils. Adapted from Williams D. 1989. Lecture Notes on
Essential Oils. With kind permission of Eve Taylor, London.
Table 3-18 h Advantages and Disadvantages of Various
Extraction Processes
Extraction Process Advantages Disadvantages
Distillation Economical Changing constituents
Large quantities can be Depending on time/temp
processed
Simple apparatus
Little labor needed
Expression No heat required Some flavoring left
Simple apparatus Only citrus peel oils
Oxidize quickly
Enfleurage Low temperature needed Time consuming
Possible problem with Labor intensive
solvent
CO
2
extraction Constant product Expensive
No heat used
Solvent extraction Constant product Solvent residues

Fig. 3-3 for more details.The water boils at temperatures between 88
o
C and 930
o
C depending on the altitude at the distillation site. Altitude can be particularly
relevant when essential oils are distilled locally. A decrease in boiling point has
significant influence on the hydrolytic effect of the steam on the essential oil
(Arctander 1960).
Most American or European stills use high-pressure steam. This is the
fastest way of distilling essential oils with high-boiling constituents such as ve-
tiver, sandalwood, and clove. The steam loosens the volatile nonpolar constituents
of the plant and they pass, with the steam, into a condenser that cools the mix-
ture. Steam also alters some of the components within an essential oil, for exam-
ple turning matricin to chamazulene. Some of the polar components from the
plant dissolve in the water producing floral water. The mixture of floral water and
essential oil come out together, but as essential oils and floral water do not mix,
they quickly separate. The majority of essential oils float above the floral water,
but some sink, depending on their specific gravity.
Chapter 3 Basic Plant Taxonomy 61
Steam
Insulation Grid
Aromatic
water
Essential
oil
Cooling
water
Cooling
coil
Steam and
volatile oil
Plant material
Figure 3-3 Steam distillation. Reproduced from Price S. 1983. Practical Aromatherapy, with
the kind permission of Harper Collins, London.
The degree of heat and the amount of time are vital parts of the distillation
process as some components of plants are very sensitive to heat and others take
much longer to distill (Guenther 1974). The distillation process for Lavandula
angustifolia is approximately one hour, but it is considerably longer for sandal-
wood or vetiver. The length of the distillation process will affect the chemical
composition of the essential oil (Guenther 1976). Steam distillation is suitable for
the highly volatile components such as the terpenes. The heavier the molecule
(sesquiterpenoids), the longer the process will take. Until fairly recently the side
product, the floral water (otherwise called hydrolat) was thrown away, but now,
hydrolats (or hydrosols) are becoming known for their own therapeutic actions,
especially for babies, children, and the elderly.
Steam-and-vacuum distillation
This method uses steam distillation with partial vacuum (Arctander 1960). The
pressure used is typically 100-200 mmHg. The advantage of this method is the
speed with which the essential oil is extracted. The disadvantage is that a very ef-
fective and fast method of cooling is required.
Portable distillation Portable distillation equipment is simple to make and can
be used for small quantities of plants when essential oils must be distilled on
site (Alkaire & Simon 1992). Otherwise, small cooker-top stills can be pur-
chased for home use.
Subdivisions of steam distillation
Cohobation means the water used in the distillation process is reused many times
(Guenther 1974).
Fractional distillation means the essential oil is distilled at specific temperatures
for specific lengths of time to collect different factions (or functional groups)
within the essential oil. For example, peppermint contains terpenes that be-
come volatile at approximately 150° C and menthone and menthol that boil
at 200°-230° C (Guenther 1974).
Rectification aims to separate the volatile and nonvolatile components of an es-
sential oil. If an essential oil is thought to contain impurities, it can be purified
by redistillation.This process is called rectification. Sometimes peppermint and
caraway seed oils can take on an unpleasant odor if they have been in contact
with the wall of a hot still. This aroma can be removed through rectification
(Guenther 1974). To give some idea of yield, 200 kg of Lavandula angustifolia
flowers will produce 1 kg of essential oil. However, between 2 and 5 metric tons
of rose petals are needed to produce the same amount of rose oil.
Expression
Only involves the peel of citrus plants such as grapefruit. The peel of the fruit is
racked or abraded by mechanical scrapers, and the essence collected by centrifugal
separation. Sometimes the whole fruit is crushed prior to the essential oil being
separated from the juice and peel. Expressed oils will naturally contain a propor-
tion of waxes and other nonsoluble components that may cause phototoxicity.
62 Section I Overview
Methods for Producing Extracts (not essential oils)
There are other methods of extraction that produce compounds mainly used by
the fragrance and cosmetics industry. One such compound is called an absolute.
An absolute is not a true essential oil but an extract obtained using petrol-based
chemicals. It is impossible to remove all of the chemical solvent. In 1989, the In-
ternational Fragrance Research Association issued guidelines as to the recommended
level of benzene in an absolute: it should not exceed 10 parts per million (ppm)
(International School of Aromatherapy 1993). Residual solvent found in extracts
could provoke an adverse reaction.
Solvent extraction
This three-stage method was first used on flowers by French chemist and phar-
macist Pierre Jean Robiquet in 1835 and rapidly became a popular method
(Guenther 1974). The advantage was extraction could occur at room temperature.
However, this is a complicated process requiring an expensive apparatus.
1st stage: Solvents such as benzene, petroleum ether, and, more recently, hexane
have been used to extract the volatile parts from plants. This first stage pro-
duces a waxy mixture called a concrete (often approximately 50% essential oil
and 50% wax). Hexane is believed to be safe and is used in several food-
extraction processes. However, it is impossible to remove all the solvent fol-
lowing extraction.
2nd stage: A solvent, usually ethanol, is used to dissolve the wax. This step is re-
peated several times.
3rd stage: The alcohol/wax mixture is evaporated by vacuum.
Enfleurage
This method was mainly used on fragile blossoms such as jasmine and tuberose
and is rarely used today. I watched this process in Grasse, France in 2000, and it
was very labor intensive. Animal fat is pounded until it is soft, and then glass
plates are coated with the fat. Each fat-covered glass plate is called a chassis. Fresh
blossoms are placed close together on the chassis and left until the fat becomes
saturated with essential oil. The chassis are constantly replenished with fresh
blossoms, and the old blossoms discarded. The resulting oil/fat mixture is called
a pomade. The pomade is mixed with alcohol to remove the fat, and the remain-
ing extract is called an absolute. However, 99% of jasmine and tuberose extract is
now produced by solvent extraction.
Carbon dioxide
Supercritical carbon dioxide (CO
2
) extraction, an innovative method using “flu-
idized” CO
2
, has been available since the 1980s and is making significant inroads
in the flavor, perfume, and aromatherapy worlds. Brew masters in Germany were
looking for a hops flavor extract that had no heat or chemical “off ” notes, and
German scientists found an extraction technique that did not involve heat or
Chapter 3 Basic Plant Taxonomy 63

chemical solvents. When the temperature of CO
2
is maintained at approximately
31° C, under pressure it acts like a fluid and dissolves the CO
2
-soluble part of an
herb. The advantages are no heat or chemical solvents are used and the process
produces a gentle, “unstressed” extraction. However, the chemistry of the result-
ing extract differs from that of essential oils extracted via steam distillation. For
example, steam-distilled German chamomile (Matricaria recutita) essential oil is
dark blue because heat and water create chamazulene, a sesquiterpene. Matricine,
the colorless precursor to chamazulene, occurs naturally in the plant and is
thought to be a superior antiinflammatory. Matricine is present in the German
chamomile extract yielded by the CO
2
method.
CO
2
supercritical extraction is an expensive and technologically sophisticated
process, but it is well accepted in creating pure flavors and perfume oils. As there
is a great deal more published research on the therapeutic properties of plants, and
this method produces a concentrated and undistorted plant extract (with volatile
oils in it), this is a method to watch. It may become a more accepted part of aro-
matherapy within the next few years.
Florasol
A fairly new chemical process has been developed and patented in England by
rose-grower and scientist Dr. Peter Wilde (Tisserand 1994). His method involves
extracting essential oils by means of a new solvent. The unique character of this
solvent is that its boiling point is around 30° C. Plant material can be extracted
at room temperature and the solvent removed without boiling. This ensures the
plant material is not damaged by high temperatures. The solvent residue is 1000
times less than the hexane content in a concrete or absolute obtained using tra-
ditional methods. The extract is neither acid nor alkaline. (When using liquid
CO
2
, some dissolves, which lowers the pH and produces a slightly acidic prod-
uct.) Florasol oils are used routinely by the flavor and food industry and have the
approval of the European Commission on Foods for Human Consumption. The
United States Food and Drug Administration has accepted Florasol extracts as
generally regarded as safe. Of particular note is the fact that these products do not
produce concretes that require further refining with alcohol (Wilde 1995).
Aroma Intensities
The aromas of essential oils have different intensities, and these may last for dif-
fering periods of time. The perfume industry refers to these properties as notes
and divides them into top, middle, and base notes (Price 1983). These divisions
indicate how rapidly the essential oil will lose its vitality. A top note might last,
in an unstopped bottle, for a few hours before losing its odor, a middle note might
last a couple of days, and a base note may last for several weeks.
In the 19th century, Septimus Piesse (1855), a chemist and perfumer, created
a classification system for perfume that corresponded to a musical scale (Poucher
1993). In 1923, a man named Poucher built onto the work of Piesse and devel-
oped a classification method based on a perfume’s evaporation rate scaled from 1
64 Section I Overview

to 100. Scents that evaporated quickly (1-15) were called top notes, for example,
mandarin (2) and nutmeg (11). Middle notes (16-69) included marjoram (18),
ylang ylang (24), and rose (43). Base notes lasted the longest (70-100), for exam-
ple angelica (94). Perfumes with the highest ratings last the longest and evapo-
rate the slowest (for example, frankincense, patchouli, sandalwood, and vetiver).
Poucher’s classification system was updated in 1991 and is still used today by per-
fumers (Poucher 1993).
The odor of an essential oil deteriorates as a result of oxidation. Some essen-
tial oils evaporate more quickly than others. As an essential oil evaporates, certain
components within it combine with oxygen in the air. This process is called oxi-
dization. For example, alcohols combine with oxygen to become aldehydes
(Bowles 2000). The rate of evaporation depends on the volatility of the essential
oil, and volatility depends on the components within the essential oil. Citrus oils
such as bergamot or grapefruit will evaporate faster than flower oils such as rose.
Therefore they will oxidize more quickly. The least volatile oils are the resins and
woods. Heat and sunlight can speed up oxidation. The oxidization of an essential
oil will affect the odor of an essential oil and its therapeutic potential (Tisserand
& Balacs 1995).
Resinoids are obtained from resins such as amber and mastic, balsams such
as benzoin, or gum-like substances such as frankincense and myrrh. Frequently
the method used to obtain resinoids is extraction by hydrocarbon solvents. Frank-
incense and myrrh can also be obtained by straight steam distillation. Resins are
soluble in alcohol but not in water; gums are soluble in water but not in alcohol
(International School of Aromatherapy 1993).
Biosynthesis: How and Why Plants Make
Essential Oils
Essential oils come from aromatic plants. Green plants are capable of synthesizing
complex carbohydrates from hydrogen, carbon, and oxygen. Life, as we know it,
would not continue if there was not an independent mechanism that synthesized
complex molecules from simple ones. The huge task of providing “energy for life”
is the sole responsibility of green plants, but this chemical process requires energy.
The energy required by plants to change hydrogen, carbon, and oxygen to complex
carbohydrates comes from the sun. This process is called photosynthesis.
Until the late 1950s, essential oils and all other secondary metabolites were
thought to be the waste products of a plant. This was because human energy had
been focused on the structure of compounds found in plants (and essential oils)
rather than on their function. Essential oils occurred in such small amounts
in plants that they were thought to be unimportant. However, some scientists sus-
pected that essential oils were relevant to the plant and began to explore their
therapeutic potential.
Not every plant produces essential oils; aromatic plants tend to congregate
in specific families like Asteraceae (chamomiles), Rutaceae (citrus oils), or
Chapter 3 Basic Plant Taxonomy 65

Lamiaceae (lavender and mints). Overall, only 1% of flowering plants produce es-
sential oils in any significant amount. However, plants produce more than
100,000 different chemical compounds, and the vast majority of these are not es-
sential to the physiology of the plant or its reproduction. Interestingly, some
chemical components found in plants, particularly some of the essential oils, can
actually be harmful to the plant and are stored in special cellular compartments
to prevent injury to the plant. Leakage of these essential oils can impair the
process of photosynthesis on which the plant depends for its life.
There are hundreds of aromatic plants, but not all of them produce essential
oils in sufficient quantity for distillation to be viable. For example, hyacinth is
usually obtained by solvent extraction, and then the solvent is distilled (Lawless
1992). The same is true for lily of the valley and lilac (International School of
Aromatherapy 1993). Some plants produce essential oils that can be toxic, such
as thuja, wintergreen (Tisserand 1988), and arnica (Lawless 1992). (Arnica, the
herb but not the essential oil, is traditionally used in very small amounts in home-
opathic treatments.) The amount of essential oil contained in a plant varies
tremendously and so do the components within essential oil. Sometimes the
smallest quantity of a chemical in an essential oil has a major part to play. For ex-
ample, the smell of a rose (Rosa damascena) originates from a component found
in rose that is only 0.1 parts per million.
Photosynthesis
Photosynthesis is the process by which a plant, under the influence of sunlight,
can make, in its chlorophyll-containing cells, carbohydrates from the carbon diox-
ide of the atmosphere and hydrogen from the water in the soil. Photosynthesis is
vital to the survival of the plant because carbohydrates are essential for life. The
main function of carbohydrates is to store energy.This includes sugars, starch, and
cellulose. Cellulose is used for the structure of the plant.
Carbohydrates have the general formula (CH
2
O)n, when n represents the
number of CH
2
O “units” present. The name of the carbohydrate is determined by
the number of carbons it contains (Tables 3-19 and 3-20).
The last two, di- and polysaccharides, are known as complex carbohydrates and
are the types that occur in plants. When plants convert carbon dioxide and water
into complex organic molecules, oxygen is released back into the atmosphere. Ulti-
mately these complex organic molecules made by the plant will be degraded by
plant-eating animals back into carbon dioxide and water, along with the release of
energy required for further synthesis of compounds or metabolic processes.
CO
2
H
2
O light, energy, chlorophyll CH
2
O O
2
Plant metabolism has two distinct stages. The first occurs in light and is
called photosynthesis. The second takes place without sunlight and is sometimes
called the “dark reaction” (Mann 2001b). During this stage carbon dioxide is re-
duced to produce carbon sugars. Photosynthesis takes place in the green leaves of
66 Section I Overview

plants in tiny organs called chloroplasts,which are where the green pigment chloro-
phyll is stored. Chlorophyll is responsible for capturing sunlight’s energy and con-
verting it to chemical energy. The quantity of essential oil in aromatic plants in
dry, hot, Mediterranean countries peaks in the summer months. For example,
common sage (Salvia officinalis) produces three times the amount of essential oil
in the summer as it does in the winter.
The light stage: photosynthesis
There are two stages to the light-mediated process (photosynthesis). The first
part of the light stage involves light absorption by chlorophyll. The second stage
involves splitting of water molecules. Water from the soil enters the plant via the
roots and is transported to the leaves by a specialized system called the xylem.
From there it diffuses into the chloroplasts where photolysis splits the hydrogen
and oxygen bonds, producing high-energy electrons, then adenosine triphosphate
(ATP) and more water. ATP is a form of chemical energy.
The dark stage
In the dark stage, CO
2
from the atmosphere is converted into carbohydrates, the
main product being monosaccharide sugar. This process, when hydrogen is added
to the molecule, is called reduction. CO
2
enters the plant’s leaves from the air
through tiny pores on the underside of the leaf, called stomata. The CO
2
then
travels via large, air-filled spaces to the cells containing the chloroplasts. The re-
duction of CO
2
and the subsequent synthesis of carbohydrates is achieved by a
number of enzyme-controlled reactions, all of which require energy. The energy
is supplied by ATP, which is created in the light stage of photosynthesis and also
in another metabolic process known as respiration. Written chemically, photosyn-
thesis looks like this:
6CO
2
12H
2
O → C
6
H
12
O
6
6H2O 6O
2
Chapter 3 Basic Plant Taxonomy 67
Table 3-19 h Sugars Occuring in Plants
Six carbon atoms C
6
H
12
O
6
Hexose sugar (glucose)
Five carbon atoms C
5
H
10
O
5
Pentose sugar
Three carbon atoms C
3
H
6
O
3
Triose sugar
Table 3-20 h Sugars and Their Names
Sugar molecules in isolation Monosaccharides
Sugar molecules in pairs Disaccharides
Sugar molecules in chains Polysaccharides

Natural Products
There are two major classes of natural products: primary and secondary metabo-
lites (Mann 2001a). However the dividing line between primary and secondary
metabolism is rather blurred (Mann 2001b) as the two types of metabolism are
interconnected. Primary metabolism involves the synthesis and utilization of spe-
cific chemicals essential for the survival and health of the organism. Such chem-
icals are sugars, amino acids, fatty acids, nucleotides, and the polymers obtained
from them. Secondary metabolism uses a different metabolic pathway and in-
volves the production of chemicals that have no apparent importance to the or-
ganism (Mann 2001a). Secondary metabolism produces alkaloids, bitters, glyco-
sides, gums, saponins, steroids, and essential oils. Secondary metabolism is further
discussed in the section titled “Chemistry of Essential Oils” (see page 43).
Storage of Essential Oils in Plants
Essential oils are stored in specific parts of a plant (Table 3-21). For example, rose
essential oil is found in the petals of the flowers, not the roots, leaves, or stem.
However, sometimes an essential oil is found in different parts of the same plant,
as in the case of angelica root and angelica seed. In this particular case the chem-
istry of each essential oil is different. The essential oil from the root of angelica is
phototoxic (can cause a skin reaction when ultraviolet light is used on the skin
within 24 hours of applying), but essential oil from the seed is not phototoxic.
68 Section I Overview
Table 3-21 h Parts of Plant Where Essential Oils Are Stored
Rose Flower
Angelica Root, seed
Eucalyptus Leaf
Juniper Berry
Sandalwood Wood
Cinnamon Bark, leaf
Clove Leaf, bud
Myrrh Resin
Black pepper Seed
Rosemary Whole herb
Mandarin Fruit peel
Pine Needles

Secretory and Storage Structures of Essential Oils in Plants
For additional reading, Svoboda and Svoboda’s excellent, illustrated book, Secre-
tory Structures of Aromatic and Medicinal Plants (2001), is a must, and the infor-
mation in this section is based on it. Essential oils are stored in special secretory
structures (Table 3-22), either on the surface of the plant or within the plant tis-
sue, and are found in many different types of plant: perennial, annual, biennial,
evergreen, and deciduous (Svoboda & Svoboda 2001). Secretory structures vary
and include single, secretion-containing cells that are similar to the surrounding
cells, secretory ducts, secretory cavities, osmophores, glandular trichomes, and
epidermal cells. Often the family or genus of a plant will have a similar secretory
system. This can be useful in plant identification.
Single, secretion-containing cells are common in many aromatic plants such
as the leaves of lemongrass, rhizome of ginger, seed coat of cardamom, fruit wall
of black pepper, bark of cinnamon, and root of valerian. Secretory ducts are elon-
gated cavities found in plants such as coriander, cumin, angelica, dill, anise, and
fennel (all members of the Umbelliferae family). Secretory cavities are prevalent in
the fruit and leaves of lemon, orange, and bergamot in the Citrus family. They are
also found in the bark of myrrh and frankincense and in clove buds. Osmophores
are found in orchids and are areas of tissue with secretory cells different structurally
from the surrounding cells. Glandular trichomes are modified epidermal hairs
found on leaves and stems of plants such as basil, lavender, and marjoram in the
Lamiaceae family. Epidermal cells diffuse essential oil directly through the cyto-
plasm and cell wall to the outside, and the amount of essential oil diffused is very
low. Examples of aromatics with epidermal cells are rose and jasmine.
There are various theories as to why some plants produce secondary metabo-
lites such as essential oils. They could be a defense. Secondary metabolites appear
to protect the plant from being eaten by herbivores (plant-eating animals or in-
sects), by repelling them. For example, wild tobacco (Nicotiania sylvestris) can in-
crease its production of nicotine by three or four times when it is under attack,
and the bitter taste deters predators (Mann 2001b). Often a secondary metabo-
lite can reduce the growth or maturation of an insect eating the aromatic plant.
Grasshoppers eating Cyperus iria become sterile, and tenulin (a sesquiterpene
lactone) in Helenium amarum disrupts the growth and development of insect
Chapter 3 Basic Plant Taxonomy 69
Table 3-22 h Types of Storage for Essential Oils
Part Plant
Single secretion cells Ginger, black pepper, cardamom, valerian, lemongrass
Secretory cavities Citrus fruits, clove, myrrh, frankincense
Secretory ducts Tarragon, angelica, aniseed, pine
Secretory hairs Many plants in the Lamiaceae and Geraniaceae families

larvae (Mann 2001b). Although mammals can cope with terpenes in their diet,
many mammals and rodents find the aroma (and taste) of terpenes repellent and
will not feed from aromatic plants. Voles, (a small rodent common in Europe) for
example, will not eat pine needles. However, there are obvious exceptions. Aus-
tralian possums and kangaroos are two mammals that have adapted and live off a
diet of Eucalyptus leaves.
Certain plants exude aromas that deter insects. The Lamiaceae family has two
well-known plants, pennyroyal and peppermint, that deter insects. The mosquito
that carries yellow fever is repelled by mugwort (Artemisia vulgaris), and recent
clinical studies have found that the mosquito carrying malaria is repelled by
Artemisia annua. Artemisinin (called qinghaosu in Chinese medicine) is a
sesquiterpene found in Artemisia annua and is responsible for repelling mosqui-
toes. This plant has been used in Chinese medicine for that purpose for 2000 years!
Another possibility for the purpose of essential oils is to increase pollination
by attracting insects. Many chemical compounds found in the odor glands of in-
sects are also found in flower fragrances. Usually it is a mixture of compounds that
generates the aroma the insect is seeking. Each part of the fragrant area of the
plant may present a different volatile profile. The rose, for example, produces dif-
ferent aromas in its petals than in the sepals and stamens.
Odor is thought to be more important to a pollinating insect than color. This
is obvious with night-flying creatures. Some flowers are pollinated by bats and
others are pollinated by moths. Insects are so sensitive to smell they can pick up
a scent at 1/100 the level discernible to a human. Floral fragrances such as
monoterpenes are important insect attractants. Some plants, such as Datura in-
noxia produce a narcotic, so the hawkmoth becomes addicted and returns regu-
larly for “fixes” (Mann 2001a). Insects live in a world where actions are triggered
by smell rather than noise or light.
Another theory as to why plants produce secondary metabolites is to prevent
attack by bacteria, viruses, and fungi. Plants respond to attack from bacteria,
fungi, or viruses by producing stress metabolites called phytoalexins. Some phy-
toalexins are used by pharmaceutical companies to protect foodstuffs from infec-
tion or spoiling (Guenther 1972).
Allelopathy is the ability of a plant to prevent other plants from growing too
close to it. Bracken and ferns leach germinating inhibitors (usually phenols) into
the ground to deter other species from germinating or growing too close. Aro-
matic plants can use essential oils such as camphor to protect the land around
them from other plants. Terpenes are the largest group of chemical components
found in aromatic plants, and many terpenes can inhibit the respiration of other
plants (Mann 2001b). The sage bush (Salvia leucophylla), which is prolific in the
near-desert terrain of southern California, contains chemical compounds 1,8-
cineole and camphor that deter other plants’ germinating.
Yet a further hypothesis for the production of essential oils is their antitran-
spirant activity. Essential oils aid survival in difficult climatic conditions when a
haze of volatile oils may influence stomatal closure and prevent excess water loss
from the leaves.
70 Section I Overview

Quality of Essential Oils
Finally, there are many factors that can affect the quality of the essential oil (Table
3-23). The chemical makeup of all living plants depends on climate and environ-
mental conditions (such as rainfall, sunlight, soil acidity, altitude) and pollution
(Guenther 1972). The chemistry of the same species of rose grown in Bulgaria will
be subtly different from one grown in England. Similarly, Lavandula angustifolia
grown high in the mountains will contain more esters, which are thought to have a
greater antispasmodic effect, than Lavandula angustifolia grown closer to sea level.
If Lavandula angustifolia is distilled at a high altitude this will also increase the
amount of esters. Lavandula angustifolia essential oil with a higher percentage of es-
ters will have an aroma that is softer and fruitier. There are so many variables that
the simplest way to be sure of the composition of the essential oil is to use modern
analytical methods as well as the nose. This will be covered in the next section.
What Are Essential Oils Used For?
Of the hundreds of essential oils produced, there are classics in common, everyday
use the world over. These essential oils have research-based therapeutic properties
and a long history of use. Many aromatic herbs are used in cooking, such as basil,
thyme, coriander, rosemary, dill, oregano, and bay. Some are drunk in tisanes, in-
cluding peppermint, lime flower, and chamomile. Several names of plants that pro-
duce essential oil will already be familiar. Some have been used in orthodox medi-
cines for centuries, for example peppermint in mouthwashes and eucalyptus in Vicks
VapoRub. Essential oils continue to play an important part in our lives. You may be
surprised at the uses for some of them, as illustrated in Table 3-24 (Guenther 1972).
Chapter 3 Basic Plant Taxonomy 71
Table 3-23 h Factors affecting quality of essential oil.
Soil type
Climate
Geography
Altitude
Use of fertilizers and pesticides
Time of harvest (including both time of year and time of day)
Genetics
Age of plant
Temperature at which essential oil is distilled
Length of time essential oil is distilled
Number of times essential oil is distilled

Analysis Tests for Purity in Essential Oils
Gas chromatography linked to mass spectrometry (GCMS) is one of the most
important tests to ascertain purity. The GC part separates the essential oil into
individual constituents (like linalyl acetate) and shows their relative concentra-
tions in a computerized printout showing a succession of peaks. The lighter
molecules will peak first, and the MS part will identify those peaks. Although a
GCMS will identify and quantify the chemical components, it may not always
detect additional synthetic chemicals that have been added to extend or alter the
essential oil.
To begin the test, a minute amount (about 1 microliter) of essential oil is in-
jected into a tubular column temperature controlled to vaporize the sample. The
constituents are separated by the differences in their solubilities in a nonvolatile
absorbent that coats the inner walls of the tube. The vaporized sample is carried
through the tube in a slow stream of helium or nitrogen, and all constituents are
kept in the vaporous state by means of hot air circulating in the column. The re-
sults of the analysis are recorded as a series of peaks drawn by a pen recorder that
plots a trace of each of the components of the essential oil as it exits the column.
As the components exit, they are bombarded with high-energy electrons that
72 Section I Overview
Table 3-24 h Uses for Essential Oils
Adhesives, alcoholic beverages, animal feed, automobile industry
Baked goods
Candle makers, canning industry, ceramics, chewing gum, confectionery, contact
lenses
Dental preparations
Food industry (especially prepared foods)
Household goods (including furniture polish, lavatory cleaner, air-freshener, and
washing powder)
Ice cream, insecticides
Meat-packing
Paint, paper, perfume, pharmaceuticals, printing
Rubber manufacturing
Soap, soft drinks
Textile production, tobacco
Veterinary supplies (including meats)

fragment them. The characteristic fragmentation pattern for each molecule is
identified by comparing it with a computerized pattern in a database.
A second important method of analysis is through optical rotation. The mol-
ecules within essential oils have the ability to rotate a plane of polarized light.
This activity is measured by a polarimeter. Molecules that rotate counterclockwise
are called laevorotatory, or l for short. Those that rotate clockwise are called dex-
trorotatory, or d. This designation is indicated in the name of the molecule, as in
d-limonene. The angle at which the light is rotated is an important physical char-
acteristic by which an essential oil can be recognized. Almost all essential oils
show optical activity. This test can reveal synthetic compounds that alter the op-
tical rotation.
Another method of analysis is the refractive index. When light passes
through a liquid it is refracted. This refraction can be measured and is consistent
for a given essential oil. In scientific terms, it is the ratio of the speed of light of
a given frequency in a vacuum to the speed of light in a medium of some kind, at
a specified temperature. It is important that the test be carried out at the same
temperature as the reference (the standard).
A fourth analysis is the infrared test. Electromagnetic radiation can be passed
through an essential oil and produces a spectrum that is like the fingerprint of the
essential oil. Adulteration of the oil will show up clearly with this method.
The fifth and most important tool of analysis is the nose. When first exper-
imenting with essential oils, you may find it hard to notice differences between
synthetic and real essential oils and pure oils and adulterated ones. However with
patience the nose learns. To sample an essential oil correctly, do not smell directly
from the bottle. Put one or two drops on to a special smell strip (made from pa-
per a little like blotting paper). Recap the bottle. Holding the smell strip approx-
imately 6 inches in front of your face, move it slowly from one side to the other
and back again. The sense of smell may be different from one nostril to the other
as the aroma reaches different parts in the brain. One nostril may detect a sweeter
smell than the other. Move the strip back and forth several times. Closing your
eyes might aid concentration. It can be useful to rate the aroma on a scale of 0 to
10: 0 means disliking the odor intensely, and 10 means the odor is very pleasant.
Write down a word or sentence that describes the aroma. When testing essential
oils from an unknown source, first try one known to be authentic to “fix” the smell
imprint in the mind. Then try the new one. The trained human nose is the most
important piece of equipment in finding out whether the essential oil has been
adulterated.
Buying Essential Oils
In the last few years there has been a rapid increase in the number of essential-oil
companies. Many operate by direct mail. The commercial sections of healthcare
journals include advertisements for many essential oil distributors. In the USA,
most health-food shops, some drugstores, and certain department stores also
Chapter 3 Basic Plant Taxonomy 73
carry a range of essential oils. Many essential oil mail-order companies have been
set up quickly and with little knowledge of the oils. Customers believe they are
buying essential oils of the highest grade (Scholes 2001).
Although many companies appear to provide true essential oils, this is not al-
ways the case. Some dealers openly state in their literature or on the bottles that
their oils are diluted. Other companies are not so honest, and customers are led
to believe that they are purchasing 100% pure essential oil. The phrase “pure es-
sential oil” can mean many things. Essential oils are extremely easy to dilute or
adulterate (Guenther 1972). The most common method of dilution is the addi-
tion of a vegetable oil. When this occurs, the essential oil leaves a ring as it evap-
orates. If alcohol is added to dilute the oil, it is sometimes discernible in the
aroma. Adulteration by adding a cheaper substitute, for example, putting gera-
nium oil in rose oil or petitgrain or bergamot in neroli, is commonplace. Real
melissa oil is extremely difficult to find, because it is frequently adulterated with
lemongrass or citral. Sometimes particular components are added, such as cit-
ronella, geraniol, or linalol (Wagner et al 1984). Some of the best melissa is actu-
ally grown in Ireland.
When purchasing essential oils, Scholes (2001) suggests first to determine the
purpose for which the essential oil is being purchased. He lists several categories:
1. Medicinal or internal use
2. Candles and soaps
3. Massage and therapeutic applications
4. Cleaning products or environmental fragrancing
The second important factor is the oil’s country of origin; several countries
produce the same essential oil but of varying quality. For example, rose is grown
and distilled in France, Bulgaria, Turkey, China, and Morocco. Scholes notes that
only a few essential oils are produced in the United States—mainly peppermint,
citrus, and some lavender. However, these are not suitable for the aromatherapy
market because they have been grown with pesticides. There would seem to be a
huge market out there for farmers wanting to grow something different!
For safety, you should only buy an essential oil that is correctly labeled. Much
more information is needed than just the generic name. Product lists and bottle
labels should bear the oil’s complete botanical name, the country of origin, the
part of the plant from which it was derived, and should note whether the oil is
wild crafted or organic. Some of the best suppliers tell the buyer whether the
whole flowering plant was used, or just the flowering heads. Reputable suppliers
are happy to provide gas-chromatography/mass spectrometry (GCMS) informa-
tion and material safety data sheets (MSDS) for their products. The chemotype,
when relevant, also needs to be specified. Also mentioned on the product list
should be the type of extraction used and whether the batch number is known.
Organically grown plants used for essential-oil production are certified, and the
bottles carry a stamp to prove it. There are various accepted organic stamps. In
the United Kingdom, most authentic distributors are members of the Essential
Oils Trade Association (EOTA) or the Aromatherapy Trade Council (ATC).
74 Section I Overview

In the United States, the National Association for Holistic Aromatherapy offers
the certification label “true aromatherapy product” (TAP). French and German
oils usually have their own stamps of authenticity.
Bottles should contain integral droppers and be made of colored glass. “Pure
100 per cent essential oil” should be clearly marked. Basic safety precautions such
as “do not take by mouth,” “keep away from children,” and “avoid contact with
eyes” should also appear on the label. Apart from the label and the price, the only
reliable indicators of authentic essential oils are an experienced nose and pur-
chasing from a reputable company that would lose too much by compromising
itself. It is best to ask around. Qualified aromatherapists tend to buy from the
same small group of suppliers.
REFERENCES
Arctander S. 1960. Perfume and Flavor Materials of Natural Origin. Wheaton, IL:
Allured Publishing, 13.
Alkaire B, Simon J. 1992. A portable steam distillation unit for essential oil crops. Hort-
Technology 2(4) 473-476.
Bowles J. 2000. The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Printers.
Guenther E. 1972. The Essential Oils, Vol. I. Melbourne, FL: Krieger Publishing.
Guenther E. 1974. The Essential Oils: Individual Essential Oils of the Plant Families.
Melbourne, FL: Krieger Publishing.
Guenther E. 1976. The Essential Oils, Vol. V. Melbourne, FL: Krieger Publishing.
Lawless J. 1992. Encyclopedia of Essential Oils. Shaftesbury, UK: Element Books.
Mann J. 2001a. Chemical Aspects of Biosynthesis. Oxford, UK: Oxford Science Publica-
tions, 2.
Mann J. 2001b. Secondary Metabolism. Oxford, UK: Oxford Science Publications, 7.
Poucher W.1993. Poucher’s Perfumes, Cosmetics and Soaps, Vol 2, 9th ed. Chapman &
Hall.
Piesse S. 1855. The Art of Perfumery. London: Longman, Brown & Green.
Price S. 1983. Practical Aromatherapy. London: Thorsons.
Scholes M. 2001. Finding the true essential oil. Aromatherapy Journal. 11(1) 19-23.
Suskind P. 1986. Perfume: The Story of a Murderer. London: Penguin Books, 62.
Tisserand R. 1985. The Essential Oil Safety Data Manual. Brighton, UK: Tisserand
Aromatherapy Institute.
Tisserand R. 1994. Profile: Peter Wilde. International Journal of Aromatherapy. 6(2) 3-7.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Svoboda K, Svoboda T. 2001. Secretory Structures of Aromatic and Medicinal Plants.
Wales, UK: Microscopix Publications.
Wagner H, Bladt S, Zgainski E. 1984. Plant Drug Analysis. Berlin, Germany: Springer-
Verlag.
Wilde P. 1995. Flavour, fragrances and essential oils. In 13th International Congress
Proceedings, Istanbul. Eskisehir, Turkey: Anadolu University Press, 351-357.
Chapter 3 Basic Plant Taxonomy 75

W
76
4
Essential Oil Toxicity
and Contraindications
J
UST BECAUSE essential oils are natural does not mean they do not have poten-
tial risks or hazards if used inappropriately. This section addresses toxicity and
contraindications. Put in context, essential oils are extremely safe and carry
few of the risks of many modern medicines. However, it is pertinent to the in-
creasingly high profile of aromatherapy that all those using essential oils must be
aware of possible side effects and interactions. The author is grateful to the help
and advice of the expert reviewers of this section: Tony Balazs, PhD, and Ron
Guba.
Part I: Essential Oil Toxicity
A sensory problem associated with fragrances is that they become less intense with
repeated sniffs.
Schiffman (1992)
There is a certain amount of controversy about the toxicity of essential oils. There
are those who say essential oils are dangerous and should never be taken orally.
There are those who take essential oils orally or give them to their patients to take
orally and see no problem. There are those who use essential oils every day, and
there are those who believe taking an essential oil for longer than three weeks
could lead to liver damage. Each point of view is usually based on the kind of aro-
matherapy training the person has received.

Jellinek (1999) writes that because the concentrations of substances in essen-
tial oils enter the body in the vapor state, the amount is smaller than the usual
pharmacologic mode of application, and the likelihood of systemic side effects are
reduced. Guba (2000) believes much of the concern about toxicity of essential oils
is based on myth, and he gives a very strong argument to support his case. Scare
tactics are counterproductive. Essential oils have been in the public domain for
hundreds of years, and the number of toxicity problems is so few common sense
indicates that, when used sensibly, essential oils must be safe. Perhaps what is
needed is a large dose of common sense. Everything, even water, can be toxic if
taken in too large a quantity.
This is where most potential problems with essential oils lie: use of extremely
large amounts. For example, tea tree oil has become very popular and appears in
shampoos, gels, creams, and lotions. It has been recommended for treating ticks
and fleas in pets. However, Villar et al (1994) showed that, in some circumstances,
large amounts of topically applied tea tree oil can be toxic to dogs and cats. Symp-
toms were depression, weakness, uncoordination, and muscle tremors. When tea
tree oil was withheld, these symptoms disappeared within 2 or 3 days.
Toxicity and Approaches to Aromatherapy
The English approach to aromatherapy focuses on using diluted essential oils (up
to 5%) applied to the skin in a massage. Essential oils are used mainly for relax-
ation, stress management, and sometimes for upper respiratory-tract infections.
There are no reports of toxic effects from using essential oils in this way. The
French approach to aromatherapy may use several milliliters of undiluted essen-
tial oil on the skin at a time, sometimes several times a day. Physicians may also
give patients gelatin capsules (each containing three or four drops of essential oils
diluted in a carrier oil or gel) to be taken orally three or four times a day. Essen-
tial oils given in this way are used to treat infection or chronic conditions and are
rarely used for relaxation. There is more chance of toxicity from the oral route, al-
though there have been virtually no cases recorded. The majority of French physi-
cians who use essential oils in this way are working alongside bacteriologists and
pharmacists, and are well aware of toxicity issues. A potential toxicity hazard
could occur when untrained people use essential oils orally and ingest too much.
Some aromatherapists (including myself ) are trained in both external and in-
ternal methods of aromatherapy. Clearly there is a need and a place for both ap-
proaches, and perhaps a compromise that uses both could be the best of both
worlds. However, each approach needs to take into consideration the experience,
training, and expectations of the person giving the essential oils. The internal use
of essential oils clearly means using them as medicines and, in the United States
at least, this might be seen as outside the license of many health professionals.
However, there is no licensing process for practitioners who wish to dispense
herbal medicine in the United States, and the oral method of aromatherapy
could easily be integrated under herbal medicine. There is an excellent chapter in
Chapter 4 Essential Oil Toxicity and Contraindications 77

Essential Oil Safety (Tisserand & Balacs 1995) that covers toxicity in depth. This
is recommended reading. There are also useful articles on the subject by Guba
(2000) and Burfield (2001).
Ingestion Reactions
Toxicity can be nonspecific or specific. Nonspecific toxicity covers all essential oils
when used in very large amounts. Specific toxicity pertains to those essential oils
that can cause toxicity at lower levels, and these are outlined here (Table 4-1).
Specific toxicity is roughly divided into two types: acute (short term) and chronic
(long term). In acute toxicity, the worst scenario is poisoning. The symptoms of
78 Section I Overview
Table 4-1 h Reported cases of overdose with common essential oils.
Amount
Essential oil in ml Symptoms Source
Cinnamon 60 Pilapil 1989
Citronella 15 Mant 1961
Clove 5-10 Lane et al 1991
Hartnoll et al
1993
Eucalyptus 5 Craig 1953
Patel & Wiggins
1980
Hyssop 10-20 Convulsions Millet 1981
Dizziness, double vision,
nausea, vomiting, collapse
Vomiting, shock, frothing at
the mouth, deep rapid
respiration, cyanosis, con-
vulsions, brain hemor-
rhage, death
Severe acidosis, central ner-
vous system depression,
ketones in urine, deterio-
rating liver function, ex-
tremely low blood glu-
cose, generalized seizure,
deep coma
Vertigo, loss of coordina-
tion, abnormal respira-
tion, epigastric pain, cold
sweats
Lesser amounts: excess res-
piratory tract mucus
Greater amounts: de-
creased respiratory tract
mucus, pinpoint pupils,
rapid drowsiness, uncon-
sciousness

poisoning with ingested essential oils are nausea, vomiting, ataxia, confusion,
convulsions, and coma (Patel & Wiggins 1980). Many papers about essential-oil
poisoning cite instances when essential oils were taken orally; these cases usually
involve children. In most instances, the amount of essential oil taken was
substantially greater than is normally used orally, topically, or in inhalation
aromatherapy.
Burfield (2001) cites an analysis of more than 100 pediatric poisoning acci-
dents involving ingested eucalyptus. The study indicates that in 74% of cases, ac-
cess to eucalyptus had been gained via the home vaporizer. The popularity of aro-
matherapy and today’s easy access to bottles of essential oils mean poisoning is a
potential hazard if someone decides to drink the essential oil. However most rep-
utable companies supply bottles with integral droppers. Symptoms of oral poi-
soning can occur rapidly and include a burning sensation in the mouth and
throat, abdominal pain, and spontaneous vomiting, although the latter may be de-
layed by up to 4 hours. Dangerous respiratory depression also can occur with deep
coma. Convulsions may occur in children, but are rare in adults. Some fatalities
have shown nephrotoxicity (Patel & Wiggins 1980). The range of when an es-
sential oil becomes lethal is wide. For example, the safe dose for internal use of
eucalyptus is 0.006 to 0.2 ml (Martindale 1977). Death in adults has occurred af-
ter ingestion of as little as 4 or 5 ml, which seems extremely low, and is usual af-
ter ingesting 30 ml (MacPherson 1925). However, people have recovered after in-
gesting up to 220 ml of eucalyptus essential oil (Gurr & Scroggie 1965).
Craig (1953) discusses the case of a 3-year-old who consumed 10 ml of eu-
calyptus (2 teaspoons). He became deeply unconscious; his pupils constricted,
muscle tone was markedly reduced, and there were no tendon reflexes. His
breathing was shallow and irregular at a rate of 10 breaths per minute. Insertion
of an endotracheal tube produced no gag reflex. Pulse was 70 beats per minute,
and blood pressure was 75/40 mm Hg. The child’s serum urea was 6.3 μmol/L
(38 mg/100 ml) with normal electrolytes. He was given gastric lavage with
sodium bicarbonate solution. Sodium sulphate (100 ml) was left in the stomach
as a cathartic. After 2 hours, his pulse, blood pressure, and respiration were nor-
mal. He was discharged after 48 hours in hospital.
Wilkinson (1991) discusses the toxic effect of ingested essential oils on three
children admitted to an emergency room in Australia. Their ages were 19
months, 23 months, and 25 months. The 19-month-old ingested an indetermi-
nate amount of lavender. The kind of lavender was not specified because poison
reports tend not to include botanical names, but the chemistry of Lavandula an-
gustifolia, L. latifolia, and L. stoechas are very different and therefore their toxici-
ties are different. L. stoechas, which contains ketones, would be more toxic than L.
angustifolia, which contains mainly linalyl acetate or linalol. It was also not spec-
ified whether the lavender oil was synthetic or natural. The 25-month-old took
an unknown amount of tea tree oil, and the 23-month-old ingested 40 ml of eu-
calyptus oil. All three children were ataxic. All three were anesthetized and given
gastric lavage, and two were also intubated. Charcoal was given in all cases and
sorbitol in one. All three children recovered fully in the hospital.
Chapter 4 Essential Oil Toxicity and Contraindications 79

A fourth child who consumed 30 ml of eucalyptus became comatose after
falling against a coffee table. Gastric lavage was performed, and the child recov-
ered after 4 days of fluctuating consciousness.
Much hype surrounds pennyroyal as an abortificant. However there are very
few cases reported. There are a few cases of toxicity, all of them situations in
which the essential oil was ingested. Pennyroyal, although not used frequently in
aromatherapy, is used in herbal remedies and teas, and some of the teas contain
the essential oil. Bakerink et al (1996) reported on two infant siblings who were
given home-brewed tea of pennyroyal. Serum levels of pulegone and its metabo-
lite menthofuran were then taken. The first infant tested positive for menthofu-
ran (10 ng/ml) and manifested fulminant liver failure with cerebral edema and
necrosis, followed by death. The second infant tested positive for pulegone
(25ng/ml) and menthofuran (41 ng/ml) and manifested hepatic dysfunction and
several epileptic seizures. There have been no recorded instances of pennyroyal
toxicity following dermal application.
Temple et al (1991) reported on five cases of citronella poisoning. All involved
young children who drank varying amounts of the essential oil. Because citronella
is a nonspecific toxin, a large amount must be ingested to yield toxic effects. All
five children recovered. William Robertson, Medical Director of Children’s Hos-
pital and Medical Center, Seattle, Washington, comments at the end of the report
that he “would judge the risk of severe poisoning to be relatively remote.”
Even the ubiquitous linalol has been tested for toxicity. Following oral ab-
sorption in the gut of a mouse, 55% was rapidly excreted in the urine as urea, di-
hydro, and tetrahydrolinalool; 15% was eliminated in feces; and 23% was expired
with carbon dioxide after a lag period of several hours (Powers & Beasley 1985).
After oral administration, 3% remained in the tissues: 0.5% in the liver, 0.6% in
the gut, 0.8% in the skin, and 1.2% in the skeletal muscle. Acute systemic toxic-
ity was demonstrated with ataxia, a decrease in spontaneous motor activity, lateral
recumbency, vasodilation, rapid decrease in arterial blood pressure, and respira-
tory disturbance leading to death.
Measuring Toxicity
Much of the information available on toxicity is based on animal studies. Of
course, this is true of conventional drugs as well. Most essential oils have had ex-
tensive toxicologic studies carried out by the fragrance industry (for inhaled and
topically applied essential oils) and the flavor industry (for ingested essential oils).
Guba (2000) draws attention to the way toxicology studies are carried out. Usu-
ally a very large amount of essential oil is given to the test animal in a very short
period. This is totally unlike the human situation in which small amounts of es-
sential oils are given during a longer period. The huge amounts given in animal
testing are never given all at once to humans, and rarely are such large amounts
given during an extended period.
There are two ways essential-oil toxicity can be measured: oral and dermal.
Both are tested on animals. Oral lethal dose is usually tested on laboratory mice
80 Section I Overview

or rats. The animals are force-fed essential oils until 50% of them die. The
amount the test group has ingested when this occurs is the median lethal dose,
which is know as LD50. This is the number of milligrams or grams of essential
oil per kilogram of animal body weight it took to kill half the animals.
There is a difference between a poison and a lethal substance. Whereas a
lethal substance kills the system, a poison is any substance that “irritates, damages
or impairs the activity of the body’s tissues” and is “harmful in relatively small
amounts”(McFerran 1996). A poison is not always lethal. So although the lethal
dose of an essential oil can tell us what will kill a patient, substantially less than
that can have poisonous effects. Even so, the amount required to produce poiso-
nous effects is staggeringly high, depending on the oil in question.
The LD50 dermal lethal dose is determined via a test on a shaved area of the
skin of animals, usually rabbits. Human skin is less permeable than rabbit skin.
When 50% of the test subjects die, that is the dermal LD50. There have been very
few clinical tests on human skin. Those that have been carried out involved vol-
unteers who were given a patch test for a 24-hour period (Watt 1991). The largest
patch study to date was carried out by Japanese scientists, spanned 8 years, and
involved 200 human volunteers who used 270,000 patch tests. Asian skin may be
more or less sensitive than Caucasian skin (International School of Aromather-
apy 1993).
Simple math can also be used to show how close to the toxic level a 5%
solution of an essential oil used as topical application can come. If the dermal
LD50 of eucalyptus globulus is 5 g/kg (actually it is more than 10% according to
Kligman), then the following equations determine toxicity:
Average woman of 150 lbs ⫽ approximately 75 kg
5 ⫻ 75 ⫽ 375 grams ⫽ approximately 400 ml (allowing for specific gravity).
If the solution is 5%, 8000 ml are required ⫽ 8 L
It is unknown exactly how much of the eucalyptus is absorbed through the
skin—certainly not 100%. Much depends on the skin’s integrity, its temperature,
and whether it is covered after application of the oil. Let us allow for 50% ab-
sorption (which is generous). It is impossible for 4 L of essential oil to be ab-
sorbed by the skin all at once. (However, there would be considerable effects from
inhaling the essential oil as well.)
Oral LD50 of eucalyptus globulus is 2.48 g/kg
Average woman of 150 lbs ⫽ approximately 75 kg
2.48 ⫻ 75 ⫽ 186 g ⫽ approximately 200 ml (allowing for specific gravity)
Skin Reactions
In skin tests, adverse reactions can be divided into irritation, allergic sensitivity,
and phototoxicity. Sensitivity and safety are covered in Chapter 4. Some essential
oils are thought to be dangerous when used undiluted on the skin. These include
essential oils high in phenols or aromatic aldehydes (like cinnamaldehyde). I have
Chapter 4 Essential Oil Toxicity and Contraindications 81

also found some oxide-rich essential oils can be irritating to abraded mucosa.
However, many phenol-rich essential oils are used in France at high dilutions to
treat infections Tiger Balm, a popular cream for aches and sprains, contains 60%
essential oils including cassia, clove, and camphor. However Tiger Balm applied
to a scratched skin surface is not comfortable, and it should not be applied to a
baby’s skin. Guba (2000) suggests using 90% nonirritant essential oil with 10%
phenolic oil if high concentrations or undiluted essential oils are required.
Inhalation Toxicity
Inhaled essential oils are unlikely to produce a toxic reaction. Hypothetically, a
toxic reaction could occur if a person was confined to a nonventilated room, the
temperature was very high, and there was a constant diffusion of essential oil un-
til the air was saturated. However, the effect of this situation would be more like
suffocation than a reaction to the essential oil.
References
Bakerink J, Gospe S, Dimand R et al. 1996. Multiple organ failure after ingestion of
pennyroyal oil from herbal tea in two infants. Pedatrics. 98(5) 944-947.
Burfield T. 2001. Safety of essential oils. International Journal of Aromatherapy. 10(1/2)
16-29.
Craig J. 1953. Poisoning by the volatile oils in children. Archives of Disease in Child-
hood. 55(5) 475-483.
Guba R. 2000. Toxicity myths: The actual risks of essential oil use. International Journal
of Aromatherapy. 10(1/2) 37-49.
Gurr F, Scroggie J. 1965. Eucalyptus poisoning treated by dialysis and mannitol infusion
with an appendix on the analysis of biological fluids for alcohol and eucaluptol. Aus-
tralasian Annals of Medicine. 14(3) 238-249.
Hartnoll G, Moore D, Douek D. 1993. Near fatal ingestion of oil of cloves. Archives of
Disease in Childhood. 69:392-393.
International School of Aromatherapy. 1993. A safety guide on the use of essential oils.
London: Nurtured by Nature Oils, Ltd.
Jellinek S. 1999. Odors and mental states. International Journal of Aromatherapy. 9(3)
115-120.
Kligman A. 1966. The identification of contact allergens by human assay. Journal of In-
vestigative Dermatology 47(5) 393-409.
Lane B, Ellenhorn MJ, Hulbert TV et al. 1991. Clove ingestion in an infant. Human
and Experimental Toxicology. 10(4) 291-294.
MacPherson J. 1925. The toxicology of eucalyptus oil. The Medical Journal of Australia.
2:108-110.
Mant A. 1961. A case of poisoning by oil of citronella. Association Proceeding VI. Med-
icine, Science, and the Law. 1, 170-171.
Martindale W. 1977. The Extra Pharmacopoeia, 27th ed. London: Pharmaceutical Press.
McFerran T (ed.). 1996. Oxford Dictionary of Nursing, 2nd ed. Oxford, UK: Oxford
University Press.
82 Section I Overview

Millet Y. 1981. Toxicity of some essential plant oils. Clinical and experimental study.
Clinical Toxicology. 18(12) 1485-1498.
Patel S, Wiggins J. 1980. Eucalyptus poisoning. Archives of Disease in Childhood. 55(5)
405-406.
Pilapil V. 1989. Toxic manifestations of cinnamon oil ingestion in a child. Clinical Pedi-
atrics. 28(6) 276.
Powers K, Beasley V. 1985. Toxicological aspects of linalool: A review. Veterinary and
Human Toxicology. 27(6) 484-485.
Schiffman S. 1992. Aging and the sense of smell: Potential benefits of fragrance en-
hancement. In Van Toller S, Dodd G (eds.), Fragrance: The Psychology and Biology
of Perfume. London: Elsevier Applied Science, 54.
Temple W, Nerida A, Beasley M, et al. 1991. Management of oil of citronella poisoning.
Clinical Toxicology. 29(2) 257-262.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Villar D, Knight M, Hansen S et al. 1994. Toxicity of melaleuca oil and related essential
oils applied topically on dogs and cats. Veterinary and Human Toxicology. 36(2)
139-142.
Watt M. 1991. Plant Aromatics. Essex, UK: Witham.
Wilkinson H. 1991. Childhood ingestion of volatile oils. The Medical Journal of Aus-
tralia. 154:430-431.
Chapter 4 Essential Oil Toxicity and Contraindications 83

Part II: Contraindications
A good name is like a precious ointment; it filleth all around about, and will not
easily away: for the odors of ointments are more durable than those of flowers.
Francis Bacon
M
any adverse reactions can be avoided if pure essential oils are used. Es-
sential oils are steam distilled, and therefore the potential for adverse re-
actions to something other than the essential oils (e.g., a solvent) is
eradicated. It is logical to assume that essential oils that have been adulterated, or
extended, are more likely to cause a problem, although this is difficult to prove.
Nonetheless, the possibility of adverse reactions to pure, unadulterated essential
oils cannot be ruled out totally. These reactions may happen with patients who are
already on multiple drug regimens or who are allergy prone. Patch testing can do
much to detect, and therefore avoid, these reactions. There are also a few essential
oils that can cause dermal irritation if used undiluted.
The amount of essential oil used tends to be measured in percentages or
drops. However, there is some confusion over how big a drop is! Olleveant et al
(1999) investigated several suppliers of bergamot oil and showed that their drop
sizes differed. However, an average measurement used by aromatherapists is 20
drops of essential oil to 1 ml. Patch tests can be used to avoid skin reactions such
as irritation and sensitivity and are suggested for all potential-risk patients. Dilute
the essential oil to double the concentration to be used and put it on an adhesive
bandage. Place the bandage on the patient’s forearm and leave in place for 24
hours to assess any adverse reactions.
Possible Skin Reactions
Irritation
Skin irritation is produced by an irritant component within the essential oil and
occurs immediately, usually producing a red wheal or burn. The irritant compo-
nent is most often a phenol (found in clove, oregano, and thyme) or an aromatic
aldehyde (found in cinnamon). The reaction sensation is one of heat and burning.
Immediate dilution with a carrier oil is required, followed by washing with warm
water and nonperfumed soap. Do not use water initially; that pushes the essential
84 Section I Overview

oil into the dermis. This kind of instant irritation from a 2% to 5% dilution of a
pure, fresh essential oil is a rare event and is more likely to occur with much
higher concentrations. Essential oils with high percentages of phenols or aromatic
aldehydes should not be used undiluted on the skin.
Skin irritation caused by a chemical used in the extraction method may also
occur. Solvent chemicals are not used in true essential oils and their presence in-
dicates that the extract is an absolute, not an essential oil. There have also been
incidences of erythema following the use of topical benzoin (Rademaker & Kirby
1987; Lesesne 1992). Benzoin is sometimes used in a proprietary spray before ap-
plying an adhesive dressing. Old citrus peel oils (e.g., mandarin, bergamot, and
lemon) in which the terpene content has oxidized can also lead to irritation. Ex-
pressed oils do spoil quickly, and an opened bottle should be used within 6
months. The case is similar with pine oils. Cinnamon is thought to be responsi-
ble for an adverse reaction to trichlorophenol (TCP), a commonly used antisep-
tic in the United Kingdom (Calnan 1976). Cinnamon is no longer used in this
product.
Sensitivity: Contact Dermatitis
Sensitization to an essential oil is an allergic reaction that occurs over time. At the
first exposure nothing much may happen. However, in a similar manner to some
drug sensitivities (e.g., penicillin), subsequent exposures produce stronger reac-
tions. These reactions can occur in the form of a rash, sneezing, or shortness of
breath. Sensitivity also can occur after long-term habitual use. Considering the
ubiquitous use of fragrance materials in everyday products, the actual risk of side
effects from a fragrance is small (De Groot & Frosch 1997). However, fragrance
allergy is the most common cause of cosmetic contact dermatitis, affecting 1% of
the population. Of greatest concern are the “fragrance-free” products that still
contain fragrance raw materials (Scheinman 1997).
On June 20, 2001, a meeting was held at the British Fragrance Association
in London to propose European Economic Council legislation requiring labeling
for the fragrance product industry. The proposal stated approximately 20 chemi-
cals thought to be allergens would need to be listed on future labels. This legisla-
tion would apply if any of the chemicals constituted 0.001% of the product or
more. The chemicals are common, occurring in essential oils such as linalol and
geraniol. There was no differentiation between synthetic and natural chemicals.
The label was to state “Can cause an allergic reaction.” This kind of labeling could
be enforced in the United States. Although it is laudable to try to curb the on-
slaught of synthetic aromas that bombard shoppers in every mall, labeling an es-
sential oil as a potential sensitizer because it contains something on a list gives the
wrong impression. Rose and lavender soaps have been used for hundreds of years
without incident. However, now that synthetic fragrances are introduced into al-
most every product, sensitivity may well increase.
Some reactions may build up throughout many years. Juniper took 25 years
to produce sensitivity in the case of a lady who sold food smoked and spiced in
Chapter 4 Essential Oil Toxicity and Contraindications 85

juniper oils. Eventually she developed a dry cough and asthma. Skin tests showed
sensitivity to juniper, although it was not established whether the wood resin or
the berries were to blame (Roethe et al 1973). In another instance, a 53-year-old
woman who was patch tested suddenly had eczema appear on various uncovered
parts of her skin: her neck, hands, and scalp (Schaller & Korting 1995). The
woman had been using aroma lamps continuously for more than a year in her
home, and it was presumed she had become sensitive to the scents of lavender,
jasmine, and rosewood. It is not clear whether she had been using pure essential
oils. However this example does underline that the same essential oils should not
be used continuously or as “blanket cover.”
I have found that patients taking several medications at the same time are
more likely to be sensitive to essential oils than patients who are not taking sev-
eral medications. Those who have an allergy-like illness such as asthma, eczema,
or hay fever may also be more sensitive to potential allergenic components, such
as lactones, found in essential oils. A florist who presented with an allergic reac-
tion to Roman chamomile (Chamaemelum nobile) was found to have a prior sen-
sitivity to chamomile herbal teas and ointments (Van Ketel 1982). Another
florist, who had had dermatitis of the face for 1 year, was found to be allergic to
the sesquiterpenes in German chamomile (Matricaria recutita) (Van Ketel 1987).
Lavender, thought to be the safest of all essential oils, caused an allergy in a hair-
dresser who used lavender shampoo several times a day for several years. The al-
lergen involved was believed to be linalol or linalyl acetate (Brandao 1986).
Sometimes the mixture of a chemical and an essential oil can trigger an al-
lergic reaction. This was the case when an aromatherapist sprayed her roses with
an insecticide, and 24 hours later developed acute, bilateral hand eczema. She had
been using French marigold (Tagetes patula) on a patient. The oil had been ob-
tained by solvent extraction (so it was not a true essential oil). Tests showed the
allergic reaction was caused by a cross-reaction between the synthetic pyrethroid
in the insecticide and the acetone-soluble extract of the marigold leaves and flow-
ers (Bilsland & Strong 1990). French marigold is an unusual choice in aro-
matherapy; it smells unpleasant and always needs to be used with caution because
of its high percentage of tagetone, which can cause skin reactions. Its main use is
in the treatment of fungal infections, but it has been mostly replaced by tea tree
oil. One wonders whether the aromatherapist believed she was using common
marigold (Calendula officinalis), which is a nonirritant and is used for its power-
ful skin-healing properties.
Citral is a potential sensitizer on its own, but essential oils of lemongrass and
melissa, which contain high percentages of citral, rarely produce sensitivity reac-
tions when used in aromatherapy. The presence of d-limonene in the essential oils
may produce a quenching effect. The wide range and complexity of components
in essential oils suggests that nature is offering a “balanced menu” so the receiver
can take the parts of the meal the body needs and leave the rest. This may be why
the effect of an isolated ingredient can be much stronger: it is no longer part of
the “balanced menu”.
86 Section I Overview

Sandalwood, thyme, and guaiacwood oils have caused sensitivity in those
sensitive to balsams (Tisserand & Balacs 1995). Sandalwood causes frequent al-
lergic reactions, which are thought to be related to its b-santalol content
(Nakayama et al 1974). Geraniol is a component of many perfumes and may
cause cross-sensitivity in those who have used perfumed products for many years.
Ylang ylang may cause a similar problem.
The most common allergic skin reaction is a stinging, painful wheal or gen-
eralized urticaria. These reactions are sometimes accompanied by bronchial in-
flammation producing asthmalike symptoms (Watt 1991). Even tea tree oil, so
often recommended for its gentleness, has produced contact dermatitis when used
undiluted on the skin of someone allergic to a component found within tea tree.
In this particular case, the actual oil used was found to have a high eucalyptol con-
tent (De Groot & Weyland 1992). Another name for eucalyptol is 1,8-cineole,
which is an oxide. However, tea tree oil is supposed to have a high content of 1-
terpinen-4-ol, an alcohol, and a low proportion of 1,8-cineole.
Sieben et al (2001) investigated the effect of eight common components of
fragrances on 32 fragrance-allergic patients who had previously responded with a
positive skin-patch test. The eight common components studied were eugenol,
isoeugenol, geraniol, oak moss, a-amyl-cinnamic aldehyde, cinnamic aldehyde,
cinnamic alcohol, and hydroxycitronellal. These are the most common observed
contact allergens (Marks et al 1998). Data indicated positive patch tests are a cell-
mediated, antigen-specific phenomenon rather than a nonspecific irritating con-
dition. The authors believed the increase in fragrance allergies was a response to
the indiscriminate use of fragrances in food, household products, paint, and med-
icines. Larsen (2000) suggests cosmetic labels should include a list of common
fragrance allergens so people will know to avoid those to which they are allergic.
Phototoxicity
Phototoxicity is an interaction between a component in an essential oil, the skin,
and ultraviolet photons. This means exposure to sun-bed radiation or natural sun-
light can produce a skin reaction. Such reactions can vary from pigmentation of
the skin to severe full-thickness burns. The most common components causing
phototoxicity are furanocoumarins. Lemon oil contains oxypeucedanin and
bergapten, both furanocoumarins that produce phototoxic reactions. Lime
and bitter orange oils also contain these components, but in smaller quantities
(Naganuma et al 1985). Angelica root oil contains furanocoumarins and can also
produce phototoxicity (Tisserand & Balacs 1995).
Bergamot was used in self-tanning preparations until 12 cases of skin reac-
tion were reported after the use of this type of product. In two cases (in which
skin had been exposed to the sun immediately after application of the tanning
cream) symptoms of erythema as well as pigmentation were present (Meyer
1970). However, furanocoumarins can be removed from bergamot oil. The oil is
then classified as bergaptene-free or furanocoumarin-free (FCF). Some therapists
will not use FCF essential oils, and some distributors will not supply them,
Chapter 4 Essential Oil Toxicity and Contraindications 87

saying they will only use “whole” oils. However in areas with lots of sunshine,
FCF oils might be safer. Deterpenated citrus oils contain disproportionately
higher concentrations of furanocoumarins and are best avoided.
Chemical Burns
Parys (1983) reported on undiluted peppermint oil inadvertently spilled on skin
that had already been traumatized by skin grafts. The area necrosed and required
excision and further surgery.
Chronic Toxicity
Chronic toxicity is a term usually referring to the oral use of essential oils.
Chronic toxicity is dose-dependent but also related to the length of time spent
using a toxic substance. Death may eventually occur, but it is the preceding slow
tissue damage that is the main problem. It is unlikely that inhaled or topically ap-
plied essential oils would cause chronic toxicity, even if large amounts were used
over extended periods.
Reactions with Orthodox Drugs
Drug Combinations and Pharmacokinetics
Blashke and Bjornsson (1989) define an interacting drug combination as “one
that has the potential, documented in humans, to produce a clinically significant
change in the pharmacologic response to its constituent drugs that is larger or
smaller than the sum of the effects when the drugs are administered separately.”
Hansten and Horn (1989) estimate that 7.4% of all hospitalized patients experi-
ence an interacting drug combination during their hospital stay. Compounding
this problem is the knowledge that individual patients respond in varying ways to
the same dose of the same drug. This variation is thought to be directly related to
pharmacokinetics: the mathematical description of the rate and extent of absorp-
tion, distribution, and elimination of drugs in the body (Gwilt 1994). These three
processes determine the movements of drugs within the body. However, despite
advances in understanding, a great deal is not yet known about drug combinations
and pharmacokinetics.
Because there are documented differences between individuals with regard
to the absorption of several orthodox drugs like phenytoin and digoxin, it is ex-
pected that the absorption of essential oils will also vary. Absorption depends on
the mode of delivery; the transdermal route is thought to be slower and more
controlled. It is thought to reduce the difference between the maximum and
minimum drug concentrations attained during a dosing interval (Blaschke &
Bjornsson 1995). The distribution of any drug is controlled by blood flow to
the tissue or organ, as well as by the drug’s ability to bind to plasma proteins.
Distribution is also related to whether the drug molecules are lipid-soluble or
water-soluble.
88 Section I Overview

Elimination takes place at the same time as distribution and occurs primar-
ily in the kidneys, although metabolism (which can include deactivation) occurs
in the liver. Metabolism is the mechanism whereby drug action is terminated or,
in the case of drugs such as aspirin, activated (Grant 1994). Some lipid-soluble,
nonionized drugs can be completely reabsorbed in the liver. This metabolism in-
cludes a chemical conversion that allows the drug (or essential oil) to become
more water-soluble, and therefore easier to excrete in the urine. Essential oils that
are inhaled or applied topically do not go through the first stage of metabolism
by the liver (Price & Price 1999).
Because they are lipid-soluble, components within essential oils gain easy ac-
cess to the brain. While being transported by the bloodstream, the components
travel readily to the adrenal glands and kidneys (Tisserand & Balacs 1995). The
rate of elimination of a drug from the body is proportional to the concentration
of that drug in the bloodstream. It is a complicated equation because the drug (or
essential oil) begins to be eliminated while it is still being absorbed (Balazs 2002)
In most instances, the biologic half-life (t
1/2
), rather than the elimination rate, is
documented. The half-life is the time taken for the drug concentration in the
blood to decrease by one half. It depends on both the volume of distribution of
the drug and the rate at which that drug is eliminated from the body (known as
clearance) (Gwilt 1994).
Drugs and essential oils are excreted via the kidneys, lungs, skin, and feces.
In addition, many nursing mothers also excrete drugs, and therefore components
of essential oils, in their breast milk (Berndt & Stitzel 1994). Theoretically, es-
sential oils could interact with orthodox drugs in several ways: by combining with
a cellular receptor (and thereby competing with the drug), by combining with
plasma protein, or by combining with and somehow altering the chemistry of the
drug to produce a different compound with different effects (Tisserand & Balacs
1995).
Cellular Receptors
Most drugs combine with a molecular structure called a receptor, which is found
on the surface of cells. This produces a molecular change in the receptor and leads
to a chain of events called a response. The same situation occurs with naturally
formed neurotransmitters and hormones secreted by the body itself. Some drugs
produce the same effects as naturally occurring substances because they combine
with the same receptors at a cellular level. An example of this is morphine mim-
icking the effects of endorphins (Fleming 1994).
It is known that receptors only react with a limited number of substances that
have a similar molecular structure. Therefore an essential oil with a molecular
structure similar to that of a drug known to bind to a particular receptor may also
combine with that receptor. An example of this is anethole and its polymers, di-
anethole and photoanethole, which bear a striking resemblance to the cate-
cholamine dopamines adrenaline and noradrenaline (Albert-Puleo 1980). Also
worthy of mention are the nonsteroidal compounds with estrogenic activity found
Chapter 4 Essential Oil Toxicity and Contraindications 89

in plants, which mimic the A-ring of steroids (Murad & Kuret 1990). However,
just because a molecule has a similar structure does not mean it will mimic a neu-
rotransmitter (Balazs 2002).
Combining at the Plasma Level
Most drugs found in the vascular compartment bind with one of the macromol-
ecules in the plasma. Compartmental modeling is used as a theoretical vehicle for
assessing the distribution of drugs (Blaschke & Bjornsson 1995). This binding is
reversible because only an unbound drug can diffuse through the capillary wall,
produce systemic effects, be metabolized, and then be excreted. As the macro-
molecule circulates within the bloodstream, so the vascular system works as a hu-
man drug distributor.
There is no reason to suppose an essential oil could not also bind with plasma
proteins. It could bind with one of the most important plasma proteins, albumin,
because most albumin-bound drugs are only slightly soluble in water. Drug bind-
ing at this level is nonspecific, and displacements frequently occur when a newer
drug with a higher affinity comes along.This means the previous drug is suddenly
free to be distributed to another part of the body. In some diseases, such as ure-
mia, plasma-protein binding is reduced.
Changing the Action or Potency of a Drug
Certain components found in essential oils aid the penetration of drugs through
the skin of animals (Williams & Barry 1989). Therefore it is possible that the
topical application of an essential oil could increase the level of drug being re-
ceived by a patient using patch therapy (e.g., hormone replacement therapy) if the
oil is applied at the site of drug absorption. However, no documented informa-
tion has confirmed this yet.
Freitas et al (1993) found that b-myrcene affected the metabolism of barbi-
turates in rats. The rats were given b-myrcene orally 1 hour before an intraperi-
toneal injection of pentobarbital. This enhanced the sleeping time and was at-
tributed to the pentobarbital-biotransforming enzymes found in b-myrcene.
However, when b-myrcene was given 1 day before the barbiturate injection, the
sleeping time was reduced by 50%. b-myrcene is found in lemongrass (Sheppard-
Hangar 1995).
Wintergreen and sweet birch are essential oils not commonly used in aro-
matherapy, mainly because they contain high levels of methyl salicylate (closely
related to acetylsalicylic acid or aspirin). Some safety data manuals call them haz-
ardous (Tisserand & Balacs 1995; Anonymous 1993). However, they are found in
many proprietary creams (such as Deep Heat) for sprains and strains, as well as
in chewing gum and candy (Guba 2000). Wintergreen and sweet birch essential
oils are easy to purchase. Guba (2000) suggests that 10 ml of a 2.4% mix of win-
tergreen in carrier oil would give approximately 250 mg methyl salicylate, equiv-
alent to one tablet of aspirin. Methyl salicilate is absorbed through the skin and
can affect warfarin anticoagulation therapy (Littleton 1990; Yip et al 1990). Guba
90 Section I Overview

(2000) suggests that because only 50% of methyl salicilate would be absorbed, the
amount produced from wintergreen oil in this experiment would be no more toxic
than rubbing half an aspirin on the skin. However, aspirin is known to affect the
blood-clotting mechanism and prostaglandin production. The combination of
regular amounts of an aspirinlike substance (wintergreen) and warfarin could lead
to hemorrhage. Collins et al (1984) showed that blood salicylate reached maxi-
mum level 20 minutes after Deep Heat cream was applied to the skin. Guba
(2000) recommends not using wintergreen for full body treatments or when the
patient is taking warfarin or some other anticoagulant therapy. However, several
proprietary brands of creams for arthritis contain similar acetylsalicylic acid-like
components and do not offer warnings. Many volatile chemicals are absorbed
though the skin (Riviere et al 1997). There seems to be a question as to whether
essential oils reach the bloodstream in sufficient quantities after a topical aro-
matherapy treatment to have a pharmacologic effect (Balazs 2002).
Essential oils containing b-asarone or d-pulegone may increase the toxic ef-
fects of a drug because they both induce the detoxifying enzyme cytochrome
P450. (These substances are found in essential oils that are rarely used because
they are thought to be toxic themselves.) Drugs that induce this enzyme include
progestogens (found in the contraceptive pill), diphenhydramine (an antihista-
mine), pethidine, nitrazepam, phenobarbitone, and phenytoin, the last four being
frequently used hospital drugs (Tisserand & Balacs 1995). Fortunately, very few
essential oils contain b-asarone or d-pulegone, and few that do are in regular use.
They include wintergreen, cultivated carrot seed, calamus (which contains
b-asarone), and pennyroyal (which contains d-pulegone). Madhava-Madyastha
and Chadha (1986) found that 1,8-cineole, administered by inhalation, induced
the liver microsomal cytochrome P450 to a significant extent in rats. However,
Tisserand and Balacs (1995) state the amounts used in aromatherapy is insuffi-
cient to induce changes in cytochrome P450 activity. Chiou et al (1997) found
that beta-uedesmol, a sesquiterpene found in West Indian sandalwood, alleviated
electric shock-induced seizures in rat tissue and may enhance the effect of
epilepsy drugs such as phenytoin.
A study by Perez Raya et al (1990) has shown that two different species of
mint enhance the effect of pentobarbitone in rats. Both Mentha rotundifolia and
Mentha longifolia significantly enhanced sodium-pentobarbital induced sleep.
Lavender was also shown to enhance sodium-pentobarbital-induced sleep in rats,
although the effect ceased if treatment lasted longer than 5 days (Delaveau et al
1989). Guillemain et al (1989) also demonstrated the ability of lavender (Lavan-
dula angustifolia) to enhance neurodepressant effects. However, these findings are
a long way from proving a similar action on enzymes in humans.
Almirall et al (1996) found that 1,8-cineole, d-limonene, and pinene perme-
ated the skin and affected topical application of conventional drugs such as
haloperidol and chlorpromazine. Whereas 1,8-cineole and d-limonene enhanced
the transdermal permeability of haloperidol, d-limonene reduced the transdermal
permeability of chlorpromazine. The oxide 1,8-cineole (also called eucalyptol) is
Chapter 4 Essential Oil Toxicity and Contraindications 91

found in rosemary, cardamon, spike lavender, sage, and eucalyptus (Bowles 2000),
and d-limonene is found in many citrus-peel oils.
Jori et al (1969) studied the effects of several components of essential oils on
the metabolism of drugs in rats. The components, which were delivered by aerosol
or subcutaneously, were eucalyptol (1,8-cineole), guaiacol, menthol, and essential
oil of Pinus pumilio (which contained a-pinene, phellandrene, dipentene,
sylvestrene, and bornyl acetate). Eucalyptol was shown to increase the activity of
the microsomal enzymatic reaction and altered the metabolism of drugs. The dis-
appearance rate from brain and plasma of amphetamine and pentobarbital was
increased after eucalyptol administration, but eucalyptol had no influence on
phenylbutazone. An increased plasma disappearance was also shown to occur in
humans after 10 days’ treatment with eucalyptol aerosol.
Hohenwaller and Kima (1971) found that eucalyptol, either given subcuta-
neously or by aerosol, raised in vivo phenobarbital metabolism. The change of en-
zyme activity with time resembled the change of drug concentration in blood
serum. The mechanism of eucalyptol appeared to be quite different from the
mechanism of phenobarbital in three ways. First, unlike the rapid decrease of
phenobarbital, eucalyptol disappeared gradually. Second, enzyme activity contin-
ued after the end of treatment with eucalyptol. Third, a single treatment of euca-
lyptol caused reduction in enzyme activity, but several doses of phenobarbital
were required. Hohenwaller and Kima (1971) concluded “many other mecha-
nisms beside enzyme synthesis must be involved in producing the striking differ-
ences on the action of the two drugs.” Eucalyptol is used extensively in the phar-
maceutical preparations for external application and as a nasal spray. However,
Tisserand and Balacs (1995) state that because essential oils are used in such small
amounts compared with orthodox drugs, even if they are given orally, they are un-
likely to affect the therapeutic action of most orthodox pharmacology.
Certain essential oils may react with other medications. In some instances es-
sential oils may enhance the effects of orthodox drugs, whereas in other cases they
may interfere at a cellular level, reducing the effectiveness of medication. Ylang
ylang (Cananga odorata) enhances the dermal absorption of 5-Fluorouracil sev-
enfold (Williams & Barry 1989). Blue gum eucalyptus (Eucalyptus globulus) en-
hances the activity of streptomycin, isoniazid, and sulfetrone in Mycobacterium tu-
berculosis (Kufferath & Mundualgo 1954; Guillemain et al 1989). Eucalyptol
(1,8-cineole) found in gully gum (Eucalyptus smithii), and blue gum eucalyptus
(E. globulus and E. fruticetorum) produced a significant decrease in pentobarbital
effects and dose-related effects on the liver-enzyme activity of rats ( Jori et al
1969). The reduction in sedative effect occurred even when the eucalyptus had
been administered 36 hours previously.
Roman chamomile (Chamaemelum nobile) was found to be incompatible with
the administration of products containing Peruvian bark, tannin, or silver salts
(Chiej 1984). These are sometimes present in old-fashioned preparations used for
pressure-area care.
92 Section I Overview

Acetaminophen (paracetamol) is a common analgesic that reduces the level
of glutathione in the liver. Glutathione is responsible for absorbing free radicals,
and when the level of glutathione falls, reactive molecules such as free radicals can
attack the liver cells with potentially fatal consequences. It is extremely unlikely
that the small amounts of essential oils used in aromatherapy could adversely af-
fect glutathione production. However, in a patient using the maximum recom-
mended dosage of Tylenol, it might be advisable to avoid essential oils containing
transanethole, estragole, and eugenol (Tisserand & Balacs 1995). This means
avoiding the following essential oils: fennel (Foeniculum vulgare), aniseed
(Pimpinella anisum), basil (Ocimum basilicum), and clove (Syzygium aromaticum).
Terpineol is thought to enhance prednisolone absorption through the skin
(Williams & Barry 1989). Terpineol is found in many essential oils, including
niaouli, ravansara, and tea tree. Godwin and Michniak (1999) found that
terpinen-4-ol and a-terpineol enhanced the dermal penetration of hydrocortisone
four to five times in mice. Both of these chemical components are found in tea tree
oil. Limonene is thought to increase indomethacin absorption through the skin.
Indomethacin is a drug commonly used in arthritis. Limonene is a monoterpene
that occurs in many essential oils from citrus peels. Menthol lowers the melting
point of testosterone (which is solid at room temperature) and increases the per-
meation of testosterone through the skin eightfold (Kaplun-Frischoff & Touitou
1997). Bowles (2000) suggests that there could be a remote possibility of myris-
ticin (found in nutmeg) compounding the effect of serotonin-altering drugs.
Cedarwood (Cedrus atlantica) reduces the effect of barbiturate-induced sleep
(Wade et al 1968). This study also showed that cedarwood could reduce the
amount of dicoumarol in the blood. Dicoumarol is an anticoagulant that can be
obtained from sweet clover (Budavari 1996). Eugenol has been shown to have an-
tiplatelet activity ( Janssens et al 1990), and should be avoided in patients receiv-
ing anticoagulant therapy. Eugenol occurs in clove leaf and bud, pimento berry
and leaf, and cinnamon leaf. Cinnamon leaf is thought to depress liver glu-
tathione levels in rats and may interfere with the body’s metabolization of acet-
amionphen.
Finally, some patients with particular enzyme deficits or specific conditions
may be affected by certain essential oils. Male children of Chinese, West African,
Mediterranean, and Middle Eastern origin are susceptible to a deficiency of
glucose-6-phosphate dehydrogenase. This enzyme is responsible for liver detoxi-
fication of menthol. When the enzyme is missing, toxic build-up of menthol can
occur (Owole & Ramson-Kuto 1980). Large amounts of peppermint should be
avoided in these children.
Rosemary has been shown to interfere with calcium influx into the myocar-
dial cells (Tisserand & Balacs 1995) and should be not be used orally in cardiac
patients. Patients with glaucoma should avoid taking oral citral-rich essential
oils (Leach & Lloyd 1956). Tisserand and Balacs (1995) suggest that hormone
replacement therapy (HRT) is not adversely affected by aromatherapy because
Chapter 4 Essential Oil Toxicity and Contraindications 93

the hormonal effect of the essential oil is considerably weaker than the effect of
the HRT.
Essential Oils and Homeopathy
Although Hippocrates may have been the first to say “like cures like,” this tenet
is associated with homeopathic medicine, which dates back to 1810 and Samuel
Hahnemann, a German physician. Hahnemann discovered that cinchona bark
taken by a healthy person produced the symptoms of malaria. At that time, cin-
chona bark was administered as a herbal remedy to cure malaria. (Much later cin-
chona bark was found to contain quinine, a component that became a classic drug
to treat malaria.) Hahnemann thought giving a minute dose of the substance that
may have caused the disease would stimulate the body to fight that disease.
He tested this hypothesis on himself and his family, compiling a huge ency-
clopedia of knowledge that now forms the foundation of homeopathic literature.
The first homeopathic hospital opened its doors in 1850. In addition to “like cures
like,” homeopaths believe the more diluted the dose, the more potent it may be. Of-
ten their medicines are so diluted that there are no molecules of medicine left in
them. This has caused much derision among members of the medical profession,
who feel that leaving the curing of the patient to the “learned memory of water” is
something of a joke. However, rigorous scientific studies are now showing that
homeopathy is indeed a valid and useful form of medicine (Kleijinen et al 1991).
There is some controversy among homeopaths concerning the use of essen-
tial oils for patients receiving homeopathy. The traditional view has always been
that essential oils and homeopathic remedies do not mix. Many aromatherapy
courses teach that the two should not be combined. They are very different ther-
apies at opposite ends of the spectrum—one very concentrated and one very di-
lute. Peppermint, eucalyptus, thyme, and essential oils with strong aromas are
some of those best avoided by patients using homeopathy.
Stevensen (1995), who worked for many years using both homeopathy and
essential oils on a daily basis, wrote “I would find it difficult to envisage a clash of
effects between homeopathy and aromatherapy.” However, the safest option is to
restrict the choice of essential oil to florals such as rose, lavender, geranium, neroli,
and the softer herbs.
Specific Contraindications
Some essential oils are contraindicated in certain aromatherapy situations, or con-
traindicated altogether, although they may be used as food flavorings or in per-
fumery. The amount of essential oil used in flavoring is often very tiny. For ex-
ample, mustard, a well-known flavoring, is contraindicated in aromatherapy
because it is extremely toxic. Tisserand and Balacs (1995) describe the dose used
by the food industry as one-hundredth of a drop of mustard to 50 g of pickle. It
would be impossible to measure one-hundredth of a drop in aromatherapy.
94 Section I Overview

However, if just one drop was used (1%), the resulting dilution would be 1000
times greater than that in pickles!
There are several safety data manuals available that go into detail regarding
why some essential oils are contraindicated. Essential Oil Safety (Tisserand &
Balacs 1995) is particularly recommended. If hospitals are to become involved in
the use of essential oils, they should have a safety data manual. Hazardous oils are
still on sale in many health-food shops, and sometimes in bottles without inte-
grated droppers.
Some essential oils are generally contraindicated for all therapeutic uses.
These include boldo leaf, calamus, cassia, bitter fennel, mugwort, mustard, rue,
sassafras, tansy, wintergreen, and wormwood. These oils all contain toxic con-
stituents. The essential oils contraindicated for undiluted topical application in-
clude oregano, clove bud and leaf, cinnamon bark, camphor, and red thyme. Es-
sential oils that should be used with caution in patients with hypertension include
rosemary, spike lavender, hyssop, juniper, thyme, and clove, although there is no
published report of blood pressure being substantially raised by essential oils.
Contraindicated in patients with epilepsy are hyssop, fennel, peppermint, and
rosemary, although there is no published report of any of these triggering a
seizure. However, Guba (2000) writes that large doses of ketones, in particular
camphor, pinocamphone, pulegone, and thujone have been found to cause
seizures (NDPSC 1998).
Contraindications in Oncology
Some malignant growths depend on estrogen, so perhaps the use of essential oils
that are mildly estrogenlike should be avoided. However, soy products, which also
contain phytoestrogens, have cancer-fighting compounds (Weil 1998), so estro-
gen stimulating or estrogenlike essential oils may be good for estrogen-dependent
tumors. Barrett (1997) gives an interesting discussion of the pros and cons of us-
ing phytoestrogens. Franchomme & Penoel (1991) list the specific chemical com-
ponents associated with estrogen stimulation or estrogenlike properties as sclareol
and viridiflorol (sesquiterpenic alcohols), anethole (a phenyl methyl ether), and
“certain” ketones not specified. Citral was found to have an estrogenic action by
Geldof et al (1992). Animal studies suggest the topical use of citrus-peel oils such
as bergamot should be avoided in patients who have a history or symptoms of
melanoma (Elegbede et al 1986).
Contraindications in Pregnancy
The use of essential oils in pregnancy is a contentious subject, especially during
the vital first 3-month period. Some aromatherapists will not treat expectant
mothers. Because lipophilic substances can diffuse between two circulations, it is
likely that essential oils cross the placenta (Burfield 2001). Balacs suggests the
best advice is to “urge caution when giving oils to pregnant women and to avoid
pennyroyal at all costs.” However, to put this in context, remember that perfume
does not carry a warning not to be used in pregnancy. It is extremely unlikely that
Chapter 4 Essential Oil Toxicity and Contraindications 95

a nightly bath containing a few drops of essential oil will cause any problems for
the unborn child.
Many midwives are happy to use essential oils during labor to promote con-
tractions and for their analgesic properties. Mason (1996) suggests avoiding es-
sential oils during the first 24 weeks of pregnancy. Tiran suggests avoiding them
during the first trimester only (1996). Several hospital labor units using essential
oils during labor and delivery report that aromatherapy is useful, safe, and pleas-
ant. More details on obstetrics can be found in Chapter 21.
Safety and Storage of Essential Oils
Safety
Aromatherapy requires knowledge, and yes, in the wrong hands, essential oils can
be hazardous. Just like Tylenol and aspirin, which can be bought over the counter
almost anywhere, essential oils should always be kept away from children. See
Table 4-2 for potentially lethal dosages in children.
If a child appears to have drunk several spoonfuls of essential oil, contact the
nearest poison unit (often listed in the front of a telephone directory). Keep the
bottle for identification and encourage the child to drink whole milk. Do not try
to induce vomiting. If essential oils (diluted or not) get into the eyes it is impor-
tant to irrigate the eyes as rapidly as possible with whole milk or carrier oil fol-
lowed by water and then to seek medical help. If there is a skin reaction to an es-
sential oil, dilute the essential oil with carrier oil, then wash the area with a
nonperfumed soap. The majority of the components found in essential oils are
nonpolar; therefore essential oils do not mix well or dissolve in water.
Storage
Essential oils are powerful, and it is important that they be stored away from chil-
dren, the confused, or those unaware of what essential oils are. It takes just 4 ml
(less than a teaspoonful) of ingested blue gum eucalyptus to produce severe ef-
fects. Gurr & Scroggie (1965) reported on a case that necessitated emergency
peritoneal dialysis, hemodialysis, and a mannitol infusion.
Essential oils kept in a hospital should be stored in a locked container. If
stored in a cool, dry, dark place, undiluted essential oils can stay fresh for up to 6
years. They should be kept in colored (blue or amber) glass bottles to protect them
from ultraviolet light, with the bottles sealed. Bottles should have an integral drop-
per contained in the lid to prevent spillage. All opened bottles should be stored
away from heat and sunlight (ideally in a refrigerator, similar to the storage of hep-
arin). All bottles should carry a firmly attached label, stating the botanical name,
the supplier’s name, and the batch number. Most reputable companies also include
a label warning that the oils should be kept away from the eyes, out of reach of
children, and not be taken by mouth. Some also have a note printed on them stat-
ing they are of medicinal strength. It is helpful to keep a record of when each es-
96 Section I Overview

sential oil was purchased, the supplier’s name, and the price. A separate list should
be kept with the patient’s name, the name of the physician, the dates the patient
received aromatherapy, and any therapeutic (or adverse) results. Recording this in-
formation makes a portfolio on the use of essential oils easily available.
Essential oils are highly flammable, so they must be stored away from open
flame such as candles, fire, matches, cigarettes, and gas cookers. Sprinkling them
on top of light bulbs is not a good idea!
Although essential oils have been used for thousands of years, there have been
few recorded cases of sensitivity, allergy, or fatality. Lovell (1993) suggests that the
family Lamiacea, which contains many aromatic plants used in perfumery, cook-
ing, and medicine, could possibly produce allergic contact dermatitis. He cites
Canlan, who recorded six positive reactions to lavender oil patch tests in 1147
Chapter 4 Essential Oil Toxicity and Contraindications 97
Table 4-2 h Potentially Lethal Oral Doses of Essential Oil for a Child.
Oral Lethal Dose
Common Name Botanical Name for a Child
Basil Ocimum basilicum 8 ml
(estragole above 55%)
Aniseed Pimpinella anisum 25 ml
Clove Syzygium aromaticum 19 ml
Eucalyptus Eucalyptus globulus 5 ml
Hyssop Hyssopus officinalis 19 ml
German spearmint Mentha longifolia 6.5 ml
Egyptian round leaf Mentha rotundifolia 10 ml
Oregano Oreganum vulgare 21 ml
Parsley seed oil Petroselinum sativum 21 ml
Pennyroyal Mentha pulegium 3 ml
Sage Salvia officinalis 26 ml
Savory, Summer Satureja hortensis 19 ml
Tansy No botanical name given 5 ml
Tarragon No botanical name given 26 ml
Thuja Thuja occidentalis 10 ml
Wintergreen Methyl salicylate 5 ml
Adapted from Watt M. 1991. Essex, UK: Witham. This book discusses adverse reactions and
toxicity in greater detail. Not all the botanical names are given.

patients. The incidence of adverse reactions to essential oils is considerably lower
than the incidence of adverse reactions to synthetic drugs, and the reactions are
generally less severe. However, this could be because essential oils are used much
less often than orthodox drugs. In a Japanese study carried out between 1990 and
1998, a 2-day, closed patch test using 2% essential oil of lavender on people who
had suspected cosmetic contact dermatitis found a sudden increase in reactions for
the year 1997 (Sugiura et al 2000). Researchers suggested this increase could be
due to the trend of placing lavender flowers in pillows and drawers. Essential oils
are wonderful things, but over-use may lead to sensitivity—even with the ubiqui-
tous lavender.
REFERENCES
Albert-Puleo M. 1980. Fennel and anise as estrogenic agents. Journal of Ethnopharma-
cology. 2(4) 337-344.
Almirall M, Montana J, Escribano E et al. 1996. Effect of d-limonene, alpha-pinene and
cineole on in vitro transdermal human skin penetration of chlorpromazine and
haloperidol. Arzneimittelforschung. 46(7) 676-680.
Balacs T. 1992. Safety in pregnancy. International Journal of Aromatherapy. 4(1) 12-15.
Barrett E. 1997. Environmental health: Phytoestrogens. Focus. 104(5). Retrieved Sep-
tember 2002 from http://ehpnet1.niehs.nih.gov/docs/1996/104(5)focus.html.
Bartlett J. 1977. Bartlett’s Familiar Quotations, 14th ed. London: Macmillan Press, 208.
Berndt W, Stitzel R. 1994. Excretion of drugs. In Craig C, Stitzel R (eds.), Modern
Pharmacology. Boston: Little, Brown & Co., 47-53.
Bilsland D, Strong A. 1990. Allergic contact dermatitis from the essential oil of French
marigold (Tagetes patula) in an aromatherapist. Contact Dermatitis. 23(1) 55-56.
Blaschke T, Bjornsson T. 1995. Pharmacokinetics and pharmacoepidemiology. Scientific
American. 8:1-14.
Bowles J. 2000.The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Printers.
Brandao F. 1986. Occupational allergy to lavender oil. Contact Dermatitis. 15(4)
249-250.
Budavari S (ed.). 1996. Merck index, 12th ed. Whitehouse Station, NJ: Merck & Co.
Inc.
Burfield T. 2001. Safety of essential oils. International Journal of Aromatherapy. 10(1/2)
16-30.
Calnan C. 1976. Cinnamon dermatitis from an ointment. Contact Dermatitis. 2(3)
167-170.
Chiej R. 1984. The Macdonald Encyclopedia of Medicinal Plants. London: Macdonald.
Chiou L, Ling J, Chang C. 1997. Chinese herb constituent beta-eudesmol alleviated the
electroshock seizures in mice and electrographic seizures in rat hippocampal slices.
Neuroscience Letters. 231(3) 171-174.
Collins A, Notarianni L, Ring E et al. 1984. Some observations on the pharmacology of
‘deep-heat,’ a topical rubifacient. Annals of Rheumatic Diseases. 43(3) 411-415.
De Groot A, Weyland J. 1992. Systemic contact dermatitis from tea tree oil. Contact
Dermatitis. 27(4) 279-280.
98 Section I Overview

De Groot A, Frosch P. 1997. Adverse reactions to fragrances. Contact Dermatitis. 36(2)
57-86.
Delaveau P, Guillemain J, Marcisse, G et al. 1989. Neuro-depressive properties of essen-
tial oil of lavender (French). Comptes Rendus des Séances de la Societié de Biologie
et de ses Filiales. 183(4) 342-348.
Elegbede J, Maltzman T, Verma A et al. 1986. Mouse skin tumor promoting activity of
orange peel oil and d-limonene: A re-evaluation. Carcinogenesis. 7(12) 2047-2049.
Fleming W. 1994. Mechanisms of drug action. In Craig C, Stitzel R (eds.), Modern
Pharmacology. Boston: Little, Brown & Co., 9-18.
Freitas J, Presgrave O et al. 1993. Effect of b-myrcene on pentobarbital sleeping time.
Brazilian Journal of Medical and Biological Research. 26(5) 519-523.
Geldof A, Engel C, Rao B. 1992. Estrogenic action of commonly used fragrant agent
citral induces prostatic hyperplasia. Urology Research. 20(2) 139-144.
Godwin D, Michniak B. 1999. Influence of drug lipophilicity on terpenes as trans-
dermal penetration enhancers. Drug Development & Industrial Pharmacy. 25(8)
905-915.
Grant T. 1994. Metabolism of drugs. In Craig C, Stitzel R (eds.), Modern Pharmacol-
ogy. Boston: Little, Brown & Co., 33-46.
Guba R. 2000. Toxicity myths: The actual risks of essential oil use. International Journal
of Aromatherapy. 10(1/2) 37-49.
Guillemain J, Rousseau R, Delaveau P. 1989. Neurodepressive effects of the essential oil
of Lavandula angustifolia. Annales Pharmaceutiques Francais. 47(6) 337-342.
Gurr F, Scroggie J. 1965. Eucalyptus oil poisoning treated by dialysis and mannitol infu-
sion, with an appendix on the analysis of biological fluids for alcohol and eucalyptol.
Australasia Annals of Medicine. 14(3) 238-249.
Gwilt R. 1994. Pharmacokinetics. In Craig C, Stitzel R (eds.), Modern Pharmacology.
Boston: Little, Brown & Co., 55-64.
Hansten P, Horn J. 1989. Drug Interactions: Clinical Significance of Drug–Drug Inter-
actions, 6th ed. New York: Lea & Febiger.
Hohenwaller W, Kima J. 1971. In vivo activation of glucuronyl transferase in rat liver by
euacalyptol. Biochemical Pharmacology. 20(12) 3463-3472.
International School of Aromatherapy. 1993. A Safety Guide for the Use of Essential
Oils. London: Nature by Nature Oils.
Janssens J, Laekeman G, Pleters L et al. 1990. Nutmeg oil: Identification and quantifica-
tion of its most active constituents as inhibitors of platelet aggregations. Journal of
Ethnopharmacology. 29(2) 179-188.
Jori A, Bianchetti A, Prestinit P. 1969. Effect of essential oils on drug metabolism. Bio-
chemical Pharmacology. 18(9) 12081-12085.
Kaplun-Frischoff Y, Touitou E. 1997. Testosterone skin permeation enhancement by
menthol through formation of eutectic with drug and interaction with skin lipids.
Journal of Pharmaceutical Science. 86(12) 1394-1399.
Kleijnen J, Knipschild P, ter Riet G. 1991. Clinical trials of homeopathy. British Medical
Journal. 301(6772) 316-332.
Kligman A. 1996. The identification of contact allergens by human assay. Journal of In-
vestigative Dermatology. 47(5) 393-409.
Kufferath F, Mundualgo G. 1954. The activity of some preparations containing essential
oils in TB. Fitoterapia. 25:483-485.
Larsen W. 2000. How to test for fragrance allergy. Cutis. 65(1) 39-41.
Chapter 4 Essential Oil Toxicity and Contraindications 99

Larsen W, Nakayama H, Lindberg M et al. 1996. Fragrance contact dermatitis: a world-
wide multicenter investigation (part 1). American Journal of Contact Dermatitis.
7:77-83.
Leach E, Lloyd J. 1956. Experimental ocular hypertension in animals. Transactions of
the Ophthalmological Societies of the UK. 76:453-460.
Lesesne C. 1992. The postoperative use of wound adhesives. Gum mastic versus ben-
zoin, USP. Journal of Dermatologic Surgery and Oncology. 18(11) 990-991.
Littleton F. 1990. Warfarin and topical salicylates (letter). Journal of the American Med-
ical Association. 263(21) 2888.
Lovell C. 1993. Plants and the Skin. Oxford, UK: Blackwell Scientific Publications.
Madhava-Madyastha K, Chadha A. 1986. Metabolism of 1,8 cineole in rats: Its effect on
liver and lung microsomal cytochrome P-450 systems. Bulletin of Environmental
Contaminants and Toxicology. 37:759-766.
Marks J, Belsito D, DeLeo V et al. 1998. North American Contact Dermatitis Group
patch test results for the detection of delayed-type hypersensitivity to topical allergens.
Journal of the American Academy of Dermatology. 38(6 Pt 1) 911-918.
Mason M. 1996. Aromatherapy and midwifery. Aromatherapy. Quarterly spring issue.
32-34.
Meyer J. 1970. Accidents due to tanning cosmetics with a base of bergamot oil. Bulletin
de la Societé Francaise de Dermatologie et de Syphiligraphie. 77(6) 881-884.
Murad F, Kuret J. 1990. Estrogens and progestins. In Goodman and Gilman’s The Phar-
macological Basis of Therapeutics, 8th ed. New York: McGraw-Hill, 1384-1386.
Naganuma M, Hirose S, Nakayama K, et al. 1985. A study of the phototoxicity of lemon
oil. Archives of Dermatological Research. 278(1) 311-316.
National Drugs and Poisons Schedule Committee (NDPSC) Working Party on Essen-
tial Oils. 1998. Essential Oil Monographs. Canberra: Australian Therapeutic Goods
Administration.
Olleveant N, Humphris G, Roe B. 1999. How big is a drop? A volumetric assay of es-
sential oils. Journal of Clinical Nursing. 8(3) 299-304.
Owole S, Ramson-Kuto O. 1980. The risk of jaundice in glucose-6-phosphate dehydro-
genase deficient babies exposed to menthol. Acta Paediatrica Scandinavica. 69(3) 341-
345.
Parys B. 1983. Chemical burns resulting from contact with peppermint oil: a case report.
Burns Including Thermal Injury (Bristol). 9(5) 374-375.
Perez Raya M, Utrilla M, Navarro M et al. 1990. CNS activity of Mentha rotundifolia and
Mentha longifolia essential oil in mice and rats. Phytotherapy Research. 4(6) 232-234.
Price S, Price L. 1999. Aromatherapy for Health Professionals, 2nd ed. London:
Churchill Livingstone.
Rademaker M, Kirby J. 1987. Contact dermatitis to a skin adhesive. Contact Dermatitis.
16(5) 297-298.
Riviere J, Brooks J, Qiao G et al. 1997. Percutaneous absorption of volatile chemicals.
Airforce Office of Scientific Research G49620-95-1-0017. National Technical Infor-
mation Service Report American Disability Act 1-23.
Roethe A, Heine A, Rebohie E. 1973. Oils from juniper berries as an occupational aller-
gen for the skin and the respiratory tract. Berufs-Dermatosen. 21(1) 11-16.
Schaller M, Korting H. 1995. Allergic airborne contact dermatitis from essential oils
used in aromatherapy. Clinical and Expermental Dermatology. 20(2) 143-145.
100 Section I Overview

Scheinman P. 1997. Is it really fragrance free? American Journal of Contact Dermatitis.
8(4) 239-242.
Sheppard-Hangar S. 1995. The Aromatherapy Practitioner’s Reference Manual, Vol. II.
Tampa, FL: Atlantic Institute of Aromatherapy.
Sieben S, Hertl M, Masaoudi T, et al. 2001. Characterization of T cell responses to fra-
grances. International Journal of Aromatherapy. 11(3) 157-166.
Sugiura M, Hayakawa R, Kato Y et al. 2000. Results of patch testing with lavender oil in
Japan. Contact Dermatitis. 43(3) 157-160.
Tiran D. 1996. Aromatherapy in midwifery: Benefits and risks. Complementary Thera-
pies in Nursing and Midwifery. 2(4) 88-93.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Van Ketel W. 1982. Allergy to Matricaria chamomilla. Contact Dermatitis. 8(2) 143.
Van Ketel W. 1987. Allergy to Matricaria chamomilla. Contact Dermatitis. 16(1) 50-51.
Vessell ES, Lang CM, White GT et al. 1976. Environmental and genetic factors affect-
ing response of laboratory animals to drugs. Federation Proc. 35:1125-1132.
Watt M. 1991. Plant Aromatics. Essex, UK: Witham.
Weil A. 1998. Complementary care for cancer. Dr. Andrew Weil’s Self-Healing. Jan. 1,
6-7.
Williams A, Barry B. 1989. Essential oils as novel human skin penetration enhancers.
Journal of Pharmaceutics. 57:R7-R9.
Yip A, Chow W, Tai Y. 1990. Adverse effect of methyl salicylate ointment on warfarin
anticoagulation: an unrecognized potential hazard. Postgraduate Medical Journal.
66(775) 367-369.
Chapter 4 Essential Oil Toxicity and Contraindications 101

W
102
5
Psychology
“Why do women sniff bread?” I asked. It was something I often noticed Ma doing.
“To see if it is fresh I suspect,” Uncle Seth said. “I have never sniffed bread in my
life, which is the difference between me and a woman. ...And when a woman
comes to decide who to marry it comes down to the same test,” he added.
“You mean they sniff men?” I asked. I could not imagine what it would feel like
to have a woman sniff me.
“Yes, to determine if the fellow’s fresh,” Uncle Seth said. “I guess I don’t smell
fresh, which is why I’m a bachelor still.”
Larry McMurtry
Boone’s Lick
D
odd (1991) described stimulation of olfactory responses by odorants as “a
branch of molecular pharmacology that was similar to mood changes
brought about by some psychotropic drugs.” Responses to pleasant odors
are conducted unconsciously, although both olfactory nerve connections and
measured physiologic changes indicate that the response is of an emotional and
hormonal nature.
Jellinek (1999) describes four different mechanisms through which essential
oil odors affect psychologic states. He calls these mechanisms quasipharmaco-
logic, semantic, hedonic, and placebo. Quasipharmacologic refers to the small
amounts of essential oil components found in the bloodstream following inhala-
tion. Semantic refers to the odor within the context of life experience. Hedonic
refers to feelings of pleasure or displeasure on inhaling an essential oil. Placebo
refers to the expectations of the person inhaling the essential oil, which color his
or her response.

Pheromones
Smell is very important in life, beginning with newborn babies’ identification of
their mothers (Macfarlane 1975) and continuing into old age. Even subliminal
smell is important. Partners, lovers, and friends are chosen through subliminal
smells called pheromones (Watson 2000). Pheromones are airborne chemicals in-
voluntarily expelled into the air that affect the physiology or behavior of other
members of the same species. Pheromones were discovered in the 1930s by
Adolph Butenandt, a German biochemist who won the Nobel Prize in 1939 for
his work on human hormones. He was forbidden to accept the award by Hitler,
and he changed his research focus to how female moths attract males at great dis-
tance. It took Butenandt the next 20 years to identify the first pheromone,
bobykol, “a substance so powerful that if any one female moth were to release all
her store in a single spray, there would be enough to bring a trillion males to her
side” (Dossey 2001). Pheromones are linked to the vomeronasal organ: two tiny
pits just inside the nostrils (Watson 2000).
Although a person may not be aware of another person’s pheromones, they
are what really attracts him or her to that person. Couples going through mar-
riage breakdown often say their partner “no longer smells the same” (Needham
1999). This is much truer than they realize because the chemical attraction be-
tween them has changed from attracting mode to repelling mode, just as their
emotions have changed. Pheromones work in a subliminal way, meaning humans
are unaware of them, although they may still sense “something” is different.
Everyone’s body odor is unique—a “smellprint.” An electronic device known
as the Bloodhound, an artificial sniffing dog, was built at Cambridge University.
This device could identify a person’s smellprint, and by recording a particular per-
son’s unique body odor, the machine could recognize that smellprint anywhere in
the world.
Psychoaromatherapy
It is also possible, using psychoaromatherapy (environmental fragrancing), to ma-
nipulate mood or change perception through the use of subliminal smell. A cer-
tain amount of research has been conducted on this, and the results show people
can be encouraged or manipulated using this method of aromatherapy (Kirk-
Smith 1993). For example, customers in a store can be encouraged to purchase an
item, rather than another identical item, by impregnating it with a pleasant sub-
liminal smell. Companies can “persuade” customers to pay bills on time by im-
pregnating invoices with subliminal, offensive odors. The concept is disturbing,
and the possible repercussions arguably unethical.
Psychoaromatherapy is not just about subliminal smell. The perfume indus-
try is very concerned with how our choice of scent affects us (Mensing & Beck
1988). Millions of British pounds and American dollars are spent each year on
olfaction research (Dossey 2001).
Chapter 5 Psychology 103

Aromas have measurable effects on how we feel. Torii et al (1988) report on
the psychologically stimulating effect of jasmine. Manly (1993) found the effect
of lemon, lemongrass, peppermint, and basil to be psychologically stimulating,
and the effects of bergamot, chamomile, and sandalwood to be relaxing. Other
aromas found to be relaxing were rose and lavender (Kikuchi et al 1991). Pepper-
mint and lavender improved the efficiency of proofreaders (Kliauga et al 1995).
Sweet orange essential oil was effective in children for both induction of anes-
thesia and recovery time following surgery (Mehta et al 1998).
It is not necessary to be awake for an aroma to affect a person physiologically.
Whereas Sugano (1992) found jasmine stimulating to subjects who were awake,
Badia et al (1990) found the effect of jasmine was still stimulating when subjects
were asleep. Badia et al (1990) found that peppermint was also simulating. He-
liotropin relaxed some subjects and disrupted sleep in others. The aroma appeared
to cause changes in subjects’ electroencephalogram (EEG) results and blood pres-
sure, but did not affect respiration.
Yamaguchi (1990) found that aromas could affect heart rate. Van Toller et al
(1992) mapped the brain while subjects wearing a special 28-lead “hat” inhaled
aromas. Schulz et al (1998) used EEG activity to screen acute sedative effects of
several essential oils compared against diazepam, and the use of EEGs to moni-
tor the effects of aromas is becoming more commonplace. Lorig et al (1990) also
measured EEG activity during olfaction. Masago et al (2000), using lavender,
chamomile, and sandalwood, found that alpha 1 activity significantly decreased
during odor conditions in which the subjects felt comfortable, and showed no sig-
nificant change under odor conditions in which the subjects felt uncomfortable.
Alpha 1 is the 8.5-10.5 Hz frequency band of an EEG signal.
Smell is also a language, a method of communication. We involuntarily com-
municate through subliminal smell—our pheromones. We talk about “smelling
danger,” say that someone or something “smelled wrong,” or refer to “sniffing it
out.” The French have a saying, Je ne peux pas le sentir, which means “I don’t trust
him”; the literal translation is “I can’t smell him.” Unconsciously we choose our
friends and partners by smell. Research has shown that subliminal smell placed
on a waiting-room chair attracted a statistically significant proportion of patients
entering that waiting room (Kirk-Smith & Booth 1987).
Learned memory is a reaction to a smell that has been learned through ex-
perience, for example, trauma linked to an aroma. When that odor is smelled
again, fear, or the emotion originally experienced, is triggered. An example of this
phenomenon of learned memory is the use of lavender in older adults. For many
elderly people in Europe, lavender is associated with linen chests, and for some
the odor is closely linked with care of the dying. Lavender has undergone a
tremendous revival thanks to aromatherapy, and although it appears to be univer-
sally enjoyed by those younger than 60 years of age, this learned memory associ-
ation between lavender and death could be why those Europeans in their 70s or
older are sometimes not quite so enthusiastic.
104 Section I Overview

Kirk-Smith (1993) tells the story of a 55-year-old man who, as a child, was
terrified of a teacher who wore a particular perfume. In later life, that same per-
fume still evoked a sense of anxiety. Learned memory of smell is hard to undo.
The functioning of the human body is greatly affected by the mind. In recent
years, medicine has begun to accept the mind/body connection. Our immune sys-
tem has receptors for endorphins and is strongly affected by our sense of well be-
ing. Bereavement, anxiety, and stress (Quinn & Strelkauskas 1993) affect this
continual conversation between brain and immune system. By combining two ex-
ternal communicators, smell and touch, our patients’ abilities to communicate in-
ternally are greatly enhanced.
Smell is closely linked to taste (although smell is considerably more sensi-
tive), which is why when we have a cold, food does not smell appetizing. We eat
to live: food has a molecular structure, which our bodies break down into atoms;
this has both physiologic and psychologic effects. We also eat because food tastes
good. Smells can give us similar pleasure, and they too affect us physiologically
and psychologically. Aromas have also been shown to enhance the output of the
workforce, raise feelings of job satisfaction, and reduce sick-leave absences
(Chadwick & Mann 1983). Specific aromas have specific effects. Melissa has
been used for grief, lemongrass to mask offensive smells, marjoram and lavender
to aid insomnia in the elderly, and geranium and mandarin to enhance memory
recall in patients with Alzheimer’s disease.
Saeki and Shiohara (2001) investigated the physiologic response to inhaled
lavender, rosemary, and citronella on nine healthy women aged 21 to 23 who were
recruited from Nagano College of Nursing in Japan. The study measured the re-
sponses to R-wave intervals on an electrocardiogram, blood flow in the fingertips,
galvanic skin conduction (GSC), and blood pressure. Tests were performed in an
air-conditioned room at 22° to 25° C. The study began by measuring baselines.
Then 6 drops of one of the three aromas were heated in 10 ml of hot water in an
aroma pot. The subject entered the room and inhaled the essential oil for 10 min-
utes. A break of 90 minutes was allowed between each aroma to allow for aroma
dispersal.
The results showed lavender decreased systolic blood pressure within 10
minutes, decreased GSC within 2 minutes, and increased blood flow within 6
minutes. The R-R interval did not change. Rosemary increased the systolic blood
pressure and decreased the blood flow immediately, but these responses returned
to normal within minutes. There were also changes in the ECG, and the two fre-
quency components of heart rate variation, (which, simply put, means the ratio
between respiration and heart beat) increased significantly and immediately. This
appears to confirm that rosemary has stimulant effects, although they appear to
be transitory. Citronella did not change blood flow or blood pressure, but it did
increase the R-R interval after 10 minutes, although GSC decreased immediately.
Each participant’s like or dislike of the aroma could explain these conflicting
results.
Chapter 5 Psychology 105

Mind/Body Connections
Sugawara et al (1999) found that a perception of fragrance is related to the type of
work a person does. In this study the difference between mental and physical work
altered perceptions of scent. Scores were recorded for seven essential oils before and
after specific types of work. Cypress had a more favorable impression after physical
work than before. (This is interesting because cypress has a deodorant effect!) Or-
ange had a less favorable reaction after physical work. Degel & Koster (1999) found
that ambient odor could have a negative or positive effect on a variety of tests. The
researchers gave 108 subjects a variety of tests in a room weakly scented with jas-
mine or lavender or in an odorless room. The tests included viewing slides of dif-
ferent surroundings (including the room in which they were located). Subjects were
asked to rate how well specific odors matched the slides. Jasmine appeared to have
a negative and lavender a positive effect on test performance.
Jelinek and Novakova (2001) give a moving account of how aromatherapy
had a positive effect on a 14-year-old boy in prison in Bohemia. The teenager was
aggressive and had behavior problems. What was most interesting was how each
aroma triggered his memory and how that memory allowed the boy to commu-
nicate his feelings. For example ylang ylang evoked the smell of his father’s
Sunday-morning shave and the good things they did together, but after smelling
peppermint the boy said “I don’t know any more.”
Aromas affect even the unborn child. A French study (Schaal et al 2000) ex-
amined whether prenatal exposure to aroma could influence selective response. In
this randomized study the test group of mothers consumed anise-flavored candy
containing up to an estimated intake of 121 mg of anethole. When the newborn
babies were exposed to a swab with anethole, videos recorded facial and head re-
sponses in favor of the smell. The babies of the control mothers (who did not eat
any anethole candy) demonstrated an aversive or neutral response. The other ba-
bies turned toward the anethole swab.
Smell can help people cope with a traumatic experience, and may be of use
in treating panic attacks. Redd and Manne (1995) investigated the effect of using
aroma to reduce distress during magnetic resonance imaging. A small tube was
inserted in the nostrils of 57 participants who received either heliotropin (a
vanilla-like scent) or plain air. Patients who received the heliotropin reported 64%
less anxiety than the control group who had plain air, even though the respiration
and heart rate of the experimental group showed no change.
Not all aromatherapy studies have been successful in reducing perception of
anxiety. Wiebe (2000) found that vetiver (a common ingredient in men’s cologne
and aftershave), bergamot, and geranium did not reduce the stress of women
about to have an abortion. The essential oils were smelled for 10 minutes. The
control group smelled a hair conditioner containing synthetic scent.
Certain aromas may help reduce stress before and during examinations.
Fillian (2000) studied the effect of a mixture of lavender (Lavandula angustifolia)
and rosemary (Rosmarinus officinalis) on 13 adult volunteers of an advanced
106 Section I Overview

physiology class at a graduate college All students were patch tested before the
study began. During the study, subjects were asked to apply 5 drops of 2% solu-
tion to their wrists, rub their wrists together and inhale deeply for 5 minutes be-
fore the examination.This could be repeated as necessary during the examination.
The average mean score of the tests taken previously by the subjects was 85.4%.
The average score of the tests when aromatherapy was used was 89.7%. Although
the students could have become more familiar with the testing procedure (this
was their fifth test out of six), and the test itself could have been simpler, the stu-
dents all reported a feeling of calmness and clear thought.
Lavender and rosemary were the subjects of a randomized, controlled study
reported in Reuters Health (an on-line health bulletin service) on March 28,
2002. Either lavender or rosemary was given to 144 young adults; they were then
given tests of their working memory and reaction times. Mood tests were com-
pleted before and after the memory exercises. Study participants in the lavender
group reported feeling less alert in the lavender-scented cubicles, participants in
the rosemary group reported feeling more content after they completed the mem-
ory tests than they did before. The study findings were presented at the British
Psychological Society’s annual meeting in Blackpool, UK.
Age, sex, and exposure to noxious agents all affect our sense of smell. As we
become older our sense of smell deteriorates. Women are thought to have a
greater sense of smell than men. This is particularly interesting as most ‘noses’ or
professional perfumers are men. Results from a National Geographic Smell Sur-
vey (712,000 respondents) indicate that certain medicinal and environmental
agents adversely affect the sense of smell. Workers in a factory reported poorer
sense of smell after the suggestion that exposure to the factory workplace had im-
paired their sense of odor (Corwin et al 1995). Russell et al (1993) interpreted the
Smell Survey to show that there were marked changes in odor categorization
across the life span. After the age of 60, there was marked displacement for some
odors—some odors were more difficult to smell or identify.
Essential oils make up very complicated aromas that are difficult to emulate.
Rose oil is one of the most complicated and has baffled synthetic chemists for
some time. Scientists suspect that the sweet component of rose odor is made by
the breakdown of carotenoids, a compound found in the petals that gives red roses
their color. Science News describes how Japanese researchers have identified an en-
zyme that turns carotenoids into the chemical precursor to beta-damascenone,
but have been unable to replicate it. (April 15, 2000).
Espenshade (1999) discussed a select mute child in the second grade who
had not responded in class to any questions since kindergarten. He had arrived at
the school 2 years previously. The child was from Sardinian parents but was born
in the United States. He behaved normally at home. Espenshade, a teacher,
worked with the family and suggested six essential oils for the boy to choose from.
The boy chose three: frankincense, bergamot, and Scotch pine. Each morning
when he arrived at school he came to Espenshade and selected one of the scents.
Several drops were placed on a tissue he kept in his pocket. There was a gradual
Chapter 5 Psychology 107

but definite change. A few weeks into the study, the boy spoke for the first time
in class. One particular essential oil, Scotch pine, seemed to help him. When his
father learned his son had spoken in class for the first time, he asked which scent
had worked. On hearing that it was Scotch pine, his comment was, “That is just
how Sardinia smells!” The boy had never visited Sardinia. Table 5-1 indicates
some essential oils and the research carried out on them regarding their psycho-
logic effects.
Depression
Depression is one of the most widespread mental-health problems in the world
(Yarnell & Abascal 2001). It is estimated that more than 20 million Americans
suffer from depression, but only one in three seeks professional help (Papoloso &
Papoloso 1997). Although the majority of patients are treated with medication or
psychotherapy, some medications can be unacceptable because of side effects, po-
tential drug interactions, or potentially dangerous overdose (Davidson et al 1997).
Psychotherapy can be rejected as an alternative to drugs because of time, effort,
and cost. Many patients in the United States are turning to complementary
108 Section I Overview
Table 5-1 h Selected Studies on the Psychologic Effect of Essential Oils.
Basil Manly 1993
Bergamot Manly 1993
Chamomile Manly 1993
Eucalyptus Berg 1987
Citronella Saeki & Shiohara 2001
Jasmine Sugano 1992, Torii et al 1988
Lavender Kikuchi et al 1991, Kliauga et al 1995, Yamaguchi et al 1995
Lemon Sakakibara et al 1995
Lemongrass Manly 1993
Orange Baron & Thomley 1994, Mehta et al 1998
Rose Kikuchi et al 1991
Peppermint Kliauga et al 1995, Warm et al 1992
Rosemary Kubota et al 1992
Sandalwood Steiner 1994

medicine and are either self-medicating or are being treated by therapists outside
conventional medicine.
Depression can go unnoticed and sometimes be misdiagnosed as exhaustion
(Castro 1997). Depression is not always caused by emotional stress. Alcohol, sub-
stance abuse, prolonged lack of sleep, environmental pollutants, and conventional
medicines such as antibiotics or the contraceptive pill can be contributors. Sea-
sonal affective disorder (SAD) thought to be caused by lack of sunlight which
manifests in depression is particularly relevant to those living in Alaska, or other
places in the far north. Postpartum depression was thought by many to have in-
fluenced the mood and behavior of Andrea Yates, who drowned her five children
(Slater 2001).
Few patients are able to articulate their feelings of depression to a physician,
and may say they feel generally unwell. A diagnosis of clinical depression is made
when five or more of the following symptoms have been present every day, or
nearly every day, for 2 weeks or more (Diagnostic and Statistical Manual of the
American Psychiatric Association–IV [DSM-IV] 1994):
• Feelings of sadness, gloom, emptiness
• General lack of interest (apathy)
• Significant weight loss or gain or increase in appetite
• Insomnia or hypersomnia
• Physical restlessness or lack of physical motivation
• Exhaustion, not helped by sleep
• Feelings of worthlessness or excessive or inappropriate guilt
• Difficulty making decisions, thinking, remembering, and concentrating
• Recurrent thoughts of death or suicide without specific plan
Since March of 1998, psychologists in New Mexico have had prescriptive
powers and this is set to be repeated in several other states across the USA.There-
fore it is pertinent to mention the most commonly prescribed anti-depressant
drug in the USA, which is imipramine, a tricyclic antidepressant. Unlike essential
oils, there are considerable side effects to imipramine that include lethargy, dis-
orientation, dry mouth, weight gain, impaired concentration, and memory disori-
entation (Lieberman 1998). These symptoms alone could lead to depression.
Although most people agree that a foul-smelling odor does not enhance their
mood but a pleasant one might, there has been little scientific research to sub-
stantiate this. Yarnell and Abscal (2001) suggest essential oils should not be over-
looked in the treatment of depression because “inhaled volatile oils pass through
the olfactory nerve directly to the cerebrum.” Whereas antidepressants work by
making the neurotransmitter serotonin linger in the gaps between brain cells, es-
sential oils may work as serotonin agonists, which can push the serotonin system
into overdrive. This makes the brain more sensitive, rather like turning up the vol-
ume on a radio: Suddenly you can hear very weak stations.
Erlichmann and Bastone (1992) found that odors could produce psychologic
effects similar to mood states. Subjects were presented with pleasant and un-
pleasant odors while engaging in mood-sensitive tasks. The pleasant odors tested
Chapter 5 Psychology 109

were almond and coconut, representing food, and muguet and water lily, repre-
senting flowers. The unpleasant odors were pyridine and butyric acid, represent-
ing chemicals, and limburger cheese and cigar butt, representing natural sub-
stances. Synnott (1995) discusses the meaning of smell and relates that 50% of
people who use public transportation in the United States object first and fore-
most to wearers of heavy perfume. Crying babies came after that!
Knasko (1992) tested the effect of ambient odor of lemon, lavender, and di-
methyl sulfide (DSM) on the creativity, mood, and perceived health of 30 subjects
(15 women and 15 men). The test room was scented by placing five perfume blot-
ters, each containing four drops of the essential oil or four drops of DSM, in the
ceiling ducts of the room, as well as under the table and chair of the subject. On
control days, blank perfume blotters were used. During testing the room’s vents
were closed to keep the aroma in the room. Between subjects the vents were
opened and the fans run for at least 1 hour to clear the room. Before the study, 12
people rated the intensity of all 3 aromas as weak-moderate.
Subjects in the DSM group appeared to be in a less-pleasant mood after ex-
posure to the scent. Subjects in the lemon group appeared to feel healthier. There
was no demonstrated difference in creativity, but relationships emerged between
the personality of the person and the effect of the odor. The lack of impact on cre-
ativity may have been related to the weakness of the odor. Ludvigson and
Rottman (1989) found an effect from lavender and cloves on cognition, memory,
affect, and mood, but the aroma had been classified as “strong.” Warm et al (1990)
also reported a positive effect from fragrances, but they used a facemask to deliver
an intermittent scent.
Knasko (1995) found that areas diffused with a pleasant smell produced a
more positive mood in the public. One of her studies involved an exhibit at an an-
thropological museum displaying North American crafts and clothing. Three
odors—bubble gum, incense, and leather—were tested during a 3-week period,
following a first week with no odor. A surveillance camera recorded the length of
time an individual lingered by the exhibit and exit interviews were conducted.
The visitors reported the most positive mood effect during the bubble gum week.
However, visitors in the incense week felt they had learned more from the exhibit.
Itai et al (2000) found that hiba oil reduced depression and anxiety in 14 pa-
tients receiving hemodialysis in a controlled study. Hiba oil is obtained from Thu-
jopsis dolabrata, a Japanese tree (Guenther 1976). Hamilton rating scales for de-
pression (HAMD) and anxiety (HAMA) were used. Lavender reduced anxiety
but not depression.
Studies have shown the depression levels of elderly people living in assisted-
care facilities were reduced with the aromas of fruit and flowers (Schillmann &
Siebert 1991). Citrus was found to relieve depression (and improve immune func-
tion) by Komori et al (1995). A number of essential oils, including lavender, jas-
mine, rosemary, rose, and chamomile are used for treating depression. They are
primarily given as inhalants, but Valnet (1980) also suggests taking thyme and
lavender orally using between 2 to 5 drops two or three times a day.
110 Section I Overview

Research indicates that there is a link between depression and increased
deep-limbic activity when the amygdala becomes overactive (Drevets et al 1992).
Herz (2000) found most people choose to lose their sense of smell rather than any
other sense or a part of their anatomy. However, people who did lose their sense
of smell though illness or accident reported a loss of emotional richness in their
lives and tended toward depression. The link between smell and emotion is very
strong. Following bereavement, a photo may elicit sad memories, but the smell of
a loved one’s clothes is more likely to produce tears.
Depression, anger, and fear are closely related. The amygdala is the key to our
sense of fear and is thought to play a pivotal role in survival behavior. So-
matosensory stimuli have direct input into the amygdala and do not go through
the thalamus to reach the cortex. This process is unique and is thought to occur
because the olfactory cortex has only four cellular layers. Every other part of the
frontal, parietal, occipital, and temporal lobes of the brain has six layers. To facil-
itate an instant response to stimuli, the amygdala is thought to control the auto-
nomic nervous system. The main outputs of the amygdala are to the hypothala-
mus and brainstem autonomic centers. These include the vagal nuclei and the
sympathetic neurons (www.limbic.html).
Dreams
Dossey (1999) describes the divide between how dreams are perceived by West-
ern culture and by traditional cultures. Whereas orthodox medicine perceives ac-
tivity of the mind as a local event happening solely within the brain, the approach
of many other health care systems is that dreams have the ability to make people
ill or restore them to health (Severson 1979). Therefore anything that impacts
dreams and their link to our subconscious is not to be taken lightly.
Badia et al (1995) investigated the impact of odor on the sleep and dreams
of 20 undergraduate students (6 male and 14 female) using a 5-band EEG (delta,
theta, alpha, beta 1, and beta 2). Previous research had shown that stimuli pre-
sented during sleep could be detected and that the right side of the brain, specif-
ically the frontal region, was more active during rapid eye movement (REM)
sleep. REM is the period of sleep when dreams occur. (Humans may not be the
only creatures who dream; dolphins also experience REM sleep.) Test subjects
slept in a room with either filtered air or one of two odors: androsterone or pep-
permint. Contrary to expectations, there was no significant difference found in
most subjects’ EEG bands. However, there was significantly more power in the
theta band of subjects in the room with androsterone, suggesting androsterone
was disruptive to sleep, regardless of whether the subject could smell it. However,
there was little incorporation of either aroma into the participants’ dreams.
Trotter et al (1994) introduced 16 olfactory stimuli of different kinds (rang-
ing from roses and coffee to dog feces and hand lotion) for 1 minute after sub-
jects had displayed REM sleep for a minimum of 5 minutes. There were 5 sub-
jects, and they were examined during 15 nights with 48 tests during this time.
Chapter 5 Psychology 111

The scents were incorporated into the subjects’ dreams 22% of the time. One sub-
ject described a dream of walking by some gardenias that smelled like lemons.
Hoffman (1999) investigated the effect of frankincense on dreaming. Seven
subjects, who were all women and had been recording their dreams for many
years, took part in the study. During the first week the scientists took base-line
measurements: number of dreams, vividness, color intensity, length, clarity, and
quality. Each measurement was graded between 0 and 10 (0 the lowest, 10 the
greatest). For the next 2 weeks, the women put 2 drops of frankincense on a cot-
ton ball and placed the cotton ball underneath their pillowcases each night. Three
participants had a significant positive change in their dream recall. Another stated
she had solved a problem that, in her waking state, she had been working on for
some time. Two others believed that their dream recall was enhanced slightly. The
remaining two at first believed that frankincense had decreased their ability to re-
call dreams, but during the second week the quality of their dreams was en-
hanced.
Fabrici (1998) carried out a similar study using the same methodology but
used angelica (Angelica archangelica). Her four subjects were all women and were
seasoned dreamers used to recording their dreams. Each of the four women found
that angelica either stopped her dreams or interfered with them in such a way that
she did not want to continue with the study. This is a fascinating area of research
and one that has hardly been touched. As we become more aware of the subtle
messages dreams can give us, anything that can encourage the messenger is po-
tentially very valuable.
REFERENCES
Badia P, Wesensten N, Lammers W et al. 1990. Responsiveness to olfactory stimuli pre-
sented in sleep. Physiology and Behavior. 48(1) 87-90.
Badia P, Boecker M, Wright K. 1995. Some effects of fragrances on sleep. In Gilbert A
(ed.), Compendium of Olfactory Research 1982-1994. New York: Olfactory Research
Fund Ltd, 31-39.
Baron R, Thomley J. 1994. A whiff of reality. Environment and Behavior. 26(6) 766-784.
Berg K. 1987. The effect of smell on cognitive processes. DRAGOCO Report. 39,
128-129.
Castro M. 1997.The treatment of depression with homeopathy. Alternative & Comple-
mentary Therapies. 1(4) 300-305.
Chadwick J, Mann W (eds.). 1983. Hippocratic Writings. Harmondsworth, UK:
Penguin Books, 24.
Corwin J, Loury M, Gilbert A. 1995. Workplace, age, and sex as mediators of olfactory
function: Data from the National Geographic Smell Survey. The Journals of Geron-
tology. Series B, Psychological Sciences and Social Sciences. 50(4) 179-186.
Davidson J, Morrison R, Shore J et al. 1997. Homeopathic treatment of depression and
anxiety. Alternative Therapies in Health and Medicine. 3(1) 46-49.
Degel J, Koster E. 1999. Odors: Implicit memory and performance effects. Chemical
Senses. 24(3) 317-325.
112 Section I Overview

Diagnostic and Statistical Manual of the American Psychiatric Association–IV [DSM-
IV]): 1994.
Dodd G. 1991. The molecular dimension of perfumery. In Van Toller S, Dodd G (eds.),
Perfumery: The Psychology and Biology of Fragrance. London: Chapman and Hall,
19-46.
Dossey L. 1999. Dreams and healing: Reclaiming a lost tradition. Alternative Therapies
in Health and Medicine. 6(6) 12-17, 111-117.
Dossey L. 2001. Surfing the odornet: Exploring the role of smell in life and healing. Al-
ternative Therapies in Health and Medicine. 7(2) 12-16, 100-107.
Drevets W, Videen T, Price J et al. 1992. A functional anatomical study of unipolar de-
pression. Journal of Neuroscience. 12(9) 3628-3641.
Erlichmann H, Bastone L. 1992. The use of odor in the study of emotion. In Van Toller
S, Dodd G (eds.), Fragrance: The Psychology and Biology of Perfume. London:
Elsevier Applied Science, 143-159.
Espenshade T. 1999. The effects of aromatherapy on a select mute. Unpublished disser-
tation, Hunter, New York, RJ Buckle Associates.
Fabrici M. 1998. What is the effect of angelica on dreams? Unpublished dissertation,
Hunter, New York, RJ Buckle Associates.
Fillian C. 2000. Does aromatherapy have any impact on human performance Unpub-
lished dissertation, Hunter, New York, RJ Buckle Associates.
Guenther E. 1976. The Essential Oils, Vol. IV. Malabar, FL: Krieger, 323-325.
Herz R. 2000. Scents of time. The Sciences. 40(4) 34-39. Retrieved October 12, 2002
from http://infotrac.galegroup.com.
Hoffman C. 1999. Does aromatherapy enhance dream recall? Unpublished dissertation,
Hunter, New York, RJ Buckle Associates.
Itai T, Amayasu H, Kuribayashi M et al. 2000. Psychological effects of aromatherapy
on chronic hemodialysis patients. Psychiatry and Clinical Neurosciences. 54(4)
393-397.
Jelinek A, Novakova B. 2001. The psychotherapeutic use of essential oils. International
Journal of Aromatherapy. 11(1) 100-102.
Jellinek A, 1999. Odors and mental states. International Journal of Aromatherapy. 9(3)
115-120.
Kirk-Smith M, Booth D. 1983. Unconscious odor conditioning in human subjects. Bio-
logical Psychology. 17: 221-231.
Kirk-Smith M. 1993. Human olfactory communication. In Aroma 93 Conference Pro-
ceedings. Brighton, UK: Aromatherapy Publications, 83-103.
Kliauga M, Huberts K, Cenci T. 1995. Consumer panel study of fragrance and proofreading
efficiency. In Gilbert A (ed.), Explorations in Aroma-chology: Compendium of Aroma-
chology Research 1982-1994. New York: Olfactory Research Fund Ltd., 131-135.
Knasko S. 1992. Ambient odor’s effect on creativity, mood, and perceived health. Chemi-
cal Senses. 17(1) 27-35.
Knasko S. 1995. Congruent and incongruent odors: Their effect on human approach be-
havior. In Gilbert A (ed.), Compendium of Olfactory Research 1982-1994. New
York: Olfactory Research Fund Ltd., 117-128.
Komori T, Fujiwara R, Tanida M et al. 1995. Effects of citrus fragrance on immune
function and depressive states. Neuroimmunomodulation 2(3) 174-180.
Kubota M, Ikemoto T, Komaki R et al. 1992. Odor and emotion—Effects of essential oils
on contingent negative variation. In Buchbauer G, Woidich H (eds.), Proceedings:
Chapter 5 Psychology 113

12th International Congress of Flavors, Fragrances and Essential Oils. Vienna: Aus-
trian Association of Flavor & Fragrance, 456-461.
Lieberman S. 1998. Treating depression with St John’s Wort. Alternative & Comple-
mentary Therapies. 4(3) 163-168.
Lorig T, Schwartz G. 1988. Brain and Odor: Alteration of human EEG by odor admin-
istration. Psychobiology. 16(3) 281-284.
Ludvigson H, Rottman T. 1989. Effects of lavender and cloves on cognition, memory,
affect and mood. Chemical Senses. 14(4) 525-536.
Macfarlane A. 1975. Olfaction in the development of social preferences in the human
neonate. In Parent-Infant Interaction (Ciba Foundation Symposium No. 33). Amster-
dam: Elsevier, 103-107.
McMurtry L. 2000. Boone’s Lick. New York: Simon & Schuster, 87-88.
Manley C. 1993. Psychophysiological effects of odor. Critical Review of Food Science
Nutrition. 33(1) 57-62.
Masago R, Matsuda T, Kikuchi Y et al. 2000. Effects of inhalation of essential oils on
EEG activity and sensory evaluation. Journal of Physiological Anthropology & Ap-
plied Human Science. 19(1) 35-42.
Mehta S, Stone D, Whitehead H. 1998. Use of essential oils to promote induction of
anesthesia in children. Anaesthesia. 53(7) 720-721.
Mensing J, Beck C. 1988. The Psychology of fragrance selection. In Perfumery: the psy-
chology and biology of fragrance. Edited by Van Toller S and Dodd G. Chapman &
Hall, London.
Needham S. 1999. Personal communication.
Papoloso D, Papoloso J. 1997. Overcoming Depression, 3rd ed. New York: Harper
Perennial.
Quinn J, Strelkauskas A. 1993. Psychoimmunologic effects of therapeutic touch on prac-
titioners and recently bereaved recipients: A pilot study. Advances in Nursing Science.
15(4) 13-26.
Redd W, Manne S. 1995. Using aroma to reduce distress during magnetic resonance
imaging. In Gilbert A (ed.), Compendium of Olfactory Research 1982-1994. New
York: Olfactory Research Fund Ltd., 47-52.
Russell M, Cummings B, Profitt B, et al. 1993. Life span changes in the verbal catego-
rization of odors. Journal of Gerontology. 48(2) 49-53.
Saeki Y, Shiohara M. 2001. Physiological effects of inhaling fragrances. International
Journal of Aromatherapy. 11(3) 118-125.
Sakakibara K, Iguchi H, Satoh S et al. 1995. Psychological and physiological effects of
odors on mental workload. Chemical Senses. 20(3) 382.
Schaal B, Marlier L, Soussignan R. 2000. Human foetuses learn odours from their preg-
nant mother’s diet. Chemical Senses. 25(6) 729-737.
Schillmann S, Siebert J. 1991. New frontiers in fragrance use. Cosmetics & Toiletries.
106(6) 39-45.
Schulz H, Jobert M, Hubner W. 1998. The quantitative EEG as a screening instrument
to identify sedative effects of single doses of plant extracts in comparison with di-
azepam. Phytomedicine. 5(6) 449-458.
Severson R. 1979.The alchemy of dreamwork: Reflections on Freud and the alchemical
tradition. Dragonflies. Spring, 109.
Slater L. 2001. Beginning and end. New York Times Magazine. July 8, 11.
114 Section I Overview

Sugano H. 1992. Psychophysiological studies of fragrances. In Van Toller S, Dodd G
(eds.), Fragrance: The Psychology and Biology of Perfume. London: Elsevier Applied
Science, 221-226.
Sugawara Y, Hino Y, Kawasaki M et al. 1999. Alteration of perceived fragrance of essen-
tial oils in relation to type of work: A simple screening test for efficacy of aroma.
Chemical Senses. 24(4) 415-421.
Steiner W. 1994. The effects of odors on human experience and behavior. In Jellinek P
(ed.), The Psychological Basis of Perfumery. London: Blackie Academic & Profes-
sional, 200-217.
Synnott A. 1995. Roses, coffee and lovers: The meaning of smell. In Gilbert A (ed.),
Compendium of Olfactory Research 1982-1994. New York: Olfactory Research Fund
Ltd., 117-128.
Tanida M, Kikuchi A, Uenoyama S et al. 1992. Effect of odor on cardiac response pat-
terns during a fore period in reaction time task. J Soc Cosmet Chem Jap. 26(2)
113-119.
Torii S, Fukuda H, Kanemoto H et al. 1988. Contingent negative variation and the psy-
chological effects of odor In Van Toller S, Dodd G (eds.), Perfumery: The Psychology
and Biology of Fragrance. London: Chapman and Hall, 107-120.
Trotter K, Dallas K, Verdone P. 1994. Olfactory stimuli and their effects on REM
dreams. In Dossey L. 2001. Surfing the odornet: Exploring the role of smell in life
and healing. Alternative Therapies in Health and Medicine. 7(2) 12-16, 100-108.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Van Toller S, Hotson S, Kendal-Reed M. 1992. The brain and the sense of smell. In Van
Toller S, Dodd G (eds.), Fragrance: The Psychology and Biology of Perfume.
London: Elsevier Applied Science, 195-217.
Warm J, Dember W, Parasuraman R. 1990. Effects of fragrances on vigilance perfor-
mance and stress. Perfumer & Flavorist. 15(15) 17-18.
Warm J, Dember W, Parasuraman R. 1992. Effects of olfactory stimulation on perfor-
mance and stress of a visual sustained attention task. Journal of the Society of Cos-
metic Chemists. 42 199-210.
Watson L. 2000. Jacobson’s Organ. New York: WW Norton & Co.
Wiebe E. 2000. A randomized trial of aromatherapy to reduce anxiety before abortion.
Effective Clinical Practice. 3(4) 166-169.
Yamaguchi A, Koga Y, Fujimura A et al. 1995. The psychological study on the effect of
odor absorbed in cloth. Chemical Senses. 20(3) 381.
Yamaguchi H. 1990. Effect of odor on heart rate. In Indo M (ed.), The Psychophysio-
logical Effect of Odor. Tokyo: Koryo, 168.
Yarnell K, Abascal K. 2001. Botanical treatments for depression. Alternative & Comple-
mentary Therapies. 7(2) 82-87.
Chapter 5 Psychology 115

W
116
6
Evidence-Based
Aromatherapy in
Nursing Practice
Nurses are the real backbone behind the care delivered within our walls and the key
to patient and physician satisfaction.
Brian Keeley, CEO of Baptist Health Systems
(in Bender J 2001)
N
URSES COULD be described as an endangered species because an Internet
search for “nursing shortages” produces more than 58,000 sites. Although
nurses are the largest group of health care workers in the United States—
some 2.3 million—the number of people entering the profession has dropped
drastically since managed care came into being (Box 6-1). The American Med-
ical Association estimates there will be a shortage of 114,000 registered nurses by
2015 ( Jacob 2001). One could argue that managed care has managed the care out
of nursing because care itself is not reimbursable.
Disillusioned with their choice of career, many nurses are leaving the clinical
environment and setting up practice on their own. The situation is so devastating
that the nursing shortage dominates much of the discussion surrounding health
care concerns.
Of the 2.3 million registered nurses (RNs) in the United States, 1.8 million
work in hospitals (Nevidjon & Erickson 2001). There is a direct correlation be-
tween RN’s providing patient care and better patient outcome (DeMetro 2001).
Despite this rather obvious fact, managed care continues to reduce the number of
RNs and reduce the length of a patient’s stay in the hospital so the nurses’ work-
loads become more intense and demanding. Nurses often have to work 12-hour
shifts, and overtime is frequently mandatory. Burnout is commonplace (Crow
2001). Nurses’ morale was at an all-time low in 1999 (McNeese-Smith 1999) and
remains so.

Despite this, nurses are trusted by a society who ranks them above physicians
and other health care workers (Nevidjon & Erickson 2001). Although they are
frequently referred to as angels (Short 2001), nurses remain financially underval-
ued. The average nurse’s salary of $46,782 in 2001 had not changed in almost 10
years. However, the reason nurses no longer want to enter the profession is not
just money. It is inflexible, long working hours. It is looking after an increasing
number of patients so quality of care becomes compromised, and the nurse leaves
the shift feeling frustrated and angry. It is forced overtime and a poor retirement
plan. Today’s workforce has many other career choices, and they are making it
plain nursing is no longer attractive.
Many believe the growth of complementary therapies among nurses is the
result of their frustration with the limited care they can provide (Thompson
2001). Others believe nurses are simply responding to the market and giving pa-
tients what they want. Certainly complementary therapies give nurses a means of
demonstrating they care at a deep level. Many nurses combine aroma and touch,
and this mixture is proving the most popular of all complementary therapies with
patients (Reid 2001).
For many years nursing has been called a profession, but it may be more
accurate to describe it as an “emerging profession with a concept of mission
which is open to change”(Leddy & Pepper 1993). This ability to change makes
nursing an art as well as a science. There have been many changes since Florence
Nightingale’s day. The nurse’s role has become increasingly technological, with
more and more medical breakthroughs. Surgical procedures became more intri-
cate, and a field of critical-care nursing developed. Babies survived at 22 weeks
gestation, and neonatal nursing was born. Spare-part surgery became so normal
that donor cards vie for space with our credit cards.
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 117
BOX 6-1 Nursing Shortfalls
Percentage of nurses aged 50-64: 20%
Percentage of nurses aged 30-45: 65%
Percentage of nurses aged 30 or younger: 10%
Decline in entry-level nursing enrollment each of the past 4 years: 5-7%
Estimated increase in nursing positions by 2008: 23%
Percentage of New York hospitals that reported a shortage of nurses in April
2000: 82%
Average vacancy rate for hospital nursing jobs in first quarter of 2000: 14.7%
Average time it takes to fill an RN vacancy: 3 months
Average nurse’s salary (unchanged since 1992): $46,782
Salary offered by Kaiser (one of the largest health systems) for clinic nurses
in 2001: $15.84 per hour
Sources: AMA Council on Medical Service Report “Growing Nursing Shortage in the USA.
South Florida Business Journal (http://southflorida.bcentral.com); California Nurses Association.

However, even with all the changes, there is an enduring conceptual frame-
work that underlies nursing. Two other words share the same Latin derivation as
the word nurse. They are nourish and nurture. Nurses have nourished and nurtured
their patients to the best of their abilities no matter what the drug regime, surgi-
cal operation, or hospital constraints. Nursing the world over shares a common
aim: to facilitate a speedy return to health (or a peaceful and dignified death)
through nurturing the body and nourishing the soul.
How do nurses know how to nurse? The answer is a mixture. Much of what
nurses do is based upon experience. However, some of what they do is learned in
the classroom, and some is based on research. If one accepts (as many do) that
nursing is a calling —a vocation—there is a prevailing belief that much of what a
nurse does is “learned” intuition. How many nurses just “know” a patient will not
make it through the night? How many nurses just “know” they must go into that
room before a patient crashes or “know” a child’s temperature has just returned to
normal? These are similar to the instincts of a mother for her child. It is the nur-
turing instinct in nursing that gives it the dignity of a noble profession.
Leddy and Pepper (1993) think nurses’ “body of knowledge” is derived from
the experience of thousands of nurses who have gone before and from their own
intuition. However, in recent years, nursing theorists have developed frameworks
to explain the experience of nursing and put it in a theoretical context. Nursing
diagnosis is a method of defining what nurses do and the rationale behind those
actions.
There will always be resistance to change, and there will be those who ask
where the body of knowledge was when Florence Nightingale put lavender oil on
the brows of her soldier patients. Where was her nursing diagnosis and her nurs-
ing plan? There will be others who agree with Dossey (1993) who says “a body of
knowledge that does not fit with prevailing ideas can be ignored as if it does not
exist, no matter how scientifically valid it may be.”
In today’s world, nurses are being asked to define their role, so the appear-
ance of nurse academicians is apposite as they struggle to give some kind of sta-
tus to nursing. A change in status usually brings with it a change in language. This
language needs to be understood by nurses, and by others outside the field of
nursing, so everyone can be clear as to what nurses do, why they do it, and what
they hope to achieve by doing what they do.
Some might argue this is all reductionist and mechanistic. How can the the-
ory of nursing diagnosis have validity when every patient is different? The answer
is nurses are fighting for their survival and need to show a clear protocol of what
they do. This can only help the development and future of nursing, which lies in
the ability to integrate holism, nursing theory, and nursing diagnosis symbioti-
cally. Nurses need to use the science of language to reveal the true art of nursing.
Behind the scientific framework of nursing is increased discussion of the role
of holism in nursing: the art or skill of the nurse to care for the whole patient,
rather than just for the symptoms the patient is presenting. No complementary
118 Section I Overview

therapy on its own can make a nurse holistic because holism is something that
grows from within.
Aromatherapy involves smell and touch, which are basic needs. They are also
both learned memories of (hopefully) pleasurable and comforting experiences for
nurse and patient: basic needs. Clinical aromatherapy uses essential oils to target
specific outcomes that are measurable, so it gives nurses a documentable way to
nurture their patients in a truly holistic manner. Nurses can argue their case for
using essential oils with nursing theory and nursing diagnosis.
Clinical aromatherapy empowers nurses as it allows them to use the art as
well as the science of nursing. In a nutshell, aromatherapy puts some “good
scents” back into nursing and, in the process, allows nurses to feel good about
what they do. Nursing is evolving, and it is wonderful to see nurses using com-
plementary therapies as they were intended: to complement nursing.
Nursing Diagnosis*
Bulechek and McCloskey (1985) state nursing interventions are “any direct care
treatment that a nurse performs on behalf of a client.” Using this definition, all
treatments initiated by a nurse are related to nursing diagnosis. So if aromather-
apy is part of nursing, then aromatherapy would be an appropriate response to a
nursing diagnosis. Many nurses believe nursing diagnosis allows them to assess
their patients and write care plans more easily.
The development of nursing diagnosis gives focus to the specifications of
nursing needs by creating an exact language to analyze how the nurse can reach
the correct decision. Although resented by some who feel this language is just
what nursing does not need, nursing diagnosis is probably exactly what nursing
needs: a practical tool to clarify the nature, origin, and manifestations of nurs-
ing needs. Nursing diagnosis can also give validity to a complementary therapy
(like aromatherapy) within the concept of a care plan. Gordon (1982; 1990)
suggests “a nursing diagnosis is a health problem a nurse can treat but does not
mean that non-nursing consultants cannot be used. The critical element is
whether nurse-prescribed interventions can achieve the outcome established
with the client.”
The term nursing diagnosis was first introduced in 1953 by Fry, who was at-
tempting to set a standardized language for nursing care plans. However, nurses
disliked the idea of the word diagnosis, as it was too medical. They believed
nursing had a tradition of avoiding making statements about patients. Twenty
years went by before the first meeting of the National Group for the Classifica-
tion of Nursing Diagnosis was held. Eventually, in 1990, the North American
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 119
*For this section of the book, I relied heavily on the standard textbook Nursing Diagnosis: Applications
to Clinical Practice (Carpenito 1993). Sometimes similar examples have been used, followed by paral-
lel analysis to show how aromatherapy can be part of nursing diagnosis.

Nursing Diagnosis Association approved the following definition of nursing di-
agnosis: “Nursing diagnosis is a clinical judgment about individual, family, or
community responses to actual or potential health problems/life processes. Nurs-
ing diagnosis provides the basis for selection of nursing interventions to achieve
outcomes for which the nurse is accountable” (Carpenito 1993).
It is the independent function of a professional nurse to make a nursing di-
agnosis and decide upon a course of action to be followed for the solution of the
problem (Abdellah & Levine 1965). The practice of nursing often interfaces with
the practice of other health professionals; physicians and nurses collaborate in
common areas. This can necessitate a nurse having to choose between a nursing
or medical diagnosis. Sometimes a nurse can only attend to a medical diagnosis
because of time constraint. Sometimes the nurse may decide the medical diagno-
sis is more important than her own nursing diagnosis.
Looking at the areas of nursing diagnosis, it is obvious they carry very gen-
eralized headings under which more specific headings are given. There are many
headings that could lend themselves to the use of aromatherapy. These could in-
clude the following:
Altered comfort
Anxiety
Constipation
Fatigue
Fear
Grieving
Impaired communication
Infection
Pain
Powerlessness
Spiritual distress
Carpenito (1993) includes some 120 different nursing diagnosis headings on a
general level. Very few could not be helped via aromatherapy. Nursing diagnosis
represents a situation that is the primary responsibility of the nurse. Nurses may
also indicate collaborative problems in their nursing diagnosis, which would in-
dicate that both medical and nursing interventions are required, and they can pin-
point potential complications that might be collaborative problems or straight-
forward nursing problems.
For example, a patient with pneumonia would have potential complications
within the collaborative area of septic shock, paralytic ileus, and respiratory in-
sufficiency. The nursing diagnosis would be as follows:
Activity intolerance due to compromised respiration, high risk of fluid bal-
ance deficit due to fever and hyperventilation
Ineffective airway clearance due to pain and tracheobronchial secretions
Altered comfort related to hyperthermia, malaise,and pulmonary pathology
High risk for ineffective management of therapeutic regimen
120 Section I Overview

These diagnoses would be related to nutritional needs, home-care needs, restric-
tions, signs and symptoms of complications, and follow-up care. With the speci-
fication of precise needs for nursing it is easier to see those areas where aro-
matherapy could be used. These would be in the nursing diagnosis of altered
comfort and ineffective airway clearance. I shall consider the first of these as a
separate issue.
Nursing Diagnosis of Altered Comfort
In this case the cause of the altered comfort is listed as follows:
Hyperthermia
Malaise
Pulmonary pathology
This means anything that is going to alleviate those causes could help enhance
the comfort level of the patient. Malaise might respond to an essential oil with
calming and soothing properties such as lavender, frankincense, sandalwood,or
ylang ylang. Hyperthermia might be helped with a spritzer containing lavender
and peppermint. Chest problems and infections might respond to an essential oil
known to be bronchodilating, like eucalyptus or ravansara, which also have an-
tibacterial or antiviral properties. A nurse could use a mixture of several essential
oils to address the three problems.
Gordon (1990) developed an 11-area system for organizing the assessment
of the functional health pattern of a patient:
Activity and exercise
Coping and stress
Elimination
Health management
Nutrition and metabolism
Perception
Relationships
Self-perception
Sexuality
Sleep and rest
Values and beliefs
It is easy to see that aromatherapy could fit fairly readily into most of these cate-
gories. This kind of data enables nurses to make judgments on which the nursing
diagnosis will be based. As the care plan will be based on the nursing diagnosis,
careful analysis of the outcomes is necessary. Care plans are blueprints to enable
a continuous, consistent quality of care. They contain a diagnostic statement, de-
sired-nursing-outcome criteria, nursing interventions, and an evaluation of the
outcome.
The following case studies are true and were each carried out by a nurse in a
clinical setting.
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 121

122 Section I Overview
Case Study Alteration in Comfort Level: Malaise, Herpes
Outcome Criteria
Reduction of pain of lesion
Reduction of size of lesion
Increase time between outbreaks
M
rs. E was a 42-year-old female with a herpetic lesion on her nasal septum.
She had a history of cold sores and genital herpes. The nurse described
an intervention using aromatherapy, and the patient gave her informed consent
to aromatherapy. The nurse offered two essential oils, Eucalyptus globulus and
tea tree. The patient liked the aroma of eucalyptus and said it reminded her of
Vicks Vapor Rub. She was patch tested using a 100% dilution of Eucalyptus
globulus on her forearm. No irritation or sensitization was observed after 24
hours.
A 25% solution of Eucalyptus globulus in aloe vera gel was given to the patient
who applied it to the lesion using a cotton swab. The patient observed there was
an initial “slight burning sensation, which felt healing” immediately after the
first application. The application was repeated every 2 hours by the patient.
Within 2 days the lesion had decreased in size. The pustular lesion gradually
dried. The pain was reduced from an 8 to a 4 on a visual analog scale of 0-10
within 4 hours. Within 6 days the lesion had healed completely. The usual
time-frame for lesions to heal for this patient was 10 days. Following this pro-
cedure the patient reapplied eucalyptus to lesions as they occurred. Follow-up
revealed the outbreaks appeared less frequently over a period of 1 year.
Note: The clinical aromatherapy objective to alter level of comfort was mea-
sured (by visual analogue) and achieved.
Choice of Essential Oil
Eucalyptus has a well-earned reputation for being a good all-around antimicro-
bial agent. Hmamouchi et al (1990) and Saeed and Sabir (1995) found Eucalyp-
tus globulus effective against all bacteria tested, and Benouda et al (1988) found
the action to be comparable to orthodox antibiotics. Eucalyptus was also found
to help the action of conventional antibiotics (Kufferath & Mundualgo 1954).
Used topically, it has analgesic (Weyers & Brodbeck 1989) and antiinflamma-
tory properties (Moscolo et al 1987). It is antifungal and is effective against
Cryptococcus neoformans, a common infection in immune-compromised patients
(Viollon & Chaumont 1994). It is antitumoral as well (Takasaki et al 1995).
Aqueous extracts of eucalyptus have been found to be antiviral (Takechi et al
1985), and anecdotal evidence indicates eucalyptus essential oil is very useful in
treating herpes and shingles.
1

Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 123
Case Study Alteration of Level of Comfort:
Malaise, Psoriasis
Outcome Criteria
Reduce itching and cracking lesions
Reduce scaliness of lesions
Improve comfort level of patient
M
r. A, a 51-year-old male with psoriasis, was offered aromatherapy to en-
hance comfort levels. He had classic, raised, white, scaly skin patches with
red borders. These intermittent, itchy skin lesions occurred on the skin surface
with predominance over the joints, resulting in cracked skin. Discomfort level
was a 7 on a scale of 0-10. A history of allergies and sensitivity was taken. The
patient liked the aroma of lavender. Informed consent to aromatherapy was
given. A patch test of 4% lavender was applied on the upper, inner arm. No sen-
sitivity was recorded after 24 hours. A 2% solution (2 drops lavender to 5 ml
cold-pressed vegetable oil) was applied to one lesion twice a day. As 2 days
passed, the redness, scaliness, and size of the lesion decreased, but the itching re-
mained unchanged. The lavender solution was applied to all the lesions of the
same leg. Within 7 days there was marked improvement in the size, redness, and
scaliness of the lesions to the extent that aromatherapy was discontinued on that
leg. Discomfort was now a 0 on a scale of 0-10 for those areas. The lesions on
other parts of the body that did not receive aromatherapy remained the same.
Note: The clinical aromatherapy objective to alter level of comfort was mea-
sured (by visual analogue) and achieved.
Choice of Essential Oil
Lavender is a classic essential oil for skin problems. It was used for wound
cleaning in World War I and was approved by the French Academy of Medi-
cine. As well as proven antibacterial action against many pathogenic organisms
including methicillin-resistant Staphylococcus aureus (Nelson 1997), lavender has
local-anesthetic effects (Ghelardini et al 1999) and is skin regenerative (Valnet
1990). Lavender inhibits histamine release in immediate-type allergic reactions
in mice and rats (Hyung-Min & Seong-Hoon 1999) and may be useful in aller-
gic skin problems linked to immune deficiency. Lavender was also found to be a
mood elevator by Corner et al (1995) and a sedative by (Elisabtsky et al 1995).
Nachi (1990) reported on the calming effects of lavender with patients under-
going magnetic resonance imaging. Saeki (2000) found lavender to be relaxing,
and Itai et al (2000) reported on the antidepressant properties of lavender with
chronic hemodialysis patients. Many patients with psoriasis (though not neces-
sarily the one in this case study) have stress-related depression, which is another
reason lavender can be beneficial. Lavender also enhances the sedative effects of
conventional pharmaceuticals (Stanassova-Shopova et al 1972), and lavender is
readily absorbed through the skin ( Jager et al 1992).
2

124 Section I Overview
Case Study Alteration of Comfort/Chronic Low
Self-Esteem: Vaginal Yeast Infection
Outcome Criteria
Reduce discomfort
Remove vaginal yeast infection
Improve self-esteem
M
iss C was a 21-year-old woman with diabetes. Her blood sugar was
around 130. Her diabetes was stabilized with diet and insulin injections.
She had a recurrent vaginal yeast infection and had previously used conven-
tional antifungal drugs (Terazol and Femstat). These gave temporary relief, but
only after 5 days of treatment. She was frustrated and unable to cope with the
recurrent infections, which were impacting her self-esteem. Her discomfort was
8 on a numerical scale of 0-10. The patient inhaled the aroma of tea tree and
commented it didn’t smell wonderful, but she just wanted some relief from the
itching. Informed consent was given and a patch test of 4% tea tree oil was car-
ried out. No irritation or sensitization was observed after 24 hours. The patient
was directed to dilute tea tree to the correct solution and apply it to a tampon.
She was told to apply it vaginally three times a day, each time with a fresh solu-
tion of 2% tea tree oil (two drops of tea tree in 5 ml cold-pressed sweet almond
oil). She said after insertion the tea tree tampon felt pleasantly tingly, rather like
the effect of toothpaste while cleaning her teeth. She carried out the treatment
and reported all evidence of vaginal yeast infection disappeared after 3 days, and
on a numerical scale the discomfort was a 0. On follow-up, 6 months later the
infection had not reappeared. She felt empowered and happy to look after her
own vaginal comfort. Her level of self-esteem was enhanced.
Note: The clinical aromatherapy objective to alter level of comfort was mea-
sured (by visual analogue) and achieved.
Choice of Essential Oil
Melaleuca alternifolia (tea tree) is one of the classic aromatherapy choices for
treating infection and is safe to use vaginally (Northrupp 1995). Tea tree is use-
ful for either bacterial infections such as abscesses, acne (Carson & Riley 1994),
or fungal infections including athlete’s foot, tinea (Tong et al 1992), impetigo or
viral infections such as cold sores and herpes (Hammer et al 1996). Pena (1962)
showed its effectiveness for yeast infection, trichomoniasis, and anaerobic infec-
tions (Blackwell 1991). For vaginal infection, dilute the essential oil in a cold-
pressed vegetable oil (for example sweet almond) and apply on a tampon. Mix
two drops of tea tree in one teaspoonful of carrier oil. Roll a tampon in the
mixture and insert into vagina. Repeat with fresh tampon every 4 hours and
leave in overnight. Relief should occur within 3 days. Vaginal thrush is unlikely
to reoccur (Buckle 2001).
3

Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 125
The next case study discusses using aromatherapy during extubation (the
process of removing an endotracheal tube when a patient is capable of breathing
without artificial help). This is a common task within the remit of an intensive-
care nurse. Yang & Tobin (1991) state there is “no one method of weaning
which has clear superiority.” However, weaning requires patient physical and
psychological preparedness (Logan & Jenny 1990). Extubation is a skilled nurs-
ing maneuver because patients must be alert enough to breathe on their own,
but not so alert that the endotracheal tube is causing distress and they are fight-
ing the ventilator.
Case Study Dysfunctional Ventilatory Weaning Response
Outcome Criteria
Achieve weaning goals
Remain extubated
Not be exhausted by the process of weaning
T
he nursing intervention consisted of the following.
Determined readiness for weaning
Asked if patient liked the smell of an essential oil such as lavender
Asked for permission to touch the patient
Explained the weaning process and demonstrated hand “m” technique using
lavender
Explained patient’s role in the process of weaning
Enhanced patient’s feelings of self-esteem through encouragement
Promoted trust through conversation and touch
Reduced negative effects of anxiety and fatigue through the use of aro-
matherapy
Created a positive environment with aromatherapy
Optimized comfort status through aromatherapy
Please see patient’s chart, Fig 6-1. The arrow indicates when the “m” technique
was used with 2% lavender.
4
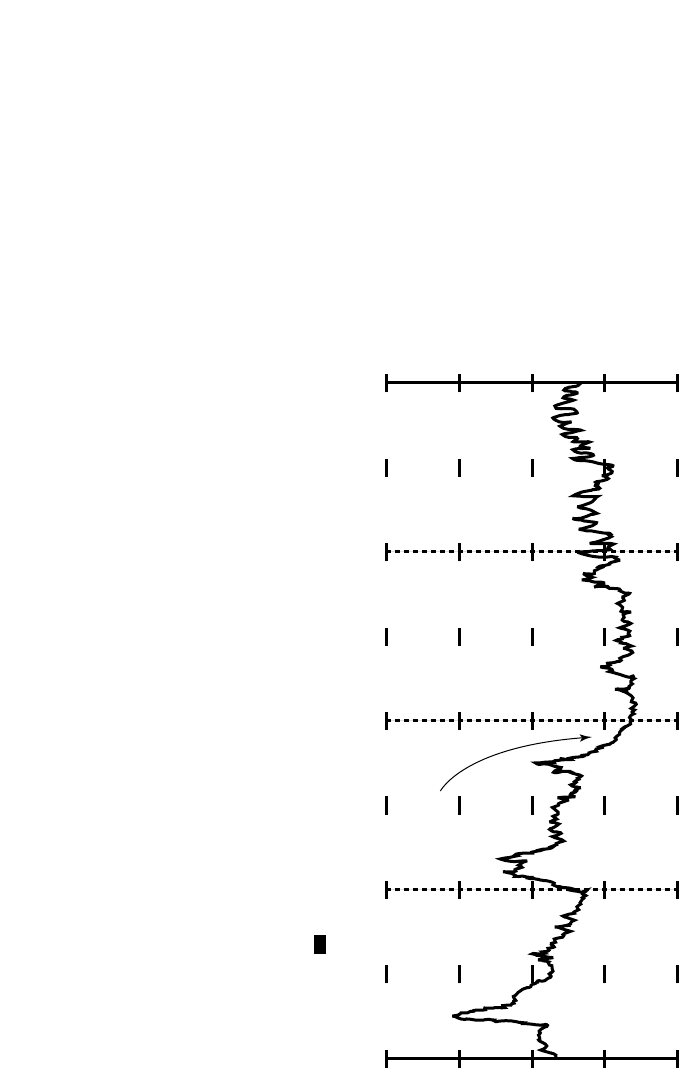
126 Section I Overview
GRAPHIC TRENDS
50
75
100
125
150
50
75
100
125
HR
bpm
150
07:58
29 Apr
Patient Name:
Bed Number: 166
Care Unit:
....
Aromatherapy was
applied topically here.
Date Printed: 29 Apr 1994
Time Printed: 16:01
Page: 1 of 1
09:58 11:58
(extubation)
13:58 15:58
29 Apr
Figure 6-1 Patient’s chart showing decrease in pulse when aromatherapy applied topically. (Courtesy Lori Mitchell)

Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 127
Case Study Alterations of Comfort Level: Chronic Pain
Outcome Criteria
Relax patient
Reduce perception of pain
M
rs. G was a 74-year-old woman with cancer and bone metastases. She
was in severe pain (8 on the numeric pain intensity scale) despite having
a patient-controlled analgesia of morphine. She was unable to find a comfort-
able position in bed and became withdrawn and depressed. Her muscles became
tight from attempting to “hold” her pain. Two drops of rose essential oil were
applied to a cotton hankie that was pinned on the patient’s nightgown. The af-
fect was almost instant: the patient took some deep breaths, opened her
clenched fists, and smiled for the first time in many weeks. This treatment was
repeated every 4 hours, and an electronic diffuser was used at night. The aroma
of the garden appeared to alter the patient’s perception of pain, reducing it to a
3 on the pain scale, and although the terminal nature of her disease was not af-
fected, the quality of her life appeared to be considerably improved.
Note: The clinical aromatherapy objective to alter level of comfort was mea-
sured (by visual analogue) and achieved.
Choice of Essential Oil
Rosa damascena (rose) is the most popular and acceptable aroma in the world,
recognized by almost every culture and religion. Bulgarian research indicates
rose oil reduces hypertension (Kirov & Bainova 1988) and counteracts the ef-
fects of isoprenaline (Brud & Szydlowska 1991). This agrees with the histori-
cally held belief that rose strengthens and calms the heart (Lawless 1995). Rose
is also an antispasmodic and a mild sedative. It has antidepressant properties (as
anyone who has sat for a while in a rose garden can affirm). A Russian study on
Rosalin (an ointment containing rose) showed the ointment had good antibac-
terial properties. This was presumably why Nostradamus used it to protect him-
self against the plague. Further studies indicate rose essential oil has an in-
hibitory effect on Helicobacter pylori (Boyanova & Neshev 1999). Rose has also
recently shown antiviral and antiHIV activity (Mahmood et al 1996).
Rose essential oil is useful to soothe radiodermatitis and is generally helpful to
all irritated skin. It is very important to use Rose otto (steam distilled) not Rose
absolute (extracted with petrochemicals) and to be sure to use pure rose oil.
Rose essential oil is expensive (between $1 and $2 per drop), but it is still less
expensive than conventional antidepressants as only a few drops are used at a
time.
5

128 Section I Overview
Case Study Spiritual Distress
Outcome Criteria
Continue spiritual practices as the patient knows them
Allow patient to express decreasing feelings of guilt and anxiety
Allow patient to express satisfaction with one’s spiritual condition
M
rs. H was an 85-year-old woman with depression. Many of her friends
were dead, and she lived a long way from her family who did not visit her
often. She did not sleep well and was prone to hyperventilation and palpita-
tions. She loved the smell of roses, which reminded her of a rose garden she
tended with her husband when he was alive. Informed consent was given. Two
drops of rose oil were inhaled on a facial tissue four times a day. In addition,
two drops of rose were added to a cotton ball placed under her pillowcase.
Within 1 week she was smiling, sleeping better, and discussing how she could
become involved with looking after the houseplants in the facility. Staff noted
she no longer hyperventilated and that she stopped complaining of palpitations.
The nursing intervention consisted of the following:
Provide privacy and quiet
Be open to the patient’s needs for spiritual peace
Contact the patient’s spiritual leader when required
Suggest aromatherapy might enhance the patient’s ability to meditate, pray,
or induce a state of peacefulness
Introduce the essential oils Boswellia carteri (frankincense) and Rosa damas-
cena (Rose)
Discuss the effects of both aromas
All people have a spiritual dimension, whether they choose to accept it or not
(Dickinson 1975). Spirituality is often at the core of a person’s distress, yet most
people find spirituality the most difficult subject about which to communicate.
During acute and chronic disease, many patients turn to their faith, lose their
faith, or seek a faith where there has been none previously. Despite this, nurses
commonly avoid addressing the spiritual dimension of a patient. Martin et al
(1978) suggest the spiritual part of nursing involves “being with” the patient
rather than “doing to” the patient. Stiles draws attention to the nurse-family
spiritual relationship in cancer care (Stiles 1990).
Aromatherapy allows nurses to “be with” their patients, even while they
may be “doing to,” in an intimate but professional way that nurtures the rela-
tionship between the nurse and the patient. This often allows a window of inner
reflection in which spiritual feelings (or needs) are verbalized. During my edu-
cation as a nurse, and subsequent to it, I noticed few patients are brought up the
subject of spiritual matters. Yet since I have been using aromatherapy, this sensi-
tive area has arisen time and time again, almost as though the aromas them-
selves provide an atmosphere of acceptance.
6

Conclusions
A few case studies have been presented above as a brief argument to support the
use of aromatherapy as an enhancement to nursing care. Nurses already use many
over-the-counter products not prescribed by a physician, such as scented soaps
and hair spray. Nurses also use synthetic sprays to mask human smells, and many
of the synthetic aromas in these sprays have not been tested for long-term effect
on patients. The time has come to think about what aromatherapy could mean in
nursing terms: how it could enhance what nurses do and how it could enhance
their job satisfaction.
One of my students said, “Aromatherapy has really changed my life; now I
notice what smells good and what doesn’t.” She went on to say, “So much in life
smells bad, doesn’t it? I wonder if that is because we have made a nonsense of na-
ture.”
We are making a nonsense of nursing care if we do not allow nurses the free-
dom to make their patients feel as comfortable as possible. What better way than
through gentle touch and the use of natural aromatics that are already part of
everyday life? Even before palliative care became an accepted specialty within
nursing, nurses still carried out palliative care. Then it became recognized as a dis-
tinctive and very caring form of health care. Before the first heart transplant, peo-
ple thought heart transplants were not possible. Now there are countless books on
surgery and cardiac nursing. Nursing as a profession is evolving as world percep-
tion changes. Nurses are already using aromatherapy in many parts of the world.
They are using it because it has validity, whether one’s view of nursing care is in-
tuitive, derived through nursing diagnosis, or derived from conceptual nursing
frameworks and theories.
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 129
Dossey (1993) writes about the need for thought to be accepted as being as
genuine as any drug or surgical procedure. The thoughts generated by gentle
touch and pleasing smell have a powerful effect on our psyche and on our spiri-
tuality. It is not only what nurses do for patients, but also their good intentions
to “be with” them that can aid the healing process. Nursing has a curative po-
tential. Despite the fact that 15% of nurses feel they are not prepared to provide
spiritual care (Stiles 1990), they can provide spiritual support just by being
there. Aromatherapy gives nurses permission to be there. A leading Buddhist
teacher wrote about his own experience with his dying father, and his words are
very indicative of what nurses do as part of nursing care. “There wasn’t much to
say. I held his hand. He was frightened. He didn’t want to know about medi-
cine. He didn’t even want to talk. What mattered was that I sat there, not being
afraid, not rejecting his fear and his pain, simply by holding his hand. He died
after several more days” (Kornfield 2000).

How Aromatherapy Could be Used in Hospitals
There are many potential uses for aromatherapy in hospitals. They range from the
simple mood-enhancing effects of smelling something pleasant to the specific ap-
plication of an antiseptic essential oil to combat cross-infections. At present most
hospitals do not smell nice, and science has shown how we feel affects how we
are. If it is possible to alter our environment to make it supportive in times of
need, surely this is something to be taken seriously.
Steele (1993) tested volunteers using an electroencephalogram to demon-
strate changes following the inhalation of certain essential oils. He discovered
changes in brain rhythms occurred within 15 seconds, and a positive change in
mood took approximately the same length of time.
Patients undergoing radiotherapy or computer-assisted tomography scans are
isolated in a room during treatment and have to lie absolutely still for lengthy pe-
riods of time. Many find this experience stressful. A soothing, relaxing essential
oil such as lavender (Lavandula angustifolia), vetiver (Vetiveria zizanoides), or
bergamot (Citrus bergamia) might help them. Balacs (1991) reports on research
that showed 60% of patients exposed to a sweet, vanilla-like fragrance (he-
liotropin) experienced less anxiety than the control group.
Emergency rooms receive victims of traffic accidents, burns, and poisoning
for whom immediate action is needed. Frequently relatives find it difficult to stay
calm enough to explain exactly what happened, and medical professionals find it
hard to maintain patience, knowing that every second is vital but needing precise
information. By combining an antiseptic essential oil with a calming one, the en-
vironment is immediately made more reassuring and more hospitable.
Wards for long-term care often have unattractive smells: a mixture of incon-
tinent patients, hospital food, and lavatory cleaner. Helen Passant, a nurse, man-
aged to change that situation in an Oxford, England hospital when she intro-
duced the use of aromatherapy. Her elderly patients responded to the use of touch
and massage, becoming “alive” again: a situation reminiscent of the film Begin-
nings. The aromas evoked memories, and the patients began to talk about their
lives and communicate their feelings. No longer isolated men and women wait-
ing to die, the patients became an active group: talking, then singing, then danc-
ing. In addition, the ward’s drug bill was reduced by a third. The hospital re-
warded her by reducing her budget by a third!
Many operating theatres have closed air conditioning. This means the same
air is ventilated constantly. It is much less expensive than open air conditioning,
which sucks in a constant stream of new air, warms (or cools) and filters it, then
vents it back into the outside environment. Research has been carried out on air-
borne infections and on the prevalence of postoperative wound infections. Cruse
(1980) found sufficient data to indicate postoperative wound infections, from pre-
operatively clean wounds, are directly related with the length of operating time.
Diffused essential oils with good antibacterial and antiviral properties may reduce
130 Section I Overview

the cost of the additional days incurred for in-patients and for those with noso-
comial (hospital-acquired) wound infections.
Some enlightened hospitals are using antibacterial essential oils in their op-
erating rooms, with the added bonus of preventing cross-infection among med-
ical staff. Each operating room has specific bacteria and viruses that are most
prevalent, so a customized cocktail of several essential oils is employed. Use of a
pleasant and uplifting essential oil, such as pine (Pinus sylvestris) or lemon (Cit-
rus limonum) can also improve the concentration of operating staff at night.
The use of aromatherapy in hospitals in England, South Africa, Switzerland,
and, more recently, in the United States shows a progressive trend toward sup-
porting patients on a more holistic basis. Physicians and hospital managers are
becoming aware that how patients feel can affect the way they respond to treat-
ment, and therefore how quickly they recover.
Planetree Hospitals Inc. is an American group of hospitals whose staff strive
to put the patient and the patient’s comfort first. It had a humble beginning in
1978; Angelica Thieriot found the routine medical treatment she received in the
late 1970s so dehumanizing she made it her mission to develop a new model of
patient-centered care.The concept of Planetree spread nationwide, and now there
are more than 40 similar hospitals and facilities throughout the United States. Pa-
tients are encouraged to take an active part in making decisions about their fu-
ture, and this begins with open medical records. Patients are also invited to have
a gentle massage prior to surgery and to ask their family and friends to bring in
their favorite food to prepare. There is a kitchen on every floor. Gentle music fills
the reception area, and nothing is too much trouble for the patient. It is no sur-
prise patients and staff gravitate toward Planetree!
Aromatherapy is a complementary therapy much accepted by the Planetree
philosophy. Desert Samaritan Hospital in Mesa, Arizona, is one of the first Plan-
etree hospitals to have sponsored nurses not just through an 18-month clinical
aromatherapy training program but to become paid instructors themselves.
Touch is known to have a dramatic effect on patients, and yet patients lying
in a hospital bed are rarely touched, except for diagnostic (palpation) or proce-
dural reasons (changing a dressing, blood-pressure recording). One method gain-
ing popularity among nurses is the “m” technique. This method of touch is de-
scribed more fully in Chapter 8 and quickly acknowledges a patient’s worth as an
individual. A foot or hand “m” takes only 5 minutes, but that time can totally
change the way patients perceive the environment around them. Touch has also
been shown to reduce blood pressure, reduce lower back pain, relieve anxiety, and
alleviate depression (Montagu 1986).
Aromatherapy using touch and smell could be a complete hospital stress-
management package, producing a happier and more content workforce with
more secure and less anxious patients. The level of interest in aromatherapy
shown by patients and nurses suggests an overwhelming desire for such integra-
tion.
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 131

Hospitals are being run like businesses. Therefore, the cost benefits of using
essential oils to promote healing need to be addressed, and I hope this book will
go some way toward that. There are a few ethical questions. What about consent?
Is it ethical to manipulate mood? What about a patient who does not like the aro-
mas? Yet how many patients sign a consent form approving the smell of antisep-
tics or air fresheners? How many nurses enter their place of work having used
scented soap, hair spray, or aftershave? How many patients are allergic or sensi-
tive to Lysol or other cleaning fluids used in hospitals? It is difficult to have one
set of rules for aromatherapy if there are no rules governing other types of scent.
Another area of concern is the potential use of synthetic or adulterated es-
sential oils that result in poor or negative results. It cannot be emphasized
strongly enough that it is the quality of the essential oil that will determine the
final result. Essential oils need to be judged like good wine. Good wine is expen-
sive, and so are the best essential oils.
Perhaps one of the greatest concerns about using aromatherapy in hospitals
is incorrect use due to ignorance. Contrary to media hype, aromatherapy is not
the panacea for everything, a kind of “comfort-blanket” smell. Of equal impor-
tance is the quality of accompanying touch. A heavy, compressing, rapid stroke
will not produce the same effect as a light, slow, gentle one. The techniques used
in aromatherapy cannot be learned solely from a book; they need to be experi-
enced.
There is an urgent need for adequate training, and reading a book is not
enough. As well as learning the “m” technique, the use of essential oils in aro-
matherapy requires knowledge and experience. A simple name like lavender cov-
ers three completely different species, each with entirely different therapeutic ef-
fects. Lavandula angustifolia is a sedative, Lavandula latifolia is an expectorant,
and Lavandula stoechas is effective against Pseudomonas aeruginosa. For Nurse
Practice Acts please see www.rjbuckle.com or www.ahna.com.
Consider the following. A patient likes the smell of lemongrass and needs an
essential oil with sedative effects. The patient feels isolated. A daily foot “m” tech-
nique is chosen and added to the care plan. The patient also has a fungal infec-
tion that appears to lessen following a number of foot massages with lemongrass.
Although lemongrass had not been used ostensibly for its antifungal properties,
it cannot stop itself from being antifungal. But what if a health professional with-
out prescriptive powers had known about the antifungal properties and had cho-
sen lemongrass primarily because of them? Would he or she have crossed the
boundaries? The International Council of Nurses states that nurses’ “fundamen-
tal responsibility is to conserve life, to alleviate suffering and to promote health.”
Using aromatherapy in this way could be seen to be alleviating suffering. How-
ever if the targeted outcome of an essential oil is changed to one outside the ju-
risdiction of the provider, a different protocol might be required.
Appendix VI is a list of hospitals using aromatherapy or having sponsored
nurse’s training in aromatherapy.
132 Section I Overview

REFERENCES
Abdellah F, Levine E. 1965. Better Patient Care Through Nursing Research. New York:
Macmillan.
Balacs T. 1991. Fragrance relaxes. International Journal of Aromatherapy. 33(3) 8.
Bender J. 2001. Nursing shortages have hospitals sending SOS. South Florida Business
Journal. Retrieved August 4, 2001 from http://www.southflorida.bcentral.com.
Benouda A, Hassar M, Benjilali B. 1988. The antiseptic properties of essential oils in
vitro, tested against pathogenic germs found in hospitals. Fitoterapia. 59(2) 115-119.
Blackwell R. 1991. Teatree oil and anaerobic vaginosis. Lancet. 337(8736) 300.
Boyanova L, Neshev G. 1999. Inhibitory effect of rose oil on Helicobacter pylori growth
in vitro: preliminary report. Journal of Medical Microbiology. 48(7) 705-706.
Brud W, Szydlowska I. 1991. Bulgarian rose oil. International Journal of Aromatherapy.
2(3) 18-19.
Buckle J. 2000. The ‘m’ technique. Massage and Bodywork. (Feb/March) 52-68.
Buckle J. 2001. The role of aromatherapy in nursing care. Nursing Clinics of North
America. 36(1) 57-72.
Bulechek G, McCloskey J. 1985. Nursing Interventions: Treatment for Nursing Diagno-
sis. Philadelphia: WB Saunders.
Carpenito L. 1993. Nursing Diagnosis: Applications to Clinical Practice, 5th ed. Mickle-
ton, NJ: JB Lippincott.
Carson C, Riley T. 1994. Susceptibility of Propionibacterium acne to the essential oil of
Melaleuca alternifolia. Letters Applied Microbiology. 19(1) 24-25.
Corner J, Cawley N, Hildebrand S. 1995. An evaluation of the use of essential oils on
the well-being of cancer patients. International Journal Palliative Nursing. 1(2) 67-73
Crow K. 2001. Healing and burnout, 12 hours at a stretch. New York Times. Sunday
June 24. 15.2-15.3.
Cruse P. 1980. The epidemiology of wound infection: a ten-year prospective study of
69,939 wounds. Surgery Clinics of North America. 60, 27-40.
DeMetro R. 2001. Medical stripmining and the new nursing shortage. Retrieved August
4, 2001 from http://www.califnurses.org.
Dickinson C. 1975. The search for spiritual meaning. American Journal of Nursing. 75,
1789–1793.
Dossey L. 1993. Healing Words. San Francisco, CA: HarperCollins.
Elisabtsky E, Coelho de Souza G, Dos Santos M et al. 1995. Sedative properties of
linalool. Fitoterapia. 66(5) 407-415.
Ghelardini C, Galeotti N, Salvatore G et al. 1999. Local anesthetic activity of essential
oil of Lavandula angustifolia. Planta Medica. 65(8) 700-703.
Gordon M. 1990. Towards theory-based diagnostic categories. Nursing Diagnosis. 1(1)
5-11.
Hammer K, Carson C, Riley T. 1996. Susceptibility of transient and commensal skin
flora to the essential oil of Melaleuca alternifolia. Australasian Journal of Infection
Control. 24(3) 186-189.
Hmamouchi M, Tantaoui-Elaraki A, Es-Safi N et al. 1990. Illustration of antibacterial
and antifungal properties of Eucalyptus essential oils. Plantes Medicinales et Phy-
totherapie. 24(4) 278-289.
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 133

Hyung-Min K, Seong-Hoon C. 1999. Lavender oil inhibits immediate-type allergic re-
action in mice and rats. Journal of Pharmacy and Pharmacology. 51, 221-226.
Itai T, Amauadu H, Kuribayashi M et al. 2000. Psychological effects of aromatherapy
on chronic hemodialysis patients. Psychiatric and Clinical Neurosciences. 54(4)
393-397.
Jacob J. 2001. AMA house goes after nursing shortage issue. Retrieved August 4, 2001
from http://www.ama-assn.org.
Jager W, Buchbauer G, Jirovetz L et al. 1992. Percutaneous absorption of lavender oil
from a massage oil. Journal of the Society of Cosmetic Chemists. 43(1) 49-54.
Kirov A, Bainova M. 1988. Rose oil: acute and subacute oral toxicity. Medico Biologic
Information. 3:8-14.
Kornfield J. 2000. After the Ecstasy, the Laundry. Woodacre, CA: Rider.
Kufferath F, Mundualgo G. 1954. The activity of some preparations containing essential
oils in Tuberculosis. Fitoterapia. 25:483-485.
Lawless J.1995. Rose Oil. London: Thorsons, 20.
Leddy S, Pepper J. 1993. Conceptual bases of professional nursing. Mickleton, NJ: JB
Lippincott.
Logan J, Jenny J. 1990. Deriving a new nursing diagnosis through qualitative research:
dysfunctional ventilatory response. Nursing Diagnosis. 1, 37-43.
Mahmood N, Piacente S, Pizza C et al. 1996. The anti-HIV activity and mechanisms of
action of pure compounds isolated from Rosa damascena. Biochemical and Biophysical
Research Communications. 229(1) 73-79.
Martin C, Burrow C, Pomilio J. 1978. Spiritual needs of patients’ surveys. In Fish S,
Shelly J (eds.), Spiritual Care: The Nurse’s Role. Downers Grove, IL: InterVarsity
Press.
McNeese-Smith D. 1999. A content analysis of staff nurse descriptions of job satisfac-
tion and dissatisfaction. Journal of Advanced Nursing. 29(6) 1332-1341.
Montagu A. 1986. Touching. New York: Harper & Row.
Moscolo N, Autore G, Capasso F et al. 1987. Biological screening of Italian medicinal
plants for anti-inflammatory activity. Phytotherapy Research. 1(1) 28-31.
Nachi K. 1990. Aromachology: the psychic effects of fragrances. The Futurist. 24, 49-50.
Nelson R. 1997. In vitro activities of five plant essential oils against MRSA and VREF.
Journal of Antimicrobial Chemotherapeutics. 40, 305-306.
Nevidjon B, Erickson, J. 2001. The nursing shortage: solutions for the short and long
term. Online Journal of Issues in Nursing. Retrieved August 4, 2001 from
http://www.nursingworld.org/ojin/topic14/tpc14_4.htm.
Northrupp C. 1995. Women’ Bodies, Women’s Minds. London: Piatkus.
Pena E. 1962. Melaleuca alternifolia oil: Its use for trichomonal vaginitis and other vagi-
nal infection. Obstetrics & Gynecology. 19(6) 793-795.
Reid J. 2001.Getting the massage across. Nursing Times. 97(15) 26-27.
Saeed M, Sabir A. 1995. Antimicrobial studies of the constituents of Pakistani eucalyp-
tus oils. Journal of Faculty of Pharmacy of Gazi University. 12(2) 129-140.
Saeki Y. 2000. The effect of foot bath with or without the essential oil of lavender on the
autonomic nervous system: a randomized trial. Complementary Therapies in Medi-
cine. 8(1) 2-7.
Short L. 2001. Nurse was an angel at accident scene. Albany Times Union. Sunday July
8, B4.
134 Section I Overview

Stanassova-Shopova S, Roussinov K, Boycheva I. 1973. On certain central neurotropic
effects of lavender essential oil. II. Communication: Studies of the effects of linalool
and terpineol. Bulletin of the Institute of Physiology. 15:149-156.
Steele J. 1993. The fragrant hospital. In Aroma 93 Conference Proceedings. Brighton,
UK: Aromatherapy Publications, 22-29.
Stiles M. 1990. The shining stranger: nurse-family spiritual relationship. Cancer Nurs-
ing. 13, 235-256.
Swansea Hospital Department of Genito-Urinary Medicine, Swansea, UK. 1991.
Teatree oil and anaerobic vaginosis. Lancet. 337(8736) 300.
Takasaki M, Konoshima T, Kozuka M et al. 1995. Anti-tumor promoting activities of eu-
glabols from eucalyptus plants. Biological and Pharmaceutical Bulletin. 18(3) 435-438.
Takechi M, Tanaka Y, Takehara M et al. 1985. Structure and antiherpetic activity among
the tannins. Phytochemistry. 24(10) 2245-2250.
Thompson C. 2001. Oil on troubled water. Nursing Times. 97(15) 24-26.
Tong M, Altman P, Barnetson R. 1992. Teatree oil in the treatment of Tinea Pedis. Aus-
tralasian Journal of Dermatology. 33(30) 145-149.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Viollon C, Chaumont J. 1994. Antifungal properties of essential oils and their main
components against Cryptococcus neoformans. Mycopathologia. 128(3) 151-153.
Weyers W, Brodbeck R. 1989. Skin absorption of volatile oils. Pharmacokinetics. Pharm
Unserer Zeit. 18(3) 82-86.
Yang K, Tobin M. 1991. A prospective study of indexes predicting outcomes of trials
of weaning from mechanical ventilation. New England Journal of Medicine. 324,
1445-1451.
Chapter 6 Evidence-Based Aromatherapy in Nursing Practice 135

W
136
7
Oral and Internal Use
of Aromatherapy*
Science and myth are one; the natural world is but a manifestation of thoughts and
impulses all occurring on endless metaphysical planes, all enveloped by the mind of
the healer.
Wade Davis
One River
T
HE TOPIC of oral and internal use of essential oils is controversial and con-
fusing. Much of the confusion is due to lack of knowledge and cultural
misconceptions because the oral and internal uses of essential oils are not
taught in most aromatherapy training programs in the United States or United
Kingdom.
There are three probable reasons for this omission.
1. Many training programs are intended for the lay public, not licensed
health professionals (LHPs).
2. Most adverse interactions with conventional medications are associated
with the oral use of essential oils.
3. There is a fear that oral use of essential oils may lead to poisoning.
However, this book is intended for LHPs who may wish (or need) to know
about the oral and internal use of essential oils so they can decide for themselves.
Ultimately, LHPs will need to decide if giving essential oils either orally or inter-
nally is within their license. The views in this chapter are mine, and this chapter
is intended to open a dialogue not provide an answer.
*I am greatly indebted to the aromatic medicine courses I took with Penoel, Franchomme, Schnaubelt,
Price, Harris, and Guba for this section. It is strongly recommended that the reader undertake a pro-
fessional course in aromatic medicine before using essential oils orally or in high concentrations, as
these methods are not covered in most aromatherapy courses.

The sale and use of essential oils, much like herbal remedies, is not controlled
in the United States (or England or France). Essential oils can be purchased by
anyone and used in any way. If, however, LHPs are using essential oils to enhance
care, they will need to decide if this use fits within the parameters of their licenses.
Broadly speaking, LHPs can be divided into those who have prescriptive
powers and those who do not. Those who have prescriptive license may feel more
comfortable using the oral route of aromatherapy than those who do not. This
does not mean only those who have prescriptive license may use the oral route,
only that they may feel more comfortable doing so. Whatever the kind of license
a health professional has, he or she has accountability. Therefore the treatment of-
fered should be based on training received.
There are several anomalies in the practice of aromatherapy in the United
States (and England). The first is over-the-counter herbal remedies and essential
oils are freely available, and many people self-medicate.
The second anomaly is that although aromatherapy uses different methods:
topical, inhalation, and oral, two major organizations in the United Kingdom
voted against the oral use of essential oils. This is important as the United States
has tended to look to the United Kingdom for aromatherapy guidelines. The
Aromatherapy Registration Council (AOC), the lead aromatherapy body in
the United Kingdom, stated the oral use of essential oils was not acceptable. The
Royal College of Nursing (RCN) in London (which decides what a nurse may
practice) also stated the oral use of essential oils lay outside the boundaries of
nursing care. The AOC may well have based its decision on the fact that the ma-
jority of aromatherapy practitioners in the United Kingdom are lay people. The
RCN may have made its decision because using the oral route of aromatherapy is
comparable to taking medicine, and nurses are not allowed to give medicines
without a prescription.
The third anomaly is the majority of aromatherapy courses focus on esthet-
ics or stress, where internal and oral methods would not be relevant. So the idea
has permeated the aromatherapy community that the oral route of essential oils
is somehow out of bounds. This is understandable, but it has never been formally
challenged or accepted. However, courses that are clinically oriented and intended
for LHPs need to address the oral and internal use of aromatherapy because these
methods could be very relevant.
The fourth anomaly is confusion between oral and internal use. The two
words are not synonymous. One includes the digestive process and the other does
not. The oral process involves taking essential oils by mouth, either in capsules or
diluted and swallowed. Very small amounts of essential oils are used in foods and
candy, such as peppermint and wintergreen, therefore thousands of people take
essential oils orally every day. The internal use of essential oils includes putting
them into any orifice: mouth, ear, nose, anus, or vagina. However, in this case, the
essential oil is not swallowed. A clear example of this is a mouthwash. Several
proprietary mouthwashes state on their labels “do not swallow.” Clearly there is
an established, recognizable difference between oral and internal use. Ear drops,
Chapter 7 Oral and Internal Use of Aromatherapy 137

nasal irrigation, and vaginal douches and creams can be applied to the internal
skin of the body and absorbed that way. They are not digested. However, all
routes, including the rectal one, are excellent ways of getting oils into the system
while bypassing the liver (Schnaubelt 1998). Several products that utilize the in-
ternal skin and include essential oils are available at drug stores and health-food
stores.
The fifth anomaly is the dilution or the amount of essential oil used. The
standard dilution for topically applied essential oils taught in aromatherapy train-
ing is between 1% and 5%. This is suitable for stress management and esthetics
and may be very effective for some clinical conditions. However in the case of an
infection, considerably higher percentages might be required. Some over-the-
counter remedies contain high percentages of essential oil components. For ex-
ample, Bengay analgesic cream contains 15% methyl salicylate (found in winter-
green) and 10% menthol (found in peppermint). Higher percentages, and in some
cases, undiluted essential oils may be required to treat chronic or acute infection.
The original concept of prescription medicine was to protect the public from
themselves. An extension of the Hippocratic oath, “first do no harm” is “keep
them from harming themselves,” which includes instructions for safe use. For
aromatherapy, this would mean knowing the maximum amount of essential oil
that could be used safely.
The sixth anomaly is in other parts of the world, where aromatherapy is not
regulated, essential oils are frequently given orally by licensed and nonlicensed
practitioners.
The seventh anomaly is the size of a drop of an essential oil can vary consid-
erably. Much depends on whether the dropper is an integral one or a pipette. The
integral droppers produce approximately 20 drops per milliliter. The pipettes pro-
duce closer to 40 drops per milliliter. This becomes very important when the
maximum amount for a particular essential oil is measured in drops per day.
The Oral Route
There is a long history in the United States of nurses and physicians giving es-
sential oils orally to their patients prior to the advent of modern pharmaceuticals.
Several essential oils such as cinnamon, clove, peppermint, sandalwood, and eu-
calyptus are actually listed in the 8th edition of Useful Drugs, a handbook pub-
lished by the American Medical Association in 1930. Sandalwood was classically
given for urinary infections. The majority of animal studies on this oil have in-
cluded the oral route, and there is a great deal of information on toxicity.
One of the main reasons for using the oral method at all is to treat the in-
testinal tract, as almost every other system can be reached by the topical or in-
haled route. The oral method is perfectly safe and nontoxic, provided the giver is
trained in this method and appropriate dosages are not exceeded. However, not
all essential oils are safe to use orally. Burfield (2000) cautions that certain essen-
tial oils such as hyssop, wormwood, and wintergreen should never be taken orally.
138 Section I Overview

Essential oils that are high in phenols should be diluted and contained in gelatin
capsules to avoid mucous irritation when administered orally.
Most insurance companies that cover aromatherapy exclude the oral use of
essential oils. However this route is a valid option, and there are several excellent
training courses available. I believe the fear of using essential oils orally is really
based on a lack of knowledge. Again, as always, education is the key. As essential
oils are very concentrated, doses are usually described in the number of drops
given. However, drop sizes vary (Olleveant et al 1999). Therefore it is more accu-
rate (and safer) to measure the amount of essential oil used in milliliters. Brinker
(2000), a naturopath, suggests the safe range for oral use is 0.5-1.0 ml/day, al-
though cautions apply for amounts greater than 0.5ml/day.
Method of Oral Use
Essential oils can be given orally in gelatin capsules, disper, activated charcoal, or
Vitamin C tablets. Some essential oils can be taken in honey for occasional use,
but not all therapists recommend this method. However some alcohol-rich es-
sential oils (such as palma-rosa) in honey can be excellent for a sore throat.
Gelatin Capsules
Size 00 capsules are filled with an essential oil or oils diluted in a vegetable oil.
The solution is made up first (up to 20% strength), then poured into the capsules
and the capsules are taken like ordinary medicines. Each capsule holds approxi-
mately 0.75 ml. The process of filling the capsules is time consuming, but this is
an excellent way to treat the small and large intestine. Guba (2002) suggests clove
bud and cinnamon oil for diarrhea and recommends 12 drops per day of each.
However, the Australian drop size may be smaller than the US drop size, so closer
to six drops per day of each may be all that is required.
Disper
Disper is a lecithin-based emulsifier that holds the essential oils in a stable dis-
persion. This emulsifier is rapidly absorbed by the stomach and is therefore use-
ful for acute and chronic infections. Disper can be combined with herbal tinctures
and is available from several aromatherapy supply companies. The recommended
proportion is one part essential oils to nine parts disper. If 1 ml of essential oil
(containing 20 US drops or 40 French drops) is added to 9 ml of disper, there will
be approximately 200 drops. Ten drops of the mixture will contain two drops of
essential oil. The disper mixture is then diluted in water and drunk. The taste will
depend on the essential oil but should not be too bitter or overwhelming. This
method is very simple to use.
Activated-Charcoal Tablets
Activated-charcoal tablets are available in many health-food stores. Two hundred-
milligram charcoal tablets are useful as a simple, effective base for carrying essen-
tial oils to the gastrointestinal tract. Each tablet will hold different amounts of an
Chapter 7 Oral and Internal Use of Aromatherapy 139

essential oil. Some essential oils dissolve the binders that hold the tablet together
so tablets should not be premixed. Charcoal tablets are not recommended for
long-term use as they can be constipating, but they can be useful for short-term
use of up to 1 week.
Vitamin C Lozenges
Guba (2002) suggests Vitamin C lozenges are also a good way of introducing an
essential oil orally. Place a few drops of the essential oil on the lozenge and wait
until it is absorbed. The lozenge can then be chewed and swallowed with water.
Honey
Essential oils can be blended with honey water. Mix the drops of essential oil in
a teaspoon of honey, add warm water, and drink. Rose is an excellent antiviral oil
to use in this way.
Enteric-Coated Gelatin Capsules
Enteric-coated gelatin capsules do not release the essential oil until they are in the
small intestine (an environment of pH 6.8 or higher). This can be useful for irri-
table bowel syndrome.
Human Studies on Oral or Internal Use
Kline et al (2001) used enteric-coated gelatin capsules containing peppermint oil
in the treatment of irritable bowel syndrome symptoms. Fifty children took part
in a controlled, multicentered study. Between one capsule (187 mg) and two cap-
sules was given three times a day. During the study eight children withdrew for
various reasons. However, 76% of the peppermint group showed significant re-
duction in symptoms compared to the placebo group (43%). No side effects were
reported, and there was no change in stool consistency.
Gravett (2001) prescribed a mixture of essential oils in honey water for pa-
tients with nausea, colicky pain, anorexia, and diarrhea who were undergoing
high-dose chemotherapy and stem-cell rescue. Eight patients took part in the
study. They took a daily dose of 15 drops of geranium, 10 drops of German
chamomile, 10 drops of patchouli, and 10 drops of turmeric (infused oil) in
honey water. The mixture was divided into three batches and taken orally at
equal intervals throughout the day. His patients had no ill effects from the es-
sential oils and felt better than members of the control group, who were using
conventional antiemetics. The cost of the aromatherapy treatment (28 pence ⫽
40 cents) was substantially less than the conventional treatment (138 pence ⫽
almost $2).
Belaiche (1985) carried out a double-blind study to examine the effectiveness
of Melaleuca alternifolia (tea tree) in the treatment of chronic cystitis. There were
26 participants in the study. The experimental group was given 24 mg of tea tree
divided into three doses of 8 mg each in enteric-coated gelatin capsules. The con-
trol group was given a placebo that had the odor of tea tree. After 6 months no
140 Section I Overview

one in the control group showed any improvement, but 7 of the 13 women in the
experimental group were completely cured (60%). During the 6 months of test-
ing, liver functions also were monitored. There were no liver problems, and no
side effects to the treatment.
Holmes (1995) describes a case study of a 23-month-old girl he treated for
cellulitis from an infected bite and a concurrent upper-respiratory viral infection
(tonsillitis). One drop each of tea tree, lavender, and calendula oils were added to
a small feeding bottle containing fruit juice, and the mixture was given to the
child to take orally, three times a day. The child also received a 20% solution of
lavender, Moroccan blue chamomile (Tanacetum annum), and calendula as a top-
ical treatment applied directly to the bite up to six times a day, as well as a 10%
dilution of tea tree, lavender, and calendula oils massaged into the chest and back
each morning and night. The fever subsided after the first day, and 4 days later
the cellulitis and tonsillitis were gone. It is difficult to extrapolate whether the oral
method would have worked on its own.
Suppositories
A suppository is another method of using essential oils not taught in many aro-
matherapy classes, but it has a place in clinical training. This internal method is
simple to use and very effective for treating many different systemic conditions.
The usual concentrations are 10% essential oil per suppository. This works
out to approximately 300 mg of essential oil per 3-g suppository. For children, one
drop of essential oil in a 25-mg suppository is appropriate. While molds are avail-
able, the standard 00-size gelatin capsule is just as effective. However, diluting the
essential oil in vegetable oil may result in leakage, so use cocoa butter, which is
solid but dissolves at body temperature. Melt the cocoa butter, mix in the essen-
tial oils, then fill the suppository mold. Store in refrigerator. Avoid using only
phenol-rich essential oils in rectal suppositories as this would produce irritation
as the suppository dissolves.
De la Motte et al (1997) used German chamomile in the form of an enema
and/or suppository to control noncomplicated diarrhea in children. Other essen-
tial oils that could have been used to control diarrhea are geranium and turmeric.
Geranium was shown to have antidiarrhea properties in animal studies (Ofuji et
al 1998), and turmeric was found to alleviate upper-abdominal pain due to biliary
dysfunction (Niederau & Opfert 1999). The rectal route is particularly suitable
for children, for those with gastric ulcers or gastritis, or when essential oils are not
tolerated via the oral route.
Licenses, Prescriptions, and Essential Oils
A dilemma may occur when oral or internal essential oils are used by an LHP
who does not have prescriptive privileges. I think nurses should know about the
oral uses of essential oils, but when they are practicing with their nursing license,
Chapter 7 Oral and Internal Use of Aromatherapy 141

the oral route should be avoided. This was made clear when the Massachusetts
Board of Nursing voted to accept aromatherapy as part of nursing care but did
not include herbal remedies, as herbal medicines are taken orally. However, nurse
practitioners, physicians, and others with diagnostic skills and prescriptive privi-
leges may wish to learn to use essential oils in this way and use them to great ef-
fect. In some states, if a lay person was to “prescribe” an essential oil to another
person, he or she could be accused of practicing medicine without a license.
Conventional medicine is not accustomed to a single medicine having sev-
eral different therapeutic effects. But essential oils clearly do have several differ-
ent therapeutic effects. They have multiple medicinal properties, but they also
give pleasure and help people relax. The Webster’s Dictionary definition of a med-
icine is “any substance used in the treatment of disease.” The word medicinal is de-
fined by the Oxford Dictionary as “something having healing properties.” Accord-
ing to several studies, prayer has a healing effect. Does this mean only a doctor
can pray? Does it mean when a rotation diet works, it is medicine and therefore
should be prescribed by a physician only? The idea is clearly absurd. Yet there is
something similar, but in reverse, happening in aromatherapy. To give an exam-
ple: when an essential oil is used for relaxation, it is not a medicine, but if that es-
sential oil is used for its antibiotic effect, it is a medicine. How could lavender be
a medicine (effective against methicillin-resistant Staphylococcus aureus) one mo-
ment and not a medicine (soothing and relaxing) the next? Does this mean a
medicine only becomes one when the giver intends it to be one?
There is growing interest and acceptance within conventional medicine for
the supplementary role of herbs in clinical practice, and some excellent studies
have been published on their efficacy. The potential for interdrug reactions and
toxicity issues is very small compared to the hundreds of thousands of deaths from
conventional drugs or drug interaction each year. In some instances essential oils
can actually enhance conventional medicines (particularly those for infection).
This will become very advantageous as more pathogens become resistant to or-
thodox antibiotics.
It is extremely unlikely that essential oils will only be available by prescrip-
tion. However, if this did occur, it would be relevant not only to physicians but
also to the growing number of nonphysician clinicians (NPCs) who have pre-
scriptive license. The next part of this section explores this option. Many of these
nonphysican clinicians are referred to as doctors or physicians by state regulation
or custom and are listed as such on many insurance forms. Cooper et al (1998)
divides the nonphysician group into three sections. See Table 7-1 for details.
For many years, physicians held a monopoly as the main providers of health
care (Cooper et al 1998). However, changes in state laws and regulations com-
bined with an increase in the numbers of practitioners in training means the
number of nonphysician clinicians is growing rapidly. As a consequence of
this growth, several NPC disciplines will soon be as large as the major specialties
in medicine (Cooper et al 1998). In 2005, it is estimated the number of NPCs in
clinical practice will be equal to the number of family physicians (Weiner 1994).
142 Section I Overview

A great number of NPC practices are involved with wellness clinics and the
treatment of uncomplicated acute and chronic conditions. These types of condi-
tions make up 50%-75% of office visits to primary-care physicians. Cooper et al
(1998) made projections as to the way each discipline would expand in 5 years.
See Table 7-2 for their estimates on the number of graduates in NPC disciplines.
NPCS are growing in popularity with the public, which perceives them as
providing a more caring service than conventional physicians, with more time to
listen to and be with their patients (Guglielmo 2001). According to the Ameri-
can Academy of Nurse Practitioners, more than 25% of NPs work in doctor-run,
Chapter 7 Oral and Internal Use of Aromatherapy 143
Table 7-1 h Types of Nonphysician Clinicians in the United States
Alternative
Conventional Medicine Practitioners Specialty Groups
Nurse practitioners (NPs) Chiropractors Optometrists
Certified nurse midwives Acupuncturists Podiatrists
(CNMs)
Physician assistants (PAs) Naturopaths Clinical nurse specialists
(CNRs)
Medical herbalists Certified registered nurse
anesthetists (CRNAs)
Table 7-2 h Projected Number of Nonphysician Clinician Graduates
in the United States
Discipline 1997 2001 (projected)
Acupuncturists 1030 2000
Certified nurse anesthetists 387 725
Certified nurse midwives 414 500
Chiropractors 4100 5200
Clinical nurse specialists 1365 2300
Naturopaths 170 350
Nurse practitioners 5350 7260
Optometrists 1235 1250
Physician assistants 2800 3400
Podiatrists 645 725

solo, or group practices. More and more health care insurance plans will begin to
cover NP and other NPC services as they are less expensive than physicians’.
This chapter has covered the oral and internal use of essential oils and has
also discussed the use of essential oils by LHPs who may or may not have pre-
scriptive privileges. The hope is that this information will start a dialogue to help
clinical aromatherapy become more accepted in health care practice.
REFERENCES
Belaiche P. 1985. Germicidal properties of the essential oil of Melaleuca alternifolia re-
lated to urinary infections and chronic ideopathic Colibacillus. Phytotherapie. 15:9-11.
Brinker F. 2000. The Toxicology of Botanical Medicine, 3rd ed. Sandy, OR: Eclectic
Medical Publications, 202.
Burfield T. 2000. Safety of essential oils. International Journal of Aromatherapy. 10(1/2)
16-29.
Cooper R, Laud P, Dietrich C. 1998. Current and projected workforce of nonphysican
clinicians. Journal of the American Medical Association. 280(9): 788-794.
Davis W. 1996. One River. New York: Simon & Schuster, 491.
De la Motte S, Bose-O’Reilly S, Heinisch M et al. 1997. Double blind comparison of an
apple pectin-chamomile extract preparation with placebo in children with diarrhea.
Arzneimittelforschung. 47(11) 1247-1249.
Fowler H, Fowler F (eds). 1972. Oxford English Dictionary (4th ed). Oxford, UK: Ox-
ford University Press.
Gravett P. 2001. Treatment of gastrointestinal upset following high-dose chemotherapy.
International Journal of Aromatherapy. 11(2) 84-86.
Guba R. 2002. Beyond Aromatherapy. Center for Aromatic Medicine. NSW. Australia.
Notes published by Center for Aromatic Medicine.
Guglielmo W. 2001. Above and beyond just doctoring. Newsweek. 72.
Hatcher R, Eggleston C (eds). 1930. Useful Drugs. Chicago: American Medical Associ-
ation.
Holmes P. 1995. Aromatherapy: applications for clinical practice. Alternative Medicine.
1(3) 177-182.
Kline R, Kline J, Di Palma J et al. 2001. Enteric coated pH dependent peppermint oil
capsules for the treatment of irritable bowel syndrome in children. Journal of Pedi-
atrics. 138: 125-128.
New Webster’s Dictionary, Thesaurus, and Medical Dictionary. 1992. New York: Otten-
heimer.
Niederau C, Opfert E. 1999. The effect of chelidonium and turmeric root extract on up-
per abdominal pain due to functional disorders of the biliary system. Results from a
placebo-controlled, double-blind study. Medizinische Klinik. 94(8) 425-430.
Ofuji K, Hara H, Sukamoto T et al. 1998. Effects of antidiarrheal containing an extract
from geranium herb on astringent action and short-circuit current actions across jeju-
nal mucosa. Nippon Yakurigaku Zasshi. 111(4) 265-246.
Olleveant N, Humphris F, Roe B. 1999. How big is a drop? A volumetric assay of essen-
tial oils. Journal of Clinical Nursing. 8(3) 299-304.
Schnaubelt K. 1998. Medical Aromatherapy. Berkeley, CA: Frog, 223.
Weiner J. 1994. Forecasting the effects of health reform on US physician workforce re-
quirements. Journal of the American Medical Association. 272:222-230.
144 Section I Overview

W
145
8
Manual Therapies
And I realized that all the world wants to be held in spite of it all.
Jack Kornfield
After the Ecstasy, the Laundry
H
IPPOCRATES DESCRIBED the importance of touch in the 5th century BC
and declared it his favorite of all health essentials. Aromatherapy is al-
ready being used in many manual therapies. This chapter is to encour-
age therapists to use it in a clinical way. The chapter has been divided into three
sections: massage therapy, chiropractic, and the “m” technique. These three sec-
tions have been subdivided into common ailments as examples of how aro-
matherapy could be used in each of these modalities.
Touch is a basic need. In times of crisis the need becomes overwhelming.
One of the most moving images of September 11, 2001 was of two firefighters
holding each other. Scores of massage therapists in New York and Maryland (and
many others from across the nation) rushed to the devastated areas. They worked
around the clock to treat rescue crewmembers who were stretched to their phys-
ical and emotional limits (Schwanz 2001). They treated emotionally traumatized
workers, many of whom had never had a massage (Pasquale 2001). Their com-
passionate and much-needed gift was huge, and the impact of touch was there for
the whole world to see.
Massage Therapy
In Florida, the definition of massage therapy was officially changed from manipu-
lation of superficial tissue to manipulation of soft tissue by Governor Jeb Bush on
July 19, 2001 (McGillicuddy 2001). Massage therapy has grown in acceptance dra-

matically throughout the last 10 years and is now the norm at sports events
worldwide, including the Olympics (Swantz 2001). In a recent survey, 17% of
Americans said they had received a massage in the past year. Thirty-five percent
of those were for medical reasons and 25% for stress relief and relaxation
(Schwanz 2001). Forty-two percent of Americans feel massage is a complemen-
tary therapy rather than just a beauty treatment, and medical practitioners ranked
massage therapy as the highest (74%) in terms of effectiveness over eleven other
modalities, including acupuncture (Anonymous 2001). Consumers spend $4 to
$6 billion annually on massage therapy. At Boeing and Reebok, headaches, back
strain, and fatigue have declined substantially since both companies began offer-
ing massage therapy to employees (Underwood 1998). Education requirements
for a massage-therapy license vary from state to state. Texas requires 250 hours
plus 50 intern hours, Oregon requires 330 classroom hours, and Nebraska re-
quires 1000 classroom hours. These figures were accurate in 1997 when only 22
states required licensing. Recently, New York and Washington states increased the
number of hours required for licensing to 1000 hours.
The physical effects of massage have been well documented throughout the last
10 years. Much of massage’s new-found respectability began in 1986 with Tiffany
Field, PhD, who found preterm babies who received massage therapy slept better,
took more milk, gained weight, and could leave hospital earlier, at a savings of thou-
sands of dollars per day, than their nonmassaged counterparts. She also found mas-
sage reduced depression (Field et al 1996) and enhanced wound healing (Field et al
1998). Research has also indicated massage enhances immune function (Harrison et
al 1992), reduces perception of pain (Nixon et al), and enhances sleep (Menehan
1997; Richards 1998). Massage, once a traditional component of nursing in the
1940s, is now returning to nursing (Mower 1997) with the beginning of the National
Association of Nurse Massage Therapists. Many massage therapists are interested in
adding aromatherapy as an enhancement to their profession (Enteen 2001).
In the state of Washington, insurance reimbursement covers whiplash injury,
provided the claim is filed within 3 years. This is often covered under personal in-
jury protection, which is usually part of vehicle insurance. The value is between
$10,000 and $20,000. As part of this coverage, massage therapy will be covered for
8 weeks, when necessary. Treatment can be biweekly and may be extended at the
discretion of the therapist. A payment of $85 is allowed per treatment, and if hy-
drotherapy (hot packs) is also used, a further $15 is allowed. The patient is reim-
bursed directly by the insurance company. Hypertension and osteoarthritis are also
conditions eligible for health-insurance reimbursement for massage therapy costs.
Fibromyalgia Syndrome
Fibromyalgia syndrome (FMS) is the most common cause of pain seen by medical
practitioners (Bennett 1995) and affects 3 to 6 million Americans, 73%-88% of
which are female and 92%-100% of which are Caucasian (Muir 1999). The symp-
toms are widespread pain for more than 3 months with at least 11 of 18 specific
146 Section I Overview

points painful to palpation. There appear to be two different types of fibromyalgia—
one involving myofascial pain and one more akin to chronic fatigue syndrome—
although both may appear in the same patient, and there is controversy as to
whether both are the same thing (Buchwald & Garrity 1994). Some patients with
chronic fatigue syndrome have been wrongly diagnosed. In one study of 68 pa-
tients with chronic fatigue, 68% had been wrongly given a psychiatric label in the
past (Deale & Wessley 2000).
There are many theories about FMS. Serotonin, a neurotransmitter in the
central nervous system that carries signals between nerve cells and interacts with
many other receptors such as dopamine, controls slow-wave sleep, and affects per-
ception of pain, is significantly lower in those with FMS (Muir 1999). On the
other hand, levels of substance P, the chemical necessary for transmission of pain,
are three times higher (Russell 1994). Certain studies indicate fibromyalgia may
be the result of a deficiency of relaxin, a neuropeptide with hemodynamic actions
(Geddes & Summerlee 1995). Relaxin is produced by the corpus luteum in the
ovary and until recently was thought to be involved only with labor (Alexander
2000). Other studies question the possibility of FMS being caused by a disorder
of the limbic system or exposure to a virus (Mountz & Bradley 1995).
FMS patients also complain of insomnia, depression, fatigue, and frequent fluid
retention in the morning. Whatever the cause, aromatherapy can help either by af-
fecting the limbic system, alleviating muscle fatigue or other specific symptoms, or
fighting a viral infection. For a more in-depth discussion on symptoms please con-
sult Chapters 5, 9, and 12 on psychology, viral infection, and pain, respectively.
Maija Grace (2001) reports on a controlled, crossover study of 20 patients us-
ing Fibromix, a commercial blend of nine essential oils diluted in carrier oil (see
Table 8-1 for details). Fibromix has been marketed in Finland for 3 years and was
Chapter 8 Manual Therapies 147
Table 8-1 h Essential Oils in Fibromix
Common Name Botanical Name
Ylang ylang Cananga odorata
Roman chamomile Chamomelum nobile
Neroli Citrus aurantium
Bergamot Citrus bergamia
Melissa Melissa officinalis
Black pepper Pipe nigrum
Ravansara Ravansara aromatica
Sandalwood Santalum album
Ginger Zingiber officinalis

formulated by the Maija Grace. The study was so successful in reducing FMS
symptoms that a second study followed with 14 women comparing Fibromix with
Chamomelum nobile (Roman chamomile) essential oil. The average age of the test
subjects was 52 years. Treatments consisted of weekly massage sessions for 6 to 8
weeks. One of the drawbacks to using just one essential oil was that patients and
therapists tired of it. However, sleep, pain, and stress all appeared to be positively
affected.
Lofgren (1998) investigated the use of antiviral essential oils (see Table 8-2
for details) for FMS using a single-case-study design. The study lasted 3 months
and included two treatments a week, producing 19 massage-therapy sessions.
Pain, sleep, and energy were measured using a visual analog (0-10). Although the
pain did not appear to change, the patient commented she had less pain in the
morning and improved mobility. She also said the cycles of pain were shortened
to hours instead of days. She also commented she no longer bruised so easily.
Lucas (1997) investigated the effects of a lemongrass, ginger, rosemary, and
Roman chamomile mix on three patients with FMS. Treatment was weekly mas-
sage with aromatherapy and daily baths with aromatherapy. The first patient (59
years old) was diagnosed with FMS 2 years previously, although she believed the
symptoms had been present for many years before that. She believed her pain was
helped by the treatments, but it was difficult to assess whether the daily bath or
the aromatherapy caused the improvement. The second patient (73 years old) had
also been diagnosed with FMS 2 years earlier. She had previously tried massage
but found “it didn’t help.” She found the baths not helpful (her bathtub was small
and uncomfortable, which may have been the cause), but the massage with es-
sential oils did seem to help a bit. The third patient (43 years old) had recently
been diagnosed with FMS. She was taking Klonopin regularly to sleep and said
massage usually helped her symptoms. She stopped taking the baths and used the
inhaled essential oils at night instead. The essential oils helped her sleep, and she
stopped taking sleep medication. Lucas used the “m” technique on this patient in-
stead of massage, as the patient requested something very gentle.
Hester (1999) used four essential oils in a jojoba carrier oil (see Table 8-3 for
details) for her study on four women who had each been diagnosed with FMS for
6 to 10 years. She measured pain perception, sleep, fatigue, and foggy thinking us-
ing a visual analog (0-10) for each condition throughout 4 weeks. Baseline mea-
148 Section I Overview
Table 8-2 h Essential-Oil Mix Used by Lofgren (1998)
Common Name Botanical Name Drops per Ounce Carrier Oil
Bergamot Citrus bergamia 5
Palma rosa Cymbopogon martini 9
Tea tree Melaleuca alternifolia 3
Ravensara Ravensara aromatica 3

surements were taken before the study. Two people had 80% improvement in
pain; two had 50% improvement. Clearer thinking received the lowest score with
an average of 35% improvement. Fatigue was improved by an average of 62.5%;
sleep was improved by an average of 72.5%. While these figures are encouraging,
the patients may have been biased to please the therapist!
Chiropractic
Chiropractic is growing exponentially—faster than massage, acupuncture, or
herbal medicine (Kessler et al 2001). The importance of massage was emphasized
at the 2001 Florida Chiropractic Convention where 150 massage therapists min-
gled with 1800 chiropractors and discussion topics included myofascial release
and neuromuscular therapy (Solien-Wolfe & McGillicuddy 2001). Many chiro-
practors either employ or actively refer patients to licensed massage therapists.
Many use massage techniques themselves to warm up the body prior to manipu-
lation. While some physicians still claim that they do not know for sure if chiro-
practic does more good than harm (Ernst 1998), the public is voting with its feet.
Stano and Smith (1996) studied 6183 patients via 2 years of insurance data and
found chiropractors were given higher satisfaction and quality ratings from pa-
tients than were medical practitioners, and they had lower costs as the initial-
contact provider. Shekelle et al (1995) found chiropractors were the primary-care
providers for 40% of back pain and had more patient visits than orthopedic physi-
cians did but at less cost.
Low-Back Pain
Eighty percent of adults suffer at least one episode of low-back pain in their lives
(Bigos et al 1994). Among patients who use alternative medicine, back problems
are the most frequently reported medical condition (Eisenberg et al 1993). In the
workforce, the cost of an average back-injury claim in 1989 was $8000 and ac-
counted for one third of worker’s compensation costs (Webster & Snook 1994).
The estimated national bill for the care of low-back pain per year is $38-$50 bil-
lion (Atlas & Deyo 2001). Seventy-five to 90% of patients with low-back pain re-
port improvement within 1 month, but 50% of patients have repeat episodes
Chapter 8 Manual Therapies 149
Table 8-3 h Essential Oils Used by Hester (1990)
Common Name Botanical Name Percentage
Lemongrass Cymbopogon citratus 3%
German chamomile Matricaria recutita 1%
Lavandin Lavandula intermedia 2%
Rosemary Rosmarinus officinalis 2%

within 1 year (Carey et al 1999). Since 1999, four major, randomized, controlled
studies and one metaanalysis have indicated massage is beneficial for low-back
pain (Crownfield 2001). A 2001 study involving 263 patients (Cherkin et al
2001) found those receiving massage needed less medication and fewer days in
bed than those receiving acupuncture.
Essential oils can be used by chiropractors to reduce muscle spasm before
manipulation, to reduce inflammation, and to reduce pain. Costa (1997), a mas-
sage therapist who works with a chiropractor, conducted a small study on the
use of aromatherapy prior to chiropractic manipulation. She used 3% Lavan-
dula angustifolia in vegetable oil massaged into the backs of six patients for 20
minutes prior to manipulation. The chiropractor assessed the ease of manipula-
tion on a scale of 1-10, with 10 being the easiest to manipulate. The members
of the experimental group were aged 16-49 and included both men and women.
Twelve treatments were given to each of the six patients. Figures indicate the
lavender massage had made manipulation easier than plain massage. Further es-
sential oils were tested, and aromatherapy is currently used by the chiropractor’s
office.
Although efficacy can be achieved with 1-5% essential oil solutions, some ther-
apists use up to 40% concentrations. Do not dilute the essential oil in a
petroleum- or mineral-based medium as this will prevent it from being absorbed
through the skin. There are specific analgesic, antiinflammatory, and antispasmodic
essential oils that can help low-back pain. The oils need to be applied topically.
Commonly used and effective antiinflammatory essential oils for acute low-
back pain are listed in Table 8-4 and include an essential oil that has a long his-
tory of use in Australia but is just becoming known in the United States (Webb
2000). Table 8-5 lists essential oils with analgesic qualities suitable for treating
low-back pain.
In a survey on management of rheumatic-disease symptoms in aromatherapy
practices in the United Kingdom, 55% therapists said they had patients referred
to them by conventional medicine (Osborn et al 2001). Musculoskeletal com-
plaints were the second most common condition treated by aromatherapists in
the United Kingdom, after stress. Aromatherapy in the United Kingdom is nearly
always used with massage.
Zivitz (2000) carried out a small pilot study on six women with low-back
pain. The subjects’ ages ranged between 24 and 73 years. Zivitz compared the ef-
fects of Boswellia carteri (frankincense) and Cymbopogon citratus (lemongrass) in
two separate 4% solutions, each diluted with sweet-almond oil. The control group
received a massage with plain vegetable oil. Each participant had experienced
low-back pain for a minimum of 2
1
⁄
2
years. A visual analog was used to rate pain
(0-10). Participants completed the pain scale immediately before treatment, im-
mediately after treatment, and 1 and 2 hours later. Despite favorable comments
from the participants, data analysis did not show any alteration in pain perception
beyond the control group (who received straight carrier oil with their massage),
although everyone enjoyed the aroma.
150 Section I Overview

Soltis (2000) compared the effects of Piper nigrum (black pepper) and Orig-
anum majorana (sweet marjoram) on patients with low-back pain. Again the sam-
ple was small, six participants. There were four women and two men. This time
each essential oil (2%) was self-applied twice a day for 1 week. Most participants
thought the black pepper was warming and this helped the pain, although two
participants did not like the aroma. Most participants believed sweet marjoram
helped, and one stopped taking Motrin for pain relief. However, there were many
Chapter 8 Manual Therapies 151
Table 8-4 h Antiinflammatory Essential Oils for Acute Low-Back Pain
Common Name Botanical Name Reference
Juniper Juniperus communis Mascolo et al 1987
Fennel (sweet) Foeniculum vulgare Mascolo et al 1987
Coriander Coriandrum sativum Mascolo et al 1987
Roman chamomile Anthemis nobilis Rossi et al 1988
Nutmeg Myristica fragrans Benet et al 1988
Everlasting Helicrysum italicum Franchomme & Penoel 1991
Yarrow Achillea millefolium Middleton & Drzewiecki 1984
German chamomile Matricaria recutita Tubaro et al 1984
Australian blue cypress Callitris intratropica Webb 2001
Lemongrass Cymbopogon citratus Seth et al 1975
Clove Syzygium aromaticum Guillleman et al 1989
Lavender Lavandula angustifolia Ghelardini et al 1999
Table 8-5 h Analgesic Essential Oils for Acute Low-Back Pain
Common name Botanical name Reference
Peppermint Mentha piperita Krall & Krause 1993
Lemongrass Cymbopogon citratus Viana et al 2000
Lavender Lavandula angustifolia Ghelardini et al 1999
Not known Artemesia caerulescens Moran et al 1989
Myrrh Commiphora molmol Dolara et al 2000
Spike lavender Lavandula latifolia Von Frohilche 1968
Clary sage Salvia sclarea Moretti 1997

variables, and it is difficult to come to any conclusion with such a small number
of participants.
Port (1999) conducted a small, controlled study on the effects of lavender and
black pepper on osteoarthritis. Participants were seven women and one man. All
participants used analgesics and antiinflammatory medication, and several took
them daily. The participants were randomly allocated to two groups. The experi-
mental group received 20 ml of 3% black pepper and lavender oils in sweet al-
mond oil. The control group received 20 ml of plain carrier oil. Both groups were
instructed to rub the mixture into the painful joint once in the morning and once
at night for 7 days. At the end of this time they were to stop the treatment and
evaluate their pain and stiffness using a visual analog (0-10).
The control group did not have any measurable effect from this process. The
experimental group did experience a reduction in stiffness and pain. One woman
stopped taking her antiinflammatory medicine, but when the study was finished
her stiffness and pain returned, and she started taking her medicine again. Two
participants had significant improvement in their range of motion. One person
was able to make a fist for the first time in years. This is a very small study but is
encouraging to those of us who are getting older!
The “M”Technique
The “m” technique is a registered method of touch suitable for the very fragile or
when massage is inappropriate (either because the receiver is too fragile or be-
cause the giver is not trained in massage). The “m” technique is a series of stroking
movements performed in a set sequence. Each movement, identified with a
mnemonic name (a name that acts as a “hook” to enable the giver to remember
it), is repeated a set number of times. Because the technique is structured in terms
of strokes, sequence, number, and pressure, it is completely reproducible and
therefore useful in research. The “m” is so gentle and soothing that a physician has
called it “physical hypnotherapy” (Merrill 1999).
The “m” first arrived in the United States in 1994 when I began teaching in
Florida and Georgia. The “m” technique was registered by the United States
Patent and Trademark Office in March 1998. Since 1994, the technique has been
taught in universities, nursing colleges, and massage schools across America. Stu-
dents have even created a new verb and talk about “m”-ing their patients! Cur-
rently more than 1000 people have learned the “m” technique, and the word is
spreading. The “m” was devised as a simple, easy to learn method of touch (one
weekend) that would allow a patient to feel relaxed as quickly as possible. Created
initially for nurses not wanting to train in massage but wanting to touch their pa-
tients, the “m” technique is used by many other licensed health professionals.
The “m” technique is quite different from massage as it follows a set structure
that never changes. Each movement and sequence is done in a distinctive pattern
that is not modified. Each stroke within each movement is repeated three times,
so a group of practitioners carrying out the technique would all be doing exactly
152 Section I Overview

the same stroke at the same time. The rationale for this set form of repetition is
simple: to build confidence and remove anxiety in the receiver. The first time pa-
tients experience an “m”-technique stroke, they will pay attention. The second
time they feel the same stroke, they will recognize it. By the third time, the re-
ceiver knows what is going to happen and will begin to relax. By experiencing
each stroke a set number of times, the receiver learns what is going to happen and
is lulled into a deep state of relaxation in a very short period of time. The “m”
technique also uses a set pressure. If pressure was measured on a scale of 0-10,
with 0 as no pressure and 10 as crushing pressure, the “m” technique ‘s pressure
should always be a 3. Conventional massage alters the pressure depending on the
situation.
Many massage therapists are learning this technique to use in their practice
alongside conventional massage therapy. Sharon Gibson, a massage therapist in
New Jersey, says normally 65% of her clients go to sleep on the table during a
massage. However, with the “m” technique, 100% fall asleep within the first 10
minutes. Lori Mitchell, a critical care nurse in Kalispell, Montana, used the “m”
technique in critical care and said it brought rapid and prolonged relaxation to her
patients, some of whom had not responded to orthodox sedation. Aurora
Ocampo, RN, a clinical nurse specialist at Beth Israel Hospital in New York City
uses the “m” technique to relax patients prior to surgery.
In 1996 the “m” technique was used in the research laboratory at Columbia
Presbyterian Medical Center in New York City. The “m” technique was applied
to the feet of medical students and a measurable effect on their parasympathetic
nervous systems was recorded using an 8-lead electrocardiogram machine at-
tached to a heart-variation monitor. Slater (2001) measured the effects of the “m”
technique in a study on muscle tension, relaxation, and mood with 14 partici-
pants. Slater compared the effect of the “m” technique applied with and without
lavender essential oil. Data were entered into a database program and analyzed
using a two-sample t-test, assuming equal variances. The effects of the “m” tech-
nique were statistically significant without the lavender (p⫽⬍0.005). However,
with lavendar, the effects were increased substantially (p⫽⬍0.00004). Limita-
tions of the study were lack of randomization, small study size, and dominance of
female participants.
Miller (2000), a critical care nurse at Desert Samaritan Hospital in Mesa,
Arizona, used the “m” technique on her patients. The first was a female patient
with a history of multiple sclerosis who was ventilator dependent and very appre-
hensive about her caregiver. Postoperatively (tracheostomy) the patient was
pulling on the ventilator tubing constantly and complaining of discomfort. The
“m” was used on her legs and feet. She fell asleep before the treatment was com-
pleted (less than 10 minutes) and slept for 2 hours. She was much calmer upon
awakening. A second patient was a 37-year-old female with cancer metastasized
to the bones and now affecting her brain. Diagnosed 4 years previously, she had
been treated with chemotherapy and radiation. She was ventilator dependent. She
wanted to stay alert so she could “say good bye to her family in a dignified way.”
Chapter 8 Manual Therapies 153

She chose rosemary essential oil to accompany her “m” technique, as she remem-
bered using it before. The “m” was used on her feet and legs. Her need for nar-
cotics decreased from every 2 hours to every 6 hours. Four of those hours she was
asleep. The third patient was a 72-year-old female who just had abdominal
surgery. She was very fragile, weak, and afraid. Pain medication was given every
2 hours. After the “m” to her hands, the patient slept for 3 hours and did not re-
quest any further pain medication for 2 more hours. The fourth patient was a 76-
year-old male who just had abdominal surgery. He rated his pain as a 7. After the
“m” to his feet, he belched and passed flatulence, which greatly relieved his pain.
He slept without analgesics and later rated his pain as a 1 or 2. The following day
he was still thanking Miller for using the “m” technique on him. Miller noted that
as well as physical responses of facial expressions in her patients, often there was
a significant drop in heart rate of 5-10 beats per minute.
The “m” is simple enough for a 5-year-old child to do and can be shared with
family members. It is empowering for the giver and beneficial for the receiver.
The chaplain of Mercy Hospice in Scranton, Pennsylvania, learned the “m” tech-
nique to “give physical comfort at a soul level.” A hand or foot “m” takes only 5
minutes and has far-reaching effects. I have found teaching the “m” technique to
be one of the most satisfying aspects of my career. Details of training programs
and an instructional video can be found at www.rjbuckle.com.
REFERENCES
Alexander M. 2000. How Aromatherapy Works, Vol 1. Odessa, FL : Whole Spectrum.
Anonymous. 2001. Post Legislative Mandate: two-thirds of group health clinician re-
spondents view CAM as effective. Integrator for the Business of Alternative Medi-
cine. (April).
Atlas S, Deyo R. 2001. Evaluating and managing acute low back pain in the primary
care setting. Journal of General Internal Medicine. 16, 120-131.
Benet A, Stamford F, Tavares I. 1988. The biological activity of eugenol, a major con-
stituent of nutmeg: studies on prostaglandins, the intestine and other tissues. Phy-
totherapy Research. 2, 125-129.
Bennett R. 1995. Fibromyalgia: the commonest cause of widespread pain. Alternative &
Complementary Therapies. 21(6) 269-275.
Bigos S, Bowyer O, Braen G et al. 1994. Acute low back pain in adults. In Clinical Prac-
tice Guidelines, No 14. Rockville, MD: Agency for Healthcare Policy and Research,
US Dept of Health & Human Services, available www.spinehealth.com.
Buchwald D, Garrity D. 1994. Comparison of patients with chronic fatigue syndrome,
fibromyalgia and chemical sensitivities. Archives of Internal Medicine. 154,
2049-2053.
Carey T, Garrett J, Jackman A et al. 1999. Recurrence and care seeking after acute back
pain: results of a long-term follow-up study. Medical Care. 37, 157-164.
Cherkin D, Eisenberg D, Sherman K et al. 2001. Trial comparing Chinese medical
acupuncture, therapeutic massage, and self care. Archives of Internal Medicine 161(8)
1081-1088.
154 Section I Overview

Costa D. 1997. Lavender eases chiropractic manipulation. Unpublished dissertation,
Hunter, New York: RJ Buckle Associates.
Crownfield P. 2001. Massage for back pain: let’s look at the research. Massage Today.
1(9) 1, 16-17.
Deale A, Wessley S. 2000. Diagnosis of psychiatric disorder in clinical evaluation of
chronic fatigue syndrome. Journal of the Royal Society of Medicine. 93, 310-312.
Dolara P, Luceri C, Ghelardi C et al. 2000. Analgesic effect of myrrh. Nature. 376, 29.
Eisenberg D, Kessler R, Foster C et al. 1993. Unconventional medicine in the United
States. New England Journal of Medicine. 328, 246-252.
Enteen S. 2001. Inside aromatherapy: how to recognize and offer high-quality aro-
matherapy. Massage Today. 1(7) 1, 8, 11.
Ernst E. 1998. Chiropractic for low back pain. British Medical Journal. 317:160-160.
Field T, Grizzle N, Scafidi F et al. 1996. Massage and relaxation therapy effects on de-
pressed adolescent mothers. Adolescence. 31, 903-911.
Field T, Peck M, Krugman S et al. 1998. Burn injuries benefit from massage therapy.
Journal of Burn Care & Rehabilitation. 19, 241-244.
Franchomme P, Penoel D. 1991. Aromatherapie Exactement. Limoges, France: Jollois.
Geddes B, Summerlee A. 1995. The emerging concept of relaxin as a centrally acting pep-
tide hormone with hemodynamic action. Journal of Neuroendocrinology. 7:511-517.
Ghelardini C, Galeotti N, Salvatore G et al. 1999. Local anesthetic activity of essential
oil of Lavandula angustifolia. Planta Medica. 65(8) 700-703.
Guillemain J, Rouseeau A, Delaveau P. 1989. Effects neurodepresseurs de l’huile
essentielle de Lavandula angustifolia. Annales Pharmaceutiques Francaises
47:337-343.
Harrison L, Groer M, Modricin-McCarthy M et al. 1992. Effect of gentle human touch
on pre-term infants. Research in Nursing and Health 23:435-446.
Hester G. 1990. The effects of aromatherapy for the treatment of fibromyalgia. Unpub-
lished dissertation, Hunter, New York, RJ Buckle Associates.
Jakovlev V, Isaac O, Thiemer K et al. 1979. Pharmacological investigations with com-
pounds of chamomile. II. New investigations on the antiphlogistic effects of a bis-
abolol and bisabolol oxide. Planta Medica. 35, 125-140.
Kessler R, Davies R, Foster D et al. 2001. Long-term trends in the use of complemen-
tary and alternative medical therapies in the USA. Annals of Internal Medicine. 135,
262-268.
Khanna T, Zaidi FA. 1993. CNS and analgesic studies on Nigella sativa. Fitoterapia.
64(5) 407-410.
Kornfield J. 2000. After the Ecstasy, the Laundry. London: Rider, 223.
Krall B, Krause W. 1993. Efficacy and tolerance of Mentha arvensis aethoeroleum. Paper
presented at 24th International Symposium on Essential Oils. Berlin, July 21-24,
1993, Germany.
Lofgren J. 1998. Aromatherapy and fibromyalgia: an antiviral approach. Unpublished
dissertation, Hunter, New York, RJ Buckle Associates.
Lucas M. 1997. Fibromyalgia and essential oils. Unpublished dissertation, Hunter, New
York, RJ Buckle Associates.
Maija Grace U. 2001. Treating fibromyalgia syndrome with essential oils. International
Journal of Aromatherapy. 11(1) 20-25.
Mascolo N, Autore G, Capasso F. 1987. Biological screening of Italian medicinal plants
for anti-inflammatory activity. Phytotherapy Research. 1(1) 28-31.
Chapter 8 Manual Therapies 155

McGillicuddy M. 2001.New legislation expands definition of massage. Massage Today.
1(8) 1, 8.
Menehan K. 1997. Massage laws nationwide. Massage Magazine. Sept/Oct 67 125.
Merrell W. 1999. Personal communication.
Middleton E, Drzewiecki G. 1984. Flavanoid inhibition of human basophil histamine
release stimulated by various agents. Biochemical Pharmacology. 33, 3333-3338.
Moran A, Martin N, Montero MJ. 1989. Analgesic, antipyretic and anti-inflammatory
activity of essential oil of Artemisia caerulescens subsp. gallica. Journal of Ethnopharma-
cology. 27(3) 307-317.
Moretti M, Peana A. 1997. A study on the anti-inflammatory and peripheral analgesic
action of salvia sclarea oil and its main components. J Essent Oil Research. 9:199-204.
Mountz J, Bradley L. 1995. Fibromyalgia in women. Arthritis & Rheumatism. 38(7)
926-938.
Mower M. 1997. Massage returns to nursing. Massage Magazine. Sept/Oct 67. 47-50.
Muir M. 1999. Fibromyalgia syndrome. Alternative & Complementary Therapies. 5(2)
79-84.
Nixon M, Teschendorff J, Finney J et al. Expanding the nursing repertoire: the effect of
massage on post-operative pain. Australian Journal of Advanced Nursing. 14(3)
21-26.
Osborn C, Barlas P, Baxter G et al. 2001. Aromatherapy: a survey of current practice in
the management of rheumatic disease symptoms. Complementary Therapies in Medi-
cine. 9:62-67.
Pasquale S. 2001. Bringing relief to the World Trade Center rescue workers. Massage
Today. 1(11) 1.
Port M. 1999. Lavender and black pepper for osteoarthritis. Unpublished disseration,
Hunter, New York: RJ Buckle Associates.
Richards K. 1998. Effects of back massage and relaxation intervention on sleep in criti-
cally ill patients. American Journal of Critical Care. 7, 288-299.
Rossi T, Melegari M et al. 1988. Sedative, anti-inflammatory and anti-diuretic effects in-
duced in rats by essential oils of varieties of Anthemis nobilis: a comparative study.
Pharmacological Research Communications. 20(Suppl.) 71-74.
Russell I. 1994. Biochemical abnormalities in fibromyalgia syndrome. Journal of Muscu-
loskeletal Pain. 2(3) 101-115.
Schwanz M. 2001. MERT (Massage Emergency Response Team) aids relief of Pentagon
rescue workers. Hands On. 17(6) 1,6.
Seth G, Kolate C, Varma K. 1975. Effect of essential oils of Cymbopogon citratus on cen-
tral nervous system. Indian Journal of Experimental Biology. 14(3) 370-373.
Shekelle P, Markovich M, Louie R. 1995. Comparing the costs between provider types
of episodes of back pain care. Spine. 20(2) 221-226.
Slater V. 2001. The effects of the “m” technique with and without Lavandula angustifolia.
Unpublished dissertation, Hunter, New York, RJ Buckle Associates.
Slater V. 2001. The “m” technique. Unpublished dissertation, Hunter, New York: RJ
Buckle Associates.
Solien-Wolfe L, McGillicuddy M. 2001. Massage therapy makes presence felt at Florida
Chiropractic Association’s national convention. 1(10) 1, 17.
Soltis K. 2000. Black pepper and sweet marjoram for low back pain. Unpublished disser-
tation, Hunter, New York: RJ Buckle Associates.
156 Section I Overview

Stano M, Smith M. 1996. Chiropractic and medical costs of low back care. Medical
Care. 34(3) 191-134.
Swantz S. 2001. Massage at the 2002 Winter Olympics. Massage Today. 1(11) 1.
Tubaro A, Zillia C, Redaeli C et al. 1984. Evaluation of anti-inflammatory activity of
chamomile extract topical application. Planta Medica. 50(4) 359-360.
Underwood A. 1998. The magic of touch. Newsweek. April 6. 71-72.
Viana G, Vale T, Pinho R et al. 2000. Antinociceptive effect of the essential oil from
Cymbopogon citratus in mice. Journal of Ethnopharmacology. 70, 323-327.
Von Frohilche A. 1968. A review of clinical, pharmacological and bacteriological re-
search into Oleum spicae. Wiener Medizinische Wochenschrift. 15:345-350.
Webb M. 2001. Australian essential oils profile: Blue cypress. Aromatherapy Today.
19:37-39.
Webster B, Snook S. 1994. The cost of 1989 compensation low back pain claims. Spine.
19, 1111-1116.
Zivitz E. 2000. Do the essential oils of frankincense and lemongrass alter perceptions of
back pain? Unpublished dissertation, Hunter, New York, RJ, Buckle Associates.
Chapter 8 Manual Therapies 157

e
section
II
Clinical Use
of Aromatherapy

General Clinical Subsection
Chapter 9 Infection
Chapter 10 Insomnia
Chapter 11 Nausea and vomiting
Chapter 12 Pain and inflammation
Chapter 13 Stress management
Part B Specialized Departments Subsection
Chapter 14 Cardiology
Chapter 15 Care of the Elderly
Chapter 16 Critical Care
Chapter 17 Dermatology
Chapter 18 Endocrinology
Chapter 19 Hospice/End of life care
Chapter 20 Immunology
Chapter 21 Obstetrics and Gynecology
Chapter 22 Oncology
Chapter 23 Pediatrics
Chapter 24 Psychiatry
Chapter 25 Respiratory Care
Introduction to Section 2
Aromatherapy is certainly viewed by many as being primarily concerned with
stress management. This may be the case today, but it would be a pity if the myr-
iad other therapeutic properties of essential oils were ignored now and in the fu-
ture. This section of the book is an exploration of how aromatherapy could be
used clinically, and is divided into two subsections: a general section and a spe-
cialized section.
In the general clinical section, I have focused on the broad-ranging problems
of infection, insomnia, nausea and vomiting, pain, and stress management. The
first four of these areas have far-reaching effects on the quality and cost of health-
care, and are of interest to a wide range of readers. While the role of aromather-
apy in stress management has been covered by other authors, I have attempted to
place the role of stress management within a clinical context.
The ability of Western medicine to contain the increasing demands of
healthcare users is reaching a breaking point. Essential oils might provide a little
more elasticity because essential oils are much cheaper than conventional medi-
cines. Just compare the use of peppermint with Zofran in the treatment of nau-
sea. While there may be many incidences when Zofran is needed and the only
drug that will work, there are also many instances when peppermint will work and

it could be offered first. So it is in the interest of healthcare providers to be con-
versant regarding what essential oils could achieve in a clinical setting.
The chapter on infection was an exciting one for me to write, as I feel there is
tremendous potential for essential oil to be used against emerging drug-resistant
pathogens. In vitro and animal studies indicating antimicrobial activity do not
prove that essential oils will necessarily be effective in a human, but such studies
are an encouraging beginning, particularly when the power of synthetic antibi-
otics is waning.
The specialized subsection focuses on a handful of specific problems within
each clinical specialty and how aromatherapy might help those problems, again
with reference to published research, my clinical experience, and case studies and
small pilot studies. The aim in writing Chapters 14–25 is to make licensed
healthcare professionals (LHP) aware of the clinical potential of aromatherapy
within specific departments. References have been given where possible although
many of them are in-vitro or animal studies. But at least it is a beginning. Where
the studies have been on whole herbs rather than essential oils, this fact is indi-
cated. There is a separate treatment of the oral use of essential oils back in Chap-
ter 7. This specialized, updated clinical section includes new chapters on
OB/GYN and psychiatric care. The chapter on immunology has been much ex-
panded and the number of references to this section has been doubled.
Obviously there will be some overlap among chapters, and the reader is ad-
vised to refer to the general index at the back of the book to find other areas in
the book where the symptom will be addressed.
I am grateful for the input of many reviewers in this section whose help and
advice was most appreciated. The reviewers include: Ann Adams BSN, Ben
Evans MSN, Claire Everson BSN, Diana Guthrie RN, PhD, Susan Hageness
MSN, Dorathy Larkin RN, PhD, Lori Mitchell BSN, Gayle Newsham PhD,
Mary Poolos RN, PhD, Ganson Purcell MD, Scottie Purol-Hershey RN, PhD,
Linda Scaz RN, PhD, Neil Schultz MD, Kay Soltis MSN, Brenda Talley RN,
PhD, and Mark Warner, MD.
Section II Clinical Use of Aromatherapy 161

W
162
9
Infection
The use of perfumes, and especially that of lavender, is a more certain and pleasant
means of combating diseases and hindering the spread of epidemics.
Rene-Maurice Gattefosse (1948)
Hospital-Acquired Infections
Infectious diseases were, until recently, the most common cause of death (Mac-
Sween & Whaley 1992). Despite an improvement in living conditions among the
technically advanced countries of the world, infections such as the common cold
and influenza are major causes of working days lost. Smallpox may have been ir-
radicated and the incidence of diphtheria greatly reduced, but viral infections and
mutated or newly discovered bacteria are on the increase. Since September 11,
2001, anthrax and other bacteria that could be potential biological weapons have
gained publicity. Three essential oils, palma rosa, basil, and black cumin, are mod-
erately effective in vitro against anthrax. However, aromatic medicine has been for
the most part ignored as a possibility for combating the pathogen. Tuberculosis
(TB) is also on the increase and will infect 8.4 million people this year and kill 2
million (Reichman & Tanne 2001). Several essential oils are effective against TB
in vitro and others augment the effect of conventional medicines.
Animals are also falling prey to new infections or infestations. Of wild hon-
eybees, 90% have been killed following an infestation of mites. The mites, which
had become resistant to conventional pesticides, were thought to have been
brought into the United States with illegally imported bees several years ago. Bob
Noel, a farmer in Cumberland, Maryland, tried fighting the mites using winter-
green essential oil mixed with shortening and sugar placed directly in the hive. It
killed all the mites but did not harm the bees. Peppermint, lavender, pennyroyal,

spearmint, and patchouli were also successful in killing mites, and the results were
posted on the Internet (Amrine 1996).
However, of greatest concern to all health professionals are the infections ac-
quired by patients as a direct result of being in a hospital (Ward 1993). Infection
is caused by organisms such as bacteria, viruses, fungi, protozoa, and parasites.
Gascoigne (1993), a British physician, suggests these organisms can be spread by
the methods listed in Table 9-1.
Being a hospital patient brings with it the threat of infection (Fig. 9-1).
Every year almost 2 million American patients acquire an infection in a hospital,
and of those 2 million patients, 80,000 die (Fisher 1994). Urinary-tract infections
increased the duration of hospitalization by 5.1 days. Rubinstein et al (1982)
found wound infections increased the period of hospitalization by 12.9 days, a
heavy price for a hospital budget.
Chapter 9 Infection 163
Table 9-1 h Spread of Infections
Spread by: Results in:
Droplet infection Common cold, influenza
Implantation Streptococcus, Staphylococcus
Direct contact Scabies, sexually transmitted diseases
Food or water contamination Cholera, Listeria
Injection, human or insect HIV virus, hepatitis, yellow fever, malaria
Lower respiratory tract
22.9%
Urinary tract
23.2%
Surgical wound
10.7%
Skin
9.6%
Septicaemia
6.2%
Gastrointestinal
4.9%
Other
22.5%
Figure 9-1 The frequency of different types of hospital-acquired infection. From Wilson
J. 2001. Infection Control in Clinical Practice, 2nd ed. London: Elsevier Science.

The most common hospital-acquired infections (HAI) are Campylobacter en-
teritis, Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA),
and vancomycin-resistant enterococci. HAI (nosocomial) can be acquired from
an outside source, such as poor hygiene standards of the hospital staff, equipment,
or even visitors, or as a result of self-infection. Sometimes infection can be due to
the enforced relocation of a commensal. A commensal is a bacterium symbiotic
to the health of the host, such as Escherichia coli in the gut. However, when the
commensal is transplanted to another part of the body, an infection ensues. A
common example is E. coli, which, when transported from the gut to the urinary
tract, causes cystitis.
Common Forms of Hospital-Acquired Infection
Campylobacter enteritis
According to Sleigh et al (1992), C. enteritis causes one of the most common
forms of infective diarrhea. This form of diarrhea is caused by organisms that af-
fect the digestive tract, many of which have not yet been identified or are totally
new.
Pseudomonas aeruginosa
P. aeruginosa has become more common in hospitals. A strictly aerobic, gram-
negative bacillus, P. aeruginosa flourishes in water and aqueous solutions. The or-
ganism produces a pigment called pyocyanin, as well as fluorescein, and these
compounds together create the characteristic blue, offensive pus seen in P. aerug-
inosa infections (MacSween & Whaley 1992). Pseudomonas is rapidly becoming
resistant to antibiotics. Nearly 70% of people with cystic fibrosis are chronically
infected with this bacterium.
Methicillin-Resistant Staphylococcus aureus
MRSA has been responsible for global outbreaks of infection. Staphylococcus
infections tend to remain localized, possibly because of the production of coagu-
lase, which clots fibronogen (MacSween & Whaley 1992). Some essential oils
such as peppermint, thyme, lavender, tea tree, and juniper have been found effec-
tive against MRSA in vitro (Nelson 1997). Hospital-acquired S. aureus bac-
teremia continues to be a frequent and serious complication of hospitalization
worldwide ( Jensen et al 1999).
Multiple-Resistant Serratia marcescens and Klebsiella
Serratia marcescens and Klebsiella were the cause of an epidemic involving four
hospitals in the 1970s. The spread of infection was finally linked to the lack of
hand washing by personnel who worked in all four hospitals. By the time the in-
fection was brought under control, 400 patients had been infected, and 17 pa-
tients had died (Fisher 1994).
S. marcescens is a gram-negative bacillus that occurs naturally in soil and wa-
ter and produces a red pigment at room temperature. It is associated with urinary
164 Section II Clinical Use of Aromatherapy

and respiratory infections, endocarditis, osteomyelitis, septicemia, wound infec-
tions, eye infections, and meningitis. Transmission is by direct contact. Droplets
of S. marcescens have been found growing on catheters and in supposedly sterile
solutions. Most strains are resistant to several antibiotics. Between 1951 and 1952
the US Army conducted a study called Operation Sea-Spray to study wind-
currents that might carry biological weapons. They filled balloons with S.
marcescens and burst them over San Francisco. Shortly afterwards, doctors noted
a dramatic increase in pneumonia and urinary-tract infections (www.sunysccc.
edu/academic/mst/microbes/23smarc.htm). Recently the Azerbaijan Medical
Association announced on their Web site (http://azma.org) that S. marascens was
killed in 30 minutes in vitro by essential oil of Nepata transcaucasica (an aromatic
herb that grows wild in the Absheron region of Azerbaijan).
Streptococcus
Group A Streptococcus (GAS) is a bacterium found in the throat and on the
skin. Many people carry it with no symptoms. Most GAS infections are mild,
such as strep throat and impetigo. However, life-threatening GAS infections can
occur when the bacterium gets into a part of the body where it is not normally
found, resulting in necrotising fasciitis (flesh-eating bacteria) and strep toxic
shock syndrome. Of patients with necrotising fasciitis, 20% die; more than 50%
of patients with strep toxic shock die. Approximately 10% to 15% of patients with
other forms of invasive GAS infections die. In 1999, there were 9400 cases of in-
vasive GAS in the United States. According to the Centers for Disease Control
and Prevention, people with chronic illnesses, those taking steriods, or those
who have low immune function are most at risk for this type infection (www.
cdc.gov/ncidod/dbmd/diseaseinfo/groupastreptococcal_g.htm).
Vancomycin-resistant enteroccoci
Vancomycin-resistant enteroccoci (VRE) were first isolated in 1987. In some
hospitals, VRE are responsible for 20% of enteroccoccal infections (Leclercq et al
1988). VRE are directly related to the dramatic increase in vancomycin use in hos-
pitals in the early 1980s and 1990s (Ena et al 1993). A metaanalysis of 420 pub-
lished reports and 98 conference reports confirms this view (Carmeli et al 1999).
Each of the bacteria mentioned previously are becoming more common in
hospitals, but there is a whole range of pathogenic organisms that surround us
every day. These common causes of HAI can be resistant to orthodox medication.
However, in-vitro studies suggest these pathogens are sensitive to the antibacter-
ial action of specific essential oils. Pathologists who are experts in the use of es-
sential oils as antibacterial agents stress that the “terrain” of the patient can affect
the efficacy of the antibacterial action of an essential oil, and an individual aro-
matogram is required. However, the standard aromatograms described here give a
general idea as to which essential oils might be efficacious in a particular patient.
Following a brief classification of bacteria, there is a description of some the
published research into the antimicrobial effects of essential oils. This research
Chapter 9 Infection 165

suggests essential oils could be used to enhance antibacterial/antifungal/antiviral
drug therapy or to treat infections on their own.
Bacterial Classification
Although the following information may seem elementary, it may be helpful to
have the basics reiterated to provide context for the information on essential oils.
Bacteria are first classified according to their shape (Fig. 9-2). The two main
groups of bacteria are cocci and bacilli (Hope et al 1993). These two groups are
then subdivided into gram-positive and gram-negative bacteria. (Gram was the
microbiologist who devised the staining method.) Gram staining uses a mixture
of violet dye and iodine to stain the magnesium ribonucleate found in some bac-
teria deep purple. The purple stain cannot be washed out by alcohol. Bacteria that
can be stained purple are said to be gram-positive. Bacteria that do not contain
magnesium ribonucleate do not retain the purple stain and are described as gram-
negative (Ward 1993). Mycobacterium (the cause of TB and leprosy) is not re-
vealed by the gram-stain method and instead is stained with an acid-fast method
166 Section II Clinical Use of Aromatherapy
Figure 9-2 Four main groups of bacteria: Clockwise from top left: Gram-positive cocci,
gram-negative cocci, gram-negative bacilli (rods), gram-positive bacilli.
From Wilson J.
2001. Infection Control in Clinical Practice, 2nd ed. London: Elsevier Science.

called the Ziehl-Nielsen method (MacSsween & Whaley 1992). A second sub-
division of bacteria is between aerobic organisms, which need air to survive, and
anaerobic organisms, which do not require air. An increasingly common anaero-
bic bacterium causes vaginitis. In optimum in vitro conditions, bacteria divide ap-
proximately every 20 minutes (MacSween & Whaley 1992).
Coccus Bacteria
The cocci bacteria include Staphylococcus, named for the Greek word staphyl,
meaning grapes, because, seen under a microscope, the bacteria have this charac-
teristic shape. Staphylococcus is the cause of many skin infections. Streptococcus is
named after the Greek word streptos, meaning twisted, because the bacteria re-
semble twisted chains. Streptococcus often causes throat infections. Other members
of the coccus family include Pneumococcus, which causes pneumonia, and Neisse-
ria, which causes gonorrhea. Streptococcus can be further classified into A, B, or
nonhaemolytic types and aerobic or anaerobic types.
Bacillus Bacteria
The bacillius group includes Enterobacteriaceae such as E. coli and Salmonella,
both of which can cause diarrhea. It also includes Proteus mirabilis and Bacillus
anthracis, which cause proteus and anthrax, respectively. Other bacteria in the
bacillus group include Corynebacterium diphtheriae, which causes diphtheria,
Pseudomonas aeruginosa, and M. tuberculosis, which causes TB. Anaerobic bacilli
include Clostridium tetani, which causes tetanus, and C. difficile, which causes
pseudomembranous colitis.
In addition to the two main groups, there are the spirochete group and a fur-
ther group of organisms that are neither viruses nor bacteria, but something in be-
tween. This group includes Rickettsia, which causes typhus fever, and Chlamydia
trachomatis, which causes genitourinary infections (Hope et al 1993). A classifi-
cation of pathogens is shown in Fig. 9-3.
Antibiotics
The antibiotics industry has seen huge growth in the last 30 years, with sales in-
creasing from $94 million in 1971 to $8 billion in 1994 (Fisher 1994). Antibiotics
(which, roughly translated, means “against life”) are secondary metabolites of mi-
croorganisms and, at high dilutions, are inhibitory to most other microorganisms.
An antibiotic is capable of inhibiting the growth of a microorganism or destroy-
ing it (Tamm 1971). It does this by inhibiting the synthesis of the bacteria’s cell
wall, protein or nucleic acid production, or by reducing the permeability of the cy-
toplasmic membrane. This prevents the bacteria from reproducing so rapidly and
enables the host to work toward eliminating the organism (Lewis & Lewis 1977).
Although many antibiotics are synthetic, most are derived from natural sub-
stances. The most commonly used type is a broad-spectrum antibiotic that is
nonselective. Laboratory testing of a swab or blood sample indicates which
Chapter 9 Infection 167

168 Section II Clinical Use of Aromatherapy
LIFE
Animals Viruses
Vertebrates Invertebrates
Helminths Arthropods,
e.g., scabies,
lice
Eukaryotes
(⬎1 chromosome; intracellular
double-membraned structures)
Prokaryotes
(1 chromosome;
no nuclear membrane;
no mitochondria)
Plants Protists
Others
Nematodes Cestodes Trematodes
Fungi
(non-photosynthetic;
rigid polysaccharide wall)
Protozoa
(motile;
unicellular;
non-photosynthetic)
Bacteria Rickettsiae Chlamydiae
Flagellate
(motile; flagellae)
e.g.,
Trypanosoma,
Trichomonas,
Giardia, Leishmania
Amoeboid
e.g.,
Entamoeba
histolytica,
Cryptosporidium
Sporozoa
(non-motile)
e.g.,
Plasmodium,
Toxoplasma
Figure 9-3 Classification of pathogens. From Hope R, Longmore J, Hodgetts T et al. 1993. Oxford Handbook of Clinical Medicine. Oxford, UK: Ox-
ford University Press, p. 172.

antibiotic is appropriate, but this method of testing has largely been abandoned
in favor of broad-spectrum antibiotics, mainly because of cost and time, but also
because physicians are under intense pressure to prescribe immediately. Broad-
spectrum antibiotics do not always succeed in killing the bacterium causing the
disease. Despite this, broad-spectrum antibiotics remain very popular and are
usually the first line of defense. Broad-spectrum antibiotics usually destroy almost
every other “friendly” gut bacterium as well. As a result, a great many people now
support colonies of fungi that have taken the place of the friendly digestive bac-
teria. Candidiasis, the existence of which was once denied by the medical profes-
sion, is thriving in the gut of millions of people who have taken broad-spectrum
antibiotics and have not replaced their friendly bowel flora.
The majority of antibiotics are (or have been until recently) active against
gram-positive microorganisms (such as Staphylococcus and Streptococcus). Although
manmade antibiotics are becoming increasingly sophisticated in an attempt to
compete with organisms that can mutate and thereby initiate resistant colonies,
they are not as complicated as most essential oils. Essential oils have 100 or more
components, so it is arguable that an organism would find it more difficult to be-
come resistant to them. Without a doubt, synthetic antibiotics have saved lives
and will continue to do so. However, the overuse and improper use of antibiotics
during the last few years has led to a growing population of antibiotic-resistant
bacteria (Fisher 1994).
Penicillin, the first antibiotic, was found to be effective against Staphylococcus but
completely ineffective against E. coli. As early as 1942, Fleming (who discovered
penicillin) was advising the medical profession of the possibility that Staphylococcus
could become resistant to penicillin. Today, 95% of Staphylococcus is resistant to peni-
cillin. Antibiotics are also listed in the group of drugs most frequently associated with
adverse reactions such as nausea and gastrointestinal problems, skin rashes, and
headaches (Blaschke & Bjornsson 1995). In addition, antibiotics are thought to be
linked to an increase in food allergies and to chronic fatigue syndrome (Schmidt
1995). Some bacteria can be killed within a few hours with direct exposure to sun-
light, and most are killed at 100° C (the boiling point of water). However, some bac-
teria are notoriously difficult to eradicate, especially in a person with a compromised
immune system. Fig. 9-4 shows how many bacilli and cocci have become resistant to
antibiotics, resulting in the development of the so-called “superbugs.”
Resistance to Antibiotics
Some strains of bacteria have become resistant to antibiotics for various possible
reasons, such as the following:
1. Patients have not completed the prescribed course of antibiotics. This means
the bacteria are not completely eradicated and become immune to the next
dose of that particular antibiotic.
2. Antibiotics have been prescribed for viral illness such as the common cold. In
the United States, some 900,000 prescriptions per year are written for antibi-
otics to treat the common cold (Fisher 1994).
Chapter 9 Infection 169

170 Section II Clinical Use of Aromatherapy
Key: 1 ⫽ susceptible, first choice; 2 ⫽ susceptible, second choice; R ⫽ resistance likely to be a problem; 0 ⫽ usually inappropriate
Penicillin V/G
Flucloxacillin
Amp/Amoxycillin
Carbenicillin/Ticarcillin
Piperacillin/Azlocillin
Cephradine/Cephalothin/Cefazolin
Cefuroxime/Cephamandole/Cefotaxime
Ceftazidime
Imipenem
Erythromycin
Lincomycin/Clindamycin
Tetracyclines
Chloramphenicol
Trimethoprim
Aminoglycosides
Vancomycin
Metronidazole
Ciprofloxacin
Staphylococcus aureus
(penicillin sensitive) 1 0 0 0020022RR2RRR22R2
Staphylococcus aureus
(penicillin resistant) R 1 R R R 20022RR2RRR2R2R2
Streptococcus
(group A) 1 0 0 0020022RRRRRR 0RR
Streptococcus pneumoniae
102 0022022RR2RRRR0RR
Enterococcus faecalis
RR1 R2RRR2 0RRRRR2RRR
Neisseria meningitidis
102 00020200R2RRRR0
Listeria monocytogenes
201 00RRR2RR02020R0
Haemophilus influenzae
R R 1R 0 R R 2 0 2 R R 2R R R 0 R R 2
E. coli
RR1RRRR2RR2RRRR1R2RRR2
Klebsiella
species R R R R R R 2R 2R 2 RRRR1R2RRR2
Serratia/Enterobacter
species R R R R R R 2R 2R 2 RRRR1R2RRR2
Proteus
species R R 1R R R R 2R R 2 RRRR1R2RRR2
Pseudomonas aeruginosa
RRR1R1RRR2R2RRRRR1RRR2
Bacteroides fragilis
RR2RRRRRR2R22R2RRRR1R
Other
Bacteroides
species R R R RRRRR2R2R2R2RRRR1R
Figure 9-4 Susceptibility of selected bacteria to certain antibacterial drugs. From: Hope R, Longmore J, Hodgetts T et al. 1993. Oxford Handbook
of Clinical Medicine. Oxford, UK: Oxford University Press, p. 176.

3. Antibiotics have been used prophylactically. In the United States, until 1992,
a 48-hour course of antibiotics was given preoperatively to patients thought to
be at risk for infection.
4. During the past 40 years, the antibiotics penicillin and tetracycline have been
added to animal feed.
5. Antibiotics are regularly used by the food industry to protect fruits and veg-
etables and are also used in the fish industry.
Over-prescription of antibiotics has been widespread. In 1991, 240 million
prescriptions for antibiotics were written in the United States, one for every per-
son in the country (Fisher 1994). This dropped to 110 million prescriptions for
antibiotics in 1995, but 50% of these are thought to be inappropriate for the dis-
ease being treated (Schmidt 1995).
Antibiotics are given to animals to increase growth: in some cases chickens
fed with a broth of antibiotics have grown to three times larger than normal
( Jukes 1973). Although only minute amounts of antibiotics produce this growth,
animals destined for human consumption regularly contain antibiotics, leading to
a potential immunity or resistance in humans to those antibiotics. This immunity
first manifested itself with an outbreak of Salmonella in England in 1965. Nor-
mally, Salmonella would have been swiftly brought under control with antibiotics.
However, on this occasion, investigations showed that the bacterium was resistant
and six people died (Corpet 1987).
Following this outbreak, the Swann Committee (composed of microbiolo-
gists and physicians) led an intensive enquiry. Their recommendation was a ban
on the use of antibiotics used in human medicine for promoting animal growth.
Although England, Scandinavia, the Netherlands, and most European countries
agreed to the ban, the US government never approved the ban and still allows
farmers to use the same antibiotics employed in human medicine as growth stim-
ulants for animals (Fisher 1994).
In fact, shortly after penicillin was discovered, researchers found some strains
of Staphylococcus could manufacture an enzyme called penicillinase, which ren-
dered penicillin inactive (Abraham & Chaine 1940). This resistant strain spread
through hospitals, and by 1955 80% of patients infected with Staphylococcus died
if penicillin was the only antibiotic used to combat the infection (Fisher 1994).
Methicillin and cephalosporin were introduced in the 1960s in an effort to
control penicillin-resistant Staphylococcus. They appeared to be effective, but then
gram-negative bacteria such as Serratia and Klebsiella began to show resistance to
these new drugs. Another antibiotic, gentamycin, appeared on the market and
seemed to have the situation under control until Staphylococcus reappeared, this
time more resistant than before, the first MRSA. The pharmaceutical business re-
grouped and produced a new antibiotic, ciprofloxacin (Cipro), but MRSA quickly
became immune. By 1980, MRSA was resistant to everything except vancomycin.
Vancomycin had been held back, not only because it was toxic, but because it was
feared that if MRSA became resistant to it there would be nothing else to throw
at the bacterium. These fears became reality in the late 1980s when hospitals
Chapter 9 Infection 171

began to report vancomycin-resistant infections. Today, a growing number of
pathogens are becoming resistant to conventional antibiotics.
Resistant bacteria are still often treated with cephalosporin, an antibiotic de-
rived from a fungus. Cephalosporin was discovered by Giuseppe Brotzu, a bacte-
riologist from Cagliari in Sardinia (Fisher 1994). The disadvantages of the
cephalosporin group of antibiotics are the hypersensitivity they cause in more
than 10% of patients and their adverse effects on blood-clotting mechanisms
(Hope et al 1993).
Many sexually transmitted diseases, including gonorrhea and chlamydia, now
are multiple-drug resistant. Shigella, the cause of many fecal-contaminated gastric
upsets, is multiple resistant, as are many respiratory infections. Chowdhury
(1998) carried out studies on monkeys infected with mutiple-resistant Shigella
flexneri and found oral doses of black cumin (Nigella sativa) essential oil (1 to 3
ml diluted in soybean oil) were very effective. The experimental group of mon-
keys became entirely free of infection within 2 days, whereas the control group
was still infected after 6 days. According to a Web site dedicated to black cumin
(www.nigella-sativa.com), the essential oil is made from the plant’s seed and was
found in Tutankhamen’s tomb. The essential oil contains 46.8% p-cymene and
21% carvone. In addition, cumin seed essential oil was found to be effective against
E. coli, Staphylococcus aureus, and Streptococcus faecalis ( Jain & Purohit 1992).
Essential Oils as Potential Antibacterial Agents
Essential oils are not just pleasant aromas. Many have specific antibiotic, antivi-
ral, and antifungal properties and have been classified accordingly (Natural Med-
icines Comprehensive Database 2002). The responsibility for prescribing an an-
tibiotic usually lies with a physician or nurse practitioner. For many other health
professionals, antibiotic prescription is outside their boundaries or scope of prac-
tice and is inappropriate. However, the use of an essential oil to reduce stress
caused by an infection is acceptable. What is needed is a more detailed look at es-
sential oils’ antibacterial properties. Can they be used to enhance orthodox med-
icine? Can they be used when antibiotics are ineffective? In a world where
pathogens are mutating faster than synthetic medicines can be created to kill
them, essential oils might have a very beneficial role to play. They may even turn
out to be the antibiotics of the future.
There is a long history of essential oils being used against pestilence. A large
number of perfumers and glovemakers appeared to survive the Black Death in Eu-
rope. This could be because glovemakers were licensed to impregnate their wares
with essential oils and because perfumes were made of essential oils. Deinenger
(1995) cites Schweistheimer, who wrote that the English town of Bucklesbury was
spared from the plague—at the time Bucklesbury was the center of the lavender
trade. Lavender has antibacterial properties and has recently been found effective
against MRSA. Nostradamus was supposed to have successfully treated the plague
with pills of crushed roses placed under the tongues of plague victims. Rose
172 Section II Clinical Use of Aromatherapy

contains l-citronellol, geraniol, nerol, linalol, and phenylethyl alcohol (Guenther
1952). Alcohols are thought to be strong antiinfection agents with antiviral prop-
erties (Franchomme & Penoel), so the actions of Nostradamus seem to be logical.
Approximately 58% of all isolated antibiotics are produced from Streptomyces,
a bacterium. Another 9% are derived from other bacteria, 19% from fungi,
lichens, and mosses, and 14% from higher plants. Lewis writes that “the total 909
antibiotics known in 1967 represent only a fraction of those found in nature. Not
a single one, used therapeutically, is from the higher plants, even though these
possess the largest single group of antibiotics for which there is no known use”
(Lewis & Elvin-Lewis 1977). Tamm (1971) reported on ansamycins, a group of
antibiotics characterized by an aliphatic bridge linking two nonadjacent positions
found in an aromatic nucleus.
Some of the plants known to have antibiotic properties include yellow cy-
press, wild ginger, golden seal, poplar tree, turnip, wallflower, hops, cabbage, sweet
clover, common bean, cashew, black walnut, potato, corn, and garlic. Each has
been tested against bacteria, fungi, viruses, or protozoa and found to be effective
in vitro (Lewis & Elvin-Lewis 1977). Valnet (1990) suggests if essential oils were
used to treat pathogens, the surrounding tissue would not be adversely affected.
Conventional medicines can sometimes destroy the surrounding tissue along with
the infection, because antibiotics typically kill bacteria by puncturing their cell
walls, which allows toxins to spill out (Service 1994).
In the case of burns, in which the breakdown of tissue causes the body to re-
absorb pathogenic toxins, Valnet (1990) suggests the use of essential oils could be
a suitable or alternative method of treatment, because many essential oils have
tissue-protecting properties that prevent putrefaction. However, essential oils
with a high phenol content can cause dermal irritation and should not be used
to treat burns. Please see Chapter 3 for more information about phenols and
phenol-rich essential oils.
Research on the Antibacterial Properties
of Essential Oils
The primary effect of essential oils on bacteria and viruses appears to be on the
cell membrane (Harris & Harris 1995) where they seem to alter the osmotic reg-
ulatory function (Savino et al 1984). Fifty years ago antibiotic researchers were
investigating possible plant alternatives. The Second National Symposium on
Recent Advances in Antibiotic Research was held in Washington in 1945, under
the auspices of the National Institutes of Health. During the proceedings, the ef-
fects of lupulon, a lipid-soluble, antibiotic-like substance prepared from hops
(Humulus lupulus) were discussed. Chin et al (1949) found lupulon inhibited the
growth of Staphylococcus aureus, Mycobacterium phlei, and Mycobacterium tuberculo-
sis in vitro at concentrations of 1.56, 5.0, and 25 g/mL, respectively. Combining
lupulon with a 2% solution of sodium chloride increased the antibiotic activity.
Hops produce an essential oil (Budavari 1996).
Chapter 9 Infection 173

Maruzella and Sicurella (1960) reported on the antibacterial activity of 133
essential oils in vitro. These were tested against six pathogens, namely E. coli,
Staphylococcus aureus, B. subtilis, Streptococcus faecalis, Salmonella typhosa, and My-
cobacterium avium. Of the essential oils tested, 71% were shown to be effective
against M. avium, 19% against B. subtilis, 14% against Staphylococcus aureus, 12%
against Streptococcus faecalis, and 6% against E. coli. Among the most effective es-
sential oils were lemongrass, oregano, savory, red thyme, and cinnamon. This re-
search was conducted just 2 years after an earlier paper (Maruzella & Percival
1958) investigated the antimicrobial activity of perfume oils.
Deans and Svoboda (1987) found that marjoram (Oregano majorana) was ef-
fective against Pseudomonas aeruginosa, Salmonella pullorum, and Yersinia enteroco-
litica in vitro at a concentration of 1:10 in absolute ethanol. All three organisms
are of significance in public health. Essential oils of black pepper (Piper nigrum),
geranium (Pelargonium graveolens), nutmeg (Myristica fragrans), oregano (Orig-
anum vulgare), and thyme (Thymus vulgaris) were tested against 25 different gen-
era of bacteria, and each was found to exhibit considerable inhibitory effect
(Dorman & Deans 2000). Peana et al (1999) found sage (Salvia officinalis) and
clary sage (Salvia sclarea) effective against various bacteria including Staphylococ-
cus aureus, E. coli, and S. epidermidis.
P. aeruginosa appears to be less susceptible to tea tree than many bacteria, and
this tolerance is thought to be because of the bacteria’s outer membrane. How-
ever, the addition of polymyxin B nonapeptide (PMBN) to the essential oil ap-
pears to permeabilize the outer membrane, allowing tea tree to become effective
(Mann et al 2000). PMBN may also help other essential oils become effective
against P. aeruginosa.
Zakarya et al (1993) examined the antimicrobial activity of 21 essential oils
of eucalyptus. The effects of the volatile constituents of lemon gum (Eucalyptus
citriodora) were found to be the most effective against E. coli (gram-negative) and
B. megaterium and S. aureus (both gram-positive). Although, when the whole es-
sential oil was used, sugargum (Eucalyptus cladocalyx) was most effective. This
brings up the point, which has been paralleled in many other studies, that isolat-
ing the active, common constituents of essential oils will not produce the same ef-
fects as using the whole essential oil. It is interesting that E. globulus, E. smithi,
and E. radiata were not among the eucalyptus types selected for testing, as they
are regularly used in aromatherapy to treat infections (Penoel 1991/1992).
Ferdous et al (1992) studied the effect of black cumin (Nigella sativa) essen-
tial oil on the treatment of dysentery, and it was shown effective against several
multiple-drug-resistant organisms, such as Shigella, Vibrio cholera, and E. coli. The
activity of the oil was compared with that of ampicillin, tetracycline, cotrimoxa-
zole, gentamycin, and nalidixic acid and was active against all of the bacterial
strains tested, except for one strain of Shigella dysenteriae (strain 1548). Black
cumin is commonly known as Roman coriander, nutmeg flower or fennel flower,
although it is not in any way related to fennel. It actually belongs to the butter-
cup family. The French formerly used the seeds as a substitute for pepper, and in
174 Section II Clinical Use of Aromatherapy

India the seeds are commonly used in curries (Greive 1931). Lemon essential oil
(Citrus limon) was found to completely inhibit Vibrio cholera in a further study by
de Castillo et al (2000). Vibrio species also showed a high sensitivity to basil and
sage essential oils in a study by Koga et al (1999).
Helichrysum picardii, a member of the everlasting flower family, was shown to
be effective against gram-positive bacteria such as Staphylococcus aureus, Bacillus
subtilis, B. cereus, B. maegaterium, and gram-negative E. coli. Its antibacterial ac-
tivity was thought to be less potent than clove and thyme (de la Puerta et al
1993). Helichrysum is used as a tobacco flavorant.
Deans and Ritchie (1987) of the Department of Biochemical Sciences, at the
Scottish Agricultural College in Auchincruive, Scotland, tested the effect of 50 es-
sential oils against 25 genera of bacteria in vitro. Their research found that the most
effective essential oils were bay, cinnamon, clove, thyme, marjoram, pimento, gera-
nium, and lovage. One year later, Deans and Svoboda (1988) found French tarragon
(Artemesia dracunculus) to be effective against P. aeruginosa, S. aureus, S. faecalis, and
Yersinia enterocolitica. In this study, the whole oil was tested against several of the
main chemical constituents such as eugenol, limonene, linalol, menthol, cis-ocimene,
anisaldehyde, and ␣-pinene. This same study produced firm evidence that the con-
stituents of essential oils change, depending on the time of their harvesting. In this
instance, tarragon plants harvested midseason were the least potent of the tarragon
plants tested. That the constituents of tarragon essential oil alter according to the
time of harvesting is not new to aromatherapy, but this is one of the few studies that
actually demonstrates this. Also of interest is the way the physical configuration of
the molecule affected the essential oil (the difference between cis- and transisomers).
In tarragon, the cis configuration produced a more antimicrobial plant. Tarragon is
used as a flavor ingredient in many foods, as well as in alcoholic beverages and soft
drinks. It is also an important ingredient of bearnaise sauce. Several hybrids (man-
made cultivars) of lavender, sage, savory, and thyme were also tested against 25 bac-
teria in vitro. All four hybrids showed substantial antibiotic activity, but each was
most potent against specific bacteria. See Table 9-2 for details.
Chapter 9 Infection 175
Table 9-2 h Hybrids and Their Antibacterial Properties
General Common Name Bacteria Affected
Thymus thyme Moraxella spp., Clostridium sporogenes
Salvia sage Acinetobacter calcoacetica, Brevibacterium
linens, Clostridium sporogenes, Moraxella
spp.
Satureja savory Brevibacterium linens, Enterobacter aero-
genes, Klebsiella pneumonia, Moraxella spp.
Lavandula lavender Brevibacterium linens, Clostridium sporo-
genes, Moraxella spp, Staphylococcus aureus

In another paper Deans et al (1992) demonstrated the antibacterial proper-
ties of Oregano officinalis (a specially bred strain from Israel) and West Indian
lemongrass (Cymbopogon citratus). Other essential oils found to have antibacter-
ial activity were tarragon, basil, sage, thyme, and celery. Among the bacteria tested
were Salmonella pullorum, E. coli, Klebsiella pneumonia, P. aeruginosa, Staphylococ-
cus aureus, Streptococcus faecalis, and Proteus vulgaris. Deans and Svoboda (1989)
also found summer savory (Satureja hortensis) to be an effective antibacterial agent
against the previously mentioned organisms.
The antibacterial properties of lemongrass were the subject of a detailed in-
vestigation by Onawunmi and Ogunlana (1986). This particular lemongrass is
grown in Nigeria, where it is traditionally used for the treatment of rheumatism.
German chamomile (Matricaria recutita), renowned for its deep-blue color and
antiinflammatory properties, also has substantial antimicrobial activity, especially
against gram-positive bacteria such as Staphylococcus aureus and Streptococcus fae-
calis. The antibiotic component is thought to be ␣-bisabolol, which is more ac-
tive than chamazulene (Kedzia 1991).
Balacs (1993) reviewed the antibacterial properties of the plant family Lami-
acae, which includes rosemary (Rosmarinus officinalis), wild basil (Calamintha
nepeta), thyme (Thymus vulgaris), and savory (Satureja montana). The effective
chemical parts of these plants are thought to be carvacrol (in savory), ␣-pinene
and 1,8-cineole (in rosemary), thymol (in thyme), and pulegone and para-cymene
(in wild basil).
Benouda et al (1988) tested essential oils against hospital-pathogenic bacte-
ria. This study examined essential oils of armoise (Artemesia herba alba), oregano
(Thymus capitatus), and eucalyptus (Eucalyptus globulus) against Staphylococcus
aureus, Streptococcus C and D, Proteusspp., Klebsiella spp., Salmonella typhi, Haemo-
philus influenza, and P. aeruginosa and found that the three essential oils had an
action comparable to standard antibiotics. Thyme was the most effective essential
oil, although none of the oils were found to have any impact on Pseudomonas.
A review paper by Carson and Riley (1993) found that tea tree (Melaleuca al-
ternifolia) was an effective antibiotic against Staphylococcus, Streptococcus, and
many gram-negative bacteria, and they concluded that the full therapeutic po-
tential of tea tree had not yet been realized. In The Cowthron Report, Cooke and
Cooke (1994) found manuka (Leptospermum scoparium) and kanuka (Kunzea eri-
coides), New Zealand’s answer to tea tree, produced impressive results. This study
was supported by Maori funds and covered the effects of these two essential oils
against various bacteria and fungi. Manuka appeared to be very effective against
Staphylococcus aureus and ringworm. It was believed manuka could be a useful es-
sential oil in cases of MRSA infection, although the paper stated that no clinical
trials had been carried out.
An additional paper by Carson et al (1995) showed tea tree was effective
against MRSA. It was tested against 64 methicillin-resistant and 33 mupirocin-
resistant isolates of S. aureus and was found to be effective in all cases, using
dilutions of 0.25% and 0.50%. These results were duplicated in a UK study using
176 Section II Clinical Use of Aromatherapy

similar methods. The tea tree used in the UK study was chemotype terpineol
greater than 30%, and the cineole content (an oxide and harsher on the mucous
membrane) was less than 15%. Chan and Loudon (1998) carried out an in vitro
study on 28 isolates of MRSA and eight clinical isolates of coagulase-negative
staphylococci at Manchester Royal Infirmary in Manchester, England. The min-
imum inhibitory concentrations (MICs) were repeated three times and ranged
from 0.25% to 0.5% tea tree. No resistant isolates were found. Many cosmetic
products contain 2% to 5% tea tree. Carson found an added bonus; although tea
tree inhibited MRSA, it did not inhibit CNS and therefore preserves the skin
flora.
Human Studies
For skeptics who may argue the effective antimicrobial activity of an essential oil
in vitro does not guarantee a similar action in humans, Caelli et al (2001) carried
out a study on humans using 4% tea tree nasal ointment and 5% tea tree body
wash against a control of 2% mupirocin nasal ointment and triclosan body wash
on MRSA. The tea tree combination appeared to be better than the conventional
one. However, because of the small number of patient participants (n ⫽ 30) no
statistical significance could be drawn.
A study by Sherry et al (2001) indicates that essential oils can be effective in
humans and may be effective when nothing else works. The authors reported on
a chronic case of MRSA osteomyelitis. A 49-year-old man sustained an open
fracture to his left tibia. He underwent debridement and insertion of an in-
tramedullary nail. He underwent a free-flap procedure to the lower tibia 2 months
later to reposition the nail, and a femoral-popliteal bypass graft. Debridement of
the flap was done 8 months later. Debridement of an infective focus of the left
tibia was performed 15 months later. He subsequently developed chronic os-
teomyelitis (MRSA). Long-term antibiotic therapy (oral and intravenous) of 1 gr
flucloxacillin and 1 gr dicloxacillin every 6 hours had been unsuccessful. Ampu-
tation was being considered.
In December, 2000, via a 3-cm percutaneous incision, the lower tibia was
drilled and washed out with 4000 ml of saline. Then it was packed with calcium
sulfate pellets impregnated with lemongrass, eucalyptus, tea tree, clove, and
thyme essential oils in an ethanol base. A catheter was left in situ to allow deliv-
ery of further essential oils. One ml of antiseptic essential oil mixture was ad-
ministrated daily. The dilution and ratio of the essential oils was not given by the
authors. The wound healed and the culture was clear within 3 months. The symp-
toms resolved, and a plain x-ray examination showed resolution of the infective
process with incorporation of the bone graft. The authors commented that es-
sential oils have a strong antimicrobial action, are cheap, simple to use, and can
be used topically (Sherry et al 2001).
Many essential oils, at a dilution known to be safe, have also been shown ef-
fective against drug-resistant pathogens. In 1994, a workshop was given at the
Royal Society of Medicine in London, England, on aromatograms and the use of
Chapter 9 Infection 177

essential oils as antibacterial agents. Michael Smith, a London-based pathologist
who conducts aromatograms for several London hospitals, gave his analysis of the
antibacterial properties of several essential oils on MRSA. Every one tested was
effective. The essential oils included oregano, thymol (Thymus vulgaris CT3),
Moroccan chamommile (Ormenis mixta), Dutch mill lavendar (Lavandula x in-
termedia CT Super), Italian cypress (Cupressus sempervirens), peppermint (Mentha
piperita), ravensara (Ravensara aromatica), juniper (Juniperus communis), lemon,
palmarosa (Cymbopogon martini), eucalyptus, and gully gum (Eucalyptus smithi).
Most of these are essential oils that are commonly used for stress management
and are generally accepted as being safe. Many of them are used by health pro-
fessionals in the United States. The time is right to consider using essential oils
for all their properties.
My students have had some impressive case-study results using essential oil
compresses on wound infections and infected bedsores. Swabs to indicate infec-
tious pathogens were taken, and the relevant essential oil selected. One particu-
larly impressive case study was conducted by a nurse practitioner. A female pa-
tient had a chronically infected bedsore. This patient had been on systemic
antibiotics without effect. A wound swab showed the infection had been caused
by Clostridium. Searching through her notes, the nurse practitioner found a ref-
erence to a paper by Ross et al (1980). After she had discussed the safety and po-
tential efficacy of sweet marjoram (Origanum majorana) with the patient’s physi-
cian and had shown him the monograph, he gave his consent for her to use this
essential oil. The treatment was discussed with the patient and consent obtained.
A compress was applied directly to the infected site, using a 5% solution of
sweet marjoram. The compress was reapplied three times a day. Within 24 hours
there was a dramatic improvement, and within 5 days the wound was healed. In
other case studies, essential oils with antibacterial properties have been selected
without a swab being taken. Dilutions of up to 10% have been used. Not one case
has shown any negative side effect to date. In most instances, the infection has
healed very rapidly. For more information on wounds and protocols please see
Chapter 15 on care of the elderly.
Further research is required. Animal testing has already been done for po-
tential toxicity of essential oils; atoxicity studies on human tissue have indicated
a safe level at which essential oils can be used. What is needed now is a series of
controlled trials to explore the antimicrobial efficacy of essential oils in humans.
As Peter Mansfield, MD, (1996) writes, “Science is really a method for answer-
ing questions. If we ask stupid questions, scientific methods will faithfully pro-
duce for us a stupid answer.” It is not stupid to ask questions relating to aro-
matherapy and stress, but it is perhaps stupid not to ask questions about
aromatherapy and infection. Just because these oils are natural does not mean
they are not powerful. Norman Farnsworth, Director of Pharmacognosy at the
University of Illinois College of Pharmacy is quoted as saying,: “There is not a
dime’s bit of difference between chemicals in plants and synthetics” (Sears 1995).
178 Section II Clinical Use of Aromatherapy

The Aromatogram
Just like synthetic antibiotics, many essential oils are effective against particular
pathogens. The skill lies in knowing which essential oil to use for which infection.
Conventional medicine regularly takes wound or throat swabs, or urine or blood
samples to cultivate and identify a pathogen.
Gattefosse used exactly the same principle of this process, which is called an
antibiogram, in France and renamed it an aromatogram. The only difference in
the procedure is with an aromatogram an essential oil is added to the Petri dish
instead of an antibiotic. A hypothetical example of an aromatogram is shown in
Fig. 9-5.
The Petri dish is lined with a culture medium such as agar-agar. A culture
broth of the pathogen is spread across the plate. Several small paper circles, each
impregnated with different essential oil, are placed on the agar-agar, and the Petri
dish is incubated for 24 hours. If the essential oil is the correct antidote, an area
of inhibition occurs in a circle around the impregnated paper. Sometimes an es-
sential oil not effective on its own is effective when it is close to a second essen-
tial oil. Sometimes two essential oils together give a large area of inhibition but
individually produce no area of inhibition. Aromatograms are used in France and
England and could be of great use in the United States. So far I have been unable
Chapter 9 Infection 179
Figure 9-5 Hypothetical example of an aromatogram. Six different essential oils, here
identified only by number, are being tested against one bacterial culture from the body of
a patient. The shaded area in each square is known as the “area of inhibition” and shows
how effective each oil is against the bacteria. In this case essential oils 3 and 5 would be
used to treat the patient.
From Tisserand R. 1988. Aromatherapy for Everyone. Har-
mondsworth, UK: Penguin Books.

to find a laboratory in the United States prepared to conduct an aromatogram,
but this is obviously the way of the future. Belaiche (1979), a French doctor, has
created many tables illustrating the specific uses of essential oils against specific
bacteria and their effects.
In England, Deans and Ritchie (1987) used the aromatogram technique in a
comprehensive and impressive study that examined 25 genera of bacteria and 50
essential oils. This kind of sensitivity testing for essential oils in the treatment of
bacterial infections is being carried out by several London hospitals, and there is
active campaigning to increase the understanding of how aromatograms work
(Blackwell & Smith 1995). It is hoped that this scientific method of selecting es-
sential oils in sensitivity testing will become more widespread as it becomes bet-
ter understood. However, a new microdilution method using the redox dye Re-
sazurin has also been developed for determining the MIC of an essential oil
(Mann & Markham 1998). This method overcomes the problem of adequate
contact between an essential oil and the test bacteria and obviates the need for a
chemical emulsifier.
Blackwell and Smith (1995) and Valnet (1990) both emphasize that standard
organisms do not respond in exactly the same way as a host organism. Even though
a pathogen is known and named, it may not respond in an identical way; the host
must be taken into consideration. To illustrate this, Valnet writes that a colibacillus
in one patient may respond to the essential oil of pine, whereas in another patient
it may respond to the essential oil of lavender or thyme. This is quite different from
the Western approach in which everyone is given the same antibiotic (usually
broad-spectrum). However, the selection of essential oils for testing via an aro-
matogram is based on the antibacterial properties reported in the literature.
Viruses
A virus is different than any other pathogen because it is a coiled strand of nu-
cleic acid protected by a protein coat, which can only survive and reproduce in-
side a host cell (Roberts 1986). Because viruses are so small, their biology was not
understood for many years until electron microscopy revealed what they looked
like. Many biologists still do not classify them as living organisms in their own
right but only when they are inside a host cell. There are basically two types of
virus: those that attack bacteria and those that attack the cells of other living or-
ganisms, such as animals and humans. The basic structure of a virus is illustrated
in Fig. 9-6.
Viruses are classified as either DNA viruses or RNA viruses. The DNA
viruses are subdivided into single-strand and double-strand viruses. RNA viruses
also occur as single or double strands, with retroviruses, such as AIDS, in the
single-strand group. A retrovirus contains an enzyme called reverse transcriptase
that allows the RNA in the virus to be reverse-transcribed into DNA. Drugs such
as zidovudine (AZT) and zalcitabine (HIVID) are designed to inhibit production
of reverse transcriptase. Resistance acquired by viruses during antiviral therapy
180 Section II Clinical Use of Aromatherapy

has been well documented and usually occurs when the virus mutates (MacSween
& Whaley 1992).
Viruses that cause glandular fever, hepatitis, influenza, warts, the common
cold, mumps, and measles are well known; less common is the rabies virus. More
recent viruses are herpes and Lassa fever. Of these viruses, only smallpox has been
eradicated through immunization. A compulsory immunization program in the
West has controlled mumps and measles, although they remain potential killers
in developing countries. Patients with immune deficiency (or dysfunction), both
primary and secondary, are more vulnerable to infections of any kind than persons
with intact immune systems.
Synthetic Antivirals
Geoffrey Carr (1996) of The Economist wrote, “No viral epidemic has ever been
stopped by drugs.” Synthetic viricides are difficult to manufacture, and none of
Chapter 9 Infection 181
Naked icosahedral
(e.g., poliovirus)
KEY:
Spikes (glycoprotein)
Envelope (protein and lipids)
Proteins making up
the capsid
Nucleic acid
Enveloped icosahedral
(e.g., herpesvirus)
Enveloped helical
(e.g., influenza virus)
Figure 9-6 Structure of viruses. From Ackerman B, Dunk-Richards G. 1991. Microbiology:
An Introduction for the Health Sciences. Australia: WB Saunders.
them appear to be totally effective to date. Most have moderate to severe side ef-
fects. They work in one of three ways: through immunological control, through
stimulation of the natural resistance mechanism of the host, or through
chemotherapy. One of the most successful, AZT, stops the phosphate linkage
from being formed. This means the virus cannot manufacture DNA (Craig &
Stitzel 1994). Other synthetic antivirals include acyclovir (Zovirax), famcyclovir
(Famvir), Vidarabine (Vira-A), and rimantadine (Flumadine).
Highly active antiretrovial therapy (HAART) is a powerful weapon that has
greatly affected the AIDS epidemic—an epidemic that may well turn out to be
more devastating than the plague itself. AIDS/HIV has killed three times more
Americans than the Vietnam war (Sullivan 1995). Unfortunately HAART drugs
also have potent side effects and it is difficult for patients to completely adhere to
the treatment regimen.
Antiviral Properties of Essential Oils
Many plants and their aqueous extracts have been tested for antiviral activity. In-
terestingly, when the essential oil from the plant is used, it too seems to have an
antiviral effect, although the essential oil has a different chemistry than the aque-
ous extract. Therefore a good pointer is to study the published research on the
aqueous extracts.
An investigation supported by the National Institutes of Health showed an
aqueous extract of lemon balm (Melissa officinalis) had antiviral properties
(Kucera & Herrmann 1967). The aqueous extract was tested on embryonic eggs
and in tissue culture infected with Semliki forest (a mouse brain disease), New-
castle disease, vaccinia, and herpes simplex. The results showed lemon balm pro-
tected the embryonic eggs against the lethal action of all viruses tested. It is
thought that the antiviral action was produced by the tannin-like polyphenol.
This activity is thought to be unrelated to that of tea tannins, although they are
known antivirals and effective on influenza A (Cohen et al 1964). Kucera and
Herrmann (1967) also explored the antiviral effects of the aqueous extract of
lemon balm against influenza A and B, mumps, and three different strains of
parainfluenza (1, 2, and 3). The results showed that lemon balm had an antiviral
effect on mumps and the three parainfluenza strains, but had no effect on in-
fluenza A and B. Extract of lemon balm is sold in commercial antiviral prepara-
tions in Germany (Foster & Duke 1960). I have found lemon balm essential oil
(5-25%) to be effective against herpes simplex 1 and 2.
Penoel (1991/1992) writes that essential oil of gully gum has strong viricidal
action and suggests the antiviral properties are due to 1,8-cineole (sometimes also
called eucalyptol). 1,8-cineole is found in several essential oils such as bay laurel
(Laurus nobilis), ravensara, spike lavender (Lavandula latifolia), rosemary, Span-
ish sage (Salvia lavendulaefolia), and cardamom (Elettaria cardamomum). Penoel
(1991/1992) suggests that limonene and ␣-pinene reinforce the antiviral action of
1,8-cineole, whereas alcohols strengthen its antiviral action. I have found gully
182 Section II Clinical Use of Aromatherapy

gum, ravensara, spike lavender, and rosemary all effective against both herpes and
the cold virus. I have not tested them against influenza.
Cariel and Jean (1990) tested cypress (Cupressus sempervirens) for viricidal
properties and then applied for a patent. Lemon gum was found to be an effec-
tive antiviral by Mendes et al (1990). This eucalyptus was also studied for its anti-
HIV activities, together with eight other medicinal plants from Zaire (Muanza et
al 1995). May and Willuhn (1978) found eucalyptus had antiviral properties. This
is of particular interest to patients with HIV/AIDS as eucalyptus is also known
to enhance the activity of streptomycin, isoniazid, and sulfetrone in TB, a com-
mon opportunistic infection among those with AIDS (Kufferath & Mundualgo
1954). Extract of eucalyptus was also found effective against herpes simplex I
(Takechi & Tanaka 1985). Extract of sweet marjoram was found to work as an
antiviral in a study by Kucera and Herrmann (1967). Sweet marjoram is a safe es-
sential oil to use on the skin.
Duke (1985) writes that ceylon cinnamon (Cinnamomum verum) and clove
(Syzygium aromaticum) have antiviral properties. Takechi and Tanaka (1981) sug-
gest the actual antiviral substance from the bud is eugeniin. Clove bud oil, which
is used in baking, perfumes, lipsticks, soaps, and dentistry, has caused hand der-
matitis (Lovell 1993), although clove bud essential oil is thought to be safe for use
at up to 5% dilution (Opdyke 1979).
Cinnamon produces two essential oils: one from the leaf and one from the
bark. The leaf essential oil contains less than 7% cinnamic aldehyde (a known skin
irritant), but the essential oil obtained from the bark contains up to 90% cinnamic
aldehyde (Lovell 1993). The latter is therefore contraindicated for topical appli-
cations, as even at such low dilutions as 0.01%, positive reactions have been found
in patch testing (Mathias 1980).
May and Willuhn (1979) tested 178 species of medicinal plants belonging
to 69 families for their virustatic properties. In total, 75 aqueous extracts ap-
peared to have antiviral properties. These were tested against polio, influenza,
and herpes viruses. Bay laurel, oregano, rosemary, and sage were the most effec-
tive of the Lamiaceae family against all three viruses. Juniper also showed sub-
stantial antiviral action against herpes and influenza. Bay laurel should perhaps
be avoided because it can cause contact dermatitis, although the Research Insti-
tute for Fragrance Materials (RIFM) monographs report in three separate tests
there were no reactions on human volunteers (Tisserand & Balacs 1995).
Oregano is high in phenols and known as a skin irritant so is best avoided
(Opdyke 1979). However, oregano can be used in aromatic medicine for acute
and chronic infections when taken by mouth, diluted in gelatin capsules. Please
see section of Chapter 7 on oral use. Juniper is a good choice for topical use be-
cause it contains mainly terpenes and has a very astringent action.
Essential oil of sandalwood was found to have antiviral activity in a study by
Benencia and Courreges (1999). Their study focused on herpes simplex 1 and 2
and was carried out on the kidney cells of monkeys. Sandalwood was most effec-
tive against herpes simplex 1. Benencia and Courreges speculated the antiviral
Chapter 9 Infection 183

effect could be due to sandalwood’s modulatory influence on cellular glutathione
S-transferase activity.
Isoborneol, a monoterpenic component of several essential oils, was found to
have viricidal activity against herpes simplex virus 1. Isoborneol inactivated the
virus within 30 minutes of exposure at a concentration of 0.06%, and completely
inhibited viral replication without affecting viral adsorption (Armaka et al 1999).
Isoborneol did not show significant cytotoxicity when tested against human cell
lines at 0.16%. Therefore essential oils containing major proportions of isoborneol
might be useful in treating herpes.
A lesser-known essential oil, chameleon (Houttynia cordata), was tested
against herpes simplex, influenza, and HIV-1 in a Japanese study by Kyoko et al
(1994). This oil showed remarkable effects, although it was not effective against
the polio and coxsackie virus. The research showed that essential oils have the po-
tential to interfere with the virus envelope, which results in the loss of infectivity
of the virus, because the attachment to the cell surface must necessarily involve
viral-surface glycoproteins present in the envelope.
Garlic has been used against infections for centuries and is the subject of al-
most 1000 research papers. Recent research has shown garlic to be effective
against herpes virus types 1 and 2, parainfluenza virus type 3, vaccinia virus
(cowpox), and human rhinovirus type 2 (a common cold virus). The active in-
gredients, allicin and ajoene, are thought to attack the virus inside the cell, pos-
sibly in the cell membrane (Weber 1992). Although garlic essential oil is avail-
able, it is unlikely to be used in a clinical setting because of its strong, pervasive
odor.
Franchomme and Penoel (1990) list three chemotypes of Thymus vulgaris
(CT thymol, geraniol, and linalol) as antivirals. Sweet marjoram, lemon balm, cy-
press, eucalyptus, and juniper essential oil are all safe to use for treating herpes
simplex 1 and 2. Essential oils that contain a high 1,8-cineole content should be
used with caution in high dilutions on irritated mucous membrane, because they
may cause skin sensitivity. Essential oils that contain 1,8-cineole include gully
gum, bay laurel, ravensara, spike lavender, rosemary, Spanish sage, and cardamom.
Essential oil of eucalyptus is my first choice against herpes simplex 1 and 2. Es-
sential oils can play an important role in the treatment of viral illness. For more
information about the treatment of herpes, including protocols, please see Chap-
ter 20 on immunology.
Fungal Infections
Some of the most deadly infections come from fungi in the air we breathe; when
a healthy immune system is in place, the fungi have no effect (Richardson 2000).
A fungus is a primitive organism classified as neither a plant nor an animal. Only
a few fungi are pathogenic to man, and most cause superficial, mild lesions
(MacSween & Whaley 1992). Fungi are divided into three categories: superficial,
subcutaneous, and systemic. All can be environmental in origin. Fungal infection
184 Section II Clinical Use of Aromatherapy

is caused by airborne allergens, elaborating toxins, or direct infection. A disease,
or infection, caused by fungi is called a mycosis (Parish 1991). With an airborne
allergen (such as tinea, or ringworm) the spores, or hyphae, of the fungus infil-
trate the outer layers of the skin and cause destruction of the epidermis. With
mycetoma, a localized infection occurs that may slowly spread, although with can-
didiasis and cryptococcosis the infection can become systemic.
Cryptococcosis
Cryptococcosis is a yeast infection that is spread by bird droppings and begins as a
sporadic disease manifesting with lung infestation. From the lungs, yeast cells mi-
grate to the CNS. Techically there is a blood-brain barrier (BBB) but this barrier
is not 100% leakproof and under certain conditions, such as immune deficiency,
the BBB is compromised and CNS infection can occur. Standard treatments
are fluconazole, itroconazole, or amphothericin B encapsulated in liposomes
(Cordonnier 1993). This treatment is still in use (Evans 2000). However, clinical
resistance occurs fairly quickly.
Aspergillosis
Spores of this Aspergillosis are present in the atmosphere, and many species are in-
fectious to man. The most common is Aspergillus fumigatus. Although the effect
of this fungus is not as rapid as that of Cryptococcus, the possible resulting
bronchial asthma can be debilitating. The fungus may colonize a bronchial cavity
and can result in necrotizing pneumonia. This tends to occur only in immuno-
compromised patients.
Candida albicans
Candida is normally present in the mouth, intestinal tract, vagina, and on moist
skin and does not pose a problem. However, in certain circumstances, the fun-
gus begins a mucocutaneous, or systemic, invasion. The mucosal infection occurs
when an alteration in the pH of the body tissue produces an alkaline medium
that allows the yeast fungus to proliferate. From the mucosa, Candida can invade
surrounding surfaces such as nail beds, producing chronic, granulomatous in-
flammation of the underlying tissue. It can also spread throughout the body, in-
vading the heart valves, lungs, liver, and kidneys with multiple, small abscesses
containing the fungus (MacSween & Whaley 1992). The symptoms of mucosal
infestation are severe itching, with creamy, curd-like deposits. Candida is the ma-
jor fungal pathogen of immunocompromised patients (Kwon-Chung & Bennett
1992) but is also common in diabetes, pregnancy, antibiotic therapy, and after ra-
diation and chemotherapy. Recently, Candida has become resistant to many con-
ventional drugs and metabolic inhibitors that have no commonality (Goldway et
al 1995).
The incidence of Candida overgrowth has increased dramatically during the
preceding few years and is thought to be related to immune supression, the use of
the contraceptive pill, and the overuse of antibiotics (Zarno 1994).
Chapter 9 Infection 185

Synthetic Antifungals
It is more difficult to treat fungal infections than bacterial infections, because
many fungal infections occur in tissues with poor (if any) blood supply. Examples
of infection sites are the nails, hair, and skin. However, fungal infections are
thought to be less difficult to treat than viral diseases by orthodox medicine. The
drug of choice for fungal infections is fluconazole (Diflucan) or mycostatin
(Nyastatin). Although topical application may keep the fungal infection at bay,
systemic treatment is often given to reduce the incidence of recurrence following
multiple infections. Fluconazole can affect kidney function. Of the other drugs
used to treat fungal infection, many cause nausea and induce skin rashes, and a
few can cause liver damage (Parish 1991). More recently developed antifungals
like itraconazole or Lamasil do cause liver damage (Newsham 2002).
Antifungal Properties of Essential Oils
Essential oils appear to have an antisporulating and respiration-inhibitory effect
on fungi (Inouye et al 1998). In 1927 Myers published some of the earliest re-
search on the antifungal properties of essential oils. He was prompted to investi-
gate the fungicidal properties of essential oils following successful treatment of a
lesion with a diluted solution of cinnamon oil, which caused immediate relief of
symptoms and rapid healing. He observed that thymol, carvacrol, and oil of
lemon destroyed yeast in less than a minute. His research involved nine yeast-like
organisms, which were isolated from infections in humans, including two lung in-
fections, two tongue infections, one infection involving a nail lesion, and various
other cutaneous ulcerations. Each infection rapidly became yeast-negative and
was resolved with no recurrence. Laboratory work has shown that volatile oils ex-
hibit antifungal activity at very low concentrations in growth medium. One ex-
ample is 1 to 10 L
-1
of marjoram reduced the growth of filamentous fungiby up
to 89% (Deans & Svoboda 1990). Electrical or battery-operated diffusers and
nebulizers are the most effective ways of getting essential oils into the lungs.
Nebulizers are a very suitable method of treatment for lung infestations by yeast,
fungi, or bacteria as they fill the air with an extremely fine mist of micromolecules
of essential oil. Nebulizers can be programmed to come on and off at specific
times.
Cryptococcosis
Viollon and Chaumont (1994) tested the susceptibility of a strain of Cryptococcus
neoformans isolated from the blood of a patient with AIDS to 25 essential oils and
17 separate chemical constituents found in essential oils. Many of the essential
oils used showed good fungistatic action. The best effects were from palma rosa,
geranium, savory, sandalwood, thyme, marjoram, and lavender. Pattnaik et al
(1996) reported that lemongrass, eucalyptus, palma rosa, and peppermint were
the most effective essential oils tested against Cryptococcus. Basil and thyme were
186 Section II Clinical Use of Aromatherapy

not included in this study. (Lemongrass in low dilutions was effective not only
against Cryptococcus but against all 11 other fungi tested.) MIC for each of the
four essential oils against Cryptococcus was 5 L
-1
.
In another paper, Pattnaik et al (1997a) found complete essential oils were
more effective against Cryptococcus than their isolated, active components.
Lemongrass was the exception. The effectiveness of lemongrass was equal to the
isolated parts of citral and geranial. Larrondo and Calvo (1991) compared the
topical and inhaled action of citral against the systemic effects of clotrimazole.
Although the actual way essential oils work as fungicides is not completely clear,
it seems metabolism and growth of the fungus is inhibited, often with a break-
down in the lipid part of the membrane, resulting in increased permeability or
rupture (Larrondoet al 1995).
Soliman et al (1994) found rosemary and Mehrotra and Rawat (1993) found
Artemisia parviflora (a member of the Indian tarragon family) to be effective
against Cryptococcus. Although this Artemsia is not in common use, rosemary is
used topically for muscle tension and is inhaled for its antispasmodic effect on
coughs (Price & Price 1995). Viollon and Chaumont (1994) suggest geranium,
palma rosa, savory, and thyme might also be good choices for Cryptococcus. If
the rosemary is a ketone chemotype, avoid using it for extended periods of time
(Tisserand & Balacs 1995).
Aspergillosis
Onawunmi (1989) found West Indian lemongrass (Cymbopogon citratus) and
Garg and Dengre (1988) found cumin (Cuminum cyminum) effective against as-
pergillosis. Tisserand & Balacs (1995) suggest that because cumin has a strong
photosensitizing action, it should not be used topically on patients who will
be exposed to ultraviolet light within 12 hours, and dilutions should be kept to
0.04%. Other effective essential oils include tarragon (Artemisia dracunculus)
(Mehrotra & Rawat 1993) and lemon gum (Hmamouchi et al 1990). Of these,
perhaps lemongrass and lemon gum are most commonly used. Neither of these
essential oils has any known adverse reactions at dilutions of 1% to 5 % (Opdyke
1976). Inoye et al (2000) found that just the vapor of lavender and tea tree
stopped the apical growth of hyphae of Aspergillus in closed containers.
West Indian lemongrass was found effective against Aspergillus fumigatus,
various isolates of Candida, and Trichophyton mentagrophytes by Onawunmi
(1989). The most active component of lemongrass is citral (70% to 80%), which
is thought to be responsible for the antifungal activity of this plant. In another
study, lemongrass was found to be effective against 15 fungi, including Aspergillus
terreus, A. flavus, A. ochraceus, A. parasiticus, A. fumigatus, A. ustus, A. niger, Peni-
cillin nigricans, P. melin, P. chrysogenum, P. brevicompactum, Fusarium moniliforme,
and F. oxysporum (Agarwal et al 1980). Other plants with a high citral content are
lemon grass, citronella, lemon verbena, and lemon gum. Pattnaik (1999) con-
firmed the antifungal acitivty of most Cymbopogon spp. Camphor (Cinnamomum
camphora) was found to be as effective as Ceresan, copper oxychloride, and
Chapter 9 Infection 187

Thiovit (all synthetic, commonly used antifungal agents) against Aspergillus
flavus, a common spoiler of stored food. However, essential oils of both brown
and yellow camphor are contraindicated in human use because they contain saf-
role, which is thought to be carcinogenic.
Candida albicans
Specific essential oils effective against Candida include tea tree (Belaiche 1985),
lemon grass (Larrondo & Calvo 1991), and lemon gum (Hmamouchi et al 1990).
Much has been reported about the antifungal effects of tea tree from Aus-
tralia (Belaiche 1985a; Shemesh 1991), and certainly this is one of the safest and
most effective essential oils to use, particularly in the vagina. However, many
other essential oils have antifungal properties. Caraway, clove, geranium, lavender,
lemon, lemongrass, neroli, peppermint, petitgrain, spearmint, coriander, and
sweet orange leaf are all effective to varying degrees (Galal et al 1973). Coriander
is one of the flavorants of the liqueurs Chartreuse and Benedictine (Lawless
1992). Cuong (1994) found cajuput (Melaleuca cajuputi) effective against Candida
albicans. The cajuput tree grows to a height of 45 feet, and its resilience has made
it something of an unwanted visitor in some parts of the Far East, where it ap-
pears to resist burning and cutting. The principal constituent of the oil is 1,8-
cineole. Traditionally, cajuput has been used in Vietnamese medicine to treat skin
diseases, lice, and fleas (Guenther 1952).
Research from India shows that many Indian essential oils have antifungal
properties (Satinder & Sinha 1991). Although not in common use, these essential
oils can be specially ordered from some of the leading essential-oil distributors.
Some of the Indian essential oils mentioned by Guenther (1952) are as follows:
Long pepper (Piper longum) is a climbing shrub with heart-shaped leaves and
berries that fuse together to form spike-like cylindrical cones. The es-
sential oil is pale green with an odor somewhere between that of black
pepper and ginger. It is effective against Candida albicans.
Holy basil (Ocimum sanctum) has a strong odor of cloves and contains 71%
eugenol, which has antifungal properties.
Ajowan (Trachyspermum ammi), which resembles the parsley plant although
it has a totally different smell, is used in India to treat intestinal prob-
lems. The essential oil has a high thymol content and is used in Indian
medicine to treat cholera as well as fungal infections
Deans and Svoboda (1990) found sweet marjoram effective against As-
pergillus niger and, to a lesser extent, against A. flavus, A. ochraceus, A. parasiticus,
and Trichoderma viride. Candida albicans was also inhibited by 21 different Euca-
lyptus species in a study by Faouzia et al (1993).
Lippia alba, which grows widely in Central and South America, has been shown
to have strong antifungal activity against Trichophyton mentagrophytes var. interdigi-
tale and Candida albicans. Several chemotypes of the plant exist, so the essential oil
from Aruba was thought to be most suitable because it contains 64% citral (Fun &
Svendsen 1990). Lemon verbena (Lippia citriodora) contains 30% to 35% citral.
188 Section II Clinical Use of Aromatherapy

Tea tree has been shown to be extremely effective in the treatment of C. al-
bicans (Belaiche 1985a) in deep nail infections. These infections, which are usu-
ally notoriously difficult to treat, responded well to tea tree. In all eight patients
treated, mycosic degeneration stopped. In two of the cases, the infected nail fell
off but the regrowth was healthy. In the other six cases the nail changed color.
This effect disappeared as the regrowth progressed. Belaiche noted that this has
not been observed with any other antifungal agents. Another important facet of
the study was that the treatment was pain free, and the skin appeared to be very
tolerant of this method.
Tea tree mouthwashes were effective against oral thrush in a young man who
had a bone-marrow transplant. He had a patch of white and green with some yel-
low on his tongue and had been treated for several months with Nystatin with no
success. However, after just 4 days of using a mouthwash with 2% tee tree, his
tongue was clear (Ogden 2001).
Clove (Eugenia caryophyllata) was shown to have fungicidal action at 0.4%
dilution against C. albicans in a study published by Briozzo et al (1989). Dube et
al (1989) found 22 species of fungi, including Aspergillus, were inhibited by the
essential oil of basil (Ocimum basilicum). Larrondo et al (1991) found lemon balm
to be 100% effective against C. albicans. Lemon balm contains 30% citral and 39%
citronella (Wagner 1984). Celery (Apium graveolens) and cumin used together
were effective in inhibiting the growth of 29 fungi tested, including A. flavus and
A. parasiticus. Nenoff et al (1996) reported on the antifungal activity of a compo-
nent of tea tree, y terpinene. Jedlickova et al (1992) found terpinene-4-ol en-
hanced antibiotic (ticarcillin) effects against P. aeruginosa. Terpinene-4-ol is also
an effective antifungal agent. The functional groups of alcohol and terpene are
safe to use on the mucous membrane.
These are just a few examples of the hundreds of research studies (most of
them conducted in vitro) carried out over the last few years indicating the anti-
fungal properties of essential oils. Many of these essential oils are currently being
used only for stress management, not for their antifungal properties, because their
antifungal properties are not appreciated.
Plant oils are also being investigated for agricultural use. The New York Times
reported in 1999 that benzaldehyde, the compound that gives peaches their
aroma, also kills Fusarium oxysporum, Rhizoctania solani, Pythium aphaniderma-
tum, and Sclerotinia minor,which are all common fungi found in soil. Benzalde-
hyde could be a potential replacement for methyl bromide, a widely used pesti-
cide that is toxic to people and also damages the planet’s protective ozone layer
(Cushman 1999).
Parasites
A mainly temperate country such as the United States does not have as much of
a problem with parasites as do countries farther south, where bilharzia and
malaria can be endemic. However, with international travel, West Nile virus has
Chapter 9 Infection 189

arrived in the United States and epidemiologists theorize it is only a question of
time before malaria and yellow fever follow. Bilharzia may not be common in the
United States but scabies, Trichomonas vaginalis, lice, ticks, and fleas are common
parasites, and infestations by hookworm and roundworm can be found.
Synthetic Antiparasites
The antiparasitic drug market is worth $3 billion worldwide. The first modern
anthelmintic (after mercury and arsenic), Thiabendazole, was developed in 1960.
Since then pentamidine (Diamidine) and nitroheterocyclic antiprotozoal drugs
such as metronidazole have been developed. The major problem with treating
parasites with drugs is that the patient may become infected again almost imme-
diately. Many parasites, including malaria-carrying mosquitoes, are becoming
drug resistant, particularly in Africa and Asia where there are no effective drugs
left. The World Health Organization suggests that mefloquine should only be
used for treating the most difficult, drug-resistant cases of malaria. Currently,
there are no effective drugs for Cryptosporidia, which infects the lining of the gut
and causes diarrhea, or Pneumocystis, which infects the lungs.
Antiparasitic Properties of Essential Oils
Malaria
There are approximately 300 to 500 million cases of malaria a year, resulting in
1.75 to 2.5 million deaths (Kayser et al 2002). The reemergence of malaria as
a major health problem, particularly in Africa, is due to the resistance of the
plasmodium-bearing mosquito to quinine, chloroquine, pyrimethamine, cy-
cloguanil, and mefloquine.
Essential oils from plants such as lemon grass, Palma rosa, and citronella (Cym-
bopogon nardus) have a long history of repelling mosquitoes (Ansari & Razdan
1995) and are as effective as the chemical insect repellent N,N-diethyl-meta-
toluamide (DEET) (Rutledge et al 1983). Neem (Azadirachta indica) and tumeric
are also effective (Ansari & Razdan 1995). Watanabe et al (1993) found Eucalyptus
camaldulensis effective, Chokechaijaroenporn et al (1994) found basil effective, and
Mwaiko (1992) found lemon and orange peel oils effective. Studies my students
and I carried out have confirmed the ability of basil, palma rosa, and eucalyptus es-
sential oils to deter mosquitos in human subjects.
Massoud and Labib (2000) studied the effect of extract of myrrh (Com-
miphora molmol) against mosquito larvae. Microscopic examination showed great
pathologic effect on mosquitos’ fat, muscle, gut, and nervous tissue. Currently,
clinical trials are being completed on Artemisia annua ( Juteau et al 2002). In vitro
trials using isolated, biologically active substances (artemisinin and quinghaosu)
obtained from this species of Artemisia, have shown it to have pronounced anti-
190 Section II Clinical Use of Aromatherapy

malarial properties (Klayman et al 1985; Cubukcu et al 1990; Liu et al 1992;
Chalchat et al 1994). Artemisinin and quinghaosu are not found in the essential
oil but may be the precursors, similar to matricin and chamazulene.
Scabies
Scabies (Sarcoptes scabii) produces a papular, intensely itchy rash with burrows in
the finger clefts (Hope et al 1993). Larvae, nymphal instars, and adult mites were
all were killed within 3 hours after applying 5% tea tree in vitro (Walton et al
2000).
Bilharziasis
Bilharziasis is endemic in 76 countries and affects approximately 200 million peo-
ple worldwide (Marston & Hostettmann 1991). It is spread by larvae, which pen-
etrate the host skin and are carried by the blood to the liver. In the liver they ma-
ture, mate, and relocate to the veins around the small intestine where they lay
eggs. Conventional medication is Praziquantel, which kills the worms in situ. Un-
fortunately the dead worms may still be carried back to the liver and cause intense
inflammation. By interrupting the infectious process at the level of the interme-
diate host, this is avoided. Lahlou and Berrada (2001) tested 28 essential oils from
Moroccan aromatic plants against the molluscan intermediate host of the urinary
parasite Bulinus truncatus, which causes bilharziasis. Of the essential oils tested,
75% had molluscicidal acitvity. The most effective were Citrus aurantium L. var.
valencia and Origanum compactum. These were effective within 24 hours and at
low concentrations (0.21 to 0.38 parts per million). Fringed rue (Ruta chalepen-
sis), wormseed (Chenopodium ambrosioides), and Roman chamomile were also ef-
fective.
Other Parasites
Trichomonas vaginalis is a flagellate parasite that causes vaginitis, and there are
other amoebas that cause dysentery-like symptoms. Perhaps more common in the
West are infestations by worms (both roundworms and tapeworms), lice, ticks,
and fleas. Although several aromatherapy books suggest that various essential oils
have anthelmintic properties (which would make them suitable for removing in-
testinal worms), very little research data are available. To treat the gastrointestinal
tract, essential oils need to be taken orally. Parasites that live on or just under the
skin can be effectively treated with topically applied essential oils. Several of my
students in Florida have used essential oils topically to kill sea-lice and remove
the itching and erythema that accompany infestations of this kind. The essential
oil they used was true lavender, either undiluted or at 5% dilution. The effect was
“almost instant.”
Lemon gum has been found to be antiparasitic both for amoeba and for
worms (Gilbert & Mors 1972; De Blasi & Debrot 1990). Eucalyptus has also
been found effective against certain amoeba.
Chapter 9 Infection 191

American wormseed (Chenopodium ambrosioides L. var. anthelminticum) has a
long history of use by North American Indians, who used it to dispel worms and
parasites from the intestine. (They take the herb orally.) Sometimes called
Jerusalem oak, the seeds from this plant produce an essential oil that has been
used for hundreds of years that appears to be safe enough for children (Erichsen-
Brown 1979). Grieve (1931) found this variety of Chenopodium an effective rem-
edy for hookworm and roundworm, and it was listed in the official American
Pharmacopoeia. However, there is often confusion between the herbs Chenopodium
ambrosioides L. var. anthelminticum and Chenopodium botrys L., which contains a
much higher percentage of ascaridole and can cause fatalities.
Wormseed lavant (Artemisia cina) also has a long history of use dating back
to Dioscorides. Its anthelmintic action is thought to be caused by santonin, which
accumulates in the flower heads. It is an effective agent against roundworms and,
to a lesser extent, against threadworms but has no effect on tapeworms. However
the side effects include vision disturbances that add a yellow tinge to everything
the patient sees. Santonin is not found in the essential oil but may be in the CO
2
extract. There are three wormwoods (common, sea, and Roman), which belong to
the genus Artemisia, which also includes tarragon, thought to be an anthelmintic
itself (Lawless 1992). All three herbs (Artemisia absinthium, Artemisia maritima,
and Artemisia pontica) possess anthelmintic properties.
Indian Pinkroot (Spigelia marilandica) is another North American plant that
has been used as a vermifuge by the American Indians (Lewis & Elvin-Lewis
1977). However, Duke (1995) suggests that if used, its extract should be followed
by a saline aperient because the herb is toxic and has effects similar to those of
strychnine. It is used homeopathically for mania and strabismus.
Tea tree and lavender (either Lavandula latifolia or L. angustifolia) are com-
mon essential oils used to treat lice, ticks, and fleas. L. angustifolia can also be
safely used on children and animals. Grosjean (1992) suggests geranium, sage,
or lavender for lice. Marigold (Tagetes minuta) was reported to have an-
thelmintic properties by Lawless (1992). Tisserand (1989) suggests the use of
bergamot, chamomile, camphor, eucalyptus, fennel, hyssop, lavender, lemon
balm, or peppermint. Valnet (1990) suggests all of these, plus cajuput, caraway,
cinnamon, clove, lemon, niaouli, savory, tarragon, and thyme. For the treatment
of ticks, Lawless (1992) suggests sweet marjoram, and for lice she suggests cin-
namon, eucalyptus (blue gum), geranium, spike lavender, Scotch pine, rosemary,
or thyme.
Although some of these essential oils are difficult to obtain and their use may
be controversial, essential oils or CO
2
extracts appear to have potential as an-
tiparasitic agents. In the tropics or developing countries where orthodox drugs are
expensive and difficult to obtain, essential oils might make economic sense. How-
ever, although the information provided here suggests that the essential oils dis-
cussed could have antiparasitic effects, there is no guarantee. Clinical trials are
needed.
192 Section II Clinical Use of Aromatherapy

Cross-Infection
No discussion of infection is complete without mentioning cross-infection. Al-
though this might come under the heading of hospital-acquired infections, cross-
infection can occur anywhere outside a hospital. It can become rampant in insti-
tutions or buildings, especially those that have a closed air-conditioning system.
Cross-infection includes bacterial, viral, fungal, or protozoan infections.
Bardeau (1976) investigated which essential oils can purify and deodorize the
air. Vaporized essential oils were tested for their capacity to destroy bacteria such
as Proteus, Staphylococcus aureus, and Streptococcus pyogenes. Within 3 hours, 90%
of microbes were destroyed. The oils found to be most effective were clove, laven-
der, lemon, marjoram, mint, niaouli, pine, rosemary, and thyme. Kazarinova et al
(2001) published an abstract of their research on using essential oils to “clear” a
hospital surgical unit of unspecified bacteria. The surgical rooms were routinely
irradiated with UV light from 5
PM to 9 AM, after surgery hours. Essential oils of
Organum vulgare and Origanum tyttanthum (two types of oregano) were sprayed
inside the rooms at 2
PM, the time at which the maximum number of microbes
was observed. The antimicrobial effect of the Organum vulgare and Origanum tyt-
tanthum diffused in the air lasted 1 to 4 hours. As a result of this study, the Russ-
ian Federation is confirming a patent.
Benouda et al (1988) tested six essential oils, including tarragon, Coridothy-
mus capitatus, and eucalyptus, against 16 drug-resistant bacteria, with excellent re-
sults.
Research is ongoing as more and more pathogens become resistant to con-
ventional drugs. Hammer et al (1999) tested 52 plant oils and extracts against
Enterococcus faecalis, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aerugi-
nosa, Salmonella enterica subsp. enterica serotype typhimurium, Serratia marcescens,
and Staphylococcus aureus using an agar dilution method. Lemon grass, bay, and
oregano inhibited all oganisms at concentrations of less than or equal to 2%.
Twenty of the oils were effective against Candida. Vetiver was effective against
Staphylococcus aureus at 0.008%. The authors concluded that essential oils “have a
role as pharmaceuticals.” Essential oils could be important for maintaining anti-
sepsis in operating theaters and for protecting health-care professionals. They are
simple to use, considerably less expensive than conventional drugs, have thou-
sands of years of use, have been tested for toxicologic effect, have far fewer side
effects than conventional drugs, and they smell great!
REFERENCES
Abraham E, Chaine E. 1940. An enzyme from bacteria able to destroy penicillin. Na-
ture. 3713, 837-838.
Ackerman, B, Dunk-Richards G 1991. Microbiology: An Introduction for the Health
Sciences. Sydney: Harcourt Brace Jovanovich.
Chapter 9 Infection 193

Agarwal I, Kharwal H, Methela C. 1980. Chemical study and antimicrobial properties
of essential oil of Cymbopogon citratus. Bulletin of Medico-Ethnobotanical Research.
1, 401-407.
Amrine J. 1996. Oils might help beekeepers save hives. The New Mexican, E5.
Ansari M, Razdan R. 1995. Relative efficacy of various oils in repelling mosquitoes. In-
dian Journal of Malariology. 32:104-111.
Armaka M, Papanikolaou E, Sivropoulou A et al. 1999. Antiviral properties of isobor-
neol, a potent inhibitor of herpes simplex virus. Antiviral Research. 43(2) 79-92.
Balacs T. 1993. Antimicrobial Lamiaceae. In Research Reports, International Journal of
Aromatherapy. 5(4) 34.
Bardeau F. 1976. The use of essential oils to purify and deodorise the air. Chirugien-
Dentiste de France (Paris). 46(319) 53.
Belaiche P. 1979. Traite de phytotherapie et d’aromatherapie, Tome 1: L’aro-
matogramme. Paris: Maloine.
Belaiche P. 1985. Treatment of vaginal infections of Candida albicans with essential oils
of Melaleuca alternifolia. Phytotherapy. 15:13-14.
Belaiche P. 1985a. Treatment of skin infections with essential oils of Melaleuca alternifo-
lia. Phytotherapy. 15:15-17.
Benencia F, Courreges M. 1999. Antiviral activity of sandalwood oil against herpes sim-
plex viruses 1 and 2. Phytomedicine. 6(2) 119-123.
Benouda A, Hassar M Benjilali B. 1988. In vitro antibacterial properties of essential oils
tested against hospital pathogenic bacteria. Fitoterapia. 59(2) 115-119.
Blackwell R, Smith M. 1995. Aromatograms. International Journal of Aromatherapy.
7(1) 22-27.
Blaschke T, Bjornsson T. 1995. Pharmacokinetics and pharmacoepidemiology. Scientific
American. 8:1-14.
Briozzo J, Nunez L, Chirife J et al. 1989. Antimicrobial activity of clove oil. Journal of
Applied Bacteriology. 66(1) 69-75.
Budavari S (ed.). 1996. Merck Index, 12th ed. Whitehouse Station, NJ: Merck
Co. Inc.
Caelli M, Porteous J, Carson C et al. 2001. Tea tree oil as an alternative topical decolo-
nization for methicillin-resistant Staphylococcus aureus. Journal of Hospital Infection.
46(3) 236-237.
Cariel L, Jean D. 1990. Antiviral compositions containing proanthocyanidols.
Carmeli Y, Samore M, Huskins C. 1999. The association between antecedent van-
comycin treatment and hospital acquired vancomycin resistant enterococci. Archives
of Internal Medicine. 159(20) 2461-2468.
Carr G. 1996. The profit and loss of AIDS. The Economist. 340:85-86.
Carson C, Riley T. 1993. Antimicrobial activity of essential oil of Melaleuca alternifolia.
Letters in Applied Microbiology. 16:49-55.
Carson C, Cookson B, Farrelly H et al. 1995. Susceptibility of methicillin-resistant
Staphylococcus aureus to the essential oil of Melaleuca alternifolia. Journal of Antimicro-
bial Chemotherapy. 35(3) 421-424.
Chalchat J, Garry R, Lamy J. 1994. Influence of harvest time and composition of
Artemisia annua. Journal of Essential Oil Research. 6:261-268.
Chan C, Loudon K. 1998. Activity of tea tree oil on methicillin-resistant Staphylococus
aureus (MRSA). Journal of Hospital Infection. 39(3) 244-245.
194 Section II Clinical Use of Aromatherapy

Chin Y, Chang N, Anderson H. 1949. Factors influencing the antibiotic activity of lupu-
lon. Paper presented at the Second National Symposium on Recent Advances in An-
tibiotic Research, 11-12 April. Washington, DC: National Institutes of Health.
Chokechaijaroenporn O, Bunyapraphatsara N, Kongchuensin S. 1994. Mosquito repel-
lent activities of Ocimum volatile oils. Phytomedicine. 1/2:135-139.
Chowdhury A. 1998. Therapeutic potential of the volatile oils of Nigella sativa in mon-
key model with experimental Shigellosis. Physiotherapy Research. 12(5) 361-363.
Cohen R, Kucera L, Herrmann E. 1964. Antiviral activity of Melissa officinalis. Proceed-
ings of the Society for Experimental Biology and Medicine. 117:431-434.
Cooke A, Cooke M. 1994. Cawthron Report Number 263: An investigation into the an-
timicrobial properties of manuka and kanuka oil. Nelson, New Zealand: Cawthron.
Cordonnier C. 1993. Les traitment preventifs et curatifs des mycoses en oncohematolo-
gie. In Euromedicine 1993. Monpelier-Le Corum. 9emes Rencontres internationals de
recherches et de technologies medicales et pharmaceutiques. (Conference.) Paris: 10-13
Nov 1993.
Corpet D. 1987. Antibiotic residues and drug resistance in human intestinal flora. An-
timicrobial Agents and Chemotherapy. 31(4) 587-593.
Craig C, Stitzel R. 1994. Modern Pharmacology, 4th ed. Boston: Little, Brown & Co.
Cubukcu B, Bray D, Warhurst D. 1990. In vitro antimalarial activity of crude extracts
and compounds from Artemisia abrotanum. Phytotherapy Research. 4:203-204.
Cuong N. 1994. Antibacterial properties of Vietnamese cajuput oil. Journal of Essential
Oil Research. 6:63-67.
Cushman J. 1999. Peach oil may work as a pesticide. New York Times. Sunday, March
14, 18.
De Blasi V, Debrot S. 1990. Amoebicidal effect of essential oils in vitro. Journal of Clini-
cal Toxicology and Experimental Therapeutics. 10:351-373.
de Castillo M, de Allori C, de Gutierrez R et al. 2000. Bactericidal activity of lemon
juice and lemon derivatives against Vibrio. Biological & Pharmaceutical Bulletin.
23(10) 1235-1238.
de la Puerta R, Saenz M, Garcia M. 1993. Cytostatic activity against HEp-2 cells and
antibacterial activity of essential oils from Helichrysum picardii. Phytotherapy Re-
search. 1:378-380.
Deans S, Ritchie G. 1987. Antibacterial properties of plant essential oils. International
Journal of Food Microbiology. 5:165-180.
Deans S, Svoboda K. 1988. Antibacterial activity of French tarragon (Artemisia dracuncu-
lus) essential oil and its constituents during ontogeny. Journal of Horticultural Science.
63(3) 503-508.
Deans S, Svoboda K. 1989. Antibacterial activity of summer savory (Satureja hortensis)
essential oil and its constituents. Journal Of Horticultural Science. 64(2) 205-210.
Deans S, Svoboda K. 1990. The antimicrobial properties of marjoram (Origanum majo-
ranum) oil. Flavour and Fragrance Journal. 5:187-190.
Deans S, Svoboda K et al. 1992. Essential oil profiles of several temperate and tropical
aromatic plants: Their antimicrobial and antioxidant activities. Acta Horticulturae.
306:229-233.
Deinenger E. 1995. The spectrum of activity of plant drugs containing essential oils. In
Conference Proceedings, Holistic Aromatherapy. San Francisco: Pacific Institute of
Aromatherapy, 15-43.
Chapter 9 Infection 195

Dolara P, Corte B. Ghelardini C et al. 2000. Local anesthetic, antibacterial and antifun-
gal properties of sesquiterpenes. Planta Medica. 66(4) 356-358.
Dorman H, Deans S. 2000. Antimicrobial agents from plants: Antibacterial activity of
plant volatile oils. Journal of Applied Microbiology. 88(2) 308-316.
Dube S, Upadihay P, Tripathi S. 1989. Antifungal, physiochemical and insect-repelling
activity of the essential oil of Ocimum basilicum. Canadian Journal of Botany. 67(7)
2085-2087.
Duke J. 1985. Handbook of Medicinal Herbs. Boca Raton, FL: CRC Press.
Ena J, Dick R, Wenzel R. 1993. The epidemiology of intravenous vancomycin usage in a
university hospital: A ten-year study. Journal of the American Medical Association.
269(5) 598-602.
Erichsen-Brown C. 1979. Medicinal and Other Uses of North American Plants. New
York : Dover.
Faouzia H, Fkih-Tetouani S, Tantaoui-Elaraki A. 1993. Antimicrobial activity of
twenty-one Eucalyptus essential oils. Fitoterapia. 64:1.
Ferdous A, Islam S, Ahsan M. 1992. In vitro antibacterial activity of the volatile oil of
Nigella sativa seeds against multiple drug-resistant isolates of Shigella spp. and isolates
of Vibrio cholerae and E. coli. Phytotherapy Research. 6:137-140.
Fields H. 1997. Pain: Anatomy and physiology. Journal of Alternative & Complemen-
tary Medicine. 3(Suppl 1) S41-S46.
Fisher J. 1994. The Plague Makers. New York: Simon & Schuster.
Foster S, Duke J. 1960. A Field Guide to Medicinal Plants (Eastern/Central). New
York: Houghton Mifflin Co.
Franchomme P, Penoel D. 1990. L’aromatherapie. Limoges, France: Jollois.
Franchomme P, Penoel D. 1991. L’aromatherapie Exactement. Limoges, France: Jollois.
Fun C, Svendsen A. 1990. The essential oils of Lippia alba. Journal of Essential Oil Re-
search. 2(5) 265-267.
Galal E, Adel M, El-Sherif S. 1973. Evaluation of certain volatile oils for their antifun-
gal properties. Journal of Drug Research. 5(2) 235-245.
Garg S, Dengre S. 1988. Antifungal activity of some essential oils. Pharmacie. 43(2)
141-142.
Gascoigne S. 1993. Manual of Conventional Medicine for Alternative Practitioners, Vol.
1. Richmond, VA: Jigme Press.
Gattefosse R. 1948. French lavender: Production and economics. Perfumery and Essen-
tial Oil Record. 39:318-319.
Gilbert B, Mors W. 1972. Anthelmintic activity of essential oils and their constituents.
Anais da Academia Brasileira de Ciencias. 44:423-428.
Goldway G, Teff D, Schmidt R et al. 1995. Multidrug resistance in Candida albicans:
Disruption of the BEN gene. Antimicrobial Agents and Chemotherapy. 39(2)
422-426.
Grieve M. 1931. A Modern Herbal. Harmondsworth, UK: Penguin Books.
Grosjean N. 1992. Aromatherapy from Provence. Saffron Walden, UK: CW Daniels.
Guenther E. 1952. The Essential Oils. Malabar, FL: Krieger.
Hammer K, Carson C, Riley T. 1999. Antimicrobial activity of essential oils and other
plant extracts. Journal of Applied Microbiology. 86(6) 985-990.
Harris B, Harris R. 1995. Essential oils as antifungal agents. Aromatherapy Quarterly.
44:25-27.
Hawkes N. 2001. Oxygen cuts infections by half. The Times. Wednesday June 27, 5.
196 Section II Clinical Use of Aromatherapy

Hmamouchi M, Tantaoui-Elaraki A, Es-Safi N et al. 1990. Illustrations of antibacterial
and antifungal properties of Eucalyptus essential oils. Plantes Medicinales et Phy-
totherapie. 24(4) 278-279.
Hope R, Longmore J, Hodgetts T et al. 1993. Oxford Handbook of Clinical Medicine,
3rd ed. Oxford, UK: Oxford University Press, 217.
Inouye S, Watanabe M, Nishiuyama Y et al. 1998. Antisporulating and respiration-
inhibitory effect on filamentous fungi. Mycoses. 41(9-10) 403-410.
Inoye S, Tsuruoka T, Watanabe M et al. 2000. Inhibitory effect of essential oils on apical
growth of Aspergillus fumigatus by vapor contact. Mycoses. 43(1-2) 17-23.
Jain S, Purohit M. 1992. Pharmacological evaluation of Cuminum cyminum. Fitoterapia.
6314:291-294.
Jedlickova Z, Mottl O, Sery V. 1992. Antibacterial properties of the Vietnamese Cajeput
oil and Ocomum oil in combination with antibacterial agents. Journal of Hygiene,
Epidemiology, Microbiology and Immunology. 36(3) 303-309.
Jensen A, Wachmann C, Poulsen K et al. 1999. Risk factors for hospital acquired Staphy-
lococcus aureus bacteremia. Archives of Internal Medicine. 159(13) 1437-1444.
Jukes T. 1973. Public health significance of feeding low levels of antibiotics to animals.
Advances in Applied Microbiology. 16:1-29.
Juteau F, Masotti V, Bessieve V. Antibacterial and antioxidant activiy of Artemesia annua
essential oil. 2002. Fitoterapia. 73 (6) 532-535.
Kayser O, Kiderlen A, Croft S. 2002. Natural products as potential antiparasitic drugs. Freie
Universitat Berlin. Berlin, Germany.
Kazarinova N, Tkachenko K, Shurgaja A. 2001. Essential oils of Origanum vulgare and
Origanum tyttanthum Gontsch as the remedy of struggle against intrahospital infec-
tions. Botanical Institute, Russian Academy of Sciences. St. Petersburg, Russia.
Kedzia B. 1991. Antimicrobial activity of oils of chamomile and its components. Herba
Polonica. 37(1) 29-38.
Klayman D. 1985. Qunghaosu (artemisin): An antimalarial drug from China. Science.
228(4703) 1049-1055.
Koga T, Hirota N, Takumi K. 1999. Bactericidal activities of essential oils of basil and
sage against a range of bacteria and the effect of these essential oils on Vibrio para-
haemolyticus. Microbiological Research. 154(93) 267-273.
Kole C. 1997. Antibacterial and antifungal activity of aromatic constituents of essential
oils. Microbios (Cambridge). 89:39-46.
Kucera L, Herrmann E. 1967. Antiviral substances in plants of the mint family (Labi-
atae). 1. Tannin of Melissa officinalis. Proceedings of the Society for Experimental Bi-
ology and Medicine. 124:865, 874.
Kufferath F, Mundualgo G. 1954. The activity of some preparations containing essential
oils in TB. Fitoterapia. 25:483-485.
Kwon-Chung K, Bennett J. 1992. Medical Mycology. Philadelphia: Lea & Febiger,
280-336.
Kyoko H, Kamiya M, Hayashi T. 1994. Viricidal effects of the steam distillate from
Houttynia cordata and its components on HSV-1, influenza virus and HIV. Planta
Medica. 61(3) 237-241.
Lahlou M, Berrada R. 2001. Potential of essential oils in schistosomiasis control in Mo-
rocco. International Journal of Aromatherapy. 11(2) 87-96.
Larrondo J, Calvo M. 1991. Effects of essential oils on Candida albicans: A scanning
electron microscope study. Biomedical Letters. 46(184) 269-272.
Chapter 9 Infection 197

Larrondo J, Agut M, Calvo-Torres M. 1995. Antimicrobial activity of essences from
labiates. Microbios. 82:171-172.
Larrondo J, Calvo M. 1991. Effect of essential oils on Candida albicans: A scanning elec-
tron microscope study. Biomedical Letters. 46(184) 269-272.
Lawless J. 1992. Encyclopedia of Essential Oils. Shaftesbury, UK: Element Books.
Leclercq R, Derlot E, Duval J et al. 1988. Plasmid-mediated resistance to vancomycin
and teicoplanin in Enterococcus faecium. New England Journal of Medicine. 319(3)
157-161.
Lewis W, Elvin-Lewis M. 1977. Medical Botany. New York: Wiley Interscience.
MacSween R, Whaley K (eds.). 1992. Muir’s Textbook of Pathology, 13th ed. London:
Edward Arnold.
Liu K, Yang S, Roberts M. 1992. Antimalarial activity of Artemisia annua flavonoids
from whole plants and cell cultures. Plant Cell Reports. 11(12) 637-640.
Lovell C. 1993. Plants and the Skin. Oxford, UK: Blackwell Scientific Publications.
Mann C, Cox S, Markham J. 2000. The outer membrane of Pseudomonas aeruginosa
NCTC 6740 contributes to its tolerance to the essential oil of Melaleuca alternifolia.
Letters in Applied Microbiology. 30(4) 294-297.
Mann C, Markham J. 1998. A new method for determining the minimum inhibitory
concentration of essential oils. Journal of Applied Microbiology. 84(4) 538-544.
Mansfield P. 1996. Animal experiments are an obstacle to health. Holistic Health. 50:4-7.
Marston A, Hostettmann K. 1991. Assay for molluscicidal, cercaricidal, schistosomicidal
and piscicidal activities. Methods in Plant Biochemistry. 6:153-178.
Maruzella J, Percival H. 1958. Antimicrobial activity of perfume oils. Journal of the
American Pharmaceutical Association. XLVII, 471-476.
Maruzella J, Sicurella N. 1960. Antibacterial activity of essential oil vapors. Journal of
the American Pharmaceutical Association (Scientific Edition). 49(11) 693-695.
Massoud A, Labib I. 2000. Larvicidal activity of Commiphora momol against Culex pipiens
and Aedes caspius larvae. Journal of the Egyptian Society of Parasitology. 30(1)
101-115.
Mathias C. 1980. Contact urticaria from cinnamic aldehyde. Archives of Dermatology.
116(1) 74-76.
May G, Willuhn G. 1979. Antiviral activity of aqueous extracts from medicinal plants in
tissue cultures. Arzneimittel-Forschung Drug Research. 28(1) 1-7.
Mehrotra S, Rawat A. 1993. Antimicrobial activity of the essential oils of some Indian
Artemisia species. Fitoterapia. 14:65-68.
Mendes N, Araujo N, De Souza C et al. 1990. Molluscicidal and carcaricidal activity of
different species of Eucalyptus. Revista Societe Brasilia Medicinale Tropicale. 23(4)
197-199.
Muanza D, Euler K, Williams L et al. 1995. Screening for antitumor and anti-HIV ac-
tivities of nine medicinal plants from Zaire. International Journal of Pharmacology.
33(2) 98-105.
Mwaiko G. 1992. Citrus peel oil extracts of mosquito larvae. Insecticides. 69(4)
223-226.
Myers H. 1927. An unappreciated fungicidal action of certain volatile oils. Journal of the
American Medical Association. 1834-1836.
Natural Medicines Comprehensive Database 2002, 4th ed. Stockton, CA: Therapeutic
Research Faculty.
198 Section II Clinical Use of Aromatherapy

Nelson R. 1997. In vitro activities of five plant essential oils against methicillin-resistant
Staphylococcus aureus and vancomycin-resistant Entericoccus faecium. Journal of Antimi-
crobial Chemotherapy. 40(2) 305-306.
Nenoff P, Haustein U, Brndt W. 1996. Anifungal activity of Melaleuca alternifolia
(teatree oil) aginst pathogenic fungi in vitro. Skin Pharmacology and Applied Skin
Physiology. 9:388-394.
Newsham G. 2002. Personal communication.
Onawunmi G. 1989. Evaluation of the antifungal activity of lemongrass oil. Interna-
tional Journal of Crude Drug Research. 27(2) 121-126.
Onawunmi G, Ogunlana E. 1986. A study of the antibacterial activity of essential oil of
lemongrass. International Journal of Crude Drug Research. 24(2) 64-68.
Opdyke D. 1976. Inhibition of sensitization reactions induced by certain aldehydes. Food
and Cosmetics Toxicology. 14(3) 197-198.
Opdyke D (ed.). 1979. Monographs on Fragrance Raw Materials. Oxford, UK: Perga-
mon Press.
Parish P. 1991. Medical Treatments: The Benefits and the Risks. Harmondsworth, UK:
Penguin Books.
Pattnaik S, Subramanyam V, Kole C. 1996. Antibacterial and antifungal activity of es-
sential oils in vitro. Microbios. 86(349) 237-246.
Pattnaik S, Subramanyam V, Bapaji M et al. 1997. Antibacterial and antifungal activity
of aromatic constituents of essential oils. Microbios. 89(358) 39-46.
Peana A, Moretti M, Juliano C. 1999. Chemical composition and antimicrobial action of
the essential oils of Slavia desoleana and Salvia sclarea. Planta Medica. 65(8) 752-754.
Reichman L, Tanne J. 2001. Timebomb: The Global Epidemic of Multi-Drug-Resistant
Tubercuolosis. New York: McGraw-Hill.
Penoel D. 1991/1992. Eucalyptus smithi essential oil and its use in aromatic medicine.
British Journal of Phytotherapy. 2(4) 154-159.
Price S. 1995. Aromatherapy for Health Professionals. London: Churchill Livingstone.
Richardson K. 2000. www.organicessentialoils.com/articles/kenrichardson/html.
Roberts M. 1986. Biology: A Functional Approach, 4th ed. Walton on Thames, UK:
Nelson.
Ross S, El-Keltawi N, Megella, S. 1980. Antimicrobial activity of some Egyptian aro-
matic plants. Fitoterapia. 51(4) 201-205.
Rubinstein E, Green M, Molan M. 1982. The effects of nosocomial infections on
the length and costs of hospital stay. Journal of Antimicrobial Chemotherapy.
9(Suppl.) 93.
Rutledge L, Collister D, Meixsell V et al. 1983. Comparative sensitivity of representative
mosquitos to repellents. Journal of Medical Entomology. 20(5) 506.
Satinder K, Sinha G. 1991. In vitro antifungal activity of some essential oils. Journal of
Research into Ayurveda and Siddha. 12:200-205.
Savino A, Lollini M, Menghini A. 1994. Antimicrobial activity of the essential oil of
Pneumus boldus (boldo). Aromatogram and electron microscopy observations. Bollet-
tino di Microbiologia e Indagini Laboratorio. 14(1) 5-12.
Schmidt M. 1995. Antibiotics: The promise and the peril. In Conference Proceedings,
Holistic Aromatherapy. San Francisco: Pacific Institute of Aromatherapy, 81-88.
Sears C. 1995. How to sell drugs. New Scientist. Nov 4, 37-40.
Service R. 1994. E. coli scare spawns therapy search. Science. 265:475-476.
Chapter 9 Infection 199

Shemesh A. 1991. Australian tea-tree: A natural antiseptic and fungicidal agent. Aus-
tralian Journal of Pharmacy. 12:802-803.
Sherry E, Boeck H, Warnke P. 2001. Percutaneous treatment of chronic MRSA os-
teomyelitis with a novel plant-derived antiseptic. BioMed Central Surgery. www.
biomedcentral.com.
Sleigh J, Pennington T, Lucas S. 1992. Microbial infection. In MacSween R, Whaley K
(eds.), Muir’s Textbook of Pathology, 13th ed. London: Edward Arnold, 301–302.
Soliman F, El-Kashoury E, Fathy M et al. 1994. Analysis and biological activity of es-
sential oil of Rosmarinus officinalis. Flavour and Fragrance Journal. 9:29-33.
Sullivan A. 1995. When plagues end. New York Times Magazine. Nov 10, 52-84.
Takechi M, Tanaka Y. 1981. Purification and characterisation of antiviral substance eu-
genin from the bud of Syzygium aromatica aromaticum. Planta Medica. 42:69-71.
Takechi M, Tanaka Y, Takehara M et al. 1985. Structure and antiherpetic activity among
the tannins. Phytochemistry. 24(10) 2245-2250.
Tamm C. 1971. Recent advances in the field of antibiotics. In Wagner H, Wolffe P
(eds.), New Natural Products and Plant Drugs with Pharmacological, Biological or
Therapeutic Activity. Berlin, Germany: Springer-Verlag, 82-136.
Tisserand R. 1988. Aromatherapy for Everyone. Harmondsworth, UK: Penguin Books.
Tisserand R. 1989. The Art of Aromatherapy. Saffron Walden, UK: CW Daniels.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Viana G, Vale T, Pinho R et al. 2000. Antinociceptive effect of the essential oil of Cym-
bopogon citratus in mice. Journal of Ethnopharmacology. 70(3) 323-327.
Viollon C, Chaumont J. 1994. Antifungal properties of essential oils and their main
components against Cryptococcus neoforms. Mycopathologia. 128(3) 151-153.
Wagner H. 1984. Plant Drug Analysis. Berlin, Germany: Springer-Verlag.
Walton S, Myerscough M, Currie B. 2000. Studies in vitro on the relative efficacy of
current acaricides for Sarcoptes scabiei var. hominis. Transactions of the Royal Society of
Tropical Medicine and Hygiene. 94(1) 92-96.
Ward K. 1993. Care of the person with an infection. In Hinchcliff S, Norman S (eds.),
Nursing Practice and Health Care. London: Edward Arnold, 402-434.
Watanabe K, Shono Y, Kakimizu A et al. 1993. New mosquito repellent from Eucalyptus
camaldulensis. Journal of Agriculture & Food Chemistry. 41(11) 2164-2166.
Weber N, Andersen D, North J. 1992. In vitro viricidal effects of Allium sativum. Planta
Medica. 58(5) 417-423.
Wilson J. 2001. Infection Control in Clinical Practice, 2nd ed. London: Bailliere Tindall.
www.sunysccc.edu/academic/mst/microbes/microbes.htm. (Accessed March 16, 2003).
www.cdc.gov/ncidod/dbmd/diseaseinfo/groupastreptococcal_g.htm. (Accessed March 16,
2003).
Zakarya D, Fkih-Tetouani S, Hajji F. 1993. Antimicrobial activity of twenty-one Euca-
lyptus essential oils. Fitoterapia. 64:319-331.
Zarno V. 1994. Candidiasis. International Journal of Aromatherapy. 6(••) 20-23.
200 Section II Clinical Use of Aromatherapy

W
201
10
Insomnia
One sees clearly only with the heart, everything essential is invisible to the eyes.
Antoine De Saint-Exupery
The Little Prince
Insomnia
Today’s society is fast-moving and achievement-oriented in which thousands of
people travel daily, often across time zones. Regularity and sleep patterns are con-
stantly disturbed as new sounds and unfamiliar surroundings compound the sense
of timelessness caused by continuous movement. Sleep has become a commodity
to be bought and sold.
Patients in hospitals are separated from everything that makes them relaxed
and sleepy. They are in a strange bed, with a strange routine, and often have a
sense of fear. It is hardly surprising that sleeping pills are almost de rigueur. Aro-
matherapy offers another alternative, especially in the case of patients in the hos-
pital for a long stay who take sleeping tablets regularly.
Sleepless nights can affect us all at some time in our lives. Trauma, worries,
and jet lag can all cause insomnia. However, repeated sleepless nights result in a
poor attention span and, ultimately, in poor health, both physical and mental.
Sleep is defined by Manley (1993) as an “altered state of consciousness from
which a person can be aroused by stimuli of sufficient magnitude.” Why sleep is nec-
essary is unclear, but this period of “opting out” is essential for healthy living. Going
without sleep produces varying degrees of symptoms, ranging from feeling irritable
to psychosis. For a patient in the hospital, sleep deprivation is just one more stressor.
Sleep occurs in two modes: rapid eye movement (REM) sleep, when dream-
ing occurs, and orthodox sleep. Both types of sleep are important. Sleep is

thought to be controlled by a natural chemical called melatonin, which is secreted
by the pineal gland. It is possible to buy this compound over the counter as a sup-
plement, although it has recently been banned in the United Kingdom.
Insomnia is usually transitory, and after the trauma causing the insomnia has
passed, normal sleep rhythms return. However, chronic insomnia threatens to de-
stroy normal functioning. This kind of sleep problem can occur in two forms: fail-
ure to drift off to sleep or waking up after a short period. Both occur in a hospital,
where strange noises and smells permeate through dreams or prevent sleep from
occurring. A bedtime routine is also very difficult to maintain in the hospital.
Sleeping Tablets
Orthodox treatment of insomnia involves two types of drugs, sedatives (anxiolyt-
ics) and sedative-hypnotics. The most common sleeping tablet is a benzodi-
azepine, which is both sedative-hypnotic and anxiolytic, such as diazepam (Val-
ium), lorazepam (Ativan), or nitrazepam (Mogadon). Dependency can occur
within weeks.
Benzodiazepines
Benzodiazepines have the basic structure of a benzene ring coupled to a seven-
membered, heterocyclic structure containing two nitrogen atoms (diazepine) at
positions 1 and 4 (Dailey 1994). This molecule binds to specific macromolecules
within the central nervous system (CNS) at receptors closely associated with ␥-
aminobutyric acid (GABA) transmission. GABA is the main inhibitory neuro-
transmitter in the brain. Research has indicated that benzodiazepines potentiate
GABA transmission.
Benzodiazepines depress the CNS and in low dosages produce a feeling of
calm. As the dose is increased, a feeling of drowsiness is followed by hypnosis and
muscle relaxation. The interval between feeling drowsy and potential death by
overdose is a large one. Because these drugs have a large therapeutic index they
are extremely useful for many patients, although their long-term use can be prob-
lematic. Benzodiazepines have almost entirely replaced the previous favorite
sleeping pill, the barbiturate.
Barbiturates
Barbiturates are used to treat intractable insomnia and are increasingly rarely pre-
scribed. They, too, bind to receptors associated with GABA transmission. How-
ever, this class of drug prolongs, rather than intensifies, the GABA effect. Public
awareness of the dangers of barbiturate dependence was heightened in the 1970s
by novels like Valley of the Dolls, by Jacqueline Susann. Barbiturates have signifi-
cant drug interactions. Several of the drugs they react with are in common use,
for example, the contraceptive pill, digoxin, beta-blockers, and anticoagulants.
Barbiturates accelerate the metabolism of these drugs, necessitating an increased
dosage. In addition, if the patient is on anticoagulant therapy, when barbiturates
202 Section II Clinical Use of Aromatherapy

are discontinued a dangerous reaction resulting in severe hemorrhage can occur
(Dailey 1994). This type of reaction can also occur with other drugs because the
induction of GABA metabolism has stopped.
Essential Oils with Sedative Effects
“Lavender Beats Benzodiazepines” was a 1988 headline in the International Jour-
nal of Aromatherapy (Tisserand 1988). In this article, the use of essential oils as
sedatives in a hospital setting was outlined. Of particular note were lavender, mar-
joram, geranium, mandarin, and cardamom.
Helen Passant, possibly the most holistic nurse after Florence Nightingale, in-
troduced aromatherapy into the Churchill Hospital, in Oxford, England, where she
was in charge of a ward for the elderly. Remarkably, Passant reduced her original
drug bill by one third by gradually replacing analgesia and night sedation with es-
sential oils. She found her patients seemed to “get off to sleep just as easily, if not bet-
ter, with oils of lavender or marjoram, either vaporized or applied by massage” (Tis-
serand 1988). In the same article another hospital was mentioned. The Radcliffe
Infirmary, also in Oxford, introduced aromatherapy into Beeson Ward at about the
same time. Patients were given the option of aromatherapy instead of night sedation
or analgesics. Nearly all of the patients chose aromatherapy (Tisserand 1988).
Traditionally, true lavender (Lavandula angustifolia) has been used in aro-
matherapy to promote sleep and relaxation and to relieve anxiety. In Bulgaria,
Atanassova-Shopova et al (1973) found that linalol and terpineol were the active
components of lavender and had a depressing effect on the CNS. Oral doses
of linalool were found to be hypnotic and anticonvulsant in mice in a study by
Elisabetsky et al (1995). Elisabetsky et al (1995a) also established that linalol inhib-
ited glutamate binding in rat cortex in a way similar to phenobarbital. The glutamate
binding involved all receptor subtypes investigated. A Japanese study (Yamada et al
1994) concurred that inhaled lavender had anticonvulsant effects in mice.
In France, Guillemain et al (1989) agreed that oral doses of lavender (diluted
at 1:60 in olive oil) had marked sedative effects on mice and enhanced barbitu-
rate sleep time. In Germany, Buchbauer et al (1991) in Germany found that true
lavender had a sedative effect when inhaled by mice. Interestingly, the more agi-
tated the animal (as a result of the injection of caffeine), the more effective the
calming effect of true lavender. Jager et al (1992) established that lavender diluted
in peanut oil was absorbed through the skin.
Henry et al (1994) carried out a study on human subjects at Newholme Hos-
pital in Bakewell, England. The effects of nighttime diffusion of lavender in a
ward of dementia patients was monitored. The trial ran for 7 weeks and showed
that lavender had a statistically significant sedative effect when inhaled. Hudson
(1995) also found lavender was effective for elderly patients in a long-term unit.
Eight of the nine patients in the study had improved sleep at night and improved
alertness during the day. Lavender straw (the byproduct of distillation) was itself
found to reduce stress of pigs in transit in a study by Bradsaw et al (1998).
Chapter 10 Insomnia 203

Jager et al (1992a) found that neroli had a sedative effect on mice. In this
study, the sedative effects were observed during the first 30 minutes of exposure
to the aroma. Citronellal and phenylethyl acetate (components of essential oils)
were also found to have sedative properties. Citronellal is found in citronella
(Cymbopogon nardus), lemon gum (Eucalyptus citriodora), narrow-leaved pepper-
mint (Eucalyptus radiata), lemon, rose, melissa, lemongrass, basil, and geranium.
Phenylethyl acetate is found only in neroli, but phenylethyl alcohol is also found
in geranium (bourbon) and rose (Sheppard-Hangar 1995).
Buchbauer et al (1992) found essential oils of passionflower (Passiflora incar-
nata) and lime blossom (Tilia cordata) had sedative effects. Lime blossom and its
major component, benzyl alcohol, decreased the motility of animals in both nor-
mal and induced-agitation states. Interestingly, passionflower and its main com-
ponents, maltol and 2-phenylethanol, only reduced motility when the animals
were in an agitated state. This underscores the feeling amongt herbalists and aro-
matherapists that essential oils are adaptogens.
Khanna et al (1993) found black cumin (Nigella sativa) essential oil had a
sedative effect more powerful than the drug chlorpromazine (Largactil) and was
also an analgesic. The study suggested black cumin contained an opioid-like com-
ponent. West and Brockman (1994) reported on how aromatherapy helped de-
mentia patients with disturbed sleep and compulsive daytime activity. Several es-
sential oils were used.
Weihbrecht (1999) investigated the effect of inhaled true lavender on 10
adults (3 men and 7 women) who had a history of chronic insomnia. Subjects
took baseline measurements for the first 14 days and recorded difficulty getting
to sleep, naps taken during the day, difficulty returning to sleep, and feeling rested
in the morning. A visual analog scale of 1 to 10 was used (1 ⫽ very difficult,
10 ⫽ no difficulty). Subjects were asked not to change what they normally did
and to continue their sleep medication. For days 15 to 29 of the study, 2 drops of
true lavender were placed on the patients’ pillows or on a tissue kept nearby at
bedtime. Subjects mailed back a sleep questionnaire, and a telephone interview
was completed with each of them following completion of the study. One partic-
ipant pulled out of the study because she did not like the smell of lavender. Eight
participants had improved sleep in 1 of the 4 areas measured, and 8 reported less
difficulty in getting to sleep. One person reported that his difficulty was neither
improved nor worsened by the use of lavender, but he had the flu during the ex-
perimental stage. Of all participants, 8 reported feeling more rested in the morn-
ing. The sleep aids normally used by the participants did not change.
King (2001) tested the effect of Roman chamomile (Chamomelum nobile) and
sweet marjoram (Origanum majorana) on insomnia. Ten women between the ages
of 36 and 59 with sleep problems took part in the study. One client had an allergy
to ragweed so a patch test was completed before the study began to make sure she
was not allergic to chamomile. Each subject was given a bottle containing a mix-
ture of Roman chamomile and sweet marjoram in a ratio of 1:2. For the first 7
days, baselines were established. The second week the subjects used the aro-
204 Section II Clinical Use of Aromatherapy

matherapy mixture; the third week was a washout week with no aromatherapy;
and the fourth week was a repeat of the second week. During week 2 and week 4
(the aromatherapy weeks), 2 drops of essential oils were put on a cotton ball and
placed in the pillowcases of the subjects at bedtime. Subjects recorded time to fall
asleep, number of times waking, how long it took to fall back to sleep, span of
time from bedtime to getting up, and whether they felt rested in the morning.
The data were entered on in spreadsheet software program so results could be
compared.
Two subjects withdrew from the study because they reacted negatively to the
mixture. Neither of them liked the aroma. One subject experienced nausea and
headache, and the other had a severe headache. These two subjects were not en-
tered into the analysis. The results indicated a small improvement in almost every
category. Five women experienced an improvement in the time it took to go to
sleep. One subject took 240 minutes to fall asleep one night because of a death in
her family. The outcomes of the study were not changed to accommodate that. Six
women showed a reduction in the number of times they woke up during the night.
Only three women showed a reduction in the time taken to fall back to sleep. Five
women felt more rested after a night’s sleep with the aromatherapy mixture.
Most people enjoy the smell of roses. Rose is perhaps the most popular
aroma in the world. Despite the fact that essential oil of rose is expensive, the cost
may be justified where chronic insomnia is concerned. To date, there have been
no clinical studies to show that rose is effective in promoting sleep in humans.
However, Nacht and Ting (1921) and Rovesti and Columbo (1973) showed that
rose (Rosa damascena) essential oil has sedative effects. Certainly my personal ex-
perience, as well as that of my students and patients, suggests that rose is a strong
contender and certainly an essential oil to try for insomnia.
Finally, while conducting routine toxicity investigations of Tastromine (-
dimethylaminoethyl thymol ether), it was observed that the animals used in the
study became sedated (Ashford et al 1993). Further investigation revealed that
significant CNS depressant activity appeared when the basic ethers involved were
derived from thymol. Isomers of thymol, namely carvacrol and isothymol, were
relatively inactive. The structural requirements of morphinelike analgesics were
similar to the structure of thymol ether.
REFERENCES
Ashford A, Sharpe C, Stephens F. 1993. Thymol basic ethers and related compounds:
central nervous system depressant action. Nature. 4871(197) 969-971.
Atanassova-Shopova S, Roussinov K, Boycheva I. 1973. On certain central neurotropic
effects of lavender essential oils. II. Communications: studies on the effects of linalol
and of terpineol. Bulletin of the Institute of Physiology. 55:149-156.
Bradsaw R, Marchant J, Meredith M et al. 1998. Effects of lavender straw on stress and
travel sickness in pigs. Journal of Alternative and Complementary Medicine. 4(3)
271-275.
Chapter 10 Insomnia 205

Buchbauer G, Jirovetz L, Jager W. 1991. Aromatherapy: Evidence for sedative effects of
the essential oil of lavender after inhalation. Zeitschrift fur Naturforschung 46
(11⫺12) 1067-1072.
Buchbauer G, Jirovetz L, Jager W. 1992. Kurzmitteilungen: Passiflora and lime-
blossoms—Motility effects after inhalation of the essential oils and of some of the
main constituents in animal experiments. Archiv der Pharmazie (Weinheim). 325(4)
247-248.
Dailey J. 1994. Sedative-hypnotic and anxiolytic drugs. In Craig C, Sitzel R (eds.),
Modern Pharmacology, 4th ed. Boston: Little Brown & Co., 369-377.
Elisabetsky E, de Souza G, Dos Santos M et al. 1995. Sedative properties of linalool. Fi-
toterapia. 66(5) 407-415.
Elisabetsky E, Marschner J, Souza D. 1995a. Effects of linalool on glutamatergic system
in the rat cerebral cortex. Neurochem Res. 20(4) 461-465.
Guillemain J, Rousseau A, Delaveau P. 1989. Effects neurodepresseurs de l’huile essen-
tielle de Lavandula angustifolia. Annales Pharmaceutiques Francaises. 47(6) 337-343.
Henry J, Rusius C, Davies M et al. 1994. Lavender for night sedation of people with de-
mentia. International Journal of Aromatherapy. 6(2) 28-30.
Hudson R. 1996. The value of lavender for rest and activity in the elderly patient. Com-
plementary Therapies in Medicine. 4(1) 52-57.
Jager W, Buchbauer G, Jirovetz L, et al. 1992. Percutaneous absorption of lavender oil
from a massage oil. Journal of the Society of Cosmetic Chemists. 43(1) 49-54.
Jager W, Buchbauer G, Jirovetz L. 1992a. Evidence of the sedative effect of neroli oil,
citronella and phenylethyl acetate on mice. Journal of Essential Oil Research. 4(4)
387-394.
Khanna T, Zaidi F, Dandiya P. 1993. CNS and analgesic studies on Nigella sativa. Fi-
toterapia. 64(5) 407-410.
King P. 2001. An insomnia study using Origanum majorana and Chamomelum nobile. Un-
published dissertation. R J Buckle Associates, Hunter, NY.
Macht D, Ting G. 19211921. Sedative properties of some aromatic drugs and fumes.
Journal of Pharmacology and Experimental Therapeutics. 18:361-372.
Manley K. 1993. Care of the acutely ill. In Hinchcliff S, Norman S, Schober J (eds.),
Nursing Practice and Health Care, 2nd ed. London: Edward Arnold, 1067-1072.
Rovesti P, Columbo E. 1973. Aromatherapy and aerosols. Soap, Perfumery & Cosmetics.
46:475-477.
Sheppard-Hangar S. 1995. Aromatherapy Practitioner Reference Manual, Vol. II.
Tampa, FL: Atlantic School of Aromatherapy.
Tisserand R. 1988. Lavender beats benzodiazepines. International Journal of Aro-
matherapy. 1(1) 1-2.
Weihbrecht L. 1999. A comparative study on the use of Lavandula angustifolia and its
effect on insomnia. Unpublished dissertation. R J Buckle Associates, Hunter, NY.
West B, Brockman S. 1994. The calming power of aromatherapy. Journal of Dementia
Care. March/April, 20-22.
Yamada K, Mimaki Y, Sashida Y et al. 1994. Anticonvulsant effects of inhaling lavender
oil vapor. Biological & Pharmaceutical Bulletin. 17(2) 359-360.
206 Section II Clinical Use of Aromatherapy

W
207
11
Nausea and Vomiting
As aromatic plants bestow
No spicy fragrance while they grow;
But crushed or trodden to the ground,
Diffuse their balmy sweets around.
Oliver Goldsmith
The Captivity, Act 1.
N
ausea and vomiting are symptoms that should be addressed separately,
because nausea does not always lead to actual vomiting. However,
the causes of nausea are similar to those of vomiting. Aromatherapy
has recently been recommended by an internet-based medical consultancy,
www.mdconsult.com, as being useful in nausea related to pregnancy. Vomiting is
activated by the vomiting center in the brain, which triggers nerves supplying the
stomach and chest muscles. Vomiting can have numerous causes.
Gastrointestinal Causes
Gastrointestinal causes of vomiting include the following:
Stomach or intestinal irritation, gastroenteritis
Appendicitis
Obstruction
Hypertrophic pyloric stenosis
Central Nervous System Causes
Central nervous system (CNS) causes of vomiting include the following:
Loss of sense of balance resulting from middle or inner ear trauma, labyrinthitis
Sensory responses in the brain activated by smell, sight, or emotion

Raised pressure in the brain (caused by tumors, hemorrhage, meningitis)
Head injury
Migraine
Psychiatric disorder
Chemoreceptor trigger areas that respond to either chemicals produced by the
body (e.g., kidney and pancreas) or to motion sickness
Metabolic Causes
Metabolic causes of vomiting include the following:
Pregnancy
Uremia
Alcohol
Chemoreceptor trigger areas responding to drugs absorbed by the body (Hope et
al 1993)
Conventional Approaches to Treating Vomiting
There are seven basic categories of antiemetic agents used in conventional medi-
cine: antihistamines, anticholinergics, corticosteroids, cannabinoids, benzodi-
azepines, dopamine antagonists, and serotonin antagonists.
Antihistamines (dramamine, diphenhydramine, hydroxyzine) affect the or-
gan of balance as well as the vomiting center of the brain. These drugs also have
an effect on the chemoreceptor trigger zone (CTZ), and they block the histamine
and dopamine receptors. In addition, they inhibit acetylcholine. Antihistamines
work by reducing the sensitivity of the vomiting center to input from the inner
ear, although they do not directly affect the inner ear.
Because the vomiting center of the brain is stimulated by the neurotransmitter
acetylcholine, one of the most direct ways of inhibiting vomiting is to use anti-
cholinergic drugs (atropine, scopolamine, hyoscyamine). Transdermal scopolamine
provides up to 72 hours of antiemetic treatment. However, long-term use of anti-
cholinergic drugs can cause side effects such as poor digestion, dry mouth, blurred
vision, and constipation. Corticosteroids (dexamethasone, prednisone) can help to
reduce nausea associated with chemotherapy but can cause side effects such as ma-
nia, insomnia, and gastric irritation. Cannabinoids (dronabinol) have been used to
treat nausea and vomiting in patients with end-stage illness, but they have limited
effectiveness resulting from irregular absorption rates. Cannabinoids often take sev-
eral days to weeks to reach therapeutic blood levels and have the side effect of un-
comfortable dizziness or euphoria. Benzodiazepines such as lorazepam have been
used to treat nausea. These drugs often cause dry mouth and drowsiness.
The neurochemical that stimulates the CTZ is dopamine. Dopamine ago-
nists (e.g., prochlorperazine, chlorpromazine, haloperidol) work by blocking
dopamine-mediated transmission, thereby relieving nausea. Dopamine agonists
have common side effects of extrapyramidal symptoms, which limit their use.
208 Section II Clinical Use of Aromatherapy

The new serotonin agonists (e.g., ondansetron) are safe and effective in con-
trolling nausea and are frequently considered first-line antiemetic agents. How-
ever, these drugs are often prohibitively expensive.
Aromatherapy Approaches
Although conventional approaches are often very effective in managing nausea
and vomiting, some patients are intolerant of the drugs’ side effects or are unable
to afford them. In some cases, aromatherapy can be used both as adjunctive ther-
apy and alternative therapy for the control of nausea. Alexander (2001) suggests
that dopamine and serotonin can “cross talk,” and believes that essential oils af-
fect nausea in this manner.
Specific Essential Oils with Antiemetic Properties
Cardamom
Cardamom (Elettaria cardamomum) is listed in the Indian Materia Medica as
checking vomiting and nausea (Nadkarni 1992); it is one of the oldest essential
oils known (Arctander 1994). Tisserand (1989) also suggests it can relieve nau-
sea. Cardamom contains 50% ␣-terpinyl acetate and 1,8-cineole, with small
amounts of borneol, ␣-terpineol, and limonene. Borneol was shown to be an ef-
fective antagonist of acetylcholine in a study by Cabo et al (1986), and perhaps
this compound imbues cardamom with its antiemetic property.
Peppermint
Peppermint (Mentha piperita) has been a classic choice for the treatment of
nausea for hundreds of years. However, too much peppermint can cause nausea,
so only a few drops are needed. Used primarily to treat nausea, rather than actual
vomiting, peppermint has carminative effects both in vitro and in vivo. Pepper-
mint also has recognized antispasmodic effects; in a study of endos-
copy spasm, peppermint was found to relieve colonic spasm within 30 seconds
(Leicester & Hunt 1982).
In another study, patients were given peppermint following colostomies.
Among these patients, 18 of 20 individuals displayed reduced postoperative colic
and nausea (McKensie & Gallacher 1989). Valnet (1980) states that peppermint
is useful for the treatment of nervous vomiting. Franchomme (1980) also states
that peppermint is an antiemetic. Peppermint floral water is one of the active in-
gredients of babies’ gripe water, a traditional remedy recommended by hospitals
in the United Kingdom.
The effect of peppermint was audited in a study with 10 patients at the on-
cology center of St. Luke’s Hospital in New Bedford, Massachusetts, and found
to be effective in reducing the nausea of patients undergoing chemotherapy when
used instead of the drugs Zofran and Compazine (Figuenick 1998). Zofran is
very expensive. Peppermint proved so effective that those in the control group
Chapter 11 Nausea and Vomiting 209

demanded the peppermint, and the control part of the study collapsed! Of pa-
tients in this study, 84% stated that essential oil of peppermint relieved their nau-
sea, and 71% found it enhanced their standard antiemetic medication. One pa-
tient found it enhanced the ability to eat. Aromatherapy is now routinely offered
in many chemotherapy units in the United States and United Kingdom.
Tate (1997) carried out a controlled study of postoperative nausea on 18 pa-
tients who underwent major gynecologic surgery. Group 1 received no treatment,
group 2 received peppermint essence, and group 3 received peppermint essential
oil. Participants in group 3 were asked to inhale directly from the bottle when
they were nauseated. Measurement was made on a five-point scale ranging from
0 (no nausea) to 4 (about to vomit). The amount of antiemetic drugs (metoclo-
pramide [Maxolon], prochlorperazine [Stemetil], and ondansetron [Zofran])
used was measured. Participants in the experimental group needed 50% fewer
antiemetics. The Kruskal-Wallis test was used to establish significance, P ⫽
0.0487. The cost per treatment was approximately 75 cents (48 pence).
Spearmint is thought to also have an antiemetic effect and, according to
Lawrence (2001), may prove effective for longer periods than peppermint. Several
US hospitals are conducting clinical trials on peppermint and spearmint as this text
is being written.
Ginger
Ginger (Zingiber officinale) was introduced in Europe during the Middle
Ages. The essential oil, which does not smell anything like the dried root or can-
died ginger, contains zingiberene. In China, ginger root is classically given to new
mothers following the birth of their children. Although it is often used topically
in the treatment of chronic pain, inhaled essential oil of ginger is a very effective
remedy for nausea and is particularly suitable for pregnancy. Vutyavanich et al
(1997) studied 70 expectant mothers over a period of 5 months in a double-
masked, placebo-controlled trial. They found baseline nausea and vomiting de-
creased significantly in the group using ginger. Ginger had no adverse effects on
the mothers’ pregnancy outcomes. However, ginger may not be as effective for
nausea associated with CNS disturbances. Visalyaputra et al (1998) found that
2 gr ginger powder taken orally was ineffective at reducing the incidence of post-
operative nausea and vomiting the day after gynecologic laparoscopy. This could
be because many people find it difficult to take anything orally when nauseated.
Lavender
Everson (2000) carried out a small project with lavandin (Lavandula inter-
media CT Super) to treat postoperative nausea. She became intrigued with the
antiemetic properties of lavender while undergoing chemotherapy herself. Dur-
ing the 26 weeks Everson received chemotherapy, she never vomited and only
used six of the prescribed antiemetic pills. All of the women in her cancer sup-
port group were nauseated, and all used most of their antiemetic pills. Ten pa-
tients were included in the exploratory postoperative study, which was not ran-
210 Section II Clinical Use of Aromatherapy

domized or controlled. Consent was given by the hospital and each patient signed
an informed consent. After inhaling lavender, only two patients required an
antiemetic postoperatively, a much lower than usual incidence. Although no con-
clusions can be reached from this study, this chemotype of lavandin might be
worth pursuing for treatment of postoperative nausea alongside spearmint, pep-
permint, cardamom, and ginger.
Clove (Eugenia caryophyllata) is listed in Potter’s New Cyclopaedia of Botanical
Drugs and Preparations as an antiemetic (Wren 1988). Pharmacognosy books
suggest that cardamom, which has an antispasmodic action on the gastrointesti-
nal tract, and peppermint are both suitable as carminatives (Evans 1994). Fennel
(Foeniculum vulgare) and aniseed (Anethum graveolens) are also mentioned, but
more as carminatives than as antinausea essential oils.
Other Anticholinergic Essential Oils
In a study investigating the activity of major components of various essential oils
of aromatic plants from Granada, borneol and myrcene were found to be active
against acetylcholine. In this instance, borneol and myrcene were from essential
oils of thyme (Thymus granatensis) and Spanish sage (Salvia lavendulaefolia). The
experiment was carried out with isolated duodenum. However, if borneol and
myrcene do display anticholinergic activity, it would be logical to try other essen-
tial oils that contain these compounds to provide relief from nausea and to inhibit
vomiting. Myrcene and borneol are found in many essential oils. Gas chromatog-
raphy linked to mass spectrometry indicates how much myrcene or borneol is
present in an essential oil.
Importance of Individual Preference in Choice of Essential Oil
Several of my students have completed case studies on nausea using ginger and
peppermint and found that patients tended to prefer one essential oil over an-
other. The essential oil patients preferred was more effective against their nausea
than one they did not like. This highlights the importance of learned memory and
of involving patients in choosing their oils. The method of choice is usually in-
halation. However, a gentle abdominal rub can be very beneficial to a child or
anxious patient who is sick with worry, rather than nauseated for physical reasons.
REFERENCES
Alexander M. 2001. How Aromatherapy Works, Vol 1. Odessa, FL: Whole Spectrum
Books.
Arctander S. 1994. Perfume and Flavor Materials of Natural Origin. Carol Stream, IL:
Allured Publishing.
Cabo J, Crespo M, Jimenez J et al. 1986. The spasmolytic activity of various aromatic
plants from the province of Granada. The activity of the major components of their
essential oils. Plantes Medicinales et Phytotherapie. 20(3) 213-218.
Evans W. 1994. Trease & Evan’s Pharmacognosy, 13th ed. London: Bailliere Tindall.
Chapter 11 Nausea and Vomiting 211

Everson C. 2000. Lavandula intermedia (DT Super) as a post-operative anti-emetic. Un-
published dissertation. R J Buckle Associates, Hunter, NY.
Figuenick R. 1998. Essential oil of peppermint: A 3-part audit on nausea. Unpublished
dissertation. R J Buckle Associates, Hunter, NY.
Franchomme P, Penoel D. 1980. L’aromatherapie Exactement. Jollois, Limoge, France.
Hope R, Longmore J, Hodgetts T et al. 1993. Oxford Handbook of Clinical Medicine,
3rd ed. Oxford, UK: Oxford University Press.
Leicester R, Hunt R. 1982. Peppermint oil to reduce colonic spasm during endoscopy.
Lancet. 2(8305) 989-990.
Lawrence B•. 2001. Personal communication in September 2001.
McKenzie J, Gallacher M. 1989. A sweet-smelling success: Use of peppermint oil in
helping patients accept their colostomies. Nursing Times. 85(27) 48-49.
Nadkarni K. 1992. Indian Materia Medica, Vol. 1. Prakashan, India: Bombay Popular.
Tate S. 1997. Peppermint oil: A treatment for postoperative nausea. Journal of Advanced
Nursing. 26(3) 543-549.
Tisserand R. 1989. The Art of Aromatherapy. Saffron Walden, UK: CW Daniels.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Visalyaputra S, Petcchpaisit N, Somcharoen K et al. 1998. The efficacy of ginger root in
the prevention of postoperative nausea and vomiting after outpatient gynaecological
laparoscopy. Anaesthesia. 53(5) 506-510.
Vutyavanich T, Kraisarin T, Ruangsri R. 1997. Ginger for nausea and vomiting in preg-
nancy: randomized, double-masked, placebo controlled trial. Obstetrics and Gynecol-
ogy. 97(4) 577-582.
Wren R. 1988. Potter’s New Cyclopaedia of Botanical Drugs and Preparations. London:
Churchill Livingstone.
212 Section II Clinical Use of Aromatherapy

W
213
12
Pain and Inflammation
How did the rose ever open its heart and give to this world all its beauty?
It felt the encouragement of light against its being,
otherwise we all remain too frightened.
Hafiz
The Gift
Pain
Pain is an unpleasant sensation localized to part of the body (Fields 1997). Al-
though there are physical dimensions that reflect a commonality of pain in hu-
mans, the experience of pain is unique to the individual. People who live with
pain on a daily basis have what is to them a clear way of describing what they feel.
If the pain changes, they know it. However, describing pain to someone who does
not experience it is very subjective and can be problematic. Descriptions of pain
vary greatly. Apart from the site of the pain (for example, abdominal), one of the
most important aspects to consider is the onset of pain. The onset clarifies which
kind of pain is involved: acute or chronic.
Chronic pain costs the United States approximately $70 billion per year and
affects approximately 80 million Americans (Berman & Swyers 1997). Pain is one
of the most commonly addressed symptoms in a clinical setting.
Physiology of Pain
Pain is a complex neurophysiological phenomenon (Alavi et al 1997) and can be de-
scribed as somatic, neuropathic, or visceral. Somatic pain is well localized, persistent,
and is often described as sharp or stabbing. Neuropathic pain is usually described as
burning, numbing, or shooting and originates from compression or stimulation of a

nerve. Visceral pain tends to be poorly localized, dull, and aching and involves an A-
C fiber ratio of 1:10 in visceral afferents. In normal adults the ability to detect pain
is completely removed when A and C axons are blocked (Fields 1997). When pain
triggers the nociceptors (pain receptors), it is translated or transduced into electrical
activity. The electrical impulse is then transmitted to the spinal cord via the dorsal
root and relayed to the thalamus via the afferent pathways.
Pain is often divided into acute and chronic. Acute pain is short lasting and
has a well-defined pattern of onset. Chronic pain persists beyond the expected pe-
riod of healing (Casey 2002) and is associated with a degenerative or chronic
pathological process such as arthritis. However, sometimes the cause of the pain
is elusive.
The thalamus is involved in pain perception and interpretation (Alavi et al
1997) and is, of course, part of the limbic system, which analyzes smell; therefore
there is an implicit suggestion that smell may affect the perception of pain. Pri-
mary afferent nociceptors activate spinal pain-transmission cells through two
neurotransmitters: glutamate (an amine) and substance P (a peptide) that are
present in C fibers (Fields 1997). Greer (1995) noted substance P immunoreac-
tive processes throughout the laminae of the olfactory bulb. A variety of chemi-
cal agents can activate the primary afferent nociceptors. These include serotonin
and potassium. If the tissue is damaged or inflamed, the sensitivity of the noci-
ceptors is heightened. The whole process results in a subjective, sensory, and emo-
tional experience of pain.
Visceral pain is usually blocked by opioids (Sofaer & Foord 1993). Actually,
the body itself produces enkephalin, an opioid-like peptide that occurs in two
forms, Met-enkephalin and Leu-enkephalin.
Etiology of Pain
There are many possible causes of pain: a simple headache can have a dozen pre-
disposing factors including low blood sugar, hormonal imbalance, or a brain tu-
mor. Pain is an emotional issue because it is so intensely personal. Pain is closely
linked to feelings. Pain sufferers frequently feel guilty or that somehow they
should be able to bear their pain better, and many patients with chronic pain talk
of feeling helpless or vulnerable. Goleman (1996) writes “humanity is most evi-
dent in our feelings.” Feelings such as despair and anxiety are known to heighten
pain, and pleasure and relaxation appear to decrease pain. It is difficult to relax
and feel pleasure unaided when in pain, and it is all too easy to feel despair and
anxiety. Changing perception of pain can be difficult when tackled alone.
Orthodox Approach to Pain
In January 2001, the Joint Commission on Accreditation of Healthcare Organiza-
tions ( JCAHO), which accredits the majority of the United States’ medical facili-
ties, developed a new mandatory standard for the assessment and treatment of pain.
It was the first time JCAHO, or any other accrediting body, had issued standards
focusing on pain. Institutions began to scramble to work out how they were going
214 Section II Clinical Use of Aromatherapy

to meet the new standards and what they needed to do to deal properly with a pa-
tient in pain. As part of the standards, medical institutions are required to inform
patients of their right to appropriate pain assessment and treatment. The assess-
ment includes documenting the level and characteristics of each person’s pain using
a numeric scale of 0-10 or pictures of expressive faces (www.JCAHO.org). No pa-
tient should score his or her pain above a four. Institutions are required to develop
protocols for pain management and to educate their staff on pain management.
Orthodox Pain Relief
Analgesics (pain relievers) are divided into opioids (narcotics) and nonopioids.
The use of opioids is strictly controlled. Originally narcotics were opioid deriva-
tives and came from the plant Papaver somniferum. Recent advances in pharma-
cology have resulted in the development of several synthetic analgesics that work
on the opioid receptors in the brain.
Narcotic/Opioid Drugs
Morphine is possibly the most common analgesic in this category. Derived
from the opium poppy, morphine works by depressing the cerebral cortex, resulting
in reduced powers of concentration as well as reduced pain. However, the respira-
tory and cough centers are also depressed by morphine, as is the neurotransmitter
acetylcholine. Cananga odorata var. genuina (ylang ylang) has mild, opioid-like
properties and can sometimes enhance the effect of opioid drugs. Codeine is a com-
mon but milder narcotic also derived from the opium poppy (Martin 1994).
Codeine is used to suppress dry coughs as well as for the relief of general pain. Mor-
phine, codeine, and opioid-like drugs are addictive, although they are less likely to
be addictive for someone in severe or chronic pain. Such a patient’s chances of ad-
diction then fall to 1 in 3000 (Carter 1996). Another side effect of opioids is con-
stipation. Narcotics have an extremely important role to play in health care.
Common Nonopioid/Nonnarcotic Drugs
The two most important drugs in this category are aspirin and acetamin-
ophen. Aspirin (acetylsalicylic acid), as well as having antiinflammatory effects, is
a well-recognized analgesic. Originally this analgesic was derived from salacin, a
glycoside found in willow tree bark. Aspirin blocks prostaglandin synthesis in the
central nervous system (CNS) and peripheral nervous system. Acetaminophen
(Tylenol) is a painkiller that has no antiinflammatory effects because it blocks
prostaglandin synthesis only in the CNS (Parish 1991). A list of undesirable side
effects of antiinflammatory drugs can be found in many textbooks (Goodman-
Gilma et al 1985). They are outlined in the following sections and are divided into
the two main categories: nonsteroidal and steroidal.
Nonsteroidal Antiinflammatory Drugs
Aspirin is the most common nonsteroidal antiinflammatory drug (NSAID)
and has a long history of use. Yin et al (1998) found aspirin inhibited transcrip-
Chapter 12 Pain and Inflammation 215

tion factors that coded the production of prostaglandin sythase enzymes. Lyss et
al (1997) discovered helenalin, a lactone found in arnica, also inhibits the same
transcription factor but in a different way. However, blocking prostaglandin syn-
thesis can give rise to specific side effects. All NSAIDs, including aspirin (sali-
cylic acid)-based antiinflammatories, can increase gastric bleeding in patients
with gastric ulcers due to the inhibition of prostaglandin PGE2, which suppresses
gastric acid secretion. NSAIDs can also prolong bleeding as they inhibit produc-
tion of thromboxane (Ward 1993), upset the fluid balance by decreasing excretion
due to inhibition of renal blood flow, cause bronchospasm and nasal polyposis in
susceptible individuals, and delay the onset of labor due to loss of contractile ef-
fects of prostaglandins on the uterine muscles (Kvam 1994). Indomethacin is of-
ten used when salicylates are not tolerated. However, in arthritic patients, in-
domethacin can lead to a high incidence of CNS effects if the dose is high.
Phenylbutazone-like drugs can also cause gastrointestinal irritation, hepati-
tis, vertigo, and headaches. With prolonged usage, they can also depress the bone
marrow, leading to leukemia and aplastic anemia (Craig & Stitzel 1994).
Steroid-Based Antiinflammatory Drugs
Despite being superior in effect to NSAIDs (and affecting the inflammatory
process at each level), steroidal antiinflammatory drugs have many side effects.
These include hyperglycemia leading to diabetes, myopathy, increased intraocular
pressure with the potential for glaucoma, electrolyte imbalance leading to hyper-
tension, thinning of the skin with an increased tendency for poor healing and skin
breakdown, hirsutism, insomnia, depression, and psychosis (Craig & Stitzel
1994). These drugs are usually avoided in long-term treatment. However,
steroidal antiinflammatory drugs have provided relief for chronic inflammatory
conditions and will continue to be used until other drugs with fewer side effects
are found.
Disadvantages of Orthodox Treatments
Despite advances in pain medication, many patients suffer chronic, and some-
times severe, pain before they die. Articles published in the New England Journal
of Medicine and the Journal of the American Medical Association disclosed that chil-
dren as well as adults suffered unnecessarily from pain. Carter (1996) suggests the
poor pain-control in the studies could be because narcotics are often so tightly
controlled in hospitals that staff cannot get them when their patients most need
them. He suggests patient-controlled analgesia as the answer.
The barriers to pain management are patients’ fear of addiction and their re-
luctance to report pain, plus their concerns about the side effects of medication
and their fear their pain will not be controlled. These barriers have been com-
pounded by inadequate reimbursement, poor administrative support, the high
cost of technology, lack of continuity of care, and the lack of accountability for
poor pain management. Muddying the whole issue of pain control are drug con-
216 Section II Clinical Use of Aromatherapy

troversies such as that surrounding Oxycontin: a drug as potent as morphine that
was heavily marketed to physicians without warning them of its addictive poten-
tial, which has had devastating consequences (Meier & Petersen 2001). However,
things are changing for the better. As of January 2, 2002, pain management was
recognized and reimbursed by Medicare, along with nutrition therapy (Pear
2002), and it is hoped that many health-insurance companies will follow suit.
Chronic Pain Syndrome
Chronic pain syndrome has been described as a complex dysfunction and is ex-
tremely difficult to treat successfully. Allopathic medicine treats CPS with a mix-
ture of opioid and nonopioid drugs backed with tricyclic or Valium-type drugs
that are not antidepressants, although they are used for that purpose in this
instance.
Aromatherapy in Chronic Pain Management
Touch, relaxation, and pleasure each play an important part in how individuals
perceives the world around them, and how they feel about themselves. This in-
cludes the perception of pain (Beck & Beck 1987). Aromatherapy works on the
sensory system and appears to enhance the parasympathetic response, which is
closely linked with endorphins (Weil 1996). The intensity and depth of pain is
influenced by external factors such as previous experience, attitude, and culture.
Pain can be “put on hold” by strong emotions such as anger, fear, or elation. Con-
versely, fear can make pain feel worse. Pain is a warning system. By deadening it,
the warning system is dulled. A headache pill does not make the cause of the
headache go away; it just allows the person to carry on functioning.
Aromatherapy using touch is very gentle and can be helpful in alleviating
chronic pain. An application of diluted essential oils with either massage or se-
quenced movements (the “m” technique) is very relaxing. The odor of the essential
oils is pleasurable. Even ignoring the possibility that essential oils might have phar-
macologically active components or the possible pharmacokinetic enhancement of
orthodox drugs by essential oils, there is still a potential role for aromatherapy as part
of an integrated, multidisciplinary approach to pain management.
Aromatherapy enhances the parasympathetic response through the effects of
touch and smell, encouraging relaxation at a deep level. Relaxation has been
shown to alter perceptions of pain. Aromatherapy also enables patients to get “in
touch with” feelings of relaxation and pleasure through smell and touch. These al-
low patients to “let go,” often for the first time. A compress or gentle massage can
draw attention either to the site of the pain, or away from it, depending on what
will most meet the patient’s psychological needs. Diffusing a relaxing essential oil
can alter perceptions of pain (Buckle 1999).
The analgesic effects of aromatherapy can be traced to several factors:
1. A complex mixture of volatile chemicals reaching the pleasure memory sites
within the brain;
Chapter 12 Pain and Inflammation 217

2. Certain analgesic components within the essential oil, which may or may not
be known, affecting the neurotransmitters dopamine, serotonin, and nora-
drenaline at receptor sites in the brain;
3 The interaction of touch with sensory fibers in the skin, which could possibly
affect the transmission of referred pain;
4. The rubefacient effect of baths or friction on the skin.
Two thousand years ago, man used the plants Salix (willow) and Populus
(poplar) to alleviate pain (Lewis & Elvin-Lewis 1977). Gattefosse (1937) states
“almost all essential oils have analgesic properties,” but some are more effective
than others. Tables 12-1 and 12-2 list essential oils that are particularly suited to
the treatment of chronic pain.
218 Section II Clinical Use of Aromatherapy
Table 12-1 h Essential Oils Suitable for Chronic Pain
Common Name Botanical Name Application
Black pepper Piper nigrum Topical
Clove bud
a, b
Syzygium aromaticum Topical
Frankincense Boswellia carteri Inhaled, topical
Ginger
c
Zingiber officinale Topical
Juniper Juniperus communis Topical
Lavender (Spike)
d
Lavandula latifolia Topical
Lavender (True ) Lavandula angustifolia Inhaled, topical
Lemongrass
e
Cymbopogon citrates Inhaled, topical
Marjoram (Sweet) Origanum majorana Inhaled, topical
Myrrh Commiphora molmol Topical
Peppermint Mentha piperita Topical
Rose Rosa damascene Topical
Rosemary
f
Rosmarinus officinalis Inhaled, topical
Verbena Aloysia triphylla Inhaled, topical
Ylang ylang Cananga odorata Inhaled
a Clove bud is safer than clove leaf. Phenols can be harsh on the skin.
b Best avoid regular use of clove with patients on anticoagulant therapy.
c The CO
2
extraction contains gingerol thought to have analgesic action.
d Spike lavender can be a stimulant; best avoid regular use in hypertension.
e Lemongrass contains aldehydes; avoid in high concentrations on sensitive skin.
f Rosemary is a stimulant; best avoid regular use in hypertension or epilepsy.

Animal Studies
Lorenzetti et al (1991) found myrcene, a terpene found in up to 20% in
lemongrass (Cymbopogon citratus), had a direct analgesic effect on rats. The effect
lasted 3 hours and was similar to that of peripheral-acting opioids, but did not af-
fect the CNS, which was remarkable as the essential oil was administered orally.
The analgesic effects did not lead to tolerance during a period of 5 days (which
would have occurred with a narcotic). This is interesting as Seth et al (1976) had
previously investigated the effect of lemongrass on pain and found it enhanced
the effect of morphine in rats. However, Seth also investigated Cymbopogon nar-
dus (East Indian lemongrass) and found it to be less effective as an analgesic.
Cymbopogon nardus contains considerably less myrcene than Cymbopogon citratus
(Boelens 1994). Lorenzetti et al (1991) conclude their paper with the suggestion
that terpenes should be investigated with the “possibility of developing a new
class of analgesic with myrcene as the prototype.” Myrcene is found in small
amounts in a number of essential oils, including rosemary, frankincense, juniper,
rose, ginger, and verbena (Sheppard-Hangar 1995), all of which have traditional
analgesic qualities. The analgesic effects of lemongrass in mice was the subject of
another paper by Viana et al (2000) who concluded the essential oil worked at
both central and peripheral levels when given by oral and intraperitoneal routes.
Artemisia caerulescens was found to have an analgesic effect on rats in a study by
Moran et al (1989). Nepetalactone, a lactone found in Nepeta caesarea, was found to
have analgesic properties in a controlled, comparative study with morphine on mice
and hailed the “new opioid” (Aydin et al 1998). The essential oil was given by in-
traperitoneal injection. The lactone appeared to affect mechanical, not thermal, al-
gesic receptors, which “suggests specificity for specific opioid receptor subtypes ex-
cluding mu-opioid receptors.” Because the lactone is the main component of Nepeta
caesarea (92%-95%) it was thought to have specific, opioid-receptor-subtype ago-
nistic activity. The essential oil also had marked sedative effects. Aydin et al (1996)
had previously studied Origanum onites and found it too had analgesic activity.
Chapter 12 Pain and Inflammation 219
Table 12-2 h Essential Oils Particularly Suitable for Children
Common Name Botanical Name Application
Chamomile (Roman) Chamaemelum nobile Inhaled, topical
Geranium Pelargonium graveolens Inhaled, topical
Mandarin Citrus reticulate Inhaled, topical
Neroli Citrus aurantium Inhaled, topical
Palma rosa Cymbopogon martini var. motia Inhaled, topical
Sandalwood Santalum album Inhaled, topical
Inhaled: 2 drops on cotton ball inhaled for 5-10 minutes
Topical: 2-5 drops diluted in a compress or in a vegetable cream/gel/oil

Lavandula angustifolia was found to have a local anesthetic effect in rabbits
by Ghelardini et al (1999).
Human Studies
The analgesic effect of essential oils also occurred in human studies as re-
ported by Woolfson and Hewitt (1992) who found a 50% pain reduction in 100
patients nursed in a critical care unit. Thirty-six patients were randomly allocated
into three groups of 12: one group received massage plus lavender, one group re-
ceived massage without lavender, and a control group received no massage but
were left to “rest curtained off ” from the remainder of the unit. Treatment con-
sisted of 20 minutes of foot massage twice a week for 5 weeks. This was an in-
teresting study as 50% of the patients were artificially ventilated, and therefore the
effects of the essential oil could not be from inhalation. The most striking differ-
ence between the group receiving massage with lavender (Group A) and without
lavender (Group B) was in the effect upon heart rate. Ninety percent of Group A
showed a reduction of between 11 and 15 beats per minute whereas only 58% of
Group B showed any reduction, and it was consistently less. Only 41% of the con-
trol group showed any reduction. The study gives no formal statistics or analysis.
Wilkinson (1995) investigated the effects of 1% Roman chamomile (Chamo-
melum nobile) on 51 patients with cancer in a randomized study. The participants
ranged in age from 26 to 84 years. Ninety-four percent of the participants were fe-
male, and 6% were male. Forty-one percent had been referred for pain control.
During the study, 45% of the participants were receiving morphine, with the re-
mainder on weak opioids, nonopioids, or nothing. Seventy-six percent of the par-
ticipants had metastases. Mann-Whitney U tests on all independent variables re-
vealed no significant differences between conditions in the pretest scores for the
Rotterdam Symptom Checklist on physical or psychological symptoms, activities,
and top 10 symptoms. The data were analyzed using the Statistical Package for the
Social Sciences (Nie et al 1975) and nonparametric tests were employed for all sta-
tistical analysis. State Trait Anxiety Inventory (STAI) scores fell by an average of
16 points in the aromatherapy massage group but only 10 points in the plain mas-
sage or standard group (p 0.005), and pain was reduced statistically (p 0.003).
One patient is quoted as saying “I know now, almost definitely, that it (aro-
matherapy) has helped me in my quest for pain relief. I have told Dr. R at the pain
clinic how pain free I was while having regular (aromatherapy) treatment”
(Wilkinson 1995).
Gobel et al (1991) studied the effect of peppermint on headaches. Pain was
induced in healthy humans using pressure, thermal, and ischemic stimuli. The in-
tensity of the pain, neurophysiology, performance-related activity, and mood
states were monitored. Peppermint diluted in ethanol and applied topically pro-
duced a significant analgesic effect. Perez-Raya et al (1990) found Mentha rotun-
difolia and Mentha longifolia (both types of peppermint) had analgesic properties
in mice and rats. Peana et al (1999) found essential oil of clary sage to have an an-
tiinflammatory and analgesic action at a local level. Extracts of myrrh (Com-
220 Section II Clinical Use of Aromatherapy

miphora momol) were found to have a strong local anesthetic effect in a study by
Dolara et al (2000). The anesthetic action blocked the sodium current of excitable
mammalian membranes. Local anesthetic activity on nerve cells was measured by
incubating hippocampal brain slices, freshly dissected with a tissue chopper, from
the brain of one of the experimental male rats. The slices were stimulated with a
positive electrical current applied though electrodes.
Krall and Krause (1993) conducted an open, randomized study of 100 patients
to evaluate the effects of a topically applied gel containing peppermint oil (30%) on
periarticular pain. Effects of the peppermint gel were measured in acute (n 49) and
subacute (n 51) conditions compared to the standard treatment of 10% hydrox-
yethyl salicylate gel. Different aspects of pain (intensity on pressure and spontaneous
and movement pain) were examined using visual analog scales (0 no symptom to
100 severe symptom) for a period of 20 days. No statistical details were given. In
78% of cases both the physician and patient considered the results with the mint
therapy to be highly effective, as opposed to 50% and 34 % respectively with the
standard gel. There were 10 instances of side effects from the hydroxyethyl salicylate
gel (three of erythema and seven of itching) and only one (smell of peppermint in
the nose) from the mint oil. At the end of the study, 19% of the mint-oil patients
were still suffering from pain, as were 36% of the aspirin gel group. The results of
this comparative study were dependent on the severity of the symptoms.
Hot-pepper cream containing capsaicin has been found useful for arthritis
and shingles and also appears to relieve postsurgical pain in cancer patients. Pa-
tients who used a cream containing 0.075% capsaicin around the incision site for
8 weeks following surgery experienced a 53% reduction in pain, compared with a
17% reduction for those using a placebo cream. Side effects included redness and
burning of the skin, but those effects diminished with time. Capsaicin also ap-
pears to inhibit substance P.
Ginger (Zingiber officinale) can also have an analgesic and deeply warming
action, but the topical analgesic gingerol (a phenol) only occurs in the CO
2
ex-
tract, not in the essential oil (Wren 1988). Oleum spica was traditionally used as a
topical analgesic. Oleum spica contains one part spike lavender to four parts tur-
pentine. It is thought the analgesic effect of turpentine is enhanced by the pres-
ence of spike lavender (Von Frohilche 1968).
Benzoin, camphor, clove, coriander, ginger, hops, lemongrass, marjoram,
black pepper, pine, savory, and ylang ylang have analgesic properties (Rose 1992).
Other suggestions include white birch, chamomile, frankincense, wintergreen,
clove, lavender, and mint. Lawless (1994) writes that during the pre-Christian
era, myrrh was added to wine to provide pain relief to those about to be crucified.
Myrrh contains terpenes, esters, and a phenol called eugenol, all of which are re-
puted to be analgesics (Franchomme & Penoel 1991). Eugenol (and myrcene) are
found in West Indian Bay (Pimenta racemosa) and in clove (Syzygium aromaticum).
Use clove-bud oil (which also contains esters) not the leaf or stem oil that is
higher in phenols. Diluted clove oil is useful to use prior to venipuncture as it
make the veins more prominent and gives some local-anesthetic effect. Borneol
Chapter 12 Pain and Inflammation 221

(an alcohol) and myrcene (a terpene) were found to be effective antagonists of
acetylcholine in a study by Cabo et al (1986). This study was conducted on iso-
lated duodenum to counter contractile tissue. Acetylcholine is a central and pe-
ripheral nervous system transmitter (Craig 1994).
Muscle Spasm and Pain
Some pain is caused by muscle spasm. Several essential oils have antispasmodic
effects, particularly those high in esters. The greater the number of different es-
ters in an essential oil, the greater is thought to be the antispasmodic effect. Ro-
man chamomile has more esters than any other essential oil and is also a recog-
nized analgesic (Wren 1988). Lis-Balchin (1997) found clary sage, dill, fennel,
frankincense, nutmeg, and lavender reduced the “twitch response to nerve stimu-
lation; in isolated rat tissue.” Historically the essential oils listed in Table 12-3
have been used for their antispasmodic effect.
Enteric-coated peppermint-oil capsules were used in the treatment of irrita-
ble bowel syndrome symptoms (Kline et al 2001). Fifty children took part in the
controlled, multicentered study. The gelatin capsules did not release the oil until
they were in the small intestine (an environment of pH 6.8 or higher). Between
one capsule (187 mg) and two capsules were given three times a day. During the
study eight children withdrew for various reasons. However, 76% of the pepper-
mint group showed significant reduction in symptoms compared to the placebo
group (43%). No side effects were reported and no change in stool consistency.
Inflammation
Sometimes pain is caused by inflammation. Inflammation is a fundamentally pro-
tective mechanism (Betts 1993) and has been called “the most important of the
222 Section II Clinical Use of Aromatherapy
Table 12-3 h Some Antispasmodic Essential Oils
Common Name Botanical Name Reference
Roman chamomile Chamaemelum nobile Franchomme & Penoel 1991
Petitgrain Citrus amara Reiter & Brandt 1985
Dill Anethum graveolens Lis-Balchin 1997
Clary sage Salvia sclarea Lis-Balchin 1997
Fennel Foeniculum vulgare Lis-Balchin 1997
Frankincense Boswellia carteri Lis-Balchin 1997
Lavender Lavandula angustifolia Lis-Balchin 1997
Sage Salvia officinalis Taddei et al 1988;
Giachetti et al 1988

body’s defense mechanisms” (MacSween & Whaley 1992). Derived from the
Latin inflammare, meaning “to burn,” the function of inflammation is to restore the
body to normal functioning as quickly as possible. The symptoms of inflammation
are redness, swelling, heat, and pain—through history listed as rubor, tumor, calor,
and dolor (Mills 1991)— and a loss of function (Craig & Stitzel 1994).
Antiinflammatory Essential Oils
Essential oils have some of their most poignant antiinflammatory effects on the
dermis and epidermis (Bowles 2000). Mascolo et al (1987) screened 75 species of
plants (chosen from medicinal folklore) and their extracts for antiinflammatory
activity. The experiments were performed on rats with carrageenan-induced foot
edema. The control drug was indomethacin. Herbal extracts (not essential oils)
from the plants were administered orally. However, many of the plants selected
also produce essential oils used for antiinflammatory purposes in aromatherapy.
Coriandrum sativum (coriander), Foeniculum vulgare (fennel), and Juniperus com-
munis (juniper) all produced 45% reduction of inflammation, comparable with the
control. However, if the essential oils had been applied topically, the response
might have been greater. Essential oils are absorbed through the skin, with 70%
of the oil being absorbed within 24 hours (Bronaugh et al 1990).
Rossi et al (1988) investigated Roman chamomile (Anthemis nobilis) in a
comparative, controlled study on rats with carrageenan-induced edema. The con-
trol was indomethacin. Three essential oils of chamomile were used. White-
headed, double-flowered chamomile flowers showed a greater antiinflammatory
action than the yellow-flowered variety. Nevertheless, all three essential oils of
Roman chamomile produced significant antiinflammatory effects. In this study
the chamomile was given subcutaneously into the peritoneal cavity. Jakovlev et al
(1979) demonstrated the antiinflammatory effect of German chamomile and sug-
gested the antiphlogistic effects were due to bisabolol and bisabolol oxides.
Tubaro et al (1984) found when German chamomile (Matricaria recutita) was ap-
plied topically to mouse ears, with hydrocortisone as the control, the chamomile
showed an antiinflammatory action, although the effect was only half as strong as
that of the steroid.
Nutmeg (Myristica fragrans) may have been the inspiration for Nostradamus’
prophecies, but it also has antiinflammatory activities. Benet et al (1988), attrib-
uted nutmeg’s antiinflammatory action to eugenol. They found the greatest effect
was observed after 4 hours and was comparable to the effects of phenylbutazone
and indomethacin. However, most essential oils of nutmeg contain very small
amounts of eugenol (Lawrence 1995).
Wagner et al (1986) screened various essential oils traditionally used for their
antiinflammatory action. They concluded eugenol, eugenyl acetate, thymol, cap-
saicin, curcumin, and carvacrol were present in most of the essential oils screened,
and the antiphlogistic effects were closely linked to the vascular reaction of early
inflammation. In herbal medicine this is called the counterirritant effect. Clove
and cinnamon had the strongest effect, Dwarf pine (Pinus mugo var. pumilo) and
Chapter 12 Pain and Inflammation 223

eucalyptus (Eucalyptus globulus) had a mild effect and Chamomelum nobile had a
weak antiinflammatory effect.
Where there is topical inflammation, essential oils should be applied topi-
cally. Essential oils are absorbed into and through the skin, and they can en-
hance the penetration of other medication. Godwin and Michniak (1999) found
terpenen-4-ol and a-terpineol enhanced the penetration of a hydrocortisome
cream on mouse skin by between three and five times. Sesquiterpenenes and
sesquiterpenoids (found in many antiinflammatory essential oils) caused a 20%
increase in penetration of 5-fluorouracil, and this effect lasts for 4 days (Cornwall
& Barry 1994).
Sometimes, in cases of arthritic pain, heat can help. If this is the case, essen-
tial oils that have rubefacient effects, such as Piper nigrum (black pepper), Syzy-
gium aromaticum (clove), or Zingiber officinale (ginger) can be useful, as CO
2
ex-
tracts. Sometimes cooling will help and an essential oil like Mentha piperita
(peppermint) can be added to the topical-application mix.
It is important patients be allowed to smell the mixture before it is applied;
they will have to live with it, after all! Be gentle and slow. Allowing someone to
touch a painful area takes courage, and that courage needs to be rewarded with
respect. All the essential oils mentioned are safe to use for relief of pain. While a
1-5% solution is usually adequate, much higher concentrations can be used. In
some circumstances, and depending on the essential oils selected, 100% solutions
can be used. Lavender and tea tree are good examples of oils that can be used at
full strength.
Plant flavonoids have measurable effects on the CNS (Paladini et al 1999).
Some semisynthetic derivatives of plant favonoids were found to have an anxi-
olytic effect 30 times that of diazepam. Both natural and synthetic flavonoids
are a part of Western living and are ingested by millions of people on a daily
basis.
Finally, the pain experienced by patients with sickle cell anemia, an inherited
disease, may be helped with herbal medicine. Fakim and Sewaj (1992) found an
aqueous extract of Pelargonium graveolens (geranium) successfully reverted sickled
cells in vitro. Fennel has also been shown to reverse sickling (Fakim et al 1990).
The extract used was aqueous, and therefore not found in the essential oil, but
there could be a similar response using the CO
2
extract.
There is no suggestion that essential oils should replace conventional analge-
sia. However, topical or inhaled, applications of essential oils appears to enhance
orthodox analgesia either through the placebo response, the effect of touch and
smell on the parasympathetic nervous system, or because of pharmacologically ac-
tive ingredients within the essential oils that may have an analgesic effect. There
have been few published clinical trials, but there is growing anecdotal evidence to
suggest essential oils could have an important role in augmenting conventional
analgesia. Finally, anethole, methyl salicilate, and camphor are all analgesic com-
ponents found in essential oils, and they are all found in root beer!
224 Section II Clinical Use of Aromatherapy

REFERENCES
Alavi A, LaRiccia P, Sadek A et al. 1997. Neuroimaging of acupuncture in patients
with chronic pain. Journal of Alternative & Complementary Medicine. 3(Suppl 1)
S47-S53.
Aydin S, Beis R, Ozturk Y et al. 1998. Nepetalactone: a new opioid analgesic from
Nepeta casesarea Boiss, Journal of Pharmacy & Pharmacology. 50(7) 813-817.
Aydin S, Ozturk Y, Beis R et al. 1996. Investigation of Origanum onites, Sideritis congesta
and Saturega cuneifolia essential oils for analgesic activity. Phytotherapy Research.
10:342-344.
Beck D, Beck J. 1987. The Pleasure Connection: How Endorphins Affect our Health
and Happiness. Anaheim, CA: Synthesis Press.
Benett A, Stamford F, Tavares I. 1988. The biological activity of eugenol, a major con-
stituent of nutmeg: studies on prostaglandins, the intestine and other tissues. Phy-
totherapy Research. 2(3) 125-129.
Berman B, Swyers J. 1997. Establishing a research agenda for investigating alternative
medical interventions for chronic pain. Primary Care. 24(4) 743-758.
Betts A. 1993. An overview of pathology. In Hinchcliff S, Norman S, Schrober J (eds.),
Nursing Practice and Health Care. London: Edward Arnold, 148-149.
Boelens M. 1994. Sensory and chemical evaluation of tropical grass oils. Perfumer &
Flavorist. 19:29-45.
Bowles J. 2000. The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Publishing.
Bronaugh R, Wester R, Bucks D. 1990. In vivo percutaneous absorption of fragrance in-
gredients in Rhesus monkeys and humans. Food and Chemical Toxicology. 28(5) 369-
373.
Buckle J. 1999. Use of aromatherapy as a complementary therapy of chronic pain. Alter-
native Therapies in Health & Medicine. 5(5) 42-51.
Cabo J, Crespo M, Jimenez J et al. 1986. The spasmolytic activity of various aromatic
plants from the province of Granada. The activity of the major components of their
essential oils. Plantes Medicinales et Phytotherapy. 20(5) 213-218.
Carter R. 1996. Give a drug a bad name. New Scientist. 150(2024)27-29.
Casey M. 2002. Aromatherapy: Pain management. Aromatherapy Today. 21:26-29.
Cornwall P, Barry B. 1994. Sesquiterpene components of volatile oils as skin penetration
enhancers for the hydrophilic permeant 5 fluorouracil. Journal of Pharmacy & Phar-
macology. 46(4) 261-269.
Craig C. 1994. Introduction to CNS pharmacology. In Craig C, Stitzel R (eds.), Mod-
ern Pharmacology, 4th ed. Boston: Little, Brown & Co., 329-336.
Brestel E, Van Dyke K. 1994. Lipid mediators of homeostasis and inflammation. In
Craig C, Stitzel R (eds.), Modern Pharmacology, 4th ed. Boston: Little, Brown &
Co., 477-485.
Dolara P, Corte B, Ghelardini C et al. 2000. Local anesthetic, antibacterial and antifun-
gal properties of sesquiterpenes from myrrh. Planta Medica. 66(4) 356-358.
Fakim G, Sofowora E, Sewaj M. 1990. Reversal of sickling and crenation in erythrocytes
by aqueous extracts of Pelargonium x asperum, Foeniculum vulgare and Sideroxylon pu-
berulum. Revue Agricole et Sucriere de l’Ile Maurice. 69, 91-93.
Chapter 12 Pain and Inflammation 225

Fakim G, Sewaj M. 1992. Studies on the antisickling properties of extracts of Sideroxylon
puberulum, Faujariopsis flexuosa, Cardispermum halicacabum and Pelargonium graveoleus.
Planta Medica. 58 (Suppl.) A648-A649.
Fields H. 1997. Pain: Anatomy and physiology. Journal of Alternative & Complemen-
tary Medicine. 3(Suppl 1) S41-S46.
Franchomme P, Penoel D. 1991. L’aromatherapie Exactement. Limoges, France: Jollois.
Gattefosse R. 1937. (Translated in 1993 by R. Tisserand.) Aromatherapie: Les Huile
Essentielles-Hormones Vegetales (Gattefosse’s Aromatherapy.) Saffron Walden, UK:
CW Daniels, 89.
Ghelardini C, Galeotti N, Salvatore G et al. 1999. Local anesthetic activity of essential
oil of Lavandula angustifolia. Planta Medica. 65(8) 700-703.
Gobel H, Schmidt G, Soyka, D. 1991. Effect of peppermint and eucalyptus oil prepara-
tions on neurophysiological and experimental algesimetric headache parameters.
Cephalalgia. 14:228-234.
Godwin D, Michniak B. 1999. Influence of drug lipophilicity on terpenes as transdermal
penetration enhancers. Drug Development and Industrial Pharmacy. 25(8) 905-915.
Goleman D. 1996. Emotional Intelligence. New York: Bantam.
Goodman-Gilma A, Goodman L, Murad F (eds.). 1985. The Pharmacological Basis of
Therapeutics. New York: Macmillan.
Greer C. 1995. Anatomical organization of the human olfactory system. In Gilbert A
(ed.), Compendium of Olfactory Research 1982-1994, 3-7.
Jakovlev V, Isaac O, Thiemer K et al. 1979. Pharmacological investigations with com-
pounds of chamomile. II. New investigations on the antiphlogistic effects of a bis-
abolol and bisabolol oxide. Planta Medica. 35:125-140.
Kline R, Kline J, Di Palma J et al. 2001. Enteric coated pH dependent peppermint oil
capsules for the treatment of irritable bowel syndrome in children. Journal of Pedi-
atrics. 138(1) 125-128.
Krall B, Krause W. 1993. Efficacy and tolerance of Mentha arvensis aethoeroleum. Paper
presented July 21-24 at 24th International Symposium on Essential Oils. Berlin, Ger-
many.
Kvam D. 1994. Anti-inflammatory and anti-rheumatic drugs. In Craig C, Stitzel R
(eds.), Modern Pharmacology, 4th ed. Boston: Little, Brown & Co., 485-500.
Lawless J. 1994. Aromatherapy and the Mind. London: Thorsons.
Lawrence B. 1995. Essential Oils 1992-1994. Carol Stream, IL: Allured Publishing.
Lewis W, Elvin-Lewis M. 1977. Medical Botany. New York: Wiley Interscience.
Lis-Balchin M. 1997. A preliminary study of the effect of essential oils on skeletal and
smooth muscle in vitro. Journal of Ethnopharmacology. 58(3) 183-187.
Lorenzetti B, Souza G, Sarti S et al. 1991. Myrcene mimics the peripheral analgesic ac-
tivity of lemongrass tea. Journal of Ethnopharmacology. 34(1) 43-48.
Lyss G, Schmidt T, Merfort I et al. 1997. Helenalin, an anti-inflammatory sesquiterpene
lactone from arnica, selectively inhibits transcription factor NF-kappaB. Biological
Chemistry. 378(9) 951-961.
MacSween R, Whaley K (eds.). 1992. Muir’s Textbook of Pathology, 13th ed. London:
Edward Arnold.
Mascolo N, Autore G, Capasso F. 1987. Biological screening of Italian medicinal plants
for anti-inflammatory activity. Phytotherapy Research. 1:28-31.
Martin B. 1994. Opioid and nonopioid analgesics. In Craig C, Stitzel R (eds.), Modern
Pharmacology, 4th ed. Boston: Little, Brown & Co., 431-450.
226 Section II Clinical Use of Aromatherapy

Meier B, Petersen M. 2001. Sales of painkiller grew rapidly but success brought a high
cost. New York Times. CL(51,683) A15.
Mills S. 1991. Out of the Earth. London: Viking Arkana.
Moran A, Martin N, Montero M. 1989. Analgesic, antipyretic and anti-inflammatory
activity of essential oil of Artemisia caerulescens subsp. gallica. Journal of Ethnopharma-
cology. 27(3) 307-317.
Nie N, Hull C, Jenkins J et al. 1975. Statistical Package for the Social Sciences. New
York: McGraw-Hill.
Paladini A, Marder M, Viola H et al. 1999. Flavonoids and the central nervous system:
from forgotten factors to potent anxiolytic compounds. Journal of Pharmacy & Phar-
macology. 51(5) 519-526.
Peana A, Moretti M, Juliano C. 1999. Chemical composition and antimicrobial action of
the essential oils of Salvia desoleana and Salvia sclarea. Planta Medica. 65(8) 752-754.
Pear R. 2002. Nutrition therapy to fall under Medicare umbrella. New York Times.
CLI(51,985) A16.
Perez-Raya M, Utrilla M, Navarro M et al. 1990. CNS activity of Mentha rotundifolia
and Mentha longifolia essential oil in mice and rats. Phytotherapy Research.
4:232-234.
Rose J. 1992. The Aromatherapy Book. San Francisco: North Atlantic Books.
Rossi T, Melegari M, Bianchi A et al. 1988. Sedative, anti-inflammatory and anti-
diuretic effects induced in rats by essential oils of varieties of Anthemis nobilis: a com-
parative study. Pharmacological Research Communications. 20(Suppl.) 71-74.
Seth G, Kokate C, Varma K. 1976. The effect of essential oil of Cymbopogon citratus on
central nervous system. Indian Journal of Experimental Biology. 14(3) 370-371.
Sheppard-Hangar S. 1995. Aromatherapy Practitioner Reference Manual, Vol. II.
Tampa, FL: Atlantic School of Aromatherapy.
Sofaer B, Foord J. 1993. Care of the person in pain. In Hinchcliff S, Norman S,
Schrober J (eds.), Nursing Practice and Health Care. London: Edward Arnold,
374-401.
Tubaro A, Zillia,C, Redaeli C et al. 1984. Evaluation of anti-inflammatory activity of
chamomile extract topical application. Planta Medica. 50(4) 359-360.
Von Frohilche A. 1968. A review of clinical, pharmacological and bacteriological re-
search into Oleum spicae. Wiener Medizinische Wochenschrift. 15:345-350.
Wagner H, Wierer M, Bauer R. 1986. In vitro inhibition of prostaglandin biosynthesis
by essential oils and phenolic compounds. Planta Medica. 52 (3)184-187.
Ward K. 1993. Care of the person with an infection. In Hinchcliff S, Norman S,
Schrober J (eds.), Nursing Practice and Health Care. London: Edward Arnold,
402-434.
Weil A. 1996. Spontaneous Healing. New York: Fawcett.
Wilkinson S. 1995. Aromatherapy and massage in palliative care. International Journal
of Palliative Nursing. 1(1) 21-30.
Woolfson A, Hewitt D. 1992. Intensive aromacare. International Journal of Aromather-
apy. 4(2) 12-14.
Wren R. 1988. Potter’s New Cyclopaedia of Botanical Drugs and Preparations. London:
Churchill Livingstone.
Yin M, Yamamoto Y, Gaynor R. 1998. The anti-inflammatory agent aspirin and salicy-
late inhibit the activity of I(kappa)Bkinase-beta. Nature. 396(6706) 77-80.
Chapter 12 Pain and Inflammation 227

228
W
13
Stress Management
History is filled with examples that demonstrate how human contact acts as one of
nature’s most powerful antidotes to stress.
James Lynch (1979)
P
atients’ stress levels will directly impact the rate of their recovery. However,
it is sometimes easy for health professionals to forget patients (and those
who care for them) are under stress as all attention is fixed on their symp-
toms or their disease. The reliability of previously used tools to measure stress is
now questioned, and there are moves to create different tools more sensitive to
psychological stress. Frazier et al (2002) found reliance on the top recognized
anxiety indicators in health care: agitation, increased blood pressure, increased
heart rate, patients’ verbalization of anxiety, and restlessness, produced an inaccu-
rate and incomplete anxiety evaluation of vulnerable patients. Frazier et al (2002)
wrote that reliance on these indicators could lead to “serious underestimation of
the extent of anxiety because anxiety is an uncomfortable, subjective phenomenon
that precedes the development of the most objectively detectable signs and be-
haviors.” O’Brien et al (2001) found no correlation of rating of stress between
coronary care patients and their attending health-care professionals. Van der
Does (1989) found a similar mismatch between patients and their caregivers in a
burn unit.
Despite these problems, health professionals now recognize stress has serious
consequences, and procedures are in place to help reduce stress when possible.
Redd and Manne (1995) investigated the effect of using aroma to reduce distress
during magnetic resonance imaging and found that a pleasant smell reduced the
stress and enhanced the coping ability of patients who had undergone traumatic
experiences. Fifty-seven participants received either heliotropin (a vanilla-like

scent) or plain air via a small tube inserted into their nostrils. Patients who re-
ceived the heliotropin reported 64% less anxiety than patients who had plain air.
However, their respiration and heart rate were not affected. Aromatherapy ap-
pears to be a quick, economical, and effective way of relieving, avoiding, and re-
moving stress, not just for patients, but also for staff and relatives.
Definitions of Stress
There are many definitions and types of stress, but it is generally agreed that Hans
Selye of McGill University conceived of the idea of stress in 1935. He was carry-
ing out research on rats and discovered those that had been injected with various
hormonal extracts developed enlarged adrenal glands, shrunken lymphatic glands,
and bleeding gastrointestinal ulcers. He called this “the stress syndrome” (Anthony
& Thibodeau 1983).
Rahe (1975), a psychiatrist at the University of Washington School of Med-
icine, found the more stress a person experienced, the more likely he or she
would fall ill. He interviewed more than 5000 people and devised what was to
become a classic, systematized method for correlating the events in people’s lives
with their illnesses (Pelletier 1992). Until that time it had been assumed only ad-
verse stress would have a significant effect. However the survey indicated any
change in the normal pattern of life, even good stress, was found to produce
symptoms.
Today, the word stress is used to describe the cause of all ills that cannot be
explained in any other way, even though the meaning of the word is unclear. A
1991 article in the British Medical Journal called stress a “chimera – an unreliable
word to be used sparingly” (Wilkinson 1991). However, there is such a thing as
good stress, which everyone feels occasionally and which galvanizes action.
A major conference held in Arizona in the 1980s brought together leading
psychologists, immunologists, and physicians to discuss stress and try to define it.
After heated debate, it was agreed there was no absolute definition of stress but
that “things” outside people caused stress. These “things” were labeled stressors. It
was suggested that people react and adapt to stressors differently. Some individ-
uals seem to be able to cope, while others do not, and there is no way of telling
who will cope and who will not.
The conference delegates agreed that stressors had measurable psychological
and physiological effects. This was borne out by Cohen et al’s later research on
stress and human susceptibility to the common cold (Cohen et al 1991), which
showed an individual under stress was more likely to “catch” a cold than someone
not under stress.
Anthony and Thibodeau (1983) wrote of the ancient Chinese custom using
anticipated physiological effects of stress. Individuals suspected of lying were
forced to chew rice powder and then spit it out. The Chinese believed the stress
of lying would render a person incapable of salivation. Indeed, perhaps this is the
origin of the saying “the dry mouth of fear.”
Chapter 13 Stress Management 229

Indicators of Stress
Selye’s List of Common Stressors (Anthony & Thibodeau 1983)
Extreme stimuli includes too much of almost anything. Consider a patient
in a hospital, perhaps in a high-dependency unit. It is obvious the pa-
tient is receiving continuous extreme stimuli in the form of bright lights
and loud or sudden noises.
Extreme deficiency including social deficiency incurred during solitary con-
finement, blindness, deafness, etc. This is called sensory deprivation, but
some patients are physically isolated for either their own protection or that
of others. Others can be made to feel outsiders to society because of their
illness, such as those with AIDS, HIV, hepatitis, or the physically handi-
capped. Perhaps a semiconscious patient would also fit into this category.
Stressors are often injurious, unpleasant, or painful. Hospital personnel do
not set out to injure their patients in the accepted sense of the word.
However, many medical procedures are unpleasant or painful.
Stressors are things an individual perceives to be a threat, whether real or
imaginary. Many hospital and nursing procedures are perceived to be
threatening, such as injections or lumbar punctures.
Stress is an intangible phenomenon. It cannot be tasted, heard, smelled, or
measured directly.
Stressors are individual. What is stressful today may not be tomorrow, and
what is stressful to one patient may not be to another.
Some indicators of stress can be easily measured, such as blood pressure rise,
tachycardia, pupil dilation, etc. But often stress cannot be measured in this way
and a psychological tool such as the stress and self-esteem questionaire developed
by Dr. Edward O’Brien (www.marywood.edu) needs to be used. Stress can be di-
vided into that which is necessary for survival and that which will eventually lead
to break down. Selye divided the physiological response to stressors into three
stages: alarm, resistance, and exhaustion. The alarm response can be life-saving—
the fight or flight phenomenon. During the alarm response, physiological changes
produced by receptors in the brain increase heartbeat and respiration rates. Un-
necessary metabolism, such as digestion, is curbed, while blood and oxygen are
swiftly redirected to the more vital centers of the body. When the danger is over,
the body quickly returns to its original state. Sweaty, clammy hands and cold feet
become warm and dry again. Respiration and pulse slow down to a normal level,
and digestion recommences.
Nixon (1976), a British cardiologist, found that when stress continued, a per-
son reached a point of no return. Fig. 13-1 indicates the point at which a person
under chronic stress would break down. Nixon thought if that person was isolated
and encouraged to rest, the mind, body, and spirit would be able to mend. Many
cardiac patients were treated successfully in this way when working with Nixon
in the 1970s.
230 Section II Clinical Use of Aromatherapy

In chronic stress, the “arousal state” of a person is never completely amelio-
rated. The measurable levels of stress in the body do not return to normal, and cor-
tisol levels remain above average. Throughout a period of time, small but damag-
ing physiological changes occur: blood sugar and pressure are raised, hormonal
functions change, and digestion and elimination are affected. Psychological stres-
sors are the most common cause of chronic stress. Pitts (1969) found lactate con-
centrations in the blood increased in patients with high levels of psychological
stress, producing anxiety neurosis. Barasch (1993) wrote prolonged stress could
create “fibrin cocoons” that prevented T cells from attacking cancerous metastases.
Stress is now recognized as one of the most serious health issues of the 20th
century. In 2002, the workforce still continues to push itself to the limit. It is al-
most as though being stressed is the acceptable face of modern life. No one seems
to consider changing his or her lifestyle. However if stress remains relentless,
change is often forced through breakdown.
If a person is unable to “switch off,” either physically or mentally, he or she
will eventually break down. It may be slow in coming, but break down they will
because the body cannot maintain that level of stress. Wilde McCormick (1992),
a British psychologist, wrote in her book on breakdown, “if we start to break down
in our bodies with symptoms that don’t seem to have an organic cause, it is a mes-
sage to us from the unconscious that we need to be taken into areas we have not
yet explored or made conscious.”
Occasionally, some individuals who have undergone stringent training in the
handling of potentially stressful situations (such as army personnel, firefighters, or
Chapter 13 Stress Management 231
Figure 13-1 The human function curve: a performance arousal curve used as a model for
a systems or biopsychosocial approach to a clinical problem.
Reproduced from: Nixon P.
1976. The human function curve. Practitioner. 217(76) 769, 935-944, with kind permission of the
author.

paramedics) will only show signs of stress when the situation is over, almost as if
their body is allowing them to “let go” when it is safe. Only then do they experi-
ence the palpitations and interrupted sleep patterns their colleagues experienced
while in the stress situation. Survivors of the 9/11 terrorist attacks in the United
States have written and spoken of this phenomenon.
Pelletier (1992a) quotes Sir William Osler: “the care of tuberculosis depends
more on what the patient has in his head than what he has in his chest.” In other
words how a patient feels will affect how he recovers. This is very relevant to the
way a patient is cared for in the hospital. Perhaps the word treat should be re-
assessed.
Stressors can be divided into several categories: physical, emotional, behav-
ioral, environmental, cultural, and political. A patient in the hospital could be ex-
periencing physical, emotional, behavioral, and environmental stress simultane-
ously. Physiological stress is usually accompanied by some psychological stress.
Psychological stress produces measurable physical changes. Even though psy-
chophysiology has found a wide range of physiological responses to psychologi-
cal stress, very little is done to address the psychological stress of patients in hos-
pitals (Anthony & Thibodeau 1983).
Physical responses to stress are governed by the hypothalamus, which is po-
sitioned next to the pituitary gland for easy hormone control (Clark & Montague
1993). The hypothalamus controls the autonomic nervous system and forms part
of the limbic system, so it is immediately apparent that stress will have a direct ef-
fect on almost all bodily functions, from temperature to hormone balance. Any-
thing that affects the sensory systems, like an odor, has a direct pathway to the
limbic system, in particular to the amygdala. LeDoux (1996) suggests this path-
way “does not allow for cortical processing and may be responsible for emotional
responses a person does not understand.”
The secretion of almost every hormone is altered in response to stress, and
the altered chemical signals immediately affect the immune system. The immune
system governs the ability to repair and heal (Linn et al 1988). Therefore the sug-
gestion that aromas might affect a response to stress is a very important one.
Common Measurable Physical Responses
Measurable physical responses to stress include the following:
Increased concentrations of adrenaline/noradrenaline in the blood and urine;
Increase in the rate and force of the heartbeat;
Rise in systolic blood pressure;
Dilation of the pupils;
Decrease in the number of white blood cells;
Increase in the level of blood adrenocorticoids;
Increase in the level of lactate in the blood;
Increase in the level of urinary adrenocorticoids.
An increase in eosinophils and lymphocytes during times of stress will lead to im-
munosuppression and decreased resistance to infection. An increase in aldosterone,
232 Section II Clinical Use of Aromatherapy

thyroxine, and glucagon will increase the level of blood glucocorticoids. An in-
crease in cortisol levels will affect carbohydrate, lipid, and protein metabolism.
This can lead to muscle wasting, thinning of the skin, and depression of immune
responses, as well as raised blood-cholesterol levels and a reduction in vitamin D
levels and calcium absorption resulting in osteoporosis.
The effect of stress is determined by whether a person becomes angry or
frightened. Proportions of adrenaline and noradrenaline are directly related to the
emotion displayed (Clark & Montague 1993). Predatory animals produce more
noradrenaline, while domestic animals produce more adrenaline. Patients in the
hospital tend to become frightened rather than angry. It would be interesting to
measure the levels of adrenaline and noradrenaline in patients to determine which
is higher and therefore what their stress response might be.
Psychological stress negatively impacts the skin and blocks the cutaneous
permeability barrier function. Coadministration of tranquilizers blocks this
stress-induced deterioration in barrier function (Garg et al 2001). This is why so
many skin diseases appear to be precipitated and exacerbated by stress. Walsh
(1996) reports on the case study of a 57-year-old mother of four who had expe-
rienced psoriasis for 30 years. Severe plaque psoriasis affected both her knees and
elbows. She had tried many orthodox treatments unsuccessfully. Bergamot, jas-
mine, sandalwood, and lavender in sweet almond oil were applied (2%) and im-
provement “beyond the normal” for prescribed medication was experienced. The
dry, flaky skin and red “scabs” disappeared, and she was able to wear a short-
sleeved blouse and knee-length skirt for the first time in years without embar-
rassment. While the psoriasis did not clear up completely, there was a great im-
provement. It is unclear whether the essential oils reduced her stress thus
impacting her psoriasis, or if the essential oils directly impacted the psoriasis.
Rimmer (1998) wrote about using aromatherapy to reduce stress in a patient
with terminal cancer. By using pleasant-smelling essential oils to reduce stress, the
patient was able to relax deeply, began to sleep better, and was better able to cope
with her pain.
Symptoms of Stress (Wilson-Barnett & Carrigy 1978)
Physical
Clenched jaw, leading to bruxism and referred neck pain
Hostility, depression, introspection, overemotionalism, nervous twitches,
nail-biting
Sweating for no obvious reason
Inability to sit still
Frequent crying or wish to cry
Lack of appetite or unnatural craving for food
Dyspepsia, indigestion/heartburn, constipation, diarrhea
Constant tiredness
Insomnia, vivid dreams, sleep disturbances
Headaches, migraines
Chapter 13 Stress Management 233

Breathlessness without exertion, palpitations, tachycardia
Dry mouth, dysphagia
Hypertension
Infertility, impotence
Mental
Constant irritability
Loss of sense of humor
Difficulty in concentrating
Lack of interest in life
Feeling unable to cope
Depression, being unable to show feelings
Dreading the future
Fear of being alone
Illnesses
Eczema, psoriasis, acne, skin disorders
Asthma
Dysmenorrea, premenstrual syndrome, hormonal imbalance, alopecia
Pruritus
Diabetes mellitus
Overactive thyroid
Colitis, irritable bowel syndrome
Pitt (1969), in Scientific American, made a list of 26 symptoms that are a result of
prolonged stress. The list is as follows:
1. Tires easily 14. Insomnia
2. Breathlessness 15. Unhappiness
3. Nervousness 16. Shakiness
4. Chest pain 17. Fatigued all the time
5. Sighing 18. Sweating
6. Dizziness 19. Fear of death
7. Faintness 20. Smothering
8. Apprehensiveness 21. Syncope
9. Headache 22. Nervous chill
10. Paresis 23. Urinary frequency
11. Weakness 24. Vomiting and diarrhea
12. Trembling 25. Anorexia
13. Breath unsatisfactory 26. Palpitations
Stress and Immunology
The immunological effects of stress are not always clear because each person deals
with them in his or her own way and because the effects are cumulative. How-
ever, there is a growing body of published evidence (both scientific and anecdo-
234 Section II Clinical Use of Aromatherapy

tal) to show that specific stressors are linked to depressed immune function. A
decrease in immunoglobulin A was measured in a study of dental students during
their first year (Ng et al 2002; Klecolt-Glaser & Glaser 1993). A similar study of
medical students prior to and during the first day of their final examinations re-
peated those findings; the students’ ability to produce interferon was drastically
reduced. Pelletier (1992a) discussed Bartrop’s study on bereavement, which
showed a lower lymphocyte function during the first 8 weeks following bereave-
ment. Quinn (1993) used this knowledge for her research on bereavement, which
looked at lowered immunological function and the effects of therapeutic touch.
Pert (1997), a molecular biologist and research scientist, described immunol-
ogy as a network of information with the mind flowing along it. Karl Pibram
(1976), who carried out neurophysiological research at Stanford University for
many years, describes the brain as a hologram storing information available to all
its different parts. In this case, could it be that when a person becomes stressed,
this hologram is affected and communication between neuropeptides (the net-
work of information) becomes blocked? Certain types of people appear to be pro-
tected from feelings of chronic stress. Jeanne Achterberg, an American psycholo-
gist, noted that at two institutions for the criminally insane, inmates who had
carried out horrendous crimes had been unusually protected from life-threaten-
ing diseases such as cancer, despite poor health habits such as heavy smoking.
Further studies showed mentally handicapped people were less likely to die from
cancer. On the basis of these studies it was suggested that a higher level of intel-
ligence could be linked to a higher incidence of chronic diseases such as cancer
(Barasch 1993). Do intelligent people tend to suppress their feelings, which then
suppress their immunological systems?
Stress and Patients
Arguably, one of the most stressful situations in anyone’s life is to be institution-
alized. To many people a hospital can seem like a prison. This attitude is well doc-
umented ( Jamison et al 1987). In a hospital is it all too easy for patients to lose
their sense of identity. Patients often feel anonymous. This feeling of anonymity
is compounded by Western medicine, which treats the medical condition rather
than the patient. An appendix is removed or a cancer is irradiated with little re-
gard for the gender, age, or weight of the person. Yet human beings are all unique,
so how can such a blanket treatment be right?
Patients in hospital are encouraged to conform. Questioning procedures of-
ten labels a patient as “difficult”. The medical profession is trained to diagnose,
not to discuss. Responsibility and choice of treatment are often removed from the
patient in the current medical model. Patients are rarely asked how they feel about
their treatment, or given a choice in it.
One of the most stressful things in life is to feel a loss of control. Being a hos-
pital patient means exactly that. This is not just the loss of control produced by
an alien environment (being unable to choose when to sleep or eat) but also the
Chapter 13 Stress Management 235

loss of control of intimate bodily functions. The more seriously ill the patient, the
more severe the loss of control and the ensuing stress. Compounding this sense
of loss is the feeling of invasion. Privacy, personal space, and the body itself are
invaded.
Of all surgery, perhaps heart surgery is the most feared, and a high percent-
age of patients experience psychological disturbances following open-heart
surgery (Layne & Yudofsky 1971). This may be due to the bypass machinery, but
it may have a closer connection to being in an intensive care unit and the relent-
less stressors found there: total loss of privacy, loss of sleep, bright lights, and con-
tinuous noise (Roberts 1991). It is ironic that the stress induced by a high-
dependency unit may impact the psyche of a patient to such an extent that he or
she may not survive the miracle of modern medicine.
Aromatherapy and Stress
Familiar smells associated with happy memories can help reestablish feelings of
happiness. To be happy is to be unstressed. Most essential oils from plants and
flowers have the potential to reduce stress. Certain essential oils, such as lavender,
rose, neroli, and petitgrain, are well known for this ability.
Each hospital department, whether oncology or dermatology, carries its
own particular brand of stress and fear. One of the most common, but least life-
threatening, stresses in oncology is a patient’s fear of hair loss. For women espe-
cially, this may produce profound anxiety. The simple act of a gentle head mas-
sage with a diluted essential oil such as lavender (Lavandula angustifolia ) can do
a tremendous amount to “touch the spot” and help reassure the patient that their
hair will grow back. In a randomized, controlled study, hair loss due to alopecia
responded well to topically applied essential oils (Hay et al 1998).
Organ transplant brings with it intense relief but also feelings of guilt and
anger. Sometimes these two emotions are not fully addressed, despite counseling.
For the patient receiving the transplant, it may not be the fact that another human
being has had to suffer, or die, but that a part of their own body has been “thrown
away” (Sylvia & Novak 1997). In the case of heart transplants, when patients have
literally “lost their hearts,” aromatherapy can introduce smell and touch to help re-
lease these feelings of grief and pain. Essential oils such as frankincense, ylang
ylang, angelica, and neroli can be useful tools in the healing process.
Outpatient departments are associated with long waits, dark corridors,
fraught staff, and physicians who rarely have time to look up from their notes.
Aromatherapy can help reduce the stress of waiting. Lehrner et al (2000) con-
ducted a randomized, controlled study with 72 participants and found Citrus
sinensis (sweet orange) had a calming and relaxing effect on patients waiting in a
dentist’s office.
Schulz et al (1998) conducted two multiple-crossover studies, each involving
12 female subjects and electroencephalograms to screen for acute sedating effect
of eight different plant extracts. Lavandula angustifolia (1200 mg) was given in
236 Section II Clinical Use of Aromatherapy

capsule form (orally), and 140 minutes later 100 mg of caffeine was given orally
in tablet form. Conventional medications decreased theta frequency but increased
beta in these studies. However, several plant extracts increased theta but had no
effect on beta. Theta and beta are brain waves generated by the thalamus
(http://brain.web-us.com/brainwavesfunction.htm).
Tasev et al (1969) and Sugano and Sato (1991) found rose was gently uplift-
ing. Muruzzella and Sicurella (1960) found eucalyptus was antibacterial. So, a va-
porizer containing rose (Rosa damascena) or eucalyptus (Eucalyptus globulus) could
gently uplift patients and staff and reduce the possibility of cross-infection.
Stress and Hospital Staff
Stress in hospitals is not confined to patients. The nursing staff is under tremen-
dous stress; their numbers have been cut even though their workload has re-
mained just as heavy, and morale is very low. Hospital managers show signs of
stress as they attempt to keep hospitals functioning. Physicians, too, are often de-
pressed and stressed. They have been forced into the “role of God” by the public,
and are then pilloried if they get it wrong. Healthcare is not healthy.
From the interns, many of whom still work 80-hour weeks, to consultant
surgeons who dash between operating rooms, there is no way these people could
avoid stress. Few physicians find it easy to linger over a meal or to resist answer-
ing the telephone by the second ring. Stress is something accepted as part of the
job in medicine. Alcoholism, drug abuse, and suicide were the downsides of work-
ing in medicine in the 1980s (Bennett 1987), and little has changed.
Health professionals find it hard to look after themselves. Since September
11, 2001, it has become more acceptable to acknowledge a sense of vulnerability
but it is still not OK for a health professional to admit being overwhelmed. The
pressure may be more manageable if some aromatherapy is used. Mandarin (Cit-
rus reticulata), lavender (Lavandula angustifolia), or chamomile (Chamaemelum no-
bile) inhaled for 5 minutes to help relaxation, or a few drops of peppermint (Men-
tha piperita), black pepper (Piper nigrum), or rosemary (Rosmarinus officinalis) oil
on a tissue, to revive and stimulate, might make long nights more tolerable.
Health professionals experience many emotional and disturbing scenes. This
is always distressing. Often there is no way of ameliorating emotions until the
next break, and frequently there are no breaks. However, a 2-minute hand “m”
technique with some neroli (Citrus aurantium var. amara) could be a quick, effec-
tive, and therapeutic pick-me-up (Penson 1991). Just inhaling angelica, petit-
grain, or rose could also be helpful. Touch and smell may be as old as the hills, but
they can be deeply comforting.
Stress and Visitors
Visiting a sick relative is stressful. What to say? What to do? Where to sit? Fre-
quently, the patient has insufficient energy to carry on a conversation, and the si-
lences become longer and longer.The sicker the patient, the more stressed the vis-
itors, and yet they come, sometimes long distances, if only for a few moments, to
Chapter 13 Stress Management 237

show that they care. Learning a simple hand or face “m” technique and using fa-
miliar smells can empower a visitor and make the patient feel wanted and cared
for. No words are necessary; touch can say it all.
It does not matter how ill patients are, they still need this kind of compas-
sion, especially from their loved ones. Research indicates the sicker the patients,
the less likely they are to be touched by their relatives, who are frequently afraid
to upset the complicated equipment around the patients. Research has also shown
patients with the poorest prognosis, or who are the most acutely ill, are often
touched least by the hospital staff (Ashworth 1984), although one of the most ba-
sic human, emotional needs is to feel physical contact (Weiss 1979).
Nurses, physicians, physical therapists, and others represent a large reservoir of
professionals who touch other people throughout life—from pediatrics to the care
of the elderly. For nurses in particular, aromatherapy offers a simple and acceptable
way of care. Children can learn how to give a gentle aromatherapy “m” technique to
elderly relatives, such as grandparents, in long-term care. Often a child visitor is
restless and awkward. This kind of structured touch is easy for a child to learn. It is
a simple and loving thing to do and costs little in terms of money, time, or energy,
but it communicates a great deal. Learning the “m” technique can be empowering.
It is the little things in life that are important, and in sickness the little things be-
come more significant, including fresh air, natural light, plants, peace and quiet,
kindly touch, and pleasant smells. Few of these occur in a hospital. Perhaps this is
what Florence Nightingale meant when she said the “least fortunate were those
who found themselves nearest to a hospital” (Landsdown 1994).
Relaxation
Relaxation is not just the opposite of stress, it is the answer to stress, and is im-
portant to our quality of life and to our survival. However, sometimes it is diffi-
cult to “switch off,” especially in a strange environment. The harder a person tries,
the more elusive relaxation seems to become. Modern life is geared to doing, not
being. What do you do? What do you want to do? These are the questions we use,
not Who are you? or Who do you want to be? When people become sick, the
ability to do is replaced with an enforced “being.” This alone is stressful to people
who have spent most of their lives in a doing mode. Dossey (1993) writes, “The
most effective way to reverse illness is sometimes to focus primarily on being.”
Health professionals frequently ask the impossible. “Just relax,” nurses mur-
mur before plunging hypodermic needles deep into the upper, outer quadrant.
“Just relax,” physicians suggest before probing the rectum with a finger. “Just
breathe naturally,” the voice murmurs as a gowned, masked man inserts a cardiac
catheter into the femoral artery, aimed at the heart. What do health profession-
als actually do to help patients relax?
Relaxation brings with it manifold benefits both for patients and health pro-
fessionals. Benson (1975) suggested many years ago that a relaxation break should
replace a coffee break. Despite this, stress management is not emphasized enough
238 Section II Clinical Use of Aromatherapy

in nurses’ or physicians’ training. However, there are programs developing to ad-
dress this issue.
In a discussion of massage and aromatherapy as supportive therapies in
health care, Sheena Hildebrand (1994) quotes from Wang Wei, who wrote in the
8th century, “Look in the perfumes of flowers and of nature for peace of mind and
joy of life.” Drury (1989) also wrote:
Caring, loving, touching,
Absence of connection to stress factors,
Being a part of reality but
Being centered in caring
for the whole person, Functioning with a positive
confident, loving presence.
Touch and relaxation
Many people find it pleasant and soothing to be stroked gently with something
that smells pleasant. In The Caring Touch (1981), reference is made to Sidney
Simon, who wrote of “skin hunger” and said “every human being comes into the
world needing to be touched, and the need for skin contact persists until death,
despite society’s efforts to make us believe otherwise”(Pratt & Mason 1981). He
also pointed out that “touch is quite distinct from sexual contact” and called for
“touch nourishment strategies.”
Touch presents a large body of reference that indicates a relaxation response.
In Palliative Care for Patients with Cancer, Victor Brewer, a patient with advanced
cancer, is quoted as describing the effects of touch as follows: “You unwind with
the gentleness of the human touch. It would be marvelous if nurses could do it in
hospital....With touch, as soon as the hands go on, you know she’s there, she’s
calm, she has time for you” (Penson 1991). The type of touch used in the “m”
technique is different from regular massage. It is much lighter and slower and is
not intended to address muscle tone, but to address soul tone. Please see the sec-
tion in Chapter 8 on the “m” technique.
Relaxation and Pain Relief
Touch aids the release of endorphins. Some endorphins can block the release of
substance P, one of the neurotransmitters involved in the sensation of pain. Some
pain can also be alleviated by rubbing the skin. In the gate theory, rubbing the
skin stimulates large-diameter afferent sensory fibers that excite interneurons,
causing enkephalin release (Turk & Nash 1993). Enkephalin release inhibits the
release of substance P from activated unmyelinated C fibers. This prevents T cell
activation and closes the pain gate (Fields 1997). The pain most often relieved by
massage is chronic pain that is poorly localized (Sofaer & Foord 1993). This type
of pain can be associated with many chronic conditions and with postoperative
recovery, although not with immediate postoperative care. Although deep massage
is contraindicated following recent surgery, the gentleness of the “m” technique
Chapter 13 Stress Management 239

around the affected area is highly appropriate and is a very useful adjunct to pain
control.
Some fragrances have deeply relaxing effects. Japanese research has shown
contingent negative variation (CNV), namely the upward shift in the brain waves
recorded by electrodes attached to the scalp, occurs in situations in which subjects
are expecting something to happen. CNV alters in response to odor. Following ex-
periments with diazepam and caffeine that produced central nervous system
(CNS) depression or stimulation, Torii et al (1988) found lavender had a depress-
ing effect and jasmine had a stimulating effect on the CNS. Further investigation
revealed that although odor had an effect on the brain, it did not appear to affect
physiological functions. Even in individuals who have no sense of smell (anosmia),
a chemical reaction to odors occurs in the brain if the olfactory nerve is intact.
In conclusion, touch and smell are two powerful relaxation tools available to
health professionals. It would be a shame not to use them.
Stress, Relaxation, and Psychoneuroimmunology
The American physicians Bernie Siegal and Larry Dossey have done much to
raise awareness of the importance of psychoneuroimmunology (PNI). The term
first became popular in 1986 with the publication of Siegal’s book, Love, Medicine
and Miracles (1986). In the book he wrote of patients who had survived cancer.
He calls them “exceptional cancer patients.” In one famous address to eminent,
orthodox physicians (many of whom were openly hostile to his views), he read
aloud from the novel Lady Chatterley’s Lover. He read for some time, until the
conservatively dressed men in front of him were fidgeting and red-faced. Then he
paused, closed the book, and said quietly “Now then, gentlemen, don’t tell me that
your mind has not affected your body!”
PNI is a medical subspeciality that involves the study of the connection be-
tween the mind (psycho), the brain (neuro), and the body’s ability to defend itself
against disease (immune). Humans do have the ability to affect their wellness or
disease-susceptibility through the power of thought. This finding has not been
accepted readily within orthodox medicine. Indeed, Siegal quotes from Dosto-
evsky at the beginning of his book: “A new philosophy, a way of life, is not given
for nothing. It has to be paid for dearly and is only acquired with much patience
and great effort.” Perhaps this quote is as relevant to aromatherapy as it is to PNI.
Norman Cousins, a patient, decided to apply the principle of PNI to himself.
Diagnosed with ankylosing spondylitis, he was told his spinal connective tissue
was dissolving (Cousins 1979). A regimen of medication consisting of 26 aspirin
and 12 phenylbutazone tablets daily resulted in hives all over his body but no pain
relief. Appalled by his hospital treatment (one day he had to give four separate
samples of blood for the same test because the pathology laboratory was in
chaos), he checked out of the hospital and into a hotel. Cousins knew pain could
be affected by attitude, and he instinctively chose to try laughter instead of
medication.
240 Section II Clinical Use of Aromatherapy

It was a brave and desperate move, but one that showed him 10 minutes of
genuine belly laughter had an anesthetic effect and gave him 2 hours of pain-free
sleep. Wanting “real” proof, Cousins took blood tests that confirmed his erythro-
cyte sedimentation rate fell by at least five points following laughter therapy. Bet-
ter still, the effect was cumulative. It seems laughter was stimulating the produc-
tion of endorphins, which resulted in a profound reduction of his joint
inflammation. Bolstered by this discovery, he refused to let his friends see him un-
less they could bring a new joke, cartoon, or film to make him laugh. Cousins un-
derstood how he felt affected how he was, and that included his illness.
It would be interesting to see if laughter could become a commodity provided
by hospitals. True, some get-well cards can be slightly amusing, but laughter ther-
apy, although effective, is not an approach easily incorporated into either a West-
ern medical model or the Western temperament. Illness is serious business, and
in the private sector, serious illness means serious money and long faces. No one
wants to be seen laughing! However Wilde McCormick (1990), in her book on
changing one’s life through self-help psychotherapy, advises “Make sure you laugh
every day.”
The relationship between an emotional reaction brought on by an illness and
the survival rate of a patient is highlighted by Fiore (1979), a patient with cancer.
Health professionals are in a unique position to encourage PNI, because “care
givers have the power to be dispiriting or inspiring to their patients” (Young
1990). Yet how many health professionals actually use this power to encourage
patients to draw on their own self-healing abilities?
Aromatherapy and PNI
Aromatherapy is a perfect way of utilizing PNI. Many patients find them-
selves lulled by repeated stroking movements, which encourage a series of endor-
phins into play. The pleasant smell of an essential oil will enhance this effect. To-
gether, smell and touch can produce a synergy of social, physical, psychological,
and neurological interactions in the patient. The most common comment made by
patients is how relaxing they find the treatment and how the feeling of relaxation
remains for several days. This may be highly relevant. Although it is recognized
that smell is instant, the effect of smell wears off very quickly as olfactory neurons
become inured to the odor. Perhaps by administering the “smell” transdermally, a
slow-release smell that produces a longer-lasting effect could be achieved.
Antoni et al (1990) wrote relaxation “may influence the immune function of
those patients with HIV, and retard disease progression among early HIV-1
seropositive individuals.” Supportive personal relationships improved the immune
function of women with breast cancer (Kiecolt-Glaser & Glaser 1993). Dean
Ornish’s study on reversing heart disease was based on diet, exercise, and stress
management. He wrote he was “increasingly convinced that the root of chronic
stress is a sense of isolation—from oneself, from others, and from something spir-
itual” (Ornish 1991).
Chapter 13 Stress Management 241

Farrow (1990) used massage in an acute medical ward. She found it reduced
anxiety in patients receiving morphine-pump therapy for pain during the period
when the pump was being changed, and it enabled a teenager to cope better with
her disfiguring postoperative ileostomy tubes and drains. Tisserand and Balacs
(1988) wrote about the “emotionally uplifting and comforting oils” that can be used
with cancer patients. King (1993) wrote about the ability of odor impressions to
“produce effects partly through mood changes” and concludes “fragrance provides a
useful adjunct for relaxation and has considerable potential for future development.”
Birchall (1990), writing for the New Scientist, asked whether aromatherapy
matches the potency of Valium and Librium, two drugs often used for stress, stat-
ing many of aromatherapy’s claims are now being validated by research. In fact,
as early as May 1988, the International Journal of Aromatherapy bore the headline
“Lavender beats benzodiazepines”(Tisserand 1988).
Reed and Norfolk (1993) found 36 of 38 patients experienced a feeling of re-
laxation following aromatherapy. This British study was carried out by two mid-
wives who were investigating whether lavender might reduce pain during child-
birth. Patients took baths with five drops of lavender during labor. There was no
control to this study. However, the results suggested aromatherapy did alter pain
perception in 30 women, and 36 women felt their ability to relax during labor was
enhanced. Stevenson (1992) concluded 100% of patients found the effects of a
foot massage with essential oil relaxing. She was investigating the effects of neroli
(Citrus aurantium flos) on 100 patients in London’s Middlesex Hospital cardiac
intensive-care unit following open-heart surgery. This was a controlled, random-
ized study using a modified Spielberger State Trait Anxiety Inventory for Adults
State Evaluation Questionnaire to measure pain, anxiety, tension, calmness, rest,
and relaxation. Physiological measurement showed a decrease in respiration, sug-
gesting an increased parasympathetic response. This conclusion was supported by
the psychological measurements. Stevenson showed patients who received a
neroli foot massage felt their anxiety decreased more than the patients who re-
ceived a foot massage without neroli essential oil.
Woolfson and Hewitt (1992) found 91% of patients experienced a reduction in
their heart rate of between 11 and 15 beats per minute following aromatherapy
massage. This study was carried out in the intensive-care unit of Royal Sussex
County Hospital in the United Kingdom. A total of 36 patients were allocated to
one of three groups: those massaged with essential oils, those massaged without es-
sential oils, and a control group who just rested. The results of this study appear to
agree with Stevenson’s findings that massage with an essential oil, in this case laven-
der, was more effective in reducing stress than massage without an essential oil.
Dunn et al (1995) found 122 patients felt anxiety reduction following aro-
matherapy massage with lavender in an intensive-care unit. Dunn led one of the
first formal trials to be conducted in a hospital, which paved the way for further
trials. Burns and Blamey (1994) studied 585 women in labor to determine
whether aromatherapy with any of 10 essential oils could reduce anxiety, increase
contractions, and reduce pain. The oils used were lavender, clary sage, pepper-
242 Section II Clinical Use of Aromatherapy

mint, eucalyptus, mandarin, chamomile, jasmine, rose, frankincense, and lemon.
The study was set up when the two investigators discovered aromatherapy was
part of the curriculum and examination syllabus for all student midwives in Ger-
many. Their results showed much satisfaction expressed by the mothers and the
delivery team concerning the reduction of stress with all of the essential oils used.
The study was not randomized or controlled but was an important investigation
and has led the way for the use of aromatherapy in other maternity units. A fur-
ther analysis of 8058 mothers who had received aromatherapy between 1990 and
1998 indicated more than 50% of mothers found it helpful for relaxation (Burns
et al 2000).
More than 10 years ago Wise (1989) wrote, “Aromatherapy helps to take the
anxiety out of being in hospital and quickens the patient’s return to self-care.”
Whether patients choose drops of essential oil on a pillow or an aromatic “m”
technique, there is no doubt that aromatherapy as a method of stress therapy is a
valid and important part of health care.
Spontaneous Remission
Finally, no chapter that refers to PNI would be complete without a mention
of spontaneous remission. The Institute of Noetic Sciences was founded in 1973
by astronaut Edgar D. Mitchell, following his experience of walking on the moon.
It is a research foundation and educational institution and has 30,000 members
worldwide. The word noetic comes from the Greek word nous, meaning mind, in-
telligence, and transcendental knowing.
In 1993, the Institute of Noetic Sciences and the Fetzer Institute published a
book documenting the results of a 10-year research program on the healing response.
Their program was “based on the belief that the ability of the physician to promote
health and to heal the sick in the future may be as dependent on the deeper under-
standing of the mind-body relationship as on the development of new technologies.”
Their study revealed a large body of evidence of extraordinary healing, in-
cluding regression of normally fatal tumors, with no currently available scientific
explanation (O’Regan & Hirschberg 1993). This discovery was not new to med-
icine. Nearly a century earlier Handley (1909) wrote in the British Medical Jour-
nal that “the recorded cases of natural repair of cancer, far from being anomalous
and exceptional, merely illustrate more strikingly than usual the natural laws
which govern every case of the disease.” The study carried out by the Institute of
Noetic Sciences was the largest investigation of spontaneous remission to date. It
concluded, “The evidence suggests this kind of healing can be triggered by a va-
riety of stimuli, diverse in nature, including signals, suggestions and guidance
from the physical, mental and/or spiritual realm of every individual.”
Sadly, Brendan O’Regan, the visionary responsible for the program, died in
1992 before the study was completed. Although a great portion of the study was
completed in 1990, more than 300 additional references to spontaneous remission
from cancer and other diseases (which were published in medical journals be-
tween 1990 and 1992) have been collated subsequently.
Chapter 13 Stress Management 243

There is no suggestion that aromatherapy could result in spontaneous remis-
sion, but aromatherapy does have a profound impact on the mind-body link. It
would be interesting to measure immune levels before and after an aromatherapy
treatment. To quote the Institute of Noetic Sciences, “We are at the threshold of
a new field of inquiry.” Ralph Waldo Emerson wrote that “thought is the blos-
som, language the bud, action the fruit behind it.” I hope this chapter will serve
as the bud to encourage a little fruit!
REFERENCES
Anthony G, Thibodeau G. 1983. Textbook of Anatomy and Physiology. London: CV
Mosby.
Antoni M, Fletcher M, Goldstein D et al. 1990. Psychoneuroimmunology and HIV-1.
Journal of Consulting and Clinical Psychology. 58(1) 38-49.
Ashworth P. 1984. Staff-patient communication in coronary care units. Journal of Ad-
vanced Nursing. 9(1) 35-41.
Barasch M. 1993. The Healing Path. New York: Putnam.
Bennett G. 1987. The Wound and the Physician. London: Secker & Warburg.
Benson H. 1975. The Relaxation Response. New York: Avon.
Birchall A. 1990. A whiff of happiness. New Scientist. 127(1731) 44-47.
Burns E, Blamey C. 1994. Soothing scents in childbirth. International Journal of Aro-
matherapy. 6(1) 24-28.
Burns E, Blamey C, Ersser S et al. 2000. An investigation into the use of aromatherapy
in intrapartum midwifery practice. Journal of Alternative & Complementary Medi-
cine. 6(2) 141-147.
Clark E, Montague S. 1993. The nature of stress and its implications for nursing prac-
tice. In Hinchcliff S, Norman S, Schober J (eds.), Nursing Practice and Health Care.
London: Edward Arnold, 214-247.
Cohen S, Tyrrell D, Smith A. 1991. Psychological stress and susceptibility to the com-
mon cold. New England Journal of Medicine. 325(9) 606-612.
Cousins N. 1979. Anatomy of an Illness as Perceived by a Patient. New York: WW Nor-
ton.
Dossey L. 1993. Healing Words. San Francisco: Harper.
Drury M. 1989. Caring. In McGuire C (ed.), Visions of Nursing. Sedona, AZ: Light
Technology, 44.
Dunn C, Sleep J, Collett D. 1995. Sensing an improvement: an experimental study to
evaluate the use of aromatherapy, massage and periods of rest in an intensive-care
unit. Journal of Advanced Nursing. 21(1) 34-40.
Farrow J. 1990. Massage therapy and nursing care. Nursing Standard. 4(17) 26-28.
Fields H. 1997. Pain: Anatomy and Physiology. Journal of Alternative and Complemen-
tary Medicine 3 (suppl. 1). 541-546.
Fiore N. 1979. Fighting cancer: one patient’s perspective. New England Journal of Med-
icine. 300(21) 284-289.
Frazier S, Moser D, Riegel B et al. 2002. Critical care nurses’ assessment of patients’
anxiety: reliance on physiological and behavioral parameters. American Journal of
Critical Care. 11(1) 57-64.
Garg A, Chren M, Sands L et al. 2001. Psychological stress perturbs epidermal perme-
ability barrier homeostasis. Archives of Dermatology. 137(1) 53-59.
244 Section II Clinical Use of Aromatherapy

Handley W. 1909. The natural cure of cancer. British Medical Journal. 582-589.
Hay L, Jamieson M, Ormerod D. 1998. Randomized trial of aromatherapy: successful
treatment for alopecia areata. Archives of Dermatology 134(11) 1349-1352.
Hildebrand S. 1994. Massage and aromatherapy. In Wells R (ed.), Wells’ Supportive
Therapies in Health Care. London: Bailliere Tindall, 110-111.
Jamison R, Parris W, Maxson W. 1987. Psychological factors influencing recovery from
outpatient surgery. Behavioural Research Therapies. 25(1) 31-37.
Kiecolt-Glaser J, Glaser R. 1993. Mind and immunity. In Goleman D, Curin J (eds.),
Mind-Body Medicine. New York: Consumer Reports Books, 39-65.
King J. 1993. Have the scent to relax. World Medicine. 29-31.
Landsdown R. 1994. Living longer? Qualitative survival. Journal of the Royal Society of
Medicine. 87:636.
Layne O, Yudofsky S. 1971. Postoperative psychosis in cardiotomy patients. New Eng-
land Journal of Medicine. 284(10) 518-520.
LeDouz J. 1996. The Emotional Brain. New York: Simon & Schuster.
Lehrner J, Eckersberger C, Walla P et al. 2000. Ambient odor of orange in a dental of-
fice reduces anxiety and improves mood in female patients. Physiology & Behavior.
71(1-2) 83-86.
Linn B, Linn M, Klimas N. 1988. Effects of psychophysical stress on surgical outcomes.
Psychosomatic Medicine. 50(3) 230-244.
Lynch J. 1979. The broken heart—the medical consequences of loneliness. San Fran-
cisco: Harper-Row.
Muruzzella J, Sicurella N. 1960. Antibacterial activity of essential oil vapors. Journal
of the American Pharmaceutical Association (Scientific Edition). 49(11)
692-695.
Ng V, Koh D, Mok B et al. 2002. Stressful life events of dental students and salivary
diomarker (abstract). International Journal of Immunopathology and Pharmacology
15(2) 5.
Nixon P. 1976. The human function curve. Practitioner. 217(76) 769, 935-944.
O’Brien J, Moser D, Riegel B et al. 2001. Comparison of anxiety assessments between
clinicians and patients with acute myocardial infarction in cardiac critical care units.
American Journal of Critical Care. 10(2) 97-103.
O’Regan B, Hirshberg C. 1993. Spontaneous Remission. Sausalito, CA: Institute of
Noetic Sciences.
Ornish D. 1991. Reversing heart disease through diet, exercise and stress management.
Journal of the American Dietetic Association. 91(2) 162-165.
Pelletier K. 1992. Mind-body health: research, clinical and policy implications. American
Journal of Health Promotion. 6(5) 345-348.
Pelletier K. 1992a. Mind as Healer, Mind as Slayer. New York: Delta.
Penson J. 1991. Complementary therapies. In Penson J, Fisher R (eds.), Palliative Care
for People with Cancer. London: Edward Arnold, 233-246.
Pert C. 1997. Molecules of emotion. New York: Scribner.
Pibran K. 1976. Consciousness and the brain. New York: Plenum Press.
Pitts F. 1969. The biochemistry of anxiety. Scientific American. 220(2) 69-75.
Pratt J, Mason A. 1981. The Caring Touch. London: Heyden.
Quinn J. 1993. Psychoimmunologic effects of therapeutic touch on practitioners and re-
cently bereaved recipients. Advanced Nursing Science. 15(5) 13-26.
Rahe R. 1975. Epidemiological studies of life change and illness. International Journal of
Psychiatry in Medicine. 6(2) 133-146.
Chapter 13 Stress Management 245

Redd W, Manne S. 1995. Using aroma to reduce distress during magnetic resonance
imaging. In Gilbert A (ed.), Compendium of Olfactory Research 1982-1994. New
York: Olfactory Research Fund Ltd., 47-52.
Reed L, Norfolk L. 1993. Aromatherapy in midwifery. International Journal of Alterna-
tive and Complementary Medicine. 11:15-17.
Rimmer L. 1998. The clinical use of aromatherapy in the reduction of stress. Home
Healthcare Nurse. 16(2) 123-126.
Roberts R. 1991. Preventing PDD (post-pump delirium) after surgery. Nursing. 4(27)
28-31.
Schulz H, Jobert M, Hubner W. 1998. The quantitative EEG as a screening instrument
to identify sedative effects of single doses of plant extracts in comparison to diazepam.
Phytomedicine. 5(6) 449-458.
Siegal B. 1986. Love, Medicine and Miracles. New York: Arrow.
Sofaer B, Foord J. 1993. Care of the person in pain. In Hinchcliff S, Norman S, Schrober
J. (eds.), Nursing Practice and Health Care. London: Edward Arnold, 374–401.
Stevenson C. 1992. Orange blossom evaluation. International Journal of Aromatherapy.
4(3) 22-24.
Sugano H, Sato N. 1991. Psychophysiological studies of fragrance. Chemical Senses.
16:183-184.
Sylvia C, Novak W. 1997. A Change of Heart. Boston: Little, Brown & Co.
Tasev T, Toleva P, Balabanova V. 1969. The neuro-psychic effect of Bulgarian rose,
lavender and geranium. Folia Medica. 11(5) 307-317.
Tisserand R. 1988. Lavender beats benzodiazepines. International Journal of Aro-
matherapy. 1(1) 1-2.
Tisserand R, Balacs T. 1988. Essential oil therapy for cancer. International Journal of
Aromatherapy. 1(4) 20-25.
Torii S, Fukuda H, Kanemoto H et al. 1988. Contingent negative variation (CNV) and
the psychological effects of odor in perfumery. In Van Toller S, Dodd G (eds.),
Perfumery: The Psychology and Biology of Fragrance. London: Chapman & Hall,
107-120.
Turk D, Nash J. 1993. Chronic pain: New ways to cope. In Goleman D and Gurin J
(eds.). Mind/Body Medicine. New York: Consumer Reports. 111-131.
Van der Does A. 1989. Patients’ and nurses’ rating of pain and anxiety during burn
wound care. Pain. 39(1) 95-101.
Walsh D. 1996. Using aromatherapy in the management of psoriasis. Nursing Standard.
11(13-15) 53-56.
Weiss S. 1979. The language of touch. Nursing Research. 28(2) 76-80.
Wilde McCormick E. 1990. Change for the Better. London: Unwin-Hyman Ltd.
Wilde McCormick E. 1992. Healing the Heart. London: Optima Books.
Wilkinson G. 1991. Stress: another chimera? British Medical Journal. 302(3) 191-192.
Wilson-Barnett J, Carrigy A. 1978. Factors influencing patients’ emotional reactions to
hospitalization. Journal of Advanced Nursing. 3(3) 221-229.
Wise R. 1989. Alternative therapies: Flower power. Nursing Times. 85(22) 45-47.
Woolfson A, Hewitt D. 1992. Intensive aromacare. International Journal of Aromather-
apy. 4(2) 12-13.
Young S. 1990. The exceptional cancer patient support group: coping with cancer. In
Clements S, Martin E (eds.), Nursing and Holistic Wellness. Dubuque, IA:
Kendall/Hunt Publishing, 233-247.
246 Section II Clinical Use of Aromatherapy

W
247
14
Cardiology
Whatever the physiological problem with the heart, its function is affected by what
each individual asks of their heart in terms of effort. This is determined by the
person we are, by the way we live within our own body and by the relationship
we do or do not make with it.
Elizabeth McCormick (1997)
A
lterations in mental status are common among patients in a cardiac
intensive-care unit. These changes can be due to medication, brain
trauma, or metabolic function (Beauchamp et al 2000). However, contin-
uous stress, insomnia, sensory deprivation, and loss of privacy can also cause
changes in mental state. These all occur in an intensive-care unit. The heart is of-
ten described as the seat of emotion, and aromatherapy can play an important role
in assisting patients as they come to terms with feelings that may have been
blocked. Aromatherapy can also help them cope with a highly stressful situation.
While aromatherapy cannot replace a damaged valve or repair an atrial septal de-
fect, it can be useful for reducing the stress that surrounds a heart attack and may
reduce the period of recovery following a heart attack or surgery. Aromatherapy
is used in some medical and surgical cardiac units, and many of the essential oils
have a history of being supportive to the heart, as well as being generally relaxing.
Several cardiac conditions can benefit from aromatherapy: borderline hyper-
tension, anxiety associated with myocardial infarction, and postpump depression
or delirium (PPD).
Borderline Hypertension
Hypertension and its complications affect an estimated 50 million Americans, 30%
of whom are unaware they have hypertension. Only 70% of those who are aware of

their condition receive treatment (Manger & Gifford 2001). Approximately 35,000
Americans die each year from conditions directly associated with hypertension.
Hypertension, an abnormal rise in blood pressure, occurs when the arterioles be-
come constricted, reducing the ability of the blood to flow and making the heart
work harder. Ninety percent of all cases of hypertension are essential hypertension,
which means there is no apparent reason. However, there are some associated risk
factors: obesity, smoking, alcohol consumption, a diet high in fat or salt, gender
(men are more likely to have hypertension than women), race (African Americans
are more likely to develop hypertension than any other group), and genetics. Sec-
ondary hypertension is defined as an elevation in blood pressure caused by a preex-
isting condition such as coarctation of the aorta, kidney disease, or thyroid mal-
function. However, Samuel Mann, a professor of clinical medicine at Cornell
University, believes emotion may play a major role in hypertension (Mann 1997).
An elevated blood-pressure reading is above 140/90. Antihypertensive drugs
appear to be effective at reducing mortality and morbidity in the elderly (Mulrow
et al 1997). However, the British National Health Service Center for Reviews and
Dissemination at the University of York (1999) reported all the main classes of an-
tihypertensive drugs are associated with adverse side effects, although the majority
of symptoms were mild, such as dizziness, headache, or rash. In addition, the report
continued, the older the patient, the more severe the side effects become, including
arrhythmias or renal dysfunction. Both the older types of beta-blocker and diuretic
drugs and the newer angiotensin-converting enzyme (ACE) inhibitors and calcium-
channel blockers had side effects. Instead, light exercise, change in diet, relaxation,
and meditation are often encouraged to reduce borderline blood pressure.
Aromatherapy can help as an adjunctive relaxing therapy, and some essential
oils are thought to help reduce borderline hypertension. Thymol isolated from es-
sential oil of Trachyspermum ammi reduced the blood pressure of anesthetized rats
(Aftab et al 1995). This herb has a history of being used in Pakistan to reduce hy-
pertension. However, in this study quite large amounts of thymol were given (1-
10 mg/kg) by intraperitoneal injection. The authors postulate the hypotensive ef-
fect of thymol was due to its calcium-channel-blocking ability. Thymol is also
found in Thymus vulgaris (common thyme), an inexpensive essential oil. Thymol
is a phenol and as such is not something that immediately comes to mind for hy-
pertension, as phenols are generally thought to be stimulating.
Tisserand and Balacs (1995) state “it is extremely unlikely that an essential oil
could exacerbate hypertension or hypotension.” Guba (2000), an Australian clinical
aromatherapist, completed an extensive search of the available literature and con-
cluded that an essential oil was unlikely to elevate high blood pressure and many aro-
matherapy cautions regarding essential oils and hypertension were based on myth.
A recent study carried out on human subjects did show inhaled rosemary in-
creased systolic and diastolic measurements, but the effects were transient, lasting
only a few minutes (Saeki & Shihora 2001). The same study found lavender re-
duced systolic pressure, again for a short period of time. Other essential oils such
as geranium and clary sage have shown measurable hypotensive effect in animal
248 Section II Clinical Use of Aromatherapy

studies. Essential oils, like herbs, appear to be adaptogenic; they balance the body
when it is out of balance. Adaptogens constitute a novel class of metabolic regu-
lators that can have different psychological and physiological effects depending
on the requirement of the host (Panossian et al 1999).
Despite a lack of evidence, many schools of aromatherapy suggest avoiding
stimulant essential oils such as Rosmarinus officinalis (rosemary), Mentha piperita
(peppermint), or spike lavender(Lavandula latifolia) with any patient who has hy-
pertension. These essential oils will be discussed individually.
O’Brien (1997) reported on her experiences with the hypertensive effects of
rosemary in elderly, long-term-care patients suffering transient hypotension as a
side effect of antidepressants. Patients inhaled two drops of rosemary for 5 min-
utes before getting up from a seated position. Blood pressure was measured be-
fore and after getting up. A control group was given carrier oil with no known
pharmacological properties to smell. Blood pressures of all patients had been
recorded since their admission to the hospital, prior to beginning the antidepres-
sant medication. The number of instances in which a subject fell down immedi-
ately after rising from a sitting position (presumably as a result of hypotension)
was compared with falls within the same timeframe the previous year. The num-
ber of falls dropped by more than 50%. Rosemary did not appear to have any hy-
pertensive effect on normal blood pressure.
Rosemary was also found to have pharmacological stimulatory effects in
animals by Kovar et al (1987). However, rosemary was shown to have slight
anxiety-reducing effects in a study at the University of Wolverhampton. Unfor-
tunately, the botanical name and chemotype of the rosemary used were not stated
(Morris et al 1995).
Peppermint is traditionally considered to have stimulating properties.
Menthol-flavored cigarettes and peppermint confections have both been responsi-
ble for atrial fibrillation in cardiac patients prone to that condition who were previ-
ously stabilized on quinidine (Thomas 1962). l-menthol was found to dilate sys-
temic blood vessels when given intravenously (Agshikar & Abraham 1957). It is
extremely unlikely that inhaled peppermint would have any negative effect on pa-
tients with high blood pressure, and peppermint is very useful for nausea. However,
peppermint has a pervasive smell and is difficult to tolerate for several hours. Perez-
Raya et al (1990) found two other mints, Mentha rotundifolia and Mentha longifo-
lia, which grow wild in Spain, enhanced sodium barbitone-induced sleep in rats.
Spike lavender (Lavandula latifolia) has a history of being an expectorant and
mycolytic and was found useful in upper respiratory-tract infection (Charron
1997). It is also thought to be a stimulant. Certainly a few drops of this
camphorous-smelling lavender is more likely to clear the sinuses than induce
sleep; however, there is no record of spike lavender increasing blood pressure.
Freund (1999) conducted a small pilot study on 13 patients with borderline
hypertension. The age range was 21-71 years, and the group included five males
and eight females. Eleven patients were more than 15 pounds overweight.
Baseline blood pressure was taken with each patient in a supine position. Patients
Chapter 14 Cardiology 249

rated their stress level based on a visual analog. Subjects were asked to inhale five
drops of ylang ylang essential oil for 15 minutes. Blood pressure was remeasured,
and the stress level recording was reassessed. The same group received a control
aroma (carrier oil with no pharmacological effect) at a different time. The ylang
ylang (Cananga odorata) group experienced a 50% greater drop in systolic and di-
astolic pressure than did the control group. The stress visual analog also indicated
the ylang ylang group felt a 50% greater reduction in stress. Ylang ylang has an
anecdotal history of being used to reduce blood pressure and is used by British
midwives to help reduce hypertension in pregnancy.
Essential oils that could help reduce hypertension are ylang ylang, Roman
chamomile, true lavender, and clary sage. Neroli, sandalwood, spikenard, and
sweet marjoram might also have advantageous effects. Whatever the choice of es-
sential oil, it is important to ask patients which aromas remind them of pleasant
memories and use those. Gentle touch is one of the most soothing actions that
can be offered another human being in distress. Holism is about being present for
the patient. Aromatherapy can put the heart back into health care.
Anxiety and Myocardial Infarction
Acute myocardial infarction (known more commonly as a heart attack) is the lead-
ing cause of death in the Western world with one million deaths each year (Rogers
et al 1994). It is also a leading reason for hospitalization in the United States (Hill
et al 1992). Approximately 90% of those who reach a hospital survive (Hill et al
1992). Twenty to 30% of the cost associated with acute myocardial infarction is re-
lated to the length of time a patient stays in the coronary-care unit (Sgura et al
2001). The main symptom of acute myocardial infarction is defined by the World
Health Organization as intense, prolonged, or intolerable chest pain necessitating
hospitalization. Fifty percents of deaths caused by myocardial infarction occur
within 2 hours of the onset of symptoms (Hope et al 1993). In the United King-
dom, the number of deaths from heart attacks each year is equal to the number of
babies born (McCormick 1993). Standard treatment is primary reperfusion ther-
apy and the judicious use of aspirin, beta blockers, angiotensin-converting enzyme
(ACE) inhibitors, and glyoprotein antagonists. These have reduced the length of
time patients spend in a high-dependency unit (Sgura et al 2001).
Despite analgesics and sedatives, many patients are anxious when they arrive in
a coronary-care unit. Their arrival at the hospital is usually unexpected, so they come
unprepared. Unattended business meetings and unanswered e-mail are difficult to
forget, and patients find it a challenge to switch off their worries. Anxiety can extend
infarction areas or precipitate further arrhythmias (Summers Dunnington et al
1988). Anxious patients are more likely to experience severe or chronic psychologi-
cal distress. Rowe (1989) discovered patients’ anxieties tend to be focused on their
own illness. The severity of the infarction and how close to death patients perceive
themselves to be will influence the level of psychological distress they experience.
Vlay and Fricchione (1985) reported on heart-attack patients’ emotional distur-
250 Section II Clinical Use of Aromatherapy

bances, which are often expressed as depression, anger, frustration, and fear. Mood
has a powerful influence on prognosis after acute myocardial infarction (Petty 2000).
Aromatherapy attempts to alleviate these feelings and to reduce anxiety. Be-
cause these patients have constant monitoring and/or visitors, it is important to
select essential oils that will be acceptable to all those who will smell them. Aro-
mas of citrus and herbs are usually acceptable. Gould et al (1973) reported on the
relaxing cardiac effects of chamomile tea on a group of 12 hospitalized patients
who were undergoing cardiac catheterization. They found there was a small but
significant rise in the group’s mean brachial-artery pressure, so there was some
hemodynamic change but essentially no cardiac effect. However, the scientists
were more struck that 10 of the 12 patients fell into a deep sleep within 10 min-
utes of drinking the tea. Sleeping is a rarity during cardiac catheterization. Pa-
tients had not been premedicated and received no other sedation during the pro-
cedure.
Yamada et al (1996) found chamomile essential oil reduced stress-induced
increases in plasma adrenocorticotropic-hormone levels in rats and concluded es-
sential oil of Roman chamomile might be useful against stress in humans. Finally,
Avollone et al (1996) studied an aqueous extract of German chamomile flowers
and found it behaved as both central and peripheral benzodiazepine receptor lig-
ands, with anxiolytic effects. Viola et al (1995) identified the anxiolytic compound
as apigenin. German and Roman chamomile are different essential oils with dif-
ferent chemistries. Roman may be more conducive to use in a cardiac unit as it
has a more pleasant aroma. Table 14-1 lists essential oils used following myocar-
dial infarction along with the studies that have been done on their effects.
Chapter 14 Cardiology 251
Table 14-1
h Anxiolytic Essential Oils for Use Following
Myocardial Infarction
Common Name Botanical Name Reference
Melissa Melissa officinalis Wagner & Sprinkmeyer 1973
Buchbauer et al 1993
Lavender Lavandula angustifolia Bauhbauer et al 1991,
Woolfson & Hewitt 1991
Roman chamomile Chamaemelum nobile Rossi et al 1988
Neroli Citrus aurantium flos Jager et al 1992
Rosewood Aniba rosaeodora Nacht & Ting 1921
Marjoram Origanum majorana Nacht & Ting 1921
German chamomile Matricaria recutita Viola et al 1995
Rose Rosa damascena Nacht & Ting 1921,
Buchbauer et al 1994

Postpump Depression/Delirium
Alterations in mental status are common following bypass surgery (Beauchamp
et al 2000). Up to 75% of patients have deterioration in performance on neu-
ropsychiatric tests (Mahanna et al 1996), and up to 32% develop Postpump
depression/delirium (PPD) (Roach et al 1996). Glick et al (1996) suggest PPD is
often not recorded, so it is difficult to analyze how many patients are affected. A
2001 article in the New York Times suggested depression is more common after
bypass surgery than other types of surgery (Epstein 2001) and occurs in 30%-75%
of patients. The article quotes Dr. R. Scott Mitchell, a cardiovascular surgeon at
Stanford, and Dr. Roy John, professor of psychiatry and director of the brain re-
search laboratories at New York University Medical Center. Dr. John suggests
atherosclerotic plaques in the aorta could become dislodged during surgery and
bombard the brain, or that the anesthesia and cooling used during the operation
could alter brain chemistry. A doctor at one British university suggests PPD
(delirium) could be caused by sensory imbalance or disorientation (Lidster 2001).
Danilowicz and Gabriel (2001) compared two matched groups of patients
from the National Heart Institute and found the incidence of PPD (delirium) was
higher among men than women and higher in those who were not able to com-
municate in English. The study emphasizes the importance of communication.
PPD is thought to play a major role in the development of sternal instability
(Bimmel et al 2001), which has a major influence on postoperative recovery after
bypass surgery.
Many patients arriving in a critical-care unit have undergone elective surgery,
so they have been prepared for the ordeal that awaits them. British psychologist
McCormick (1993) suggests “preparation by the feeling heart for the worker
heart’s surgery is essential.” Many surgeons, including Mehmet Oz, MD, at Co-
lumbia Presbyterian Medical Center in New York, believe she is right. Patients
who are prepared are better able to cope with their condition postoperatively
(Roberts 1991), as fear of surgery is a factor that can strongly influence a patient’s
emotional response to hospitalization (Wilson-Barnett & Carrigy 1978). Of all
the operations performed, open-heart surgery is possibly the most feared.
The symptoms of PPD are hyperventilation, tachycardia, auditory hallucina-
tions, disorientation, and paranoid delusions (Layne & Yudofsky 1971). The
symptoms are distressing for the patient, their relatives, and for those who care
for them. The Rancho Los Amigos Cognitive Scale lists eight different states of
consciousness (Herndon 1997). They range from no response, through confused-
inappropriate, to purposeful appropriate and could be a very good tool to use in
measuring PPD.
Although there are several theories concerning the pathogenesis of PPD,
nothing is clear. It is thought that older patients, those undergoing aortic valve re-
placement, and male patients are more at risk. However, Layne and Yudofsky
(1971) found a reduction in postoperative psychosis was achieved in 50% of pa-
tients by conducting a preoperative psychiatric interview. This interview allowed
252 Section II Clinical Use of Aromatherapy

and encouraged patients to ask questions about their disease and surgery and to
discuss openly any worries they had (Layne & Yudofsky 1971). Preoperative psy-
chological preparation is now recognized as being important not just for the pa-
tient, but also for the relatives who will be supporting the patient postoperatively
(Roberts 1991). Discussing current or potential marital or relationship problems
can help indicate which patients are more likely to succumb to PPD (Egerton &
Kay 1964). Any illness will force a relationship to change, and open-heart surgery
will certainly test the strength of every relationship.
Utilizing the preparation time, aromatherapy can set a safe, gentle pattern
which, when repeated postoperatively, could affect the patient positively through
learned memory. If patients feel relaxation and pleasure when they receive a foot,
hand, or face “m” technique with a favorite aroma preoperatively, chances are they
will feel the same relaxation and pleasure when the aromatherapy is repeated
postoperatively. Table 14-2 lists essential oils that have been used to prevent
and/or treat PPD, along with the studies undertaken to determine the possible
benefits.
Chapter 14 Cardiology 253
Table 14-2 h Essential Oils for the Possible Reduction of PPD
Common Name Botanical Name Reference
Neroli Citrus aurantium flos Jager et al 1992,
Stevensen 1994
Angelica Angelica archangelica (root) Franchomme & Penoel
1991
Lavender Lavandula angustifolia Dunn et al 1995
Rosewood Aniba rosaeodora Nacht & Ting 1921
Marjoram Origanum majorana Nacht & Ting 1921
Rose Rosa damascena Nacht & Ting 1921,
Rovesti & Columbo 1973
Lemon Citrus limon Komori et al 1995
Bergamot Citrus bergamia Komori et al 1995
Geranium Pelargonium graveolens Morris et al 1995
Roman chamomile Anthemis nobilis Rossi et al 1988, Moate
1995
Melissa Melissa officinalis Wagner & Sprinkmeyer
1973
Sandalwood Santalum album Kikuchi et al 1995

Komori et al (1995) demonstrated the positive effects of lemon oil (Citrus
limon) mixed with bergamot, sweet orange, and cis-4-hexanol on depressed inpa-
tients who were exposed to the fragrance for 4 to 11 weeks while their antide-
pressant medication was systematically reduced. By the end of the period, nine of
the 12 patients no longer needed antidepressant medication. Their levels of uri-
nary cortisol and dopamine became lower and were normalized with the citrus
aroma. The authors posited that inappropriate use of antidepressants could
weaken immune function.
Moate (1995) wrote of a patient suffering from depression who was treated
with Largactil and Sertraline (a tricyclic) but found profound relief from aro-
matherapy massage using lavender and chamomile. In another study, Sano et al
(1998) showed essence of cedarwood produced sedative effects on rats and re-
duced the time needed to achieve deeper stages of sleep in napping humans.
Templeton (2002) carried out a small study to investigate the effects of berg-
amot as an antidepressant. Ten volunteers from a natural-health clinic responded
to an advertisement to take part in a study on depression. Each agreed to take six
aromatic baths and six baths with no aroma. Subjects were to remain in the bath
for 20 minutes. While the study was self-monitoring, several subjects commented
on how this simple technique had empowered them. One wrote, “I experienced
an overwhelming feeling of tranquility.”
Vogley (2002) used bergamot in her study on anxiety in a psychiatric unit for
the elderly. A psychiatric nurse assessed each patient each morning for 10 days
and scored their level of anxiety on a scale of zero to 10. Then, bergamot was dif-
fused and the patients were reassessed. There was a notable difference in many of
the patients, which presented as enhanced communication and the ability to sit
still. One participant was hospitalized for depression and had been taking Lib-
rium for 20 years. It was decided to withdraw her from the drug. She was having
great difficulty sleeping and was feeling generally anxious. Several drops of
bergamot were placed on a cotton ball and put inside her pillowcase. The follow-
ing morning she reported it was the first good night’s sleep since she had stopped
taking Librium. She continued to use bergamot throughout her stay, and at dis-
charge she asked for and was given bergamot essential oil to take home with her,
along with instructions on how to use it.
A patient’s “pleasure memory” could have an effect even when the patient is
not fully conscious. Patients who have their chosen music played via headphones
during an operation need less medication postoperatively (Good et al 1999). Pa-
tients receiving aromatherapy using the “m” technique in a critical-care unit post-
operatively have experienced a decrease in their pain perception. Some patients
remember receiving the “m” technique when they recover consciousness. What
the patients probably remember is they received care in a manner they could rec-
ognize, even when they were not conscious. In today’s “managed care,” care seems
to be in danger of becoming marginalized simply because it is not on the reim-
bursement form. Ten years ago, when I was carrying out a pilot study on
254 Section II Clinical Use of Aromatherapy

post–open-heart surgery patients in an intensive-care unit in England, a patient
said, “You were the first person who didn’t hurt me.” That made a deep impres-
sion on me that has remained to this day. Health professionals do not want to
hurt their patients, but much of the time they do.
Talk with patients about the smells they enjoyed in their childhood and
about the smells they did not like. Were they brought up in the country, near a
wood? Have they traveled to far-away places? What kind of perfumes do they en-
joy? The answers to all of these questions will provide guidelines as to which es-
sential oils to use. This is a situation where, apart from trying to reduce the pa-
tient’s anxiety, the focus is also on giving pleasure in circumstances in which
pleasure is not often experienced.
Patients frequently experience a “high” of survival immediately after open-
heart surgery. This is often followed by a “low” of exhaustion. Touch and smell
can help a patient accept this rite of passage. Post-open-heart surgery patients
need to feel celebrated, whole, and held. They have survived one of the greatest
miracles orthodox medicine has to offer. Now it is time to help them to heal,
through the comforts of gentle touch and familiar smell.
Other Cardiac Uses for Aromatherapy
Claudia Ogden, RN, (2001) used aromatherapy on a 19-year-old girl with an in-
sufficient aortic valve as a result of a Streptococcus virus at the University of Michi-
gan’s Motts Children’s Hospital. The girl had had an initial repair at age 13. Dur-
ing open-heart surgery for this subsequent repair, she developed compartment
syndrome, which required fasciotomy. She was then required to be on bedrest, flat
on her back, while the skin grafts had an opportunity to take hold. During this
time she experienced considerable amounts of pain, anxiety, and depression.
Compounding her discomfort was constipation, and she was experiencing con-
siderable pain, anxiety, and profuse perspiration while attempting to have a bowel
movement.
Ogden was called in to see if clinical aromatherapy could help. She used
neroli floral water as a spray to immediately ease anxiety and then a 1% mixture
of frankincense and rose on the patient’s abdomen in a clockwise movement us-
ing the “m” technique. The same 1% mixture was also used on the patient’s hands
using the “m” technique. The patient calmed down a great deal. She was able to
cooperate better with the staff and required less pain medication. She managed a
bowel movement. The nurse showed the patient’s mother how to apply the aro-
matherapy mixture to her daughter’s foot or hand using the “m” technique when-
ever her daughter felt anxious. The mother reported being able to use aromather-
apy, and stated that the “m” technique had both comforted her daughter and
empowered her. The skin on the patient’s feet had become red and sore from
pushing against the sheets. After only two days, the dilute essential oils had soft-
ened and smoothed the girl’s heels, and all redness disappeared.
Chapter 14 Cardiology 255

Coumarins in Aromatherapy
There is some confusion over the possible anticoagulant effects of coumarins. A
synthetic chemical called dicoumarol forms the basis of warfarin, an anticoagu-
lant drug (Seth et al 1976). Dicoumarol is created naturally by the breakdown of
sweet clover plant but is created synthetically for the drug companies (Budavari
1996). However, a careful look at the chemical drawing of warfarin will uncover
a coumarin group within it (Bowles 2000). This does not mean an essential oil
containing coumarin could or would cause bleeding. Coumarins are present in
small amounts, less than 6%, in a few essential oils used in aromatherapy, and it
is extremely unlikely they would affect anticoagulant therapy, especially using 1-
5% dilutions on the skin. To put things into perspective, wintergreen, a common
flavoring in chewing gum and toothpaste, is also used in proprietary topical ap-
plications for sprains and strains. Wintergreen is almost all methyl salicylate and
as such is much more likely to increase the effect of anticoagulant therapy. De-
spite this, there are no warnings on chewing gum, so the risk must be extremely
small!
Unlike the commonly prescribed tranquilizer, droperidol, which caused fatal,
irregular heartbeats at far lower doses than expected (prompting the manufacturer
to enact a global withdrawal of the product), aromatherapy is a safe, gentle ther-
apy to use in cardiology that may well help a patient’s anxiety.
REFERENCES
Aftab K, Ur-Rahman A, Usmanghani K. 1995. Blood pressure lowering action of active
principle from Trachyspermum ammi. Phytomedicine. 2(1) 35-40.
Agshikar N, Abraham G. 1957. The effect of l-menthol on the systemic blood pressure.
Journal of the American Pharmaceutical Association. 46:82-84.
Akorm’s injectable droperidol gets FDA black box warning on Label. Jan. 2002.
http://www.mosbydrugconsult.com/drugconsult/newsaf2001.html –37.
Avollone R, Zanoli P, Corsi L et al. 1996. Benzodiazepine-like compounds and GABA
in flower heads of Matricaria chamomilla. Physiotherapy Research. 10:S177-S179.
Beauchamp K, Baker S, McDaniel C et al. 2000. Reliability of nurses’ neurological as-
sessments in the cardiothoracic surgical intensive care unit. American Journal of Criti-
cal Care. 10(5) 298-305.
Bimmel D, Mellert F, Ashraff O et al. Dec. 20, 2001. Does postoperative delirium syn-
drome promote sternal instability? Thoracic Cardioavascular Surgery. Thema: Perma-
nent Poster. www.theime.de/thoracic.abstracts2001/daten/pp6.html.
Bowles J. 2000. The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Publishing.
Budavari S (ed.). 1996. The Merck Index, 12th ed. Whitehouse Station, NJ: Merck.
Charron J. 1997. Use of Lavandula latifolia as an expectorant. The Journal of Alternative
& Complementary Medicine. 3(3) 211.
Danilowicz A, Gabriel H. 1971. Post cardiotomy psychosis in non-English-speaking pa-
tients. The International Journal of Psychiatry in Medicine. 2(4) 314-320.
256 Section II Clinical Use of Aromatherapy

Dunn C, Sleep J, Collett D. 1995. Sensing an improvement: an experimental study to
evaluate the use of aromatherapy, massage and period of rest in an intensive care unit.
Journal of Advanced Nursing. 21(1) 34-41.
Dunnington C, Johnson M, Finkelmeier B et al. 1988. Patients with heart rhythm dis-
turbances: variables associated with increased psychologic distress. Heart and Lung.
17:381-389.
Egerton N, Kay J. 1964. PPD and relationship problems. British Journal of Psychiatry.
110(RSM) 433-439.
Epstein R. Nov. 27, 2001. Facing up to depression after a bypass. New York Times. F8.
Franchomme P, Penoel D. 1991. Aromatherapie Exactement. Limoges, France: Jollois.
Freund D. 1999. Does ylang ylang inhalation have a hypotensive effect on unmedicated
resting blood pressure in individuals with borderline hypertension? Unpublished dis-
sertation, Hunter, NY: R J Buckle Associates.
Gattefosse R. 1937. (Translated in 1993 by R. Tisserand.) Aromatherapie: Les Huile
Essentielles-Hormones Vegetales (Gattefosse’s Aromatherapy.) Saffron Walden, UK:
CW Daniels, 89.
Good M, Stanton-Hicks M, Grass J et al. 1999. Relief of postoperative pain with jaw re-
laxation, music and their combination. Pain. 81(1-2) 163-172.
Gould L, Reddy R, Gomprecht R. 1973. Cardiac effects of chamomile tea. Journal of
Clinical Pharmacology. 13(11-12) 475-479.
Guba R. 2000. Toxicity myths. International Journal of Aromatherapy. 10(1/2)
37-50.
Herndon R (ed.). 1997. Handbook of Neurologic Rating Scales. New York: Demost
Medical Publishing.
Hill J, Brown R, Chu D et al. 1992. The Impact of Medicare Risk Program on the Use
of Services and Cost to Medicare. Princeton, NJ: Mathematica Policy Research, Inc.,
31-98.
Hope R, Longmore J, Hodgetts T et al. 1993. Oxford Handbook of Clinical Medicine,
3rd ed. Oxford, UK: Oxford University Press.
Jager W, Buchbauer G, Jirovetz L. 1992. Evidence of the sedative effect of neroli oil, cit-
ronella and phenylethyl acetate on mice. Journal of Essential Oil Research. 4(4)
387-394.
Kikuchi A, Shoj K, Nakamura S et al. 1995. Effect of fragrance on insomniac tendency
in healthy human subjects. In published conference proceedings, Vol. 1: Flavors, Fra-
grances, & Essential Oils. Istanbul. 15-19 October.
Komori T, Fujiwara R, Tanida M et al. 1995. Effects of citrus fragrance of immune func-
tion and depressive states. Neuroimmunomodulation. 2(3) 174-180.
Kovar K, Gropper D, Friess D et al. 1987. Blood levels of 1,8 cineole and locomotor ac-
tivity of mice after inhalation and oral administration of rosemary oil. Planta Medica.
53(4) 315-318.
Layne O, Yudofsky S. 1971. Postoperative psychosis in cardiotomy patients. New Eng-
land Journal of Medicine. 284(10) 518-520.
Lidster G. 2001. Retrieved Dec. 20, 2001, from www.leeds.ac.uk/students/ugmodules/
done3033.htm.
Lowe R. 1989. Anxiety in a coronary care unit. Nursing Times. 85(45) 61-63.
Macht D, Ting G. 1921. Experimental inquiry into the sedative properties of some aro-
matic drugs and fumes. Journal of Pharmacology and Experimental Therapeutics.
18(5) 361-372.
Chapter 14 Cardiology 257

Mahanna E, Blumenthal J, White W et al. 1996. Defining neuropsychological dysfunc-
tion after coronary artery bypass grafting. Annals of Thoracic Surgery. 61(5)
1342-1347.
Manger W, Gifford R. 2001. 100 Questions and Answers About Hypertension. New
York: Blackwell Science Inc.
Mann S. 1997. Healing Hypertension: Uncovering the Secret Power of Your Hidden
Emotions. New York: Wiley.
McCormick E. 1997. Psychological interventions for patients with heart disease. The
British Journal of Cardiology. 4(7) 268-271.
McCormick E. 1993. Healing the Heart. London: Optima.
McCormick E. 1997. Psychological interventions for patients with heart disease. British
Journal of Cardiology. 4(7) 268-271.
Moate S. 1995. Anxiety and depression. International Journal of Aromatherapy. 7(7)
18-21.
Morris N, Birtwistle S, Toms M. 1995. Anxiety reduction. International Journal of Aro-
matherapy. 7(2) 33-39.
Mulrow C, Lau J, Cornell J et al. 1997. Pharmacotherapy for hypertension in the elderly.
Cochrane Database Syst Rev. 2000(2):CD000028.
National Health Service Center for Reviews and Dissemination. 1999. The University of
York. 4(2) 1-8. Retrieved Dec. 20, 2001, from www.york.ac.uk/inst/crd/em42.htm.
O’Brien B. 1997.Experience with aromatherapy in the elderly. Journal of Alternative &
Complementary Medicine. 3(3) 211.
Ogden C. 2001. Personal communication.
Panossian A, Wikman G, Wagner H. 1999. Plant adaptogens III: Earlier and more re-
cent aspects and concepts of their mode of action. Phytomedicine. 6(4) 287-300.
Perez-Raya M, Utrilla M, Navarro M. 1990. CNS activity of Mentha rotundifolia and
Mentha longifolia essential oils in mice and rats. Phytotherapy Research. 4(6) 232-235.
Petty J. 2000. Surgery and complementary therapies: a review. Alternative Therapies in
Health and Medicine. 6(5) 64-74.
Roach G, Kanchuger M, Mangano C et al. 1996. Adverse cerebral outcomes after coro-
nary bypass surgery. New England Journal of Medicine. 335(25) 1857-1863.
Roberts R. 1991. Preventing PPD after surgery. Nursing. 4(6) 28.
Rogers W, Bowlby L, Chandra N et al. 1994. Treatment of myocardial infarction in the
USA (1990-1993): observations from the National Registry of Myocardial Infarction.
Circulation. 90(4) 2103-2114.
Rossi T, Melegari M, Blanchi A. 1988. Sedative, anti-inflammatory and anti-diuretic ef-
fects induced in rats by essential oils of varieties of Anthemis nobilis: a comparative
study. Pharmacological Research Communications. 20(Suppl. V) 71-74.
Rovesti P, Columbo E. 1973. Aromatherapy and aerosols. Soap, Perfumery and Cosmet-
ics. 46:475-477.
Saeki Y, Shihora M. 2001. Physiological effects of inhaling fragrances. International
Journal of Aromatherapy. 11(3) 118-125.
Sanders K, Glick R, O’Gara H et al. 1991. Failure to record delirium as a complication
of intra-aortic balloon pump treatment: a retrospective study. Paper presented at the
Annual meeting of the Academy of Psychosomatic Medicine, Georgia. Spring.
Sano A, Sei H, Seno H et al. 1998. Influence of cedar essence on spontaneous activity
and sleep of rats and human daytime naps. Psychiatry and Clinical Neuroscience. 8(6)
133-135.
258 Section II Clinical Use of Aromatherapy

Seth G, Kolate C, Varma K. 1976. Effect of essential oil of Cymbopogon citratus on cen-
tral nervous system. Indian Journal of Experimental Biology. 14(3) 370-373.
Sgura F, Scott-Wright R, Kopecky S et al. 2001. Length of stay in myocardial infarction.
Journal of Cost and Quality Association. 7(2) 1-17.
Stevensen C. 1994. The psychophysical effects of aromatherapy massage following car-
diac surgery. Complementary Therapies in Medicine. 2(1) 27-35.
Templeton J. 2002. How effective is bergamot as an anti-depressant? Unpublished dis-
sertation, Hunter, NY: R J Buckle Associates.
Thomas J. 1962. Peppermint fibrillation. Lancet. 222-223.
Tisserand R, Balacs, T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Viola H, Wasowski C, Levi de Stein M et al. Jun. 1995. Apigenin, a component of Ma-
tricaria recutita flowers, is a central benzodiazepine receptors ligand with anxiolytic ef-
fects. Planta Med. 61(3):213-216.
Vlay S, Fricchione G. 1985. Psychological aspects of surviving sudden cardiac death.
Clinical Cardiology. 8(4) 237-242.
Vogley G. 2002. Bergamot, anxiety and the elderly. Unpublished dissertation, Hunter,
NY: R J Buckle Associates.
Wagner H, Sprinkmeyer L. 1973. Pharmacological effect of balm spirit. Deutsche
Apotheker Zeitung. 113:1156-1166.
Wilson-Barnett J, Carrigy A. 1978. Factors influencing patients’ emotional reactions to
hospitalization. Journal of Advanced Nursing. 3(3) 221-229.
Yamada K, Miura T, Mimaki Y et al. 1996. Effect of inhalation of chamomile oil vapor
on plasma ACTJ level in ovariectomized rat under restriction stress. Biological &
Pharmaceutical Bulletin. 19(9) 1244-1246.
Chapter 14 Cardiology 259

260
W
15
Care of the Elderly
The body it crumbles. Grace and vigor depart.
There is now a stone where I once had a heart.
But inside this old carcass, a young girl still dwells,
And now and again my battered heart swells.
I remember the pain, and I remember the joys,
And I’m living and loving all over again.
And I think of the years, all too few, gone too fast,
And accept the stark fact that nothing will last.
So open your eyes, nurse, open and see, not a crabbed old woman.
Look closer. See me.
Anonymous—found in a nursing home after the author’s death
(cited in Montagu 1986)
I
mproved diet and medical breakthroughs have allowed humans to survive
longer and longer. The oldest woman thus far, Jeanne Calment, lived to the
age of 121 years. Therefore it is hardly surprising that many older people will
need care and, in some instances, supervision. It is a sad part of Western culture
that age is not revered, and those who could impart so much information and life
experience to younger members of society are frequently isolated in residential
homes. This is not to denigrate such institutions, as they are obviously much
needed, but to question why civilized society either cannot, or does not want to,
look after its elderly own. Indian and Asian families who have moved to the
United States often choose to maintain their cultural choice of extended family
living.

However, for many Westerners, the world has become such a busy place there
appears to be no time to nurture or just “be” with those whose sense of time has
gone. Cases of dementia and Alzheimer’s disease appear to be increasing.
Whether this increase is because humans are living longer or because factors that
may contribute to dementia are becoming more widespread is difficult to say.
Nearly 20% of those over 80 suffer from dementia. Nearly half of those over 85
suffer from Alzheimer’s disease. Some 4 million Americans are afflicted with
Alzheimer’s, and it is now the fourth leading cause of death among American
adults. The average amount of time from onset of symptoms until death ranges
from 3 to 20 years. Conventional treatment is with tacrine (Cognex) and
donepezil (Aricept): drugs that can temporarily improve the cognitive capabilities
but do not slow the progress of the disease (Weil 1997). Alzheimer’s disease is a
very difficult condition for relatives to accept. Several years ago, a family-practice
physician in New Mexico who was investigating dementia among the Native
American population commented that there was no record of Alzheimer’s disease
among the Navaho because “it just did not occur.” She believed this was possibly
because of genetic or environmental factors.
Until recently friends of mine ran a beautiful home for the elderly in the New
Forest area of England. The average age of the residents was 88.4 years. However,
the 82-year-old mother of one of the owners regularly came in to help on week-
ends. She was a sprightly, immaculately dressed lady, and she was older than many
of the residents she cared for. This seems to indicate age often has little to do with
aging. That residential home used aromatherapy regularly, and the immediate im-
pression on walking into the lobby was of a beautiful, caring atmosphere.
Aromatherapy and the Elderly
There is no doubt the elderly become forgetful. Certain plants from the Labiatae
and Asteracae family have long histories of use as restoratives of lost or declining
cognitive functions (Wake et al 2000). Extracts from Melissa and three Salvia
species were screened for contents able to displace (3H)-(N)-nicotine and (3H0-
(N) scopolomine from nicotinic and muscarinic receptors of human cerebral-cell
membranes. Melissa officinalis had the highest (3H)-(N)-nicotine displacement
value, and Salvia elegans had the highest (3H0-(N) scopolomine deplacement
value.
Helen Passant, a geriatric-nurse manager is recognized as one of the first
nurses to use aromatherapy in care of the elderly (Passant 1990). Buckwalter
(1992) a geriatric nurse researcher described Passant’s work as “giving new mean-
ing to the term holistic care. She and her staff were able to restore harmony, to
bring body and mind together and to allow the spirit to shine through.” Pa-
padopoulos et al (1999) carried out a qualitative assessment of the use of aro-
matherapy for older patients in a hospital in Birmingham, England. Each of
the 10 participants (six clients and four caregivers) were interviewed using a
semistructured interview to explore which part of a session they liked best and
Chapter 15 Care of the Elderly 261

what they perceived as benefits of essential oils of Lavandula angustifolia and
Chamaemelum nobile.
There are classic problems that can occur among elderly patients. These in-
clude sleep-pattern alteration, dementia, constipation, skin ulcers and poor heal-
ing, and osteoarthritis. Each condition can often be treated and improved with
aromatherapy.
Sleep Pattern Alteration and Insomnia
There have been a few published studies on aromatherapy and insomnia, and the
Lancet published a letter explaining one of the studies (Hardy et al 1995). Hardy
(1991) investigated the effects of lavender (Lavandula angustifolia) on four male
residents over a 6-week period and found all four men slept approximately the
same number of hours with lavender as they did with their previous conventional
sleep medication. The worst sleeper of the four men, who also presented noisy,
aggressive behavior during the day, appeared calmer. This could have been be-
cause of the lavender or the cessation of the sleep medication. Two of the other
men in the study no longer required naps during the day, presumably because they
were getting enough sleep at night. The lavender was cost effective: about
1
⁄
3
the
price of the sleep medication.
Hudson (1996) carried out a similar study on 51 patients using Lavandula
angustifolia for 14 days. Sleep pattern and daytime alertness were monitored.
During the first week, baseline measurements were taken. During the second
week, two drops of lavender were put on the pillow of each participant; no other
changes were made. Findings were an improved sleep pattern and increased alert-
ness during the day with a 50% reduction in confusion.
Cannard (1994) investigated the effects of a “commercially pre-mixed blend
of essential oils” on 10 patients in a nursing-development unit. Eight of the pa-
tients were aged over 70. In this study inhalation and hand massage were used.
Baseline sleep patterns were established over 94 nights. Then inhaled lavender
plus hand massage were introduced for two nights. On the third day, night seda-
tion was discontinued and sleep patterns were recorded for a further 94 nights.
Some patients required no sedation at all during the second 94-night period; only
one person requested night sedation every night. Ninety-seven percent of patients
felt they had a good night’s sleep. Although the paper itself did not reveal what
was in the mixture, another source reported it contained Ocimum basilicum CT
linalool, Lavandula angustifolia, and Origanum majorana (Price & Price 1999).
Remember, the wrong lavender (Lavandula latifolia or Lavandula stoechas)
will not produce a sedative effect and too much of even the right lavender (La-
vandula angustifolia) can exacerbate a patient’s insomnia. There could also be a
problem with overdoing it if too much lavender is put in an electric nebulizer, and
it is kept on incessantly. For some elderly people, lavender can be a disliked smell,
associated with death.
The learned memory of lavender can trigger negative images of dying rela-
tives or friends, as years ago lavender was used to protect linen from moths and
262 Section II Clinical Use of Aromatherapy

mold and every linen cupboard was liberally stacked with lavender bags. In all
cases, but especially with care of the elderly, it is important to allow patients to
choose their own aromas when possible. Memories are very individual, and smell
memories can be easily triggered (Ehrlichman & Halpern 1988).
Usha Rani & Naidu (1998) discuss the use of Nardostachys jatamansi (spike-
nard) to produce tranquility and sedation in conditions of insomnia and restless-
ness and cite Arora (1965) who suggests the sedative effect of spikenard is due to
the sesquiterpene ketone, jatamansone. Gupta and Virmani’s double-blind clini-
cal study on children (1968) found isolated jatamansone caused significant im-
provement in restlessness and aggressiveness in 28 hyperkinetic children com-
pared to amphetamine. This is interesting as jatamansone is identical in structure
to valeranone, the ketone in Valeriana officinalis (Lawrence 1989) thought to pro-
duce valerian’s sedative effect. Essential oil of spikenard also was found to produce
marked relaxation of skeletal muscles and central nervous system depression by
Bose et al (1957).
Sanderson and Ruddle (1992) found lavender and sweet marjoram were of-
ten offered as alternatives to Temazepan in an Oxford, UK, nursing-development
unit. The comment was that although lavender was effective when inhaled, it was
much more effective when given in a massage.
Studies are not limited to olfaction only. In two multiple-crossover studies,
each involving 12 female subjects, Schulz et al (1998) demonstrated that extract
of Lavandula angustifolia when taken orally produced a sedative effect only
slightly less sedative than diazepam. Lavender drops have been taken orally for
their digestive and relaxing properties for hundreds of years in Europe. Frankin-
cense was found to enhance the effect of barbiturates in a study on rats by Menon
and Kar (1971). Injected frankincense also appeared to have a sedative action on
its own and in high doses (300 mg/kg) to have an action comparable to 7.5 mg/kg
chlorpromazine. Suggested essential oils for insomnia are listed in Table 15-1.
Dementia
Dementia is present in 20% of individuals over 80 years of age (Jobst et al
1994). People who suffer dementia have been identified as a special-needs group
(Kilstoff & Chenoweth 1998). Although there are more than 50 different causes
of dementia, some of which are reversible, the majority are progressive and lead
to premature death. The most common cause of dementia in the developed world
is Alzheimer’s disease. Although Alzheimer’s can affect patients as young as 35
years of age, the most recent view is that this disturbing disease is part of a patho-
logical cascade process linked with aging (Jobst et al 1994a). In total, 70% of pa-
tients older than 65 who have dementia will have Alzheimer’s disease. Currently
there is no cure.
Olfactory dysfunction is thought to be a marker for detecting early
Alzheimer’s disease (Burns 2000). While aromatherapy is not a cure for demen-
tia, smell and touch are powerful messengers, often penetrating the fog of amne-
sia in a way words do not. Knasko and Gilbert (1990) suggest patients normally
Chapter 15 Care of the Elderly 263

unable to communicate would find it “refreshing to have a nonverbal interaction
with their environment.” Ho (1996) described the sensory-stimulation groups de-
veloped at Burton Hospital in Dudley, England. Odors were matched with col-
ors, such as lavender with shades of mauve and purple. Music associated with the
aroma was played, such as the nursery rhyme “Lavender Blue Dilly Dilly,” and pa-
tients had access to herbs and photographs connected with the aroma. In many
instances patients with dementia were able to make the correct connections.
Smith et al (1992) reported on ambient odor that elicited verbal memory in
a study of 47 college students with a mean age of 20.5 years (age range was 17-
25). The two odors used were jasmine incense and Lauren perfume. Superior
memory for the 24 words chosen was found when the odor present during the re-
learning session was the same as the odor present at the time of the initial learn-
ing, thereby demonstrating a context-dependent memory.
Flanagan (1995) reported on the use of a variety of essential oils to improve
atmosphere and behavior in institutionalized patients with Alzheimer’s. One pa-
tient, who was so combative he required sedation injections, changed dramatically
when a cotton ball with essential oil of lavender was pinned to his shirt lapel. Now,
he no longer needs medication if the cotton ball can be pinned to his shirt in time.
Kilstoff and Chenoweth (1998) reported on the effect of aromatherapy on patients
in a multicultural dementia day-care center in Australia for a period of 18 months.
They used a combination of lavender, mandarin, and geranium essential oils di-
264 Section II Clinical Use of Aromatherapy
Table 15-1 h Essential Oils for Insomnia
Common Name Botanical Name Reference
Neroli Citrus aurantium flos Jager et al 1992
Mandarin Citrus reticulate Kilstoff & Chenoweth 1998
Melissa Melissa officinalis Mitchell 1993
Angelica Angelica archangelica Franchomme 1991
Spikenard Nardostachys jaamansi Usah Rani 1998
Lemongrass Cymbopogon citrates Seth et al 1976
Lavender Lavandula angustifolia Flanagan 1995
Geranium Pelargonium graveolens Flanagan 1995
Mandarin Citrus reticulate Flanagan 1995
Roman chamomile Chamaemelum nobile Rossi et al 1988
Sandalwood Santalum album Kikuchi et al 1995
Rose Rosa damascene Brud & Szydlowska 1991
Sweet marjoram Origanum majorana Price & Price 1999

luted in a hand massage. Patients were thought to have become more alert and less
agitated, although it was unclear whether this was from the hand massage or the
essential oils. The use of aromathreapy appeared to have had a positive effect on
the staff and caregivers as well, possibly because of empowerment.
Smith (2000) studied the effects of inhaled lavender and sweet marjoram on
17 residents of the Northboro Senior Care Center in Northboro, Massachusetts.
Subjects who had memory-impaired agitation were chosen for the study, and
their relative or responsible party was approached for written consent. The most
frequent time for agitation was between 6 pm and 7:30 pm, and behavior ranged
from mild to severe agitation. The study took 9 weeks. During the first week, a
baseline was taken, and it was noted how many times the alarm was set off. (This
is a safety alarm set off when patients who cannot stand on their own attempt to
get out of their seats unaided.) For the next 4 weeks, essential oil of Lavandula
angustifolia was diffused into the meeting room 15 minutes prior to each session.
As of the fifth week, Origanum majorana (sweet marjoram) was diffused into the
meeting room 15 minutes prior each session. The whole residential-care team ob-
served subjects during the study to avoid bias. The team discussed the effects and
decided lavender had the best effect, as all subjects were able to remain engaged
with a marked decrease in agitation. No alarms went off during the lavender,
which was very unusual. Sweet marjoram appeared less effective.
MacMohan and Kermode (1998) found aromatherapy dramatically im-
proved motivational behavior in a 2-month study (n⫽1). However, not all stud-
ies have shown improvement in dementia. Brooker et al (1997) investigated the
effects of lavender inhalation and massage on four severely demented patients and
found two patients became severely agitated. The lavender may have evoked dis-
tressing memories, or perhaps they did not like being massaged.
In cases where patients cannot or will not remain stationary, walking along-
side them while simultaneously conducting a gentle, hand “m” technique can lead
to some positive changes in the patient, such as renewed eye contact and speech
coherence. In cases in which patients are confined to bed and incapable of walk-
ing or are violently resistant to any form of touch, vaporizers and nebulizers can
be used. Even in instances such as these, when it seems the patient will be unable
to help with the selection of an aroma, offering a choice of two different smells
can elicit a response. Laraine Kyle, MSN, in Boulder, Colorado, has done much
to introduce aromatherapy into the geriatric setting in the United States. She
writes aromatherapy can help “transport Alzheimer patients to memories of their
past. Seeing facial expressions change from mask-like to animated smiles is feed-
back enough to know that something is happening” (Kyle 1996).
Mitchell (1993) used melissa and lavender in a randomized, controlled
crossover study of 12 patients with Alzheimer’s aged between 64 and 91 at a res-
idential and day-care unit. Six drops of lavender were added to the morning wash.
A 3% solution of melissa was applied to the patients’ chins at midday, and three
drops of lavender were applied to their pillows at night. Mild behavioral and ver-
bal improvements were observed.
Chapter 15 Care of the Elderly 265

Other suitable essential oils are those the patients might be familiar with ei-
ther from their childhood or from positive life experiences. For example,
Trumpers, possibly the oldest gentlemen’s hairdressers in London, has used es-
sential oil of geranium (Bourbon) in their pomade for more than 100 years (Free-
man 1996).
Rosmarinus officinalis CT cineole or borneol (rosemary) will be remembered
by most elderly patients as a common ingredient in cooking and from gardening.
“There’s rosemary—that’s for remembrance” said Shakespeare’s Ophelia, and it is
a valid comment. Rosemary is traditionally thought to be helpful as a memory
aid. Suggestions for other aromas to try are listed in Table 15-2. There are in no
particular order. If a patient has lived in India or Asia, lemongrass, ginger, or ylang
ylang might be appealing and soothing.
Dales Occupational Therapy Service in Derbyshire, United Kingdom, used
aromatherapy to improve the quality of life of their Alzheimer’s patients. Essen-
tial oils they found useful include pine, eucalyptus, and peppermint to trigger
conversation and memory and lavender and geranium to trigger thoughts of
cooking and plants (Henry 1993).
266 Section II Clinical Use of Aromatherapy
Table 15-2 h Essential Oils for Dementia
Common Name Botanical Name
Geranium Pelargonium graveolens
Lavender Lavandula angustifolia
Sandalwood Santalum album
Patchouli Pogostemon patchouli
Clary sage Slavia sclarea
Rose Rosa damascene
Lavender Lavandula angustifolia
Mandarin Citrus reticulate
Geranium Pelargonium graveolens
Rosemary Rosmarinus officinalis
Melissa Melissa officinalis
Peppermint Mentha piperita
Eucalyptus Eucalyptus globules
Ginger Zingiber officinalis
Ylang ylang Cananga odorata var. genuine

Constipation
The slowed-down passage of food through the large intestine may be a result of
reduced exercise or insufficient roughage in the diet. The latter could be due to
poor appetite for various reasons ranging from ill-fitting dentures to boredom
with institutional food. Another cause of constipation is regular use of night se-
dation.
One of the simplest and most gentle ways to ease constipation is through ab-
dominal massage using essential oils. This is effective for mild constipation. A
slight improvement was documented in a study by Klauser et al (1992), although
in that instance no essential oils were used. In the residential home owned by my
friends, this form of massage produced very good results and was used success-
fully for several years. See Table 15-3 for a list of essential oils Barker (1995) sug-
gests for treating constipation.
Use a 3% solution (three drops of essential oil/s in 5ccs of cold-pressed veg-
etable oil). Let the patient choose which oil to use from the selection in Table
15-3. Work slowly and rhythmically up the ascending colon, along the transverse
colon, and down the descending colon, paying attention to both hepatic and
splenic flexures. This gentle massage only takes 5 minutes, but it can be really use-
ful. It is best repeated up to five times a day or until relief is obtained.
Skin Ulcers and Slow Healing
Aging slows down the body’s ability to heal. Skin becomes thinner and more frag-
ile, and the slightest knock can cause a deep bruise, especially if the person is tak-
ing steroids. Very gentle massage with cold-pressed vegetable oils, such as oil of
evening primrose, can aid the elasticity of aging skin, and certain essential oils can
enhance aging skin’s ability to heal. Alan Barker, a clinical aromatherapist em-
ployed by the British National Health Service, has used floral waters to irrigate
wounds (Barker 1994). Table 15-4 lists some floral waters used for this purpose.
Floral waters are the byproduct of steam distillation and can be obtained from
many essential-oil suppliers. Slightly acidic, they are refreshing to use, smell
lovely, and are excellent for skin care. (Floral waters are slightly acidic because
they contain parts of the essential oil that are most soluble.) When using floral
Chapter 15 Care of the Elderly 267
Table 15-3 h Essential Oils for Constipation
Common Name Botanical Name
Black pepper Piper nigrum
Ginger Zingiber officinale
Fennel Foeniculum vulgare
Marjoram Origanum marjorana
Grapefruit Citrus paradisi

water, make sure the distributor can supply an analysis to prove the floral water is
not contaminated with bacteria or fungi.
After irrigating the wound, a compress soaked in diluted essential oils can be
applied to aid healing. The essential oils will also reduce the chance of infection.
Apply a fresh compress twice daily, or every 4 hours if the wound is infected. Ar-
eas immediately around the wound can be gently swabbed with oil of evening
primrose or Rosa rubiginosa. Another excellent oil to use around the wound would
be a macerated oil such as Hypericum perforatum (St John’s wort) or calendula
(Calendula officinalis).
Glowania et al (1987) found Matricaria recutita (German chamomile) effec-
tive in a controlled, double-blind study of slow-healing wounds in 14 patients. A
further article, in the Journal of Tissue Viability in 1993, reported on two case stud-
ies using lavender and tea tree (Hitchin 1993). Thorne (1996) described the use of
3% oil of Lavandula angustifolia in a carrier oil of rosehip (Rosa rubiginosa) on a leg
ulcer measuring 1.5 cm by 1 cm. After one month of applying the lavender solu-
tion to the area around the wound (not the wound itself), the wound was smaller
(1cm by 1cm), and the whole area looked much healthier. It is not clear why the
mixture was not applied to the wound itself. However, after tea tree was added to
the dilution, the wound became inflamed, and a course of antibiotics was pre-
scribed. This may have been due to an allergy to the tea tree. There is no indica-
tion a patch test was taken. Two months later the wound had healed, but there is
no indication that this was due to the antibiotic rather than the essential oils.
Emeny (1994) reported on a 90-year-old woman with a diabetic foot ulcer
that had become gangrenous: amputation was scheduled. Undiluted tea tree was
applied to the ulcerated lesion between her toes in the form of soaks for 1 week.
Her pain level decreased, and there was marked physical improvement. Tea tree
was continued in a 10% solution, decreasing to 3% over the next 3 weeks. The
foot gradually became warmer. Continuing tea tree at 3% for 9 weeks, the wound
healed completely, and there was no evidence of gangrene. Belaiche (1985) a
French physician, used undiluted tea tree daily on intertrigo under the breasts and
in the groin and underarm with disappearance of all lesions within 2 months.
Ron Guba (1999) reported on the rapid healing of dermal wounds using his
own essential oil-based cream (See Table 15-5 for details.) on selected patients in
six nursing homes in Australia. Wounds were divided into two groups: skin tears
268 Section II Clinical Use of Aromatherapy
Table 15-4 h Floral Waters Used to Irrigate Wounds
Common Name Botanical Name
Niaouli Melaleuca viridiflora
Tea tree Melaleuca alternifolia
German chamomile Matricaria recutitia
Grapefruit Citrus paradisi

received once-a-day treatment, while pressure-area and venous ulcers received
treatment twice a day. Treatment consisted of putting the cream onto dry gauze
and taping it over the wound. Detailed accounts of seven patients (aged 58-93)
are given. All wounds healed, some within a week. This was remarkable as some
of the wounds had been in stasis for several months. Guba also conducted a
punch-biopsy, controlled study on five subjects who each sustained two wounds.
The wounds treated with Guba’s cream healed within an average of 12 weeks.
The control wounds took an average of 26 weeks.
My own clinical experience confirms the excellence of Guba’s wound-
healing cream. I have also found frankincense very beneficial to superficial
wounds and scars, and palma rosa is good for deeper wounds.
Finally, essential oils that contain high percentages of ketones are thought to
be beneficial in wounds and may help reduce cheloid scars. This process may be
accelerated if the carrier oil used is Rosa rubiginosa (rosehip).
Osteoarthritis
Degenerative joint pain is frequently part of the aging process, especially if there
is a family history of rheumatism. As secondary changes occur in the underlying
bone, pain and impaired function make life a misery for those who were once ag-
ile. This is particularly the case if one of the affected joints has been injured.
Chapter 15 Care of the Elderly 269
Table 15-5 h Guba’s Wound-Healing Cream (reprinted with permission)
Common Name Botanical Name Concentration
True lavender Lavandula angustifolia 40 mg/g
Mugwort Artemesia vulgaris 10 mg/g
Sage Salvia officinalis 10 mg/g
Everlasting Helichrysum italicum 18 mg/g
German chamomile Matricaria recutita 12 mg/g
Calendula Calendula officinalis 10 mg/g
Tamanu Calophyllum inophyllum vegetable oil 62.5 mg/g
Borage Borago officinalis vegetable oil 62.5 mg/g
Flaxseed Linum usitatissimum vegetable oil 62.5 mg/g
Shea butter Butrospermum parkii vegetable oil 62.5 mg/g
Grapefruit seed Citrus paradisi (as preservative) 5.0 mg/g
Rosemary Rosmarinus officinalis CT cineole CO
2
0.125 mg/g
(antioxidant)

Extract of ginger was found to be marginally effective in a randomized, con-
trolled crossover study by Bliddel et al (2000). While in the crossover period no
statistical difference could be demonstrated, during the first explorative period gin-
ger was found to be better than the control. The extracts were taken orally, which
may have contributed to the poor results. Ginger foot baths and compresses are
very good for both feet and knees; use CO
2
extract that contains gingerol.
Cote (2002) investigated the effect of topically applied Piper nigrum (black
pepper) on 11 self-selected subjects (10 women and one man) who were members
of Panorama City Retirement Community in Lacy, Florida. Following baseline
measurement of pain using a visual analog, a 4% dilution of black pepper in 5 ml
of grapeseed oil was massaged into the painful joint of each subject (7 hands, one
knee, one shoulder, one ankle, one foot). After the massage, the subjects were
asked to rate their pain immediately, then again after 2 hours and after 4 hours.
There was a slight reduction in perception of pain for most participants. It is dif-
ficult to assess whether the reduction was due to the massage or the essential oil.
Macdonald (1995) wrote about elderly patients and osteopathic pain. The
following essential oils were used in her study: eucalyptus, juniper, marjoram, and
rosemary. Unfortunately, no botanical names were given, so it is impossible to as-
sess which essential oils were actually used (there are 400 different types of Euca-
lyptus). Traditional essential oils for osteoarthritic pain are rubefacient ones that
will dilate the capillaries and give a peripheral warming effect. One such essential
oil is black pepper. An antiinflammatory essential oil such as German chamomile
or immortelle (Helicrysum italicum) can give relief, as can an analgesic essential oil
such as lavender or peppermint. For more information on antiinflammatory es-
sential oils, please see the section of Chapter 12 on inflammation. For more in-
formation on analgesic essential oils, please see the section of Chapter 12 on pain.
Franchomme and Penoel (1991) state that p-cymene has analgesic properties
and is particularly suited to osteoarthritis. Paracymene is present in cajeput
(6.8%), summer savory (7%), and Thymus vulgaris (21.9%) (Bowles 2000), al-
though at these low percentages it is dubious that the cymeme will have much
impact.
I have found Cymbopogon citratus (lemongrass) useful for alleviating os-
teoarthritic pain using a 5% compress. Lemongrass may be analgesic due to its
myrcene content (Lorenzetti et al 1991). Satureja hortensis (summer savory) is also
useful for pain, and it contains a small amount of myrcene.
Perhaps it would be pertinent to end this section with a mention of essential
oils for aging. Deans (1991) conducted substantial research into the properties of
polyunsaturated fatty acids (PUFAs) at Warwick University in England. PUFAs
form part of plant oils and are used by the human body to make cellular compo-
nents and steroid hormones. Aging is associated with a decline in PUFAs. In re-
search on aging rats, essential oils were found to restore PUFA levels almost to
the levels observed in young mice. Of the essential oils tested, red thyme and
clove appeared to give the most impressive results (Deans 1991).This research in-
volved feeding the rats essential oils by mouth. There is no suggestion we do the
270 Section II Clinical Use of Aromatherapy

same for our patients or ourselves, but the antiaging properties of essential oils
may turn out to be an exciting area. In the meantime, both West (1993) and Kyle
(1999) suggest aromatherapy can be integrated into care of the elderly very sim-
ply, and many health professionals are following her lead.
REFERENCES
Arora R. 1965. Nardostachys jatamansi: a chemical, pharmacological and clinical ap-
praisal. Special Report Series No 51. New Delhi, India: Indian Council of Medical
Research.
Barker A. 1994. Pressure sores. Aromatherapy Quarterly. 41:5-7.
Belaiche P. 1985.Treatment of skin infections with the essential oil of Melaleuca alternifo-
lia. Phytotherapy. 15:15-17.
Bliddel H, Rosetzsky A, Schlinchting P et al. 2000. A randomized placebo controlled
cross-over study of ginger extracts and ibuprofen in osteoarthritis. Osteoarthritis and
Cartilage. 8(1) 9-12.
Bose B, Gupta S, Bhatnagar J et al. 1957. Nardostachys jatamansi DC: its sedative and
depressant action as estimated by Warburg technique. Indian Journal of Medical Sci-
ence. 11:803-804.
Bowles E. 2000. The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Printers.
Brooker D, Snape M, Johnson E et al. 1997. Single case evaluation of the effects of aro-
matherapy and massage on disturbed behavior in severe dementia. British Journal of
Clinical Psychology. 36(Part 2) 287-296.
Brud W, Szydlowska I. 1991. Bulgarian rose otto. International Journal of Aromather-
apy. 3(3) 17-19.
Buckwalter K. 1992. Geropsychiatry: confessions of a geriatric nurse researcher. Journal
of Psychosocial Nursing. 30(6) 38-39.
Burns A. 2000. Might olfactory dysfunction be a marker for early Alzheimer’s disease?
Lancet. 355(9198) 84-85.
Cannard G. 1995. On the scent of a good night’s sleep: trial project. Nursing Standard.
9(34) 21-22.
Cote S. 2002. The effects of essential oils of black pepper on arthritis. Unpublished dis-
sertation, Hunter, NY: R J Buckle Associates.
Deans S. 1991. More life in your years. International Journal of Aromatherapy. 3(4) 20-22.
Ehrlichman H, Halpern J. 1988. Affect and memory: effects of pleasant and unpleasant
odor on retrieval of happy and unhappy memories. Journal of Personality and Social
Psychology. 55(5) 769-779.
Emeny P. 1994. Diabetic gangrene in case studies. International Journal of Aromather-
apy. 6(4) 23.
Flanagan N. 1995. The clinical use of aromatherapy in Alzheimer’s patients. Alternative
& Complementary Therapies. 377-380.
Franchomme P, Penoel D. 1991. Aromatherapie Exactement. Limoges, France: Jollois.
Freeman G. 1996. Personal communication.
Glowania H, Raulin C, Svoboda M. 1987. Effect of chamomile on wound healing: a
clinical double-blind study. Zeitschrift fur Hautkrankheiten (Berlin). 62(17) 1267-
1271.
Chapter 15 Care of the Elderly 271

Guba R. 1999. Wound healing. International Journal of Aromatherapy. 9(2) 67-74.
Gupta B, Virmani V. 1968. Clinical trial of jatamansome in hyperkinetic behavior disor-
ders. Neurology (India). 16(4) 168-173.
Hardy M. 1991. Sweet scented dreams. International Journal of Aromatherapy. 3(2)
12-13.
Hardy M, Kirk-Smith M, Stretch D. 1995. Replacement of drug treatment for insomnia
by ambient odour (letter). Lancet. 346(8976) 701.
Henry J. 1993. Dementia. International Journal of Aromatherapy. 5(2) 27-29.
Hitchin D. 1993. Wound care and the aromatherapist. Journal of Tissue Viability. 3(1)
56-57.
Ho C. 1996. Stirring memories through all the senses. Journal of Dementia Care. 4(4)
15.
Hudson R. 1996. The value of lavender for rest and activity in the elderly patient. Com-
plementary Therapies in Medicine. 4(1) 52-57.
Jager W, Buchbauer G, Jirovetz L. 1992. Evidence of the sedative effect of neroli oil, cit-
ronella and phenylethyl acetate on mice. Journal of Essential Oil Research. 4(4) 387-
394.
Jobst K, Hindley N, Pearce M. 1994. Clinical investigation and therapeutic aspects of
Alzheimer’s disease. Continuing Medical Education. 12:401-412.
Jobst K, Smith A, Szatmari M. 1994a. Rapidly progressing atrophy of medial temporal
lobe in Alzheimer’s disease. Lancet. 343(8901) 829-830.
Kikuchi A, Shoji K, Nakamura S et al. 1995. Effects of fragrance on insomniac tendency
in healthy human beings. In published conference proceedings, Vol. 1: Flavors, Fra-
grances & Essential Oils. Istanbul. 15-19 October.
Kilstoff K, Chenoweth L. 1998. New approaches to health and well-being for dementia
day-care clients, family carers and day-care staff. International Journal of Nursing
Practice. 4(2) 70-83.
Klauser A, Flaschentrager J, Gehrke A et al. 1992. Abdominal wall massage: effect of
colonic function in healthy volunteers and in patients with chronic constipation.
Zeitschrift fur Gastroenterologie. 30:247-251.
Knasko S, Gilbert A. 1990. Emotional state, physical well-being and performance in the
presence of feigned ambient odor. Journal of Applied Social Psychology. 20(16) 1345-
1357.
Kyle L. 1996. Clinical uses of aromatherapy. Aromatic Thymes. 4(1) 13-15.
Kyle L. 1999. Aromatherapy for elder care. International Journal of Aromatherapy. 9(4)
170-176.
Lawrence B. 1989. Essential Oils: 1981-1987. Carol Stream, IL: Allured Publishing,
116.
Lorenzetti B, Souza G, Sarti S, Gehrke A et al. 1991. Myrcene mimics the peripheral
analgesic activity of lemongrass tea. Ethnopharmacology. 30(4) 43-48.
Macdonald E. 1995. Aromatherapy for the enhancement of the nursing care of elderly
people suffering from arthritis. Aromatherapist. 2:26-31.
MacMohan S, Kermode S. 1998. A clinical trial of the effect of aromatherapy on moti-
vational behavior in a dementia care setting using single subjects. Australian Journal of
Holistic Nursing. 5(2) 47-49.
Menon M, Kar A. 1971. Analgesic and psychopharmacological effects of the gum resin
of Boswellia serrata. Planta Medica. 19(4) 333-341.
Mitchell S. 1993. Dementia. International Journal of Aromatherapy. 5(2) 20-24.
272 Section II Clinical Use of Aromatherapy

Montagu A. 1986. Touching: The Human Significance of Skin. New York: Perennial.
Papadopoulos A, Wright S, Ensor J. 1999. Evaluation and attributional analysis of an
aromatherapy service for older adults with physical health problems and carers using
the service. Complementary Therapies in Medicine. 7(4) 239-245.
Passant H. 1990. A holistic approach in the ward. Nursing Times. 86(4) 26-28.
Price S, Price L. 1999. Aromatherapy for Health Professionals. London: Churchill Liv-
ingstone, 233.
Rossi T, Melegari M, Blanchi A. 1988. Sedative, anti-inflammatory and anti-diuretic ef-
fects induced in rats by essential oils of varieties of Anthemis nobilis: a comparative
study. Pharmacological Research Communications. 20(Suppl. 5) 71-74.
Sanderson H, Ruddle J. 1992. Aromatherapy and occupational therapy. British Journal of
Occupational Therapy. 55(8) 310-314.
Schulz H, Jobert M, Hubner W. 1998. The quantitative EEG as a screening instrument
to identify sedative effects of single doses of plant extracts in comparison to Di-
azepam. Phytomedicine. 5(6) 449-458.
Seth G, Kolate C, Varma K. 1976. Effect of essential oils of Cymbopogon citratus on cen-
tral nervous system. Indian Journal of Experimental Biology. 14(3) 370-373.
Smith D, Standing L, de Man A. 2002.Verbal memory elicited by ambient odor. Percep-
tual and Motor Skills. 74(2) 339-343.
Thorne D. 1996. Healing ulcers using essential oils. Journal of Community Nursing.
10(9) 14-16.
Usha Rani P, Naidu M. 1998. Subjective and polysomnographic evaluation of an herbal
preparation in insomnia. Phytomedicine. 5(4) 253-257.
Wake G, Court J, Pickering A et al. 2000. CNS acetylcholine receptor activity in Euro-
pean medicinal plants traditionally used to improve failing memory. Journal of
Ethnopharmacology. 69(2) 105-114.
Weil A. 1997. Preventing Alzheimer’s. Dr. Andrew Weil’s Self-Healing. 1, 6.
West B. 1993. The essence of aromatherapy. Elderly Care. 5(4) 24-25.
Chapter 15 Care of the Elderly 273

274
W
16
Critical Care
We may need to be cured by flowers.
Sharman Russell
Anatomy of a Rose
C
ritical care encompasses patients with grave, long-term medical condi-
tions, those with acute myocardial infarctions who will have shorter stays,
and patients who have had major surgery. The one common factor will be
the gravity of their condition. Patients in critical care experience one of the most
stressful times in their lives (Dunn et al 1995). Often unable to breathe unaided,
their survival depends on the experience and expertise of their professional care-
givers. Communication and trust play a large role in the patient-caregiver rela-
tionship. Ingham (1989) suggests communication should be “written in to a pa-
tient’s care-plan.” Touch is a communication skill that can enhance trust.
Ashworth (1984) wrote about the importance of teaching nonprocedural touch,
commenting “it was more difficult to learn than defibrillation and cardiopul-
monary resuscitation and at least as valuable.”
A critical-care nurse who experienced being intubated as a patient in a
critical-care unit described how “her worst nightmare came true.” She felt “aban-
doned and longed for someone to reassure her.” Following her experience she un-
derstood “why it was sometimes necessary to hold a patient’s hand” (Urden 1997).
It is greatly underestimated how important it is for intensive-care unit patients to
feel trust and confidence in their caregivers. Nonprocedural touch and pleasant
aromas can do much to relive anxiety and give comfort in what is perceived by pa-
tients to be a “hostile environment” (Welsh 1997). Essential oils can be used in
many ways in a critical-care unit: from relieving the pain of intravenous insertions
to alleviating bronchial spasm to reducing anxiety (Buckle 1998).

Most of the published research has focused on physical parameters that can
be easily measured. These physical tools have not always conveyed what the pa-
tients have said if their perception of anxiety, pain, or stress have been relieved.
This could be because a more accurate tool, such as measuring blood or saliva cor-
tisol levels, has been too expensive for most nursing studies. However this would
be an excellent area of study for the future.
Aromatherapy in a Critical-Care Setting
Dunn et al (1995) reported on the effects of reducing stress using a gentle mas-
sage with of 1% lavender (Lavandula angustifolia) on 122 patients in an intensive-
care unit at Battle Hospital in Reading, United Kingdom. Patients were randomly
assigned to three groups: one with plain massage, one with massage plus 1%
lavender, and one with rest for 30 minutes. The areas of massage depended on the
areas available and lasted between 15 and 30 minutes (mean time 16.5 minutes).
The age of participants ranged from 2 years to 92 years. Physiological and psy-
chological measurements were taken before and after the treatment. Although
there appeared to be no difference between the group that received massage with
and without an essential oil, this could be because the percentage used was very
low. or it could be because when patients fell asleep during the aromatherapy
massage they were not awakened! (Dunn 1996). However, the comments indi-
cated all patients were very appreciative of the extra care they received. One pa-
tient who had received the aromatherapy massage commented, “Aromatherapy
made me feel clean and like a whole person.”
Woolfson and Hewitt (1992) used foot massage with 1% lavender in their
study of 36 patients in a medical and surgery critical-care unit at the Royal Sus-
sex County Hospital in the United Kingdom. Each patient was randomly as-
signed to three groups. The groups received either a 20-minute massage without
oil, 20-minute massage with oil, or a 20-minute rest. Two treatments per
week were given for 5 weeks. This means the majority of patients would have
been medical (as surgical patients tend not to stay that long). The massage-with-
lavender group showed the greatest benefits with a consistent decrease in blood
pressure, heart rate, respiration, and anxiety. Patients in the lavender group per-
ceived their stress as being less than patients in the control group.
Stevensen (1994) reported on the effects of a 2.5% neroli (Citrus aurantium
flos) foot massage on 100 patients in the critical-care unit at Middlesex Hospital
in London, England. In this study patients were randomly assigned to one of four
groups: massage with neroli, massage with plain oil (apricot kernel), a rest period,
or nothing. Results indicated the neroli group perceived they were less stressed,
although there were only small differences in physical measurements.
In my study (Buckle 1993) Lavandula x intermedia (lavandin) was used as a
control because at that time it was thought to have little therapeutic effect. The
study was to find out if aromatherapy had an effect beyond that of massage.
Lavandula angustifolia was chosen for the experimental group. Two-percent
Chapter 16 Critical Care 275

solutions of Lavandula angustifolia and Lavandula x intermedia, (called Lavandula
burnati by Frachomme and Penoel 2000) were supplied by the Fragrant Earth
Co. Ltd. The company labeled the solutions Lavender A and Lavender B.
At 2% dilution it was impossible to tell which lavender was which, so the in-
vestigator was blind to the intervention, and so were the patients. Each patient
was randomly allocated to one of two groups. Following analysis, it did appear
one of the lavenders was more effective at reducing respiration rate than the other
one. When the identity of the experimental group lavender was revealed, it was
lavandin, and it appeared to be twice as effective as Lavandula angustifolia. The
results were rechecked as they appeared to contradict what was being taught
about lavandin. This also indicated the relaxation was not simply due to massage
as there was a difference between the two groups. One of the comments made was
“You were the first person who didn’t hurt me.” Another was, “Why send flowers
and cards if you can send this?” Others were, “I feel like you really cared about
me,” and “I felt like I was important, not just a number, and that you really would
take care of me,” and “Until you did that, I was really scared, but you made me
feel it would be OK to relax.”
Waldman et al (1993) suggested the following essential oils would be useful
in a critical-care setting: lavender, clary sage, jasmine, peppermint, rose, rosemary,
tea tree, and ylang ylang. The oils were used in a 2% massage solution and in elec-
tric burners. Others could include neroli, Roman chamomile, sandalwood, lemon,
lemongrass, and palma rosa. Mitchell (2002), a critical-care nurse, has used aro-
matherapy in her unit for several years. She suggests frankincense, geranium, pe-
titgrain, sweet marjoram, mandarin, juniper, and German chamomile.
Each patient is someone’s child, no matter how old he or she is. Most pa-
tients in an intensive-care unit are frightened, no matter how brave they try to ap-
pear. Each patient belongs, in some capacity, to another, and the others are also
in need of nurturing. Critical-care units can be very frightening for relatives, with
so many tubes and complicated machinery around the motionless body of a loved
one. Mitchell (2002) writes relatives are often stunned by the intensive-care unit,
and they are very appreciative when their loved ones receive the loving care aro-
matherapy provides.
I remember seeing my father in a critical-care unit many years ago, and more
recently my brother-in-law, and experiencing some of the feelings of helplessness
many relatives and visitors feel even though I had trained and worked in critical
care for many years. Often relatives feel there is nothing they can do except wait
and pray. Aromatherapy presents a wonderful opportunity to give the family a
sense of control and a simple way to contribute and promote comfort and quality
of care for their loved one.
The gentle, stroking movements of the “m” technique, which can be used to
apply dilute essential oils, are extremely simple both to teach and to learn. I taught
them to a 5-year-old granddaughter who spent almost an hour lovingly stroking
her grandfather’s hands. Her sad, cross little face softened as she sang gently
under her breath, moving her hands in time to her lullaby. Her parents watched
276 Section II Clinical Use of Aromatherapy

her as she worked, amazed at the transformation. This little girl knew she had
been given an important task, one that not only empowered her but was actually
of therapeutic value.
Teaching relatives to touch in this way does not take very long—probably
only 5 minutes. Everyone can find that amount of time. Talking with relatives
about the aromas patients enjoyed before they came into hospital allows dialogue
on a safe subject, but one still linked to the patient. Finding an aroma relatives
feel could help their loved ones gives them something to think about and a way
of becoming involved. It is best to offer just a few aromas known to have relaxing
effects. The floral aromas are usually popular. The rose essential oil used on my
brother-in-law in Papworth Hospital in Cambridge, England, produced a smile
even though he was extremely ill and was appreciated by the staff who gravitated
toward the lovely smell.
Clinical aromatherapy has much to offer critical care as it reveals the softer,
more caring side of a hard, mechanistic world. In a place full of technical equip-
ment, aromatherapy allows patient and health provider a chance to get in touch
with their feelings, to trust, and to communicate. Human beings often forget how
to “be” as they are programmed to “do.” The transition from doing to being can
be a hard one to learn, but in the learning, both patient and health provider can
share in the healing process at a much deeper level. In critical care, patients have
to be. Aromatherapy enables patients to feel better as well as get better. That is
the essence of holistic care. Anxiety, pain, insomnia, and stress are major areas in
which aromatherapy could help in a critical-care setting. These have been covered
in-depth in other chapters of the book, so please refer to the index for more in-
formation. The remaining sections of this chapter address other specialized areas
of critical care where aromatherapy could be of use.
Extubation
Extubation is an alarming procedure for a patient who needs to be awake enough
to breathe without assistance, but sedated enough not to fight the endotracheal
tube. Tremendous trust is needed. Aromatherapy using the “m” technique can help
produce a deep level of trust in a very short period of time. Just because a patient
is intubated does not mean aromatherapy will have no effect. Drugs such as fen-
tanyl, scopolamine, and clonidine are absorbed through the skin. Some compound
pharmacists for hospice care are even putting Ativan and other commonly used
prescription drugs into a gel for topical delivery. Components within essential oils,
such as linalyl acetate and linalool, are also absorbed through the skin.
During extubation, fear of oversedation can be a common cause of inadequate
pain- and anxiety-relief. Aromatherapy has no side effects and can actually facili-
tate extubation by promoting relaxation, decreasing anxiety, relieving pain, and
promoting trust between patient and caregiver. After extubation, clearance of se-
cretions can be greatly aided by the skilled use of mucolytic essential oils, such as
Eucalyptus globulus or Lavandula latifolia, which can be inhaled by the patient.
Mitchell (2002) found it was possible to decrease the amount of opioid narcotics
Chapter 16 Critical Care 277

needed while enhancing pain relief with the use of the “m” technique and essential
oils. She suggests applying essential oils to the skin with the “m” technique can al-
ter the pain pathway by affecting the transduction, perception, and modulation of
nociceptive (somatic and visceral) pain. For example, an application of an anti-
spasmodic essential oil, such as Roman chamomile, clary sage, or lavender, can
minimize the transduction phase of nociception by minimizing the effects of sen-
sitizing substances, such as prostaglandin, bradykinin, serotonin, and substance P,
which are released at the periphery. Mitchell (2002) has found aromatherapy in a
critical-care unit reduces stress, anxiety, fear, and insomnia, improves mood, pro-
motes relaxation, enhances coping, and increases a patient’s sense of control, all
without side effects.
Figure 6-1 in Chapter 6 shows the effect of 2% Lavandula angustifolia given
in a hand “m” technique by Mitchell prior to extubation. There have been similar
effects from Roman chamomile and rose essential oils with the “m” technique.
Mitchell further explains the patient appeared much calmer and less anxious as
she was carrying out the “m” technique procedure. The patient felt “able to trust”
her, and extubation was achieved far more easily than normal.
Henneman et al (2002) suggest a collaborative weaning plan for patients re-
quiring prolonged mechanical ventilation, which draws on a multidisciplinary
team. One advantage of aromatherapy is it can be carried out by any member of
that team.
Fear
Patients in a critical-care unit face more invasive and obnoxious procedures and
diagnostics than in any other unit. Invasive procedures are those such as the in-
sertion of hemodynamic monitoring lines, thoracentesis, paracentesis, and chest-
tube placement and removal. Diagnostics include those such as computed to-
mography scans, magnetic resonance imaging, and angiograms. Inhaling a
familiar aroma can do much to allay fears during these procedures and really helps
the claustrophobia and hyperventilation that can ensue.
Carrying out a hand, foot, or face “m” technique prior to the scheduled pro-
cedure can minimize the fear of cardiac catheterization. This will take only 5-10
minutes and can have a dramatic effect on the need for anxiolytics during the pro-
cedure. It is also a great way to enhance trust between patient and caregiver. Es-
sential oils to choose from are rose, neroli, mandarin, lavender, or Roman
chamomile. Please see Chapter 14 on cardiology for more information.
Adding three or four drops of essential oils to bath water can greatly im-
prove the mood of patients (and their caregivers!). Geranium is an excellent
choice as it appears to lift mood and reduce anxiety and can cut through some
unpleasant odors. Spritzing the room with a solution of Eucalyptus citriadora will
do much to improve the ambience but will also help cut down cross-infection
and the possibility of resistant organisms. Please see Chapter 9 on infection for
a more in-depth discussion of specific pathogens and essential oils that would be
effective.
278 Section II Clinical Use of Aromatherapy

Pressure Sores (Decubitus Ulcers)
Critically ill patients often cannot move by themselves and need to be turned
every few hours to prevent skin breakdown. Despite good nursing care and
alternating-pressure mattresses, decubitus ulcers (pressure sores) can occur. These
lesions are notoriously difficult to heal. What is initially persistent erythema can
develop into necrotic ulceration involving muscle, tendon, and bone.
Pressure sores can be caused by the following:
simple pressure exceeding that of the blood pressure at the venous or arter-
ial end of capillaries (Pritchard & Mallett 1992);
shearing (when the patient is dragged up the bed) destroying the microcir-
culation in the underlying tissue; in serious cases, lymphatic vessels and
muscle fibers can also become torn (Waterlow 1988);
friction causing stripping of the stratum corneum leading to superficial dam-
age ( Johnson 1989).
Specific areas of the body are at risk for the development of pressure sores. These
include the sacral area when lying supine, the coccygeal area when lying supine,
the ischial tuberosities when lying laterally, and the greater trochanters when ly-
ing laterally. Inactivity, immobility, malnutrition, altered sensation, and advanced
age can contribute to the incidence of pressure sores, but they are also more com-
mon among patients with decreased levels of consciousness. Waterlow (1987)
produced at-risk scales to show the type of patient found in a critical-care unit is
more likely to be at risk for pressure sores than other type of patient.
Pressure sores can be graded according to their severity (stage I-stage IV)
and need different treatments for each stage (David et al 1983). The degrees of
severity range from unbroken skin with simple redness to destruction of skin and
the underlying tissue. Once the skin has broken down, careful treatment of the
ensuing wound is paramount to prevent infection. Gustafsson (1988) catego-
rized wounds as dry and clean, wet and oozing but clean, or open and contami-
nated.
Turner et al (1985) described an appropriate material for wound dressing as
“a material which, when applied to the surface of a wound, provides and main-
tains an environment in which healing can take place at the maximum rate”. An
essential oil diluted in a cold-pressed vegetable oil would fit this description.
When the skin is red and sore but still intact, floral waters can be used to
bathe the skin and reduce surface heat. Chamomile (Matricaria recutita), he-
lichrysum, rose, and lavender floral water are good choices. When the skin is bro-
ken, a compress using floral waters with added essential oils can be used. How-
ever, when the wound has deepened, it is kinder to dilute the essential oils in a
carrier oil (or gel) to prevent the compress sticking to the sides of the wound and
increasing the trauma when the compress is removed. Calophyllum inophyllum
(palm kernel) carrier oil is an excellent medium in which to dilute the essential oil
because of its antiinflammatory action and gentle analgesic effects. Rosehip (Rosa
rubiginosa) carrier oil is also useful in the treatment of pressure sores. Aloe vera
gel would be an another excellent choice, particularly as it is so effective in the
Chapter 16 Critical Care 279
treatment of burns, which show a similar healing pattern to pressure sores
(Zawahry 1973).
See Table 16-1, 16-2, and 16-3 for some suggestions of suitable essential
oils, phytols, and hydrolats. If the wound is grossly infected, a higher concentra-
280 Section II Clinical Use of Aromatherapy
Table 16-1 h Suitable Essential Oils for Treating Decubitus Ulcers
Common Name Botanical Name
Lavender Lavandula angustifolia
Roman chamomile Chamaemelum nobile
Frankincense Boswellia carteri
Geranium Pelargonium graveolens
Yarrow Achillea millefolium
German chamomile Matricaria recutita
Common thyme Thymus vulgaris CT linalol and CT thujone
Rosemary Rosmarinus officinalis CT verbenone
Myrrh Commiphora myrrha
Bergamot Citrus bergamia
Table 16-2 h Suitable Phytols (Infused Herbal Oils) for Treating
Decubitus Ulcers
Common Name Botanical Name
Echinacea Echinacea purpurea
St John’s wort Hypericum perforatum
Calendula Calendula officinalis
Table 16-3 h Suitable Hydrolats (Floral Waters) for Treating
Decubitus Ulcers
Common Name Botanical Name
Rosemary Rosmarinus officinalis CT borneol
Myrtle Myrtus communis
Elderflower Sambucus nigra
Roman chamomile Chamaemelum nobile
Lavender Lavandula angustifolia
Rose Rosa damascena

tion of essential oil will be needed to contain the infection; use up to 20% when
necessary. However, if the wound is just slow in healing, 3%-10% will suffice.
Hartman and Coetzee (2002) found 8% solution was effective in treating deep,
slow-healing ulcers. solution in a carrier oil or phytol is necessary. Many stage II-
III decubiti are now covered with hydrocolloidal dressings until healing has taken
place. The suggestions in the tables are particularly relevant after initial healing
has begun and the dressings are removed. The selection of essential oils, floral wa-
ter, and infused herbal oils will decrease pain, promote ongoing healing, and can
help prevent reoccurrence. Ensure that floral waters and infused herbal oils are
purchased from a reputable supplier to avoid contaminated products.
In cases in which the ulcer is infected, please select essential oils that are ef-
fective against the relevant pathogen. See Table 16-4, as well as Chapter 9 on in-
fection, for some suggestions.
REFERENCES
Ashworth P. 1984. Staff-patient communication in coronary care units. J Adv Nurs. 9(1)
35-42.
Buckle J. 1993. Aromatherapy: does it matter which lavender essential oil is used? Nurs-
ing Times. 89(20) 32-35.
Buckle J. 1998. Clinical aromatherapy and touch: complementary therapies for Nursing
Practice. Critical Care Nurse. 18(5) 54-61.
David J, et al. 1983. Normal physiology from injury to repair. Nursing. 2(11) 296-297.
Deans S, Svoboda K. 1990. The antimicrobial properties of marjoram (Origanum majo-
rana). Flavour and Fragrance Journal. 5(3) 187-190.
Dunn C. 1996. Personal communication.
Dunn C, Sleep J, Collett D. 1995. Sensing an improvement: an experimental study to
evaluate the use of aromatherapy, massage and periods of rest in an intensive care unit.
Journal of Advanced Nursing. 21(1) 34-40.
Franchomme P, Penoel D. 1990. Aromatherapie Exactement. Limoges, France: Jollois.
Chapter 16 Critical Care 281
Table 16-4 h Some Examples of Antimicrobial Essential Oils
Common Name Botanical Name Use Against Reference(s)
German Matricaria recutita Staphylococcus Franchomme &
chamomile aureus, Proteus Penoel 1991,
vulgaris Valnet 1993
Lemongrass Cymbopogon citratus Shigella, E. coli, Onawunmi &
Bacillus subtilis Ogunina 1986
Juniper Juniperus communis Pseudomonas Janssen & Chin
1986
Sweet marjoram Origanum majorana Clostrium, Deans &
Salmonella Svoboda 1990

Gustafsson G. 1988. Guidelines for the application of disinfectant in wound care. Nurs-
ing RSA. 3(11-12) 8-9.
Hartman D, Coetzee J. 2002. Two US practitioners’ experience of using essential oils for
wound care. Journal Wound Care. 11(8) 317-320.
Henneman E, Dracup K, Ganz T, et al. 2002. Using a collaborative weaning plan to de-
crease duration of mechanical ventilation and length of stay in the intensive care unit
for patients receiving long-term ventilation. American Journal of Critical Care. 11(2)
132-140.
Ingham A. 1989. A review of the literature relating to touch and its use in intensive care.
Intensive Care Nurse. 5(2) 65-75.
Janssen A, Chin N. 1986. Screening for antimicrobial activity of some essential oils.
Pharmaceutisch Weekblad Scientific Edition (Utrecht). 8(6) 289-292.
Johnson A. 1989. Granuflex wafers as a prophylactic pressure sore dressing. Care-Science
and Practice. 7(2) 55-58.
Mitchell L. 2002. Personal communication.
Onawunmi G, Ogunina E. 1986. A study of the antibacterial activity of the EO of
lemongrass. International Journal of Crude Drug Research. 24(2) 64-68.
Pritchard A, Mallett J (eds.). 1992. The Royal Marsden Hospital Manual of Clinical
Nursing Procedures, 3rd ed. Oxford, UK: Blackwell Scientific Publications.
Redd W, Manne S, Peters B, et al. 1994. Fragrance Administration to reduce anxiety
during MRI imaging. J Magnetic Resonance Imaging. 4(4) 623-626.
Sharman R. 2001. Anatomy of a rose. Cambridge, MA: Perseus.
Stevensen C. 1994. The psychophysical effects of aromatherapy massage following car-
diac surgery. Complementary Therapies in Medicine. 2(1) 27-35.
Turner T. 1985. Semi-occlusive and occlusive dressing. In Royal Society of Medicine In-
ternational Congress and Symposium Series No. 88. London: Royal Society of Medi-
cine. 5-14.
Urden L. 1997. From the patient’s eyes. Critical Care Nurse. 17(1) 104-105.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Woolfson A, Hewitt D. 1992. Intensive aromacare. International Journal of Aromather-
apy. 4(2) 12-13.
Waldman C, Tseng P, Meulman P, et al. 1993. Aromatherapy in the intensive care unit.
Care of the Critically Ill. 9(4) 170-174.
Waterlow J. 1987. Tissue viability. Calculating the risk. Nursing Times. 83(39) 58-60.
Waterlow J. 1988. Tissue viability. Prevention is cheaper than cure. Nursing Times.
84(25) 69-71.
Welsh C. 1997. Tissue viability. Touch with oils: a pertinent part of holistic hospice care.
American Journal of Hospital Palliative Care. 14(1) 42-44.
Zawahry E. 1973. Leg ulcers, acne vulgaris, seborrhea and alopecea. International Jour-
nal of Dermatology. 12(1) 68-73.
282 Section II Clinical Use of Aromatherapy

W
283
17
Dermatology
I have seen cosmic beings and other worlds, yet without seeing a flower it is nothing.
William Elliott
Tying Rocks to Clouds
I
ncreasingly, transdermal therapeutic systems (TTS) are used as an alternative
to oral and parenteral pharmaceuticals. The skin, and therefore the care of
skin (dermatology), has become an important part of new drug delivery. This
is important to aromatherapy as many essential oils are applied to the skin. Fuchs
et al (1997) reported on the ability of carvone to be absorbed systemically from a
diluted massage. Carvone is a ketone that makes up 42.8% of spearmint (Bowles
2000).
However, many drugs are unsuitable for TTS because of their low perme-
ability, and components within essential oils may improve their permeability.
Almirall et al (1996) found that cineole, d-limonene, and pinene permeated the
skin and affected topical application of conventional drugs such as haloperidol
and chlorpromazine. Whereas cineole and d-limonene enhanced the transdermal
permeability of haloperidol, d-limonene reduced the transdermal permiability of
chlorpromazine. Cineole is an oxide found in rosemary, cardamon, spike lavender,
sage, and eucalyptus (Bowles 2000). Limonene is found in many citrus-peel oils.
Cornwall and Barry (1994) investigated the ability of 12 sesquiterpenes to en-
hance the drug 5 fluorouracil and concluded several showed promise as clinically
acceptable penetration enhancers.
The skin is the largest organ of the body. It is also a stress barometer that pro-
vides the outside world with an indication of the serenity or confusion within.
Much of dermatology is concerned with putting topical drugs onto the skin.
However, skin problems may be linked to stress and diet. Possibly three of the

most common skin conditions suitable for aromatherapy are eczema, herpes, and
onychomycosis.
Eczema
Eczema is often used as a generic term to describe dermatitis although Ellis et al
(2002) suggests the two are not synonomous. Eczema is described as a “common
itching skin disease characterized by reddening (erythema) and vesicle formation
which may lead to weeping and crusting” (McFerran 1996). Eczema can be
divided into two definitive groups: specific, which includes atopic or allergic, and
a broad generic term covering generalized dermatitis. Eczema becomes clearer
if it is divided into four specific types: allergic, atopic, irritant, and seborrhoeic
(Schultz 2002).
Allergic eczema is caused by an allergen, and the allergy is unique to each
person. An example of this is latex allergy, one of the most common skin prob-
lems among health workers. Minute amounts of latex, sometimes only two mol-
ecules, can trigger a skin reaction. Other examples of allergens are wool, lanolin,
nickel found in jewelry, and rubber. Atopic eczema is associated with hay fever
and asthma and affects up to 20% of the population. Irritant dermatitis can affect
anyone and is related to the use of irritants such as biological washing powders
and detergent cleaning agents (Gascoigne 1993). The only difference is the
amount of irritant needed to produce an eczematous reaction. Seborrhoeic der-
matitis involves the nose, lips, eyes, and scalp and is associated with Pityrosporum
yeast infections.
The traditional treatment for eczema involves corticosteroid creams, avoid-
ance of foods such as dairy products, yeast, or food additives (in cases of allergic
or atopic eczema), and reduction of topical irritants.
While aromatherapy may aid the treatment of eczema either by reducing
stress or by acting at a topical, aniinflammatory level, if the underlying problems
contributing to the condition are not removed, the condition will not improve
greatly. Eczema could be made worse if an essential oil is chosen to which the pa-
tient is sensitive or, in the case of atopic eczema, if too high a concentration is
used. For this reason, patch testing should be mandatory for all eczema patients
(particularly atopic) who wish to try aromatherapy. Put double the concentration
of essential oil you wish to use on an adhesive bandage and apply to the patient’s
inner forearm. Leave in situ for 12 hours. Look for redness and itching. In addi-
tion, a careful case history, including details of potential antagonists (especially
herbal teas, flowers, and pollens in cases of atopic eczema) and cosmetics (for con-
tact allergic eczema) should be tabulated.
Anderson et al (2000) carried out a study on atopic eczema that, at first
glance, indicated massage with essential oils made the eczema worse. However,
this was a very unusual study as mothers chose the essential oil for their children
themselves from an offered selection of 36 “commonly used” essential oils. It was
not clear whether the mothers had any previous knowledge of or experience with
284 Section II Clinical Use of Aromatherapy

essential oils. Two of the oils they chose were spike lavender and Litsea cubeba.
Spike lavender contains up to 30% oxide (1,8-cineole) a common skin irritant, es-
pecially among young children (Price & Price 1999). Litsea cubeba often called
“May chang” is commonly used in natural perfumery and is 85% citral, a common
skin (and mucous membrane) irritant (Bowles 2000). It might be interesting to
revisit this study and analyze it without those two essential oils.
Kadir and Barry (1991) found that alpha-bisabolol (an ingredient in German
chamomile) enhanced the penetration of triamcinolone acetonide (a weak steroid
which was formerly used to treat severe eczema) by 73 times thereby suggesting
German chamomile could be used successfully with conventional topical treat-
ment. Another ingredient in German chamomile, chamazulene, was found to in-
hibit the production of leukotriene B4 in neutraphilic granulocytes in vitro
(Safayhi et al 1994).
Listed in Table 17-1 are some essential oils considered to be beneficial in
treating eczema, followed by a discussion of the reasons for their use.
Lavandula angustifolia (true lavender) is very useful because of its recognized
healing properties for burns and wounds. Lavender appears to have a cell-
regenerating action, is soothing and sedative, and has a topical analgesic action that
will help the itching. It is also antibacterial and moderately antifungal. This was
the essential oil that proved so effective for Gattefosse’s burns (Tisserand 1993).
The almost antihistamine-like action of Matricaria recutita (German
chamomile) essential oil is due to the strong antiinflammatory effect of its three
sesquiterpenes: azulene, bisabolol, and farnesene (Mills 1991). This makes Ger-
man chamomile invaluable in the treatment of eczema. Its antiinflammatory
Chapter 17 Dermatology 285
Table 17-1 h Essential Oils for Eczema
Common Name Botanical Name Reference
True lavender Lavandula angustifolia Tisserand 1994
German chamomile Matricaria recutita Carle & Gomaa 1992
Tubaro et al 1984
Frankincense Boswellia carteri Duwiejua et al 1992
Roman chamomile Chamamelum nobile Rossi et al 1988
Balsam Myroxylon balsamum Tisserand 1993
Nagar matha Cyperus scariosus Gupta et al 1972
Cedarwood Cedrus atlantica Tisserand 1993
Fennel Foeniculum vulgare Mascolo et al 1987
Everlasting Helicrysum italicum Buckle 2001
Juniper Juniperus communis Mascolo et al 1987

effects have been well researched, and it is used in several pharmaceutical prepa-
rations. Carle & Gomaa (1992) found the alpha-bisabolol chemotype was the
most effective.
German chamomile was tested together with a steroid and a nonsteroid (hy-
drocortisone and benzydamine, respectively) preparation on mice. Although it
was not as effective as hydrocortisone, it was as effective as benzydamine (Tubaro
et al 1984). However, in another study on humans, Kamillosan Ointment, which
contains German chamomile, was found to be as effective as hydrocortisone
in 161 patients (Aertgeerts et al 1985). German chamomile was also found to
be effective in wound healing of patients following dermabrasion of tattoos
(Glowania et al 1987).
Roman chamomile, Chamemelum nobile, is also an antiinflammatory (Rossi
et al 1988). Although not as antiinflammatory as German chamomile, Roman
chamomile might be more acceptable. German chamomile is dark blue and very
pungent. Roman chamomile is colorless to pale blue with a pleasant, apple-like
aroma. The two chamomiles have very different chemistry.
A little-known essential oil, Cyperus scariosus (nagar matha in Sanskrit),
which is a grass-like herb, showed antiinflammatory activity in rats within 3 hours
of its application. The inhibition of granulous-tissue formation was thought to be
comparable to that achieved with hydrocortisone (Gupta et al 1972). This essen-
tial oil is not readily available.
Resins such as Boswellia carteri (frankincense) have traditionally been used in
India and Africa to treat inflammatory conditions (Duwiejua et al 1992). In a study
of the antiinflammatory effects of 75 species of plants on artificially induced in-
flammation in rats, Foeniculum vulgare dulce (sweet fennel), Juniperus communis (ju-
niper), and Symphytum officinale (comfrey) decreased inflammation by up to 50%.
Comfrey (an infused oil) also has antiulcer properties (Mascolo et al 1987) and
could form a useful base for the essential oil mix. Balsam and skin problems were
the subject of a doctoral thesis by Descouleurs, written in 1896 (Tisserand 1993).
Gattefosse reported Cedrus atlantica (cedar) was used to treat skin disorders in
an Algerian hospital in 1899 with great success (Tisserand 1992). Finally, my clin-
ical experience and that of my students is that Helicrysum italicum diluted in aloe
vera gel (3%) is very effective in reducing the heat and itchiness of eczema. It will
work within a few hours if it is going to work at all and is definitely worth a try.
Herpes
Cases of herpes simplex I and II reached epidemic proportions in the 1980s, and
currently statistics from the American Social Health Association show that up to
50 million Americans have genital herpes, and there are 1 million newly diag-
nosed infections each year (Susman 2001). Further, genital herpes affects one of
every five teens and adults in the United States and has increased 30% during the
past 10 years, according to ASHA, a private, nonprofit organization dedicated to
stopping sexually transmitted diseases (ASHA 2003).
286 Section II Clinical Use of Aromatherapy

The painful clusters of blisters reappear, usually in the same area, with ago-
nizing regularity—often monthly—and once the disease has been contracted, the
patient is infected for life. Outbreaks can be triggered by sexual activity, stress,
heat, hormonal changes, diet, and low immunity. Although the blisters often oc-
cur in the genital area (either internally or externally), they may also be found on
the thighs and buttocks. Extremely contagious at the blister stage, herpes can re-
main dormant for months or years in the spinal cord, ready to migrate down the
sensory nerves to the skin.
Orthodox treatment for herpes is with nucleoside analogues, such as Acy-
clovir, that introduce intracellular impediment to viral replication. These medica-
tions are taken orally and often leave a metal-like after taste. Essential oils that
may be effective against herpes in tissue are shown in Table 17-2. The table was
compiled with reference to various research studies carried out on human tissue
using extracts from plants (Cohen et al 1964; Kucera & Herrmann 1967; May &
Willuhn 1978).
A randomized, controlled, multicentered study on 115 patients by Wolbling
and Leonhardt (1994) found the aqueous extract of Melissa effective in treating
herpes. On the final day (fifth day) of treatment, 24 patients in the Melissa group
were symptom free versus 15 symptom-free patients in the placebo control group.
Scabbing and swelling were more reduced in the Melissa group, indicating reduced
cell damage and accelerated healing. Method of treatment was a proprietary-
brand cream (Lomaherpan) that contains 1% Melissa extract. The control was an
identical cream base without Melissa. The site of the herpes treated was the lips
in 34 in the Melissa group and 33 in the control group and on the genitals in four
Chapter 17 Dermatology 287
Table 17-2 h Essential Oils for Treating Herpes Simplex I & II
Common Name Botanical Name Reference
Cubeb Piper cubeba May & Willuhn 1978
Blue gum Eucalyptus globulus May & Willuhn 1978
Juniper Juniperus communis May & Willuhn 1978
Melissa Melissa officinalis Wolbling et al 1994
Tea tree Melaleuca alternifolia Buckle 2001
Palma rosa Cymbopogon martinii Buckle 2001
Rosemary Rosmarinus officinalis May & Willuhn 1978
Rose Rosa damascena Buckle 2001
Ravensara Ravensara aromatica Buckle 2001
Moroccan thyme Thymus satureioides Buckle 2001

in the Melissa group and six in the control group. A subgroup of 67 patients tested
positive for herpes labialis (type II, on the lips). The decline of the lesions re-
mained statistically faster in the Melissa group than the placebo group.
One-percent Melissa aqueous extract was tested for topical treatment of re-
curring herpes labialis (Koytchev et al 1999). This was a double-blind, placebo
controlled, randomized trial on 66 patients who had a history of four episodes of
herpes labialis per year. The Melissa cream was applied four times a day. There was
significant reduction in size of affected area and blisters at day 2 in the Melissa
group. There was a rapid ameliorating effect on typical symptoms, reduction in
healing time, and prolonged periods between occurrences.
Both these studies used an aqueous extract. This is not the same as an essen-
tial oil. However, clinical experience of myself and my students indicates the es-
sential oil of Melissa is also extremely effective against herpes simplex I and II.
Melissa is the most expensive of all essential oils, and therefore is the most of-
ten adulterated. Frequently it is mixed with synthetics, lemongrass, or citronella.
These contaminants may have a worsening effect on irritated or abraded lesions
in irritant dermatitis, or, indeed, herpes.
A certain amount of anecdotal evidence indicates essential oils, applied to the
area when the tingling begins, can prevent herpes blisters from forming. There is
also anecdotal evidence that, when such oils are applied to the blisters, the pain
and itching are greatly relieved. The most commonly used essential oils have been
isolated from the 75 plants found to have virustatic activity. Despite the age of the
papers cited that investigated the first four essential oils listed for treating herpes
(see Table 17-2), I have found these and the other essential oils in the table ef-
fective in 10 years of clinical experience. Severity, duration, and frequency of her-
pes outbreaks have decreased substantially with their use. A suggested protocol
for application is shown in Table 17-3. Each patient will respond to one particu-
lar essential oil or mix of oils. The reason the essential oils work could be because
they are lipophyllic and appear to dissolve the lipid capsule (or capsid) of the
virus. The most successful essential oil I have used has been Ravansara aromatica
(ravensara).
288 Section II Clinical Use of Aromatherapy
Table 17-3 h Protocol for Using Essential Oils in Treating Herpes
Symptom Topical Application Frequency
Tingling Undiluted essential oil Every 4 hours
Redness and swelling Undiluted essential oil Every 4 hours
Pustule formation Undiluted essential oil Every 4 hours
Broken pustule, raw skin 25% diluted essential oil* Every 4 hours
Raw skin 5% diluted essential oil Every 4 hours
*Dilute in cold-pressed vegetable oils, like sweet almond, or aloe vera gel.

In a study by Armaka et al (1999), isoborneol, a monoterpeneol found in sev-
eral essential oils, demonstrated viricidal activity against herpes simplex virus I by
inactivating the virus within 30 minutes of exposure. Further, a concentration of
0.06% isoborneol completely inhibited viral replication without affecting viral ad-
sorption. Isoborneol did not show significant cytotoxicity when tested against hu-
man cell lines at 0.16%. Therefore essential oils containing a major proportion of
isoborneol might be useful in treating herpes. A high amount of borneol (up to
70%.) is found in Thymus satureoides ( Japanese thyme).
Geraniol, a monoterpenol found in many essential oils, was found to enhance
the antiherpetic activity of conventional treatment in a study by Shoji et al (1998).
Its action was thought to occur by changing the subcellular distribution of the
oligonucleotides. Geraniol is found in palma rosa (80%) (Bowles 2000) and Thy-
mus vulgaris CT gereniol.
Benencia and Courreges (2000) found eugenol was effective against herpes
simplex type I and II in monkey kidney-cell cultures and in vivo (in rabbits). The
monkey-cell cultures showed a dose-dependent sensitivity (higher doses in-
creased treatment effectiveness), and at least 50% of the viral activity was lost af-
ter contact with the diluted eugenol (250ug/ml) for one hour. Eugenol also ap-
peared to enhance the effect of Acyclovir. Eugenol appeared to prolong the
resistance of rabbits to developing herpes by 7 days, but all experimental animals
eventually became ill.
The antiherpetic activity of buds of Syzygium aromatica (clove) were alluded
to by Takechi et al (1985). However as clove is very high in phenols (70%), and
phenols are irritant to the skin and mucous membrane, clove bud (or leaf) is best
avoided.
Athlete’s Foot and Onychomycosis
Athlete’s foot (Tinea pedis) is the most common form of superficial dermatophyte
infection in the developed world and infects approximately 10% of the popula-
tion (Tong et al 1992).
Onychomycosis (sometimes called Tinea ingium) is a superficial fungal in-
fection that destroys the entire nail unit. It is a cousin of Tinea pedis, which causes
athlete’s foot. It is less contagious than athlete’s foot, but susceptibility increases
after trauma to the nail bed. Once contracted, it is extremely difficult to remove
completely. Symptoms are a thickened nail that becomes discolored, brittle, or
chalky and ultimately disintegrates. Medical treatment includes debridement and
topical or systemic antifungals. Oral antifungal agents began with Griseofulvin in
1959 (Buck et al 1994), which was given orally for 6 months or until the nail grew
out. Side effects to Griseofulvin are nausea, vomiting, diarrhea, mental confusion,
and headaches.
Headaches are the most common side effect and can be severe, especially at
the commencement of treatment. The cure rate is 3%-38%. Ketoconazole is an-
other option, with the added advantage that it also treats yeast. The cure rate is
Chapter 17 Dermatology 289

higher at 50%-94%, and the side effects are less common, although they are more
serious and include idiosyncratic liver dysfuntion, requiring liver transplantation
(Knight et al 1991). Unfortunately, 50% of toenail infections recur within 4 years
of completion of treatment (Torok & Stechlich 1986). Itraconazole has cure rates
of 4%-92% but has only been evaluated in small studies (Piepponen et al 1992).
The previously mentioned conventional treatments are expensive and involve oral
medication.
The incidence of onychomycosis is increasing with no real satisfactory cure.
Buck et al (1994) carried out a multicentered, double-blind, randomized, con-
trolled study on onychomycosis using tea tree or clotrimazole. One-hundred sev-
enteen patients with distal subungual onychomycosis proven by culture took part
in the study. Patients received either twice-daily applications of clotrimazole so-
lution or 100% tea tree. Debridement took place at 0, 1, 3, and 6 months. Topi-
cal use of tea tree produced a similar result to oral doses of clotrimazole, with 55%
of the clotrimazole group and 56% of the tea tree group reporting improvement
or resolution after 3 months. The number of adverse reactions were similar; three
out of 53 for the clotrimazole group and five out of 64 in the tea tree group.
Syed et al (1999) carried out a randomized, double-blind, placebo-controlled
study to examine the clinical efficacy and tolerability of 5% Melaleuca alternifolia
with 2% butenafine hydrochloride incorporated in a cream. Sixty patients took
part in the study. There were 39 men and 21 women, and the average age was 29
years. Each participant had a history of onychomycosis for 6-36 months. After
using the cream for 16 weeks, 80% of the participants in the experimental group
were cured. No participant was cured in the placebo group. Four participants in
the experimental group experienced mild inflammation but did not discontinue
treatment. During follow-up no relapse occurred in the cured patients, and no
improvement was seen in the medication-resistant and placebo participants.
Elsethager (2000) investigated the effect of two essential oils (lemongrass
and tea tree) on 12 study participants who had onychomycosis for a minimum du-
ration of 1 year. One participant had it for more than 10 years. Two dilutions, 2%
tea tree and 3% lemongrass, were mixed together in grapeseed oil and given to
each participant, who rubbed the mixture well into the affected nail bed twice a
day for 2 months. It was thought there would be some visual improvement dur-
ing this time, although participants would need to continue treatment until the
whole nail had grown out. Only four people completed the treatment for 2
months. All stated their nails were less discolored, scaly, and cracked, and the dis-
comfort was less. A visual analog on effectiveness was completed, with zero as not
effective and 10 as extremely effective. One person rated the treatment a seven,
and the other three rated it a seven. Two of the four had previously used over-the-
counter medications (Tinactin and Dr. Scholl’s) which were rated zero. One of
the four participants had been offered an oral course of Griseofulvin, which she
had declined because she was concerned about the side effects.
Garg and Dengre (1988) found Cymbopogon citratus (West Indian lemon-
grass) effective against Trichophyton mentagrophytes. The most active component
290 Section II Clinical Use of Aromatherapy

of lemongrass was citral (70%-80%), which is thought to be responsible for
the antifungal activity of this plant. Lippia alba, which grows widely in Central
and South America, also has strong antifungal activity against Trichophyton
mentagrophyes var. interdigitale. Several chemotypes of the plant exist, and the es-
sential oil from the plant grown in Aruba is thought to be most suitable as it con-
tains 64% citral (Fun & Svendsen 1990).
Even at the low concentrations, essential oils can show very significant an-
timycotic activity against Trichophyton mentagrophytes (Rai & Acharya 2001).
Sahi et al (1999) compared the efficacy of Eucalyptus citriadora with commercial
antifungal drugs and found minimal concentration of the oil inhibited all the
tested pathogens, Microsporum nanum, Trichophyton mentagrophytes, and T.
rubrum, completely with fungistatic activity. Romagna et al (1994) reported the
antifungal effects of alpha-terthienyl from Tagetes patula on five dermatophytes.
Rai and Acharya (2000) found Tagetes erecta, T. patula, and Eupatorium triplin-
erve to be effective topical antimycotics.
REFERENCES
Aertgeerts P, Albring M, Klaaschka F, et al. 1985. Comparative testing of Kamillosan
cream and steroidal (0.25% hydrocortisone, 0.75% fluocortin butyl ester) and non-
steroidal (5% bufexamac) dermatologic agents maintenance therapy for eczematous
diseases. Zeitschrift fur Hautkrankheiten (Berlin). 60(3) 270-277.
Almirall M, Montana J, Escribano E, et al. 1996. Effect of d-limonene, a pinene and ci-
neole on in vitro transdermal human skin penetration of chlorpromazine and
haloperidol. Arzneim-Forsch/Drug Research. 46(7) 676-680.
American Social Health Association. January 2003. www.ashstd.org.
American Social Health Association. June 2001. www.ashstd.org.
Anderson C, Lis-Balchin M, Kirk-Smith M. 2000. Evaluation of massage with essential
oils on childhood atopic eczema. Phytotherapy Research. 14(6) 452-456.
Armaka M, Papanikolaou E, Sivropoulou A, et al. 1999. Antiviral properties of isobor-
neol, a potent inhibitor of herpes simplex virus type 1. Antiviral Research. 43(2)
79-92.
Benencia F, Courreges M. 2000. In vitro and in vivo activity of eugenol on human her-
pes virus. Phytotherapy Research. 14:495-500.
Bowles J. 2002. The basic chemistry of aromatherapeutic essenial oils. Sydney: Good
Scents Aromapleasure.
Buck D, Nidorf D, Addino J. 1994. Comparison of two topical preparations for the
treatment of onychomycosis: Melaleuca alternifolia (teatree) oil and clotrimazole. Jour-
nal of Family Practice. 38(6) 601-605.
Buckle J. 2001. Results of 200 case studies. Unpublished dissertation. Hunter, NY: R J
Buckle Associates.
Cohen R, Kucera L, Herrmann C. 1964. Antiviral activity of Melissa officinalis. Proceed-
ings of the Society of Experimental Biology and Medicine. 117: 431-434.
Cornwall P, Barry B. 1994. Sesquiterpene components of volatile oils as skin penetration
enhancers for the hydrophilic permanent 5 fluorouracil. Journal of Pharmacy and
Pharmacology. 46(4) 261-269.
Chapter 17 Dermatology 291

Duwiejua M, Zeitlin I, Waterman P, et al. 1992. Anti-inflammatory activity of resins
from some species of the plant family Burseraceae. Planta Medica. 59(1) 12-16.
Elliott W. 1995. Tying rocks to clouds. New York: Image Books/Doubleday.
Ellis C, Drake L, Prendelgast M, et al. 2002. Cost of atopic dermaitis and eczema in the
USA. Dermatology. 46: 361-370.
Elsethager T. 2000. The use of lemongrass and teatree for fungal infections of feet and
nails. Unpublished dissertation. Hunter, NY: R J Buckle Associates.
Fuchs N, Jager W, Lenhardt A, et al. 1997. Systemic absorption of topically applied car-
vone: influence of massage technique. Journal of Society of Cosmetic Chemists. 48:
277-282.
Fun C, Svendsen A. 1990. The essential oils of Lippia alba. Journal of Essential Oil Re-
search. 2(5) 265-267.
Garg S, Dengre S. 1988. Antifungal activity of some essential oils. Pharmacie. 43(2)
141-142.
Gascoigne S. 1993. Manual of Conventional Medicine for Alternative Practitioners, Vol.
1. Richmond, VA: Jigme Press.
Gattefosse R. 1937. (Translated in 1993 by R. Tisserand.) Aromatherapie: Les Huile
Essentielles-Hormones Vegetales (Gattefosse’s Aromatherapy.) Saffron Walden, UK:
CW Daniels, 89.
Glowania H, Raulin C, Svoboda M. 1987. Effect of chamomile on wound healing: a
clinical double-blind study. Berlin: Zeitschrift fur Hautkrankheiten. 62(17) 1262,
1267-1271.
Gupta S, Sharma R, Aggarwal O. 1972. Anti-inflammatory activity of the oils isolated
from Cyperus scariosus. Indian Journal of Experimental Biology. 10(1) 41.
Jandera V, Hudson S, de West P. 2000. Cooling the burn wound: evaluation of different
modalities. Burns. 26(3) 265-270.
Kadir R, Barry B. 1991. A-bisabolol a possible safe penetration enhancer for dermal and
transdermal therapeutics. International Journal of Pharmacology. 70: 87-94.
Knight T, Shikuma C, Knight J. 1991. Ketoconazole-induced fulminant hepatitis neces-
sitating liver transplantation. Journal of the American Academy of Dermatology. 25(2
part 2) 398-400.
Koytchev R, Alken R, Dundarov S. 1999. Balm mint extract (Lo-701) for topical treat-
ment for recurring herpes labialis. Phytomedicine. 6(4) 225-230.
Kucera L, Herrmann E. 1967. Antiviral substances in plants of the mint family. (Labi-
atae) Tannin of Melissa officinalis. Proceedings from the Society for Experimental Bi-
ology and Medicine. 124(3) 865-869.
Maiche A G, Grohn P, Maki-Hokkonen H. 1991. Effect of chamomile cream and al-
mond ointment on acute radiation skin reaction. Acta Oncologica. 30(3) 395-396.
Mascolo N, Autore G, Capasso F 1987. Biological screening of Italian medicinal plants
for anti-inflammatory activity. Phytotherapy Research. 1(1) 28-31.
May V, Willuhn G. 1978. Antivirale Wirkung waBriger Pflanzenextrakte in Gewebekul-
turen. Arzneim-Forsch/Drug Research. 28(1) 1-7.
McFerran T. 1996. A Dictionary of Nursing, 2nd ed. Oxford, UK: Oxford University
Press.
Mills S. 1991. Out of the Earth. London:Viking Arkana.
Piepponen T, Blomqvist K, Brandt H, et al. 1992. Onychomycosis treated with itracona-
zole or griseofulvin alone with and without a topical antimycotic or keratolytic agent.
International Journal of Dermatology. 30: 586-589.
292 Section II Clinical Use of Aromatherapy

Price S, Price L. 1999. Aromatherapy for Health Professionals. London: Churchill Liv-
ingstone.
Rai M, Mares M, editors. 2003. Plant Derived Antimycotics. Binghamton, NY:
Haworth.
Romagna C, Mares D, Fasulo M, et al. 1994. Antifungal effects of alpha-terthienyl from
Tagetes patula on five dermatophytes. Phytotherapy Research. 8(6) 332-336.
Rossi T, Melegari M, Blanchi A. 1988. Sedative, anti-inflammatory and anti-diuretic ef-
fects induced in rats by essential oils of varieties of Anthemis nobilis: a comparative
study. Pharmacological Research Communications. 20(Suppl. V) 71-74.
Safayhi H, Sabieraj J, Sailer E et al. 1994. Chamazulene: an antioxidant-type inhibitor of
leukotriene B4 formation. Planta Medica. 60(5) 410-413.
Sahi S, Shukla A, Bajaj A, et al. 1999. Broad spectrum antimycotic drug for the control
of fungal infections in human beings. Current Science. 76(6) 836-939.
Shoji Y, Ishige H, Tamura N, et al. 1998. Enhancement of anti-herpetic activity of anti-
sense phosphorothioate oligonucleotides 5 end modified with geraniol. Journal of
Drug Targeting. 5(4) 261-273.
Susman C. 2001. Americans unaware of scope of HIV infection. www.ncm.nih.
govmedlineplus/news.
Syed T, Qureshi Z, Ali S, et al. 1999. Treatment of toenail onychomycosis with 2% bute-
nafine and 5% Melaleuca alternifolia (teatree in cream). Tropical Medicine & Interna-
tional Health. 4(4) 284-287.
Takechi M, Tanaka Y, Takehara M, et al. 1985. Structure and anti-herpetic activity
among the tannins. Phytochemistry. 24(10) 2245-2250.
Tisserand R. 1992. The book that launched aromatherapy. International Journal of Aro-
matherapy. 4(4) 20-22.
Tong M, Altman P, Barnetson R. 1992. Teatree oil in the treatment of Tinea pedis. Aus-
tralasian Journal of Dermatology. 33(3) 145-149.
Torok I, Stechlich G. 1986. Long term post treatment follow up of onychomycosis
treated with ketoconazole. Mykosen. 29(8) 372-377.
Tubaro A, Zilli C, Redaeli C. 1984. Evaluation of anti-inflammatory activity of a
chamomile extract topical application. Planta Medica. 50(4) 147-153.
Wolbling R, Leonhardt K. 1994. Local therapy of herpes simplex with dried extract
from Melissa officinalis. Phytomedicine 1: 24-31.
Chapter 17 Dermatology 293

294
W
18
Endocrinology
Without communication, no real understanding can be possible. Be sure you can
communicate with yourself. If you cannot communicate with yourself, how do you
expect to communicate with another person?
Tich Nhat Hanh
Anger
T
he endocrine system is the regulator of homeostasis (Anthony &
Thibodeau 1983). This balance is maintained through some two hundred
hormones in our bodies. The word hormone comes from the Greek hor-
maein, meaning to excite. In certain instances the nervous and endocrine systems
can regulate each other’s activities, as well as acting together to bring about
changes in physiology. Endocrine cells in the body occur in clusters in the en-
docrine glands. These glands secrete hormones directly into the bloodstream. As
hormones regulate our metabolism, growth, development, and reproduction, it is
clear they are a fundamental necessity to life. Hormones also govern our stress re-
sponse. Aromas interact with the limbic, hormonal, and endocrine systems as well
as impacting prostaglandin production and cell metabolism. This makes aro-
matherapy a valuable tool for treating conditions related to the endocrine system
(Table 18-1 introduces the main organs of the endocrine system).
Hormones play an important role in the mechanisms involving prosta-
glandins. Prostaglandins are a unique group of biological compounds that have a
5-carbon ring and serve important integrative functions in the body but do not
fit the definition of a typical hormone. They are metabolized rapidly and so the
amount in the bloodstream at one time is very low (Anthony & Thibodeau 1983).
Three classes of prostaglandins—prostaglandin A (PGA), prostaglandin E
(PGE), and prostaglandin F (PGF)—have been isolated and identified from a
wide range of tissues. Aspirin is thought to exert its antiinflammatory action by

inhibiting PGE synthesis. Eugenol, carvacrol, thymol, and gingerol (all com-
pounds found within essential oils) have also been shown to influence PGE syn-
thesis (Bennett & Stamford 1988; Wagner et al 1986). Prostaglandin F (PGF) is
important in the female reproductive system (Alexander 2001).
All prostaglandins are intimately involved in endocrine regulation by influ-
encing adenyl cyclase and adenosine 3,5-phosphate activity within the cell
(Anthony & Thibodeau 1983). Anything that interferes with that cellular activ-
ity indirectly affects the hormonal and endocrine system. Calcium regulates cel-
lular activity (Alexander 2001). Components within essential oils can interfere
with the release of calcium at a cellular level. This blocking mechanism has
been demonstrated for menthol, anethole, eugenol, and thymol (Melzig &
Teuscher 1991). These components are found in essential oils such as pepper-
mint, fennel, aniseed, star aniseed, bay, clove, Spanish marjoram, thyme, and
oregano (Sheppard-Hangar 1995; Budavari 1996).
Aromatherapy and the Female Reproductive System
Premenstrual syndrome (PMS) and menopausal problems are directly related to
the endocrine system (Alexander 2001). The uterus makes prostagladins to help
Chapter 18 Endocrinology 295
Table 18-1 h Main Organs of the Endocrine Systems
Pineal gland Regulates production of melatonin (a dark/light mech-
anism that affects how we sleep)
Pituitary gland Master endocrine gland divided into two lobes:
1) the anterior lobe governs growth, thyroid, adreno-
corticotropic, and reproductive hormones, namely
luteinizing and follicle-stimulating hormone
2) the posterior lobe secretes vasopressin (antidiuretic
hormone) and oxytocin (stimulates contraction of the
uterus during labor)
Thyroid Secretes thyroxin and governs metabolic rate
Parathyroid Controls calcium and phosphate levels
Adrenal cortex Produces corticosteroids
Adrenal medulla Produces adrenaline and noradrenaline
Islets of Langerhans Secretes insulin, glucagon, somatostatin, amylin, and
gastrin
Female gonads Produce estrogen and progesterone
Male gonads Produce testosterone

with labor, and the same prostaglandins can cause menstrual cramps. This is
why medications that block the synthesis of prostaglandin are effective in dys-
menorrhea. Alexander (2001) suggests it is possible that essential oils with va-
sodilatory or prostaglandin-antagonist properties might relieve the problem via
olfaction alone, although I think this is unlikely. During menopause, 50%-70% of
women experience a variety of physical and emotional symptoms (Schwingl et al
1994). Many of these symptoms can be ameliorated with certain essential oils.
PMS and menopause affect many millions of women every day. Fluctuation in es-
trogen levels can lead to profound mental and physical symptoms. Estrogen lev-
els drop after ovulation and at menopause.
There are three main forms of estrogen. Estradiol is the strongest form of es-
trogen our bodies make. Estrone is converted from estradiol in the liver, and Es-
triol is the weakest form of estrogen. However even estriol can have a pronounced
effect (van Der 1982).
Premenstrual Syndrome
PMS became a household name in England in 1987 when Anna Reynolds was
charged with the murder of her mother (a crime committed while suffering from
the effects of PMS) and jailed for life. Four months later, a petition signed by
6000 people launched an appeal for her release. On June 23, 1988, the British
court of appeals reduced the murder charge to manslaughter on the grounds of
PMS, and Reynolds was released. This was the first time a woman had been al-
lowed to plead diminished responsibility due to “the time of the month.”
Women have known for many years that they can become irrational, irrita-
ble, weepy, and occasionally violent a few days before their menstrual period.
No one quite knows why this phenomenon affects some women and not oth-
ers. However, the chemistry of a woman’s brain actually changes during this
time and produces reactions she cannot control (Alexander 2001). The area
deep within the limbic system involved with mood control has more estrogen
receptors than other parts of the brain, which makes it more vulnerable to
changes in estrogen levels. One in 10 women becomes irritable, depressed, and
fatigued with PMS symptoms appearing 7-10 days prior to menses. However,
the more violent or aggressive PMS symptoms usually appear within 5 days of
the menstruation time. There is a difference in PMS behavior depending on the
side of the brain involved (Alexander 2001). The left side often produces symp-
toms of depression and irritability. The right side is associated with anger and
negative emotion.
In PMS there appears to be a fluctuation in the levels of endogenous opioids
(these are abundant in the limbic system) and serotonin. In the first half of the
menstrual cycle the levels of estrogen and endorphin interact with neurotrans-
mitters serotonin, dopamine, and norepinephrine to keep mood stability. When
estrogen levels first begin to drop, immediately after ovulation, serotonin recep-
tors are primed (Rubinow et al 1998). When estrogen levels drop again prior to
menstruation, the brain registers estrogen withdrawal of serotonin.
296 Section II Clinical Use of Aromatherapy

Conventional medicine treats PMS with selective serotonin reuptake in-
hibitors (SSRIs) such as fluoxetine, paroxetine, sertraline, and citalopram or a tri-
cyclic antidepressant related to SSRI such as clomipramine (Reid 2002). A sim-
pler but almost as effective method can be a large block of chocolate! Chocolate
has been found to increase serotonin and has been dubbed “the Prozac of plants”
by Forbes magazine (Bartlett 1999).
Aromatherapy can, in many instances, produce very reasonable results in
PMS if regular treatments are given throughout a period of several months. The
essential oils chosen are usually a combination of those thought to have estrogen-
like properties, such as fennel (Foeniculum vulgare), sage (Salvia officinalis), or
clary sage (Salvia sclarea) (Zondeck & Bergmann 1938), and those that have
hormone-like properties, such as Scotch pine (Pinus sylvestris) and myrrh (Com-
miphora myrrha) (Franchomme & Penoel 1991). Salvia sclarea also has antiin-
flammatory properties (Moretti et al 1997). Belaiche, a French MD who devotes
a whole volume of his work to female problems, suggests essential oil of sage,
thyme, or geranium for PMS (Belaiche 1979). Citral (an aldehyde found in
lemongrass, melissa, and verbena) demonstrates estrogen activity when applied
dermally to rats, although in doses much higher than would be normally used in
aromatherapy (Tisserand & Balacs 1995). Table 18-2 lists essential oils used in
the treatment of PMS.
Depending on the patient’s needs, another essential oil can be added to the
“balancing” essential oil that will help alleviate the symptoms of the imbalance. For
example, if a woman is showing symptoms of depression and is weepy, an essential
oil with an antidepressant action such as bergamot (Sheppard-Hangar 1995) or
rose (Rovesti & Columbo 1973) could be added to the balancing mixture. If she is
Chapter 18 Endocrinology 297
Table 18-2 h Essential Oils for PMS
Common Name Botanical Name Reference
Fennel Foeniculum vulgare Zondeck & Bergmann 1938
Sage Salvia officinalis Zondeck & Bergmann 1938
Scotch pine Pinus sylvestris Franchomme & Penoel 1991
Myrrh Commiphora myrrha Franchomme & Penoel 1991
Clary sage Salvia sclarea Zondeck & Bergmann 1938
Geranium Pelargonium graveolens Belaiche 1979
Thyme Thymus vulgaris Belaiche 1979
Aniseed, fennel rans-anethole Albert-Puleo 1980
Lemongrass, melissa, Citral Geldof et al 1992
verbena

violent and irrational, a sedative such as angelica (Franchomme & Penoel 1991) or
ylang ylang could be used (Bucellato 1982). Geranium (Pelargonium graveolens) is
an excellent hormonal balancer. The aqueous extract of Pelargonium graveolens has
the added bonus of inhibiting platelet aggregation (Tzeng et al 1991), thereby pos-
sibly preventing extensive clotting during menstruation, which so often accompa-
nies hormonal imbalance. A Korean study (Han et al 2003) indicated that 2% clary
sage applied to the abdomen of menstruating women reduced the uterine ....and
substantially reduced dysmenorrhea.
I have had some success using tarragon in conjunction with estrogen-like es-
sential oils on women who have displayed aggressive PMS. One patient actually ad-
mitted “going for my husband with a knife.” Although tarragon (Artemisia dracun-
culus) has fallen out of favor recently due to its estragole content, the research that
gave rise to that view involved administering very large doses of estragole orally to
rats over a period of 12 months (Tisserand & Balacs 1995). The oral route would
ensure that substantially more estragole was absorbed than by the topical route, and
much higher doses were used in the study than are used in aromatherapy.
Buckingham (2000) investigated the effect of essential oils on 14 women
(aged 21-43) with moderate to severe PMS in a controlled study lasting 6
months. One symptom was chosen by each participant and matched to a specific
essential oil. The results indicated each of the chosen essential oils, except
surprisingly clary sage, had a beneficial effect on menstrual symptoms. See Table
18-3 for study findings.
Menopausal Problems
The menopause is the natural cessation of a woman’s fertility. Estrogen levels fall
to 40%-60% of premenopausal level, and progesterone levels fall to almost zero
(Moskowitz 2001). Once looked upon with secret delight as the end of menstru-
ation and its accompanying messy problems, menopause now seems to be viewed
by many women with dismay and despair and by orthodox medicine as a condi-
tion to be fixed. Menopausal depression is thought to be one of the main symp-
298 Section II Clinical Use of Aromatherapy
Table 18-3 h Essential Oils Used in Buckingham’s Study
Essential Oil Disorder Treated
True lavender Anxiety
True lavender Breast tenderness
Juniper Fluid retention
Juniper Breast tenderness
Clary sage Low-back pain
Geranium Mood swings
Geranium Nervous tension

toms of women seeking hormone replacement therapy (HRT) (Andrist 1998), al-
though older women seem more concerned with osteoporosis and younger
women with hot flashes (Ettinger & Pressman 1999). Between one- and two-
thirds of woman discontinue HRT during the first 2 years because of weight gain
and unwanted side effects such as bloating and breakthrough bleeding (Den
Tonkelaar & Oddens 2000).
Hot flashes, night sweats, sleep disturbance, depression, loss of energy,
and loss of concentration are all common symptoms of menopause (Schmid &
Rubinow 1994). However, cessation of estrogen and progesterone production
does not happen overnight, and it is the interim imbalance that is so difficult.
Essential oils such as rose (Belaiche 1979), cypress (Valnet 1993), or clary
sage can be helpful when used in a hydrosol spray or spritzer sprayed around the
face, neck, and shoulders during a hot flash. A few drops of peppermint added to
the mix is wonderfully cooling. Essential oils that could be used for estrogen sup-
port include fennel (Marini-Bettolo 1979), sage (Franchomme & Penoel 1991),
and aniseed (Albert-Puleo 1980). Geranium (Holmes 1993) and rose give added
support. Using a mixture of essential oils on a daily basis can be very beneficial ei-
ther on a tissue or in a bath or body lotion. I used menopausal oils in this way
for several years with no ill effect. Rotating the mix of calming and estrogen-
supportive essential oils will prevent the body from becoming inured to the es-
sential oils. The combinations and permutations of some 20 essential oils can
work out to be a great number of different mixes—all therapeutic and beneficial
for menopausal symptoms (Table 18-4).
For night sweats, cypress, with its recognized deodorant effect and hormonal
properties, is comforting (Valnet 1993). For insomnia, any of the gently relaxing
and sedative oils could be added, but try also root of Angelica archangelica (Duke
1985). Increasing soy intake and taking daily food supplements such as red clover
and black cohosh will also help tremendously as these phytoestrogens can help
balance wildly fluctuating hormone levels.
Chapter 18 Endocrinology 299
Table 18-4 h Essential Oils for Menopause
Common Name Botanical Name Reference
Fennel Foeniculum vulgare Marini-Bettolo 1979
Geranium Pelargonium graveolens Holmes 1993
Rose Rosa damascena Buckle 1997
Clary sage Salvia sclarea Rose 1996
Sage Salvia officinalis Franchomme & Penoel 1991
Anise seed Pimpinella anisum Albert-Puleo 1980
Cypress Cupressus sempervirens Valnet 1993

Shiffman (1995) explored the effects of a selection of fragrance sprays currently
on the market with 56 women aged 45-60 in a placebo-controlled study. Four groups
were assigned depending on hormonal status: 1) still menstruating, 2) no longer
menstruating and taking estrogen, 3) no longer menstruating and taking estrogen
and progesterone, 4) no longer menstruating and not taking either estrogen or prog-
esterone. While the scents supplied were not specified and probably were synthetic,
the effects indicated that pleasant scents alleviated depression and confusion in
women at midlife and were more effective in those women taking hormone replace-
ment. Schiffman suggests the positive effects may be because pleasant aromas im-
prove mood, thus releasing a broad range of transmitters in the limbic system.
Kozlowski (2000) explored the use of clary sage and geranium on 11
menopausal women aged 47-56 using a 5% solution applied to the reflexology
point for ovaries and uterus on the feet. Clary sage produced some useful changes
in hot flash intensity. One subject wrote that two nights after stopping clary sage,
the hot flashes returned to their original intensity.
Both the above conditions occur exclusively in women and, fall more under
gynecology than endocrinology, so perhaps a very brief mention of diabetes (an
endocrine disorder that affects both men and women) and the use of essential oils
might be in order.
Diabetes
Baschetti (1998) explored the hypothesis that the epidemic of diabetes in newly
Westernized populations could be due to genetically unknown foods as well as a
surge in calories from increased fat intake. There were no instances of diabetes in
Nauru, an island in the Pacific, in a 1933 medical survey. But by 1978, 44% of the
population had noninsulin-dependent diabetes mellitus (NIDDM). Similarly,
there was only one possible incidence of NIDDM among Pima Indians in Ari-
zona in 1908, but currently it is present in 50% of adults over 35 years of age
(Knowler et al 1981).
These two studies, and the dramatic increase in diabetes in the United States
during the last 10 years, suggest Westernized people could be adding something
to their diets that their bodies cannot metabolize. The increase in diabetes has
been linked to the increase in sugar consumption and to the increase in obesity.
Rosmarinus officinalis (rosemary) was shown to suppress the insulin response
in a glucose-tolerance test in rabbits when plasma glucose levels remained at 55%
for 2 hours. Rosemary also caused hyperglycemia in rabbits with artificially in-
duced diabetes (Al-Hader & Hasan 1994).
Another study showed that Eucalyptus citriodora (lemon-scented gum) had a
hypoglycemic effect on rabbits (Revoredo 1958). Valnet states that geranium has
antidiabetic properties, although no clarification is given (Valnet 1993). Ylang
ylang is another essential oil thought to be useful in diabetes (Franchomme & Pe-
noel 1991; Sheppard-Hangar 1995; Price 1995), although again no research to
substantiate this view was given.
300 Section II Clinical Use of Aromatherapy

REFERENCES
Albert-Puleo M. 1980. Fennel and anise as estrogenic agents. Journal of Ethnopharma-
cology. 2(4) 337-344.
Al-Hader A, Hasan Z. 1994. Hyperglycemic and insulin release inhibitory effects of
Rosmarinus officinalis. Journal of Ethnopharmacology. 43(3) 217-211.
Alexander M. 2001. How Aromatherapy Works, Vol. 1: Principle Mechanisms in Olfac-
tion. Odessa, FL: Whole Spectrum Books, 293.
Andrist L. 1998. The impact of media attention, family history, politics and maturation
on women’s decisions regarding hormone replacement therapy. Health Care For
Women International. 19(3) 243-260.
Anthony C, Thibodeau G. 1983. Textbook of Anatomy and Physiology. St. Louis, MO:
Mosby.
Bartlett J. Nov. 11, 1999. Meltdown. Forbes.com. www.forbes.com
Baschetti R. 1998. Diabetes epidemic in newly Westernized populations: is it due to
thrifty genes or to genetically unknown foods? Journal of the Royal Society of Medi-
cine. 91(12) 622-626.
Belaiche P. 1979. Syndrome premenstruel. In Traite de Phytotherapie et d’Aromathera-
pie. Paris: Maloine SA. 3: 60-64.
Bennett A, Stamford F. 1988. The biological activity of eugenol, a major constituent of
nutmeg, on prostaglandins, the intestine and other tissues. Phytotherapy Research.
2(3) 125-129.
Buccellato F. 1982. Ylang survey. Perfumer & Flavorist. 7(4) 9-10.
Buckingham C. 2000. Effects of Aromatherapy on PMS. Unpublished dissertation.
Hunter, NY: R J Buckle Associates.
Buckle J. 1997. Clinical Aromatherapy in Nursing. London: Arnold.
Budavari S (ed.). 1996. The Merck Index, 12th ed. Whitehouse Station, NJ: Merck.
Den Tonkelaar I, Oddens B. 2000. Determinants of long-term hormone replacement
therapy and reasons for early discontinuation. Obstetrics & Gynecology. 95(4) 507-
512.
Duke J. 1985. Handbook of Medicinal Herbs. Boca Raton, FL: CRC Press.
Ettinger B, Pressman A. 1999.Continuation of postmenopausal hormone replacement
therapy in a large health maintenance organization: transdermal matrix patch versus
oral estrogen therapy. American Journal of Managed Care. 5(6) 779-785.
Franchomme P, Penoel D. 1991. Aromatherapie Exactement. Limoges, France: Jollois.
Geldof A, Engel C, Rao B. 1992. Estrogenic action of commonly used fragrant agent
citral induces prostatic hyperplasia. Urological Research. 20(2) 139-144.
Han S, Hur M, Buckle J. 2003. A randomized trial of effect of aromatherapy on the
menstrual cramps in college students. In press.
Hahn T. 2001. Anger. New York: Riverhead.
Holmes P. 1993. The Energetics of Western Herbs. Berkeley, CA: NatTrop.
Knowler W, Pettit D, Savage P, et al. 1981. Diabetic incidence in Pima Indians: contri-
butions to obesity and parental diabetes. American Journal of Epidemiology. 113(2)
114-156.
Kozlowski G. 2000. Use of clary sage and geranium on menopausal symptoms. Hunter,
NY: R J Buckle Associates.
Marini-Bettolo G. 1979. Plants in traditional medicine. Journal of Ethnopharmacology.
1(3) 303-306.
Chapter 18 Endocrinology 301

Melzig M, Teuscher E. 1991. Investigations of the influence of essential oils and their
main components on the adenosine uptake by cultivated epithelial cells. Planta Med-
ica. 57(1) 41.
Moretti M, Peana A, Satta M. 1997. A study on anti-inflammatory and peripheral anal-
gesic action of Salvia sclarea oil and its main components. Journal of Essential Oil Re-
search. 9(2) 199-204.
Moskowitz D. 2001. Hormones and balance. In Wilson K, Moskowitz D, Thomas D
(eds.), A Woman’s Health Resource. Portland, OR: Transitions for Health, Inc., 3-37.
Price S, Price L. 1999. Aromatherapy for the Health Professional. London: Churchill
Livingstone.
Reid R. 2002. Premenstrual syndrome. Retrieved March 17, 2003 from
www.endotext.org.
Revoredo N. 1958. Hypoglycemic action of Eucalyptus citriodora. Monitor de la Farmacia
y de la Terapeutica. 64: 37-38.
Rose J. 1992. The Aromatherapy Book. San Francisco: North Atlantic Books.
Rovesti P, Columbo E. 1973. Aromatherapy and aerosols. Soap, Perfumery and Cosmet-
ics. 46: 475-477.
Rubinow D, Schmidt P, Roca C. 1998. Estrogen-serotonin interactions: implications for
affective regulation. Bio Psychiatry. 44(9) 839-850.
Schmidt P, Rubinow D. 1991. Menopausal related affective disorders: a justification for
further study. American Journal of Psychiatry. 148(1) 844-852.
Schwingl P, Hulka B, Harlow S. 1994. Risk factors for menopausal hot flashes. Obstet-
rics & Gynecology. 84(1) 29-34.
Sheppard-Hangar S. 1995. The Aromatherapy Practitioner’s Reference Manual, Vol. 1.
Tampa, FL: Atlantic Institute of Aromatherapy.
Shiffman S. 1995. Pleasant odors improve mood of women and men at midlife. In
Gilbert A (ed.), Compendium of Olfactory Research. New York: Olfactory Research
Fund, Ltd., 97-103.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Tzeng S, Ko W, Ko FN. 1991. Inhibition of platelet aggregation by some flavonoids.
Thrombosis Research. 64(1) 91-100.
Valnet J. 1993. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
van Der V. 1982. The pharmacology of oestriol. Maturitas. 4(4) 291-299.
Wagner H, Wierer M, et al. 1986. In vitro-Hemmung der Prostaglandin-Biosynthese
durch etherische Ole und phenolische Verbindungen. Planta Medica. 184-187.
Zondeck B, Bergmann E. 1938. Phenol methyl ethers as estrogenic agents. Biochemical
Journal. 32: 641-645.
302 Section II Clinical Use of Aromatherapy

W
303
19
Hospice and End-of-Life Care
The whole natural world is scented, yet until today, no one has sought to know why.
Rene-Maurice Gattefosse
Foreword to Gattefosse’s Aromatherapy
H
ospice care may involve care of the actively dying, but it is not the same
as end-of-life care. End-of-life care is just that: care of a person who is
in the immediate process of dying. Hospice care (also known as pallia-
tive care) means caring for someone who may not get better, but who is never-
theless not at death’s door and may live for many years (McCusker 1983). There-
fore, palliative care involves alleviating the effects of disease without curing
(Fowler & Fowler 1964). This may be unattractive to a medical system based on
curing, and Lagay (2001) suggests patients deemed incurable may be neglected.
Hospice care is a great challenge to health-care professionals because there are no
set protocols; each patient is different with different needs. However, this should
be health care’s finest hour.
The philosophy of caring cannot be reduced to a series of actions (Drew &
Dahlerg 1995). To be caring is to be holistic, so it is hardly surprising that aro-
matherapy is used and accepted so readily in hospice care, which sees itself as
holistic—dealing with the whole person. Chapman (1998) suggest that in hospice
care, professional judgement is mainly intuitive. Hillier (2001) writes hospice care
is like an iceberg, with the obvious “doing” comprising less than 15% of the ac-
tual care.
Ninety percent of cancer patients spend their last year of life in their own
homes (Doyle 1986), although during that last year many patients will be admit-
ted to a hospital for a short time. Most Americans say they would like to die at
home, but in reality 20%-50% of Americans die in hospitals (Wennberg 1999).
Hospice care is the process of helping patients live fully for as long as possi-
ble while alleviating suffering. Suffering can be emotional as well as physical. One
of the greatest emotional shocks a person can receive is the knowledge that he or
she has a terminal illness. This sets off an internal process of mourning, with the
associated feelings of numbness, anger, depression, and finally acceptance
(Childs-Gowell 1992). Many patients remain stuck in the second stage with the
question “why me?,” or they displace their anger and sense of unfairness to oth-
ers and make their lives miserable (Kubler-Ross 1978). Perhaps the answer to this
dilemma could be found in the following quotation:
The Pathless Path
There is no answer,
There never has been an answer.
There never will be an answer.
That’s the answer. (Gertrude Stein, 1925)
Our society does little to honor the process of mourning; there is no rite of
passage. The idea of mourning something other than death is given little support,
but patients in palliative care are mourning the death of their future. They know
there will be no happy ending, and although everyone has to die sometime, real-
ization of the close proximity of death comes as a bitter blow to many patients.
There is no way of knowing (outside a hospital) whether a person has a limited
time to live unless he or she chooses to share this knowledge. Many do not share
this information because they feel they cannot. Some find it difficult to put their
feelings into words, and some are fearful of an uncertain response (pity and forced
humor being equally unacceptable), so fear can keep patients locked in a world of
their own, unable or unwilling to communicate.
Aromatherapy and Palliative Care
Gentle touch and beautiful smells can cross these barriers. Touch communicates
a sense of acceptance to such patients, many of whom may have feelings of self-
disapproval (Pratt & Mason 1981). Touch and smell often penetrate the despon-
dency of a patient who is struggling to accept that life is no longer going to be as
he or she had hoped. Touch is an important commodity during palliative care be-
cause patients can often feel more “skin hunger” (Simon 1976). It opens up dia-
logue, while smells nudge memories. Together they can help patients who may
struggle with feelings of anger, denial, guilt, and frustration by allowing them to
verbalize those feelings and communicate at a deeper level.
Attractive smells give pleasure and can relax a patient sufficiently to allow
him or her to open up. Aromatherapy using the “m” technique allows a patient to
experience pleasure, relaxation, and acceptance simultaneously. Trust can occur at
a deep level between caregiver and patient. This level of intimacy allows caregivers
to show their profound love of humanity in a deeply moving way and provide
“comfort care” to their patients (Kolcaba 1995). Many health professionals desire
to give this level of care (Montgomery 1996).
304 Section II Clinical Use of Aromatherapy

Palliative care should embrace the whole family, who may be trying to “re-
main brave.” Smells are not easily hidden, and beautiful smells are an easy way to
begin dialogue with family members. It is not unusual for aromatherapy to act as
the catalyst, allowing patients and their relatives to begin talking to one another
at a useful level. This period before a patient enters the terminal stage is impor-
tant for a peaceful death. It is a time to clear old scores and resolve past disagree-
ments. It is a time of completion, so the process of dying, when it finally occurs,
can be as serene and dignified as possible.
Aromatherapy can aid the management of pain and nausea in a complemen-
tary way, but perhaps aromatherapy’s greatest strength in palliative care lies in its
ability to facilitate communication at an emotional and spiritual level, giving feel-
ings of comfort and pleasure. For this reason, the choice of essential oils should
rest with the patient. Concentrate on offering a selection that could give pleasure
to the patient. If he or she is particularly withdrawn or depressed, an uplifting es-
sential oil known for its gentle antidepressant properties, such as bergamot (Cit-
rus bergamia) or frankincense (Boswellia carterii) would be appropriate. However,
at this particular stage of illness caregivers are offering esthetic aromatherapy,
rather than targeting specific problem areas.
End-of-Life Care
End-of-life care is estimated to account for up to 12% of all health-care spend-
ing in the United States (Emmanuel 1996). Annual expenditure for hospice care
is about $3.5 billion (Levitt et al 2000), although hospices operate with little fi-
nancial aid and are given little state or federal help. For example, New York City
reimburses hospice medications at $1.50 per day, although the average cost for
drugs is $12 per day (Raphael et al 2001). Of the 9.3 million Americans who are
over the age of 85, 83% are women and 43% live alone. By 2060, the population
over the age of 85 (both sexes) will increase by 240%. Medicare spends 40% of its
budget on the last 30 days of a person’s life. However, the cost of the end-of-life
care for a 85-year-old is
1
⁄
3
lower than the cost of a 65-75-year-old patient
(Hogan et al 2000).
The Last Acts project, funded by the Robert Wood Johnson Foundation, was
created in 1997 to educate the public, policymakers, and health-care profession-
als on end-of-life care (Cassel & Demel 2001). The Last Acts project suggests the
following are fundamental to end-of-life care:
respecting patient goals, preferences, and choices;
comprehensive caring;
utilizing the strengths of interdisciplinary resources;
acknowledging and addressing caregivers’ concerns;
building systems and mechanisms of support.
The physical process of dying is recognizable (Newbury 1995). Bodily func-
tions cease, and the peripheral temperature drops as circulation fails, leaving the
skin mottled and discolored. Thirst is often the last craving, with food refused.
Many dying patients breathe through their mouths, which can become dry and
Chapter 19 Hospice and End-of-Life Care 305

cracked. Often their eyes are open, even though the patient may be asleep or un-
conscious. Rattling in the throat occurs when secretions collect in the throat and
the patient is too weak to cough. Although the patient may be unaware of the
sound, it is frequently distressing for relatives in the same room. A change in po-
sition may help, but aromatherapy and gentle massage may also alleviate this
problem (Tattam 1992). Cheyne-Stoke breathing (irregular breathing when the
patient doesn’t appear to breathe for long periods) often occurs in the days prior
to death. Patients may be aware someone is with them, even though they appear
to be deeply unconscious. Hearing is one of the last senses to go, so what is said
in front of a dying patient is important. This is the time for soothing music such
as the work of Therese Schroeder-Sheker (1998).
Many people have a fear of dying alone. Abandonment is a major patient fear,
and anecdotal evidence suggests patients who have “Do Not Resuscitate” orders
are ignored by medical staff (Sulmasy & Rahns 2001). When patients are at the
point of death, they may have been unconscious for some time, but it is still im-
portant to really be there with them. Talk gently to them, read their favorite po-
ems, tell their favorite jokes, and play their favorite music. Tell them you are there
for them, but be sure to give them permission to go. Touch and smell remain im-
portant, and aromatherapy using the “m” technique is a wonderful way to say good-
bye. Pleasant smells are of particular importance in terminal nursing. The smell of
death is something most people working in hospice work can recognize. Certainly
if there are any suppurating lesions, the smell in a patient’s room can be quite un-
pleasant, and patients remain aware of both smell and touch almost until the end.
Other small but highly effective ways to use aromatherapy in terminal nurs-
ing include incorporating floral waters. Currently available antiseptic mouth-care
lotions can be uncomfortable or burn mouths that are fragile and sensitive
(Gravett 1995). Floral waters (hydrolats) are ideal to use as they are water based,
dilute, and very gentle (Kusmerik 1996). Chamomile and cornflower floral waters
are useful for eye care, and linden flowers, myrtle, and orange blossom are useful
for mouth care.
Floral waters provide a gentle way of using aromatherapy. Choose carefully as
some, like neroli, are more astringent than geranium and rose, which are more suit-
able for dry, papery skin (Catty 2001). Wounds can also be cleansed with floral wa-
ters as they are antiseptic and slightly acidic. Floral waters can also be used as com-
presses and are a soothing way to wipe a face.They are excellent to spray around the
bed and on the linen, as they are refreshing to both the dying person and relatives.
Floral waters will leave a very delicate scent behind and are usually tolerated even
by those with a heightened sense of smell. It is important to use true floral waters
and not synthetic blends added to water. Purchase them from a reputable supplier
to ensure the floral water does not contain fungal or bacterial contaminants.
Relatives learn more from what health-care professionals do than from what
they say (Dossey 1994). There is a need to involve relatives in end-of-life care, and
some can be encouraged to massage their loved one’s hands or feet gently. Help
them to choose a particular blend of aromas that has meaning for their loved one.
Perhaps the patient was particularly fond of the rose garden or maybe they always
306 Section II Clinical Use of Aromatherapy

potted geraniums. Perhaps they traveled extensively and enjoyed the scent of or-
ange blossom and ylang ylang. Maybe they lived in foreign countries and walked
through forests of eucalyptus or sandalwood. Perhaps they had a special herb gar-
den. Their favorite smells can be mixed together in a “farewell blend.” This highly
personal blend can be used constantly during the dying process and will become
identified with the person. Following death, this personalized “farewell blend” can
give tremendous comfort to relatives and will help during bereavement.
Katz (1999) carried out a study on 20 patients in the active dying process ex-
periencing terminal agitation or anxiety at her hospice in Pennsylvania. She ap-
plied 1% Lavandula angustifolia with the “m” technique to hands and feet. All the
patients had a decreased pulse and respiration, and all demonstrated physical re-
laxation by unclenching their hands. In 75% of cases, family members verbalized
that they had observed a decrease in agitation. Two comments from her study are
haunting. “There is a sense of peace I haven’t felt since the diagnosis was made,”
and, from a five-year-old “My granny feels better, and I helped.”
O’Keefe (2000) carried out a study on 10 patients using frankincense in a
foot and leg “m” technique and a drop of lavender on the pillow at her hospice in
Arizona. All patients were in the active stage of dying, and some of them died
within hours or days. After treatment, the restlessness of nine of the patients de-
creased. For most, their respiration slowed and became deeper as they became
quieter. Most of them slept peacefully following the treatment. The response of
the patients’ relatives was one of deep appreciation for this level of caring.
Ocampo (2000) carried out a controlled study on six terminally ill patients
experiencing moderate to severe pain at her hospice in New York. Eight volun-
teers were trained in the “m” technique and performed it on patients’ hands. All
patients receiving the “m” technique experienced considerable reduction in their
pain perception, according to a visual analog.The treatment group slept for longer
periods than the control group.
Perhaps the soul does not die but moves on, and just as a newborn child is
welcomed into this world, so should a soul be welcomed into its death. Whatever
the health-care provider believes, by caring for a dying patient in this way, using
familiar smells and gentle touch, the transition from life as we know it is cele-
brated in the most supportive and holistic way possible. Health-care providers are
privileged to be midwives and facilitators of this transition.
Thank you, my friend
For sharing your dying.
I can be with you
To catch a glimpse of the life you are leaving
And the life to which you return.
In the process, I can accompany your tumult,
Your fear, resistance,
And hope.
Thank you my friend
For sharing your soul. (Dorothea Hover-Kramer, 1993; reproduced with
kind permission of the author)
Chapter 19 Hospice and End-of-Life Care 307

REFERENCES
Cassel C, Demel B. 2001. Remembering death: public policy in the USA. Journal of the
Royal Society of Medicine. 94(9) 433-436.
Catty S. 2001. Hydrosols: The Next Aromatherapy. Rochester, VT: Healing Arts Press.
Chapman J. 1998. Agonising about assesssment. In Fish D, Coles C, editors: Developing
Professional Judgement in Health Care: Learning through Critical Appreciation of
Practice. Oxford: Butterworth-Heinemann. 157-181.
Childs-Gowell E. 1992. Good Grief Rituals. Raleigh, NC: Station Hill Press.
Dossey B. 1994. Dynamics of consciousness and healing. Journal of Holistic Nursing.
12(1) 4-10.
Doyle D. 1982. Domiciliary care: terminal care and demands on statutory services.
32(237) 285-291.
Drew N, Dahlerg K. 1995. Challenging a reductionistic paradigm as a foundation for
nursing. Journal of Holistic Nursing. 13(4) 334-337.
Emmanuel E. 1996. Cost savings at the end of life: what do the data show? Journal of
the American Medical Association. 275(24) 1907-1914.
Fowler H, Fowler F, editors. 1964. The Concise Oxford Dictionary of Current English,
5th ed. Oxford, UK: Oxford University Press.
Gattefosse R. 1937. (Translated in 1993 by R. Tisserand.) Aromatherapie: Les Huile
Essentielles-Hormones Vegetales (Gattefosse’s Aromatherapy.) Saffron Walden, UK:
CW Daniels, 89.
Gravett P. July 23,1995. Medicine Now. BBC Radio 4 (broadcast transcript).
Hillier R. 2001. From cradle to grave: palliative medicine education in the UK. Journal
of the Royal Society of Medicine. 94(9) 468-471.
Hogan C, Lynn J, Gable J, et al. 2000. Medicare Beneficiaries’ Costs and Use of Care in
the Last Year of Life: Final Report to the Medicare Payment Advisory Commission.
Washington, DC: Medicare Payment Advisory Commission.
Hover-Kramer D. 1993. Thank you my friend. Journal of Holistic Nursing. 11(1)
115-116.
Katz J. 1999. Does aromatherapy enhance the dying process? Unpublished dissertation.
Hunter, NY: R J Buckle.
Kolcaba K. 1995. Comfort as process and product, merged in holistic nursing art. Journal
of Holistic Nursing. 13(2) 117-131.
Kubler-Ross E. 1978. To Live Until We Say Good-Bye. London: Prentice Hall.
Kusmerik J. 1996. Floral waters. Aromatherapy Quarterly. (49) 5-7.
Lagay F. 2001. Report from the Council on Ethical and Judicial Affairs, September
2001. www.ama-assn.org.
Levitt K, Cowan C, Lazenby H. 2000. Health spending in 1998: signals of change.
Health Affairs. 19: 124-132.
McCusker J. 1983. Where cancer patients die: an epidemiological study. Public Health
Reports. 98(2) 170-176.
Montgomery C. 1996. The care-giving relationship: paradoxical and transcendent as-
pects. Alternative Therapies. 2(2) 52-57.
Newbury A. 1995. The care of the patient near the end of life. In Penson J, Fisher R
(eds.), Palliative care for people with cancer. London: Edward Arnold, 178-198.
O’Keefe M. 2000.The effects of Boswellia carteri and Lavandula angustifolia on the dying
process. Unpublished dissertation. Hunter, NY: R J Buckle Associates.
308 Section II Clinical Use of Aromatherapy

Ocampo A. 2000. The effect of frankincense of alternation of pain perception in hospice
patients. Unpublished dissertation. Hunter, NY: R J Buckle Associates.
Pratt J, Mason A. 1981. The Caring Touch. London: Heyden.
Raphael C, Ahrens J, Fowler N. 2001. Financing end-of-life care in the USA. Journal of
the Royal Society Medicine. 94(9) 458-461.
Schroeder-Sheker T. 1998. The Chalice of Repose Project: prescriptive music in care of
the dying. Third Annual Alternative Therapies Symposium. April 1-4. San Diego,
CA: Innovision. 222.
Simon S. 1976. Caring, Feeling, Touching. London: Argus Communications.
Stein G. 1925. The pathless path. In Dossey L. (ed.). 1995. Healing Words. San Fran-
cisco: HarperSanFrancisco.
Sulmasy D, Rahns M. 2001. Time spent at the bedside of terminally ill patients with
poor progress. American Journal of Medicine. 111(5) 385-389.
Tattam A. 1992. The gentle touch. Nursing Times. 88(32) 16-17.
Wennberg J (ed.). 1999. The Dartmouth Atlas of Health Care. Washington, DC: Amer-
ican Hospital Association Press.
Chapter 19 Hospice and End-of-Life Care 309

310
W
20
Immunology
Everything we need to be whole and healthy is provided for us by nature but,
somewhere along the way, most of us have lost sight of this ancient wisdom.
Dr. Mariano Spieza
Holistic Physician and CEO Speizia Organic Care, Cornwall, England
A
ndrew Weil, MD, (1998) wrote “There is growing evidence that adjunc-
tive therapies can enhance immunity as well as increase the effectiveness
of conventional treatments and minimize their side effects.” During the
last few years it has become evident that essential oils, both through topical ap-
plication and inhalation, can positively impact the immune system by improving
mood, increasing brain activity, and enhancing other biological functions impor-
tant to health and healing (Alexander 2001). Indeed olfaction has a close link
with immunology; the secret of each of our individual aromas may lie in our im-
munology and the way our cells communicate with each other (Lewis 1974).
Immunology is a rapidly growing field, this growth possibly having been pre-
cipitated by the HIV/AIDS epidemic and nurtured by mind-body medicine.
How we feel affects how we are, and that is of particular importance in the use of
aromatherapy. Candace Pert (2000) created a major conceptual shift in neuro-
science with the discovery that the brain, nervous, and immune systems commu-
nicate. She discovered a “gut feeling” about something is a tangible, physiological
function because the gut has opioid receptors. Recent studies indicate stress-
induced neuroendocrine activation can produce profound changes in immune
function (Robinson 1999).
The limbic system has the largest number of peptides and receptors, which
are the substates of emotion, and these are in constant communication with the
immune system. Lymphocytes also secrete endorphins and adrenocorticotropic

hormone (ACTH), a stress hormone previously thought to be excreted exclu-
sively by the pituitary gland. Cells can pick up the “scent” of a peptide on the re-
ceptors of its surface using a process known as chemotaxis (Pert 2000).
Immune System Function
The immune system is highly complicated: a sensitive balancing act linked by nerve
cells that receive directions from and send directions to the brain. Psychological and
emotional factors impact both antibody- and cell-mediated immune function. One
important function of the immune system is its ability to distinguish between self
and nonself. This allows the body to defend itself against infection without harming
its own cells. Alexander (2001) draws attention to the similarity between the im-
mune and olfactory systems: both respond instantly to vast numbers of molecules.
The organs of the immune system produce lymphocytes. These white blood
cells include T cells (so called because they mature in the thymus) and B cells,
which circulate antibodies. Antibodies are tiny proteins belonging to a family of
immunoglobulins. Antibodies will attach themselves to the surface of an antigen
(a foreign invader) much the way a key fits into a lock. Each antibody recognizes
and attaches to a specific antigen.
T cells do not produce antibodies. There are four types of T cells and they
attack foreign invaders in different ways.
Killer cells are constantly on the alert in the bloodstream, looking for foreign in-
vaders. When they find them, the killer cells attach themselves and release
toxic chemicals to destroy the invaders. Just like antibodies, killer cells are
programmed only to kill one thing, whether it is an infective agent, a cell that
has been infected, or transplanted tissue.
Nonkiller cells are also constantly on the alert. These cells can attack a broad
range of targets including both tumor and infection.
Helper cells stimulate B lymphocytes to produce antibodies.
Suppressor cells shut off the helper cells when enough antibodies have been pro-
duced.
For optimum health, helper and suppressor cells should be in balance.
HIV/AIDS patients have a deficiency of helper cells, whereas people with au-
toimmune disease have too many helper cells.
The basic role of the immune system is to defend the body. To do that, it
needs to know what is body and what is not. B lymphocytes tell the body if it has
been invaded, but there is another arm to the body’s defense system, namely the
cellular response, which involves the T lymphocytes.
Psychoneuroimmunology is the study of the reaction between the mind, the
nervous system, and the immune system. In an article published in the Lancet,
stress was linked to a depressed immune system (Cohen & Felten 1995). Research
has shown changes in hormone and neurotransmitter levels alter human immune
responses (Glaser & Glaser 1993). Research also indicates stress can affect the
immune response (Kiecolt-Glaser & Glaser 1991), increase susceptibility to the
Chapter 20 Immunology 311
common cold (Cohen et al 1991), adversely affect conception (Domar et al 1990),
increase the incidence of skin disease (Panconesi 1984), and affect a patient’s per-
ception of pain (Turk & Nash 1993).
Aromatherapy and the Immune System
If aromatherapy elicits the “feel-good” factor, then it may well enhance the im-
mune system. However, some essential oils may impact immune function at a cel-
lular level. Although there is nothing clear-cut here, Penoel (1993) suggests the
effects of phenols could be compared to those of human immunoglobulin M
(IgM). IgM is secreted for a short period of time when the immune system en-
counters a pathogenic organism.
Immunoglobulin G (IgG) is secreted for long-term defense. Penoel (1993)
thinks the action of IgG is mirrored by the behavior of monoterpenic alcohols.
Berkarda et al (1983) reported on the ability of coumarins to increase lymphocyte
transformation values in cancer patients. Coumarins are found (although only in
small quantities) in citrus-peel oils and lavender. Perhaps this is why Rovesti
(1973) thought lavender stimulated lymphocytosis. Lapraz is quoted as saying the
presence “of essential oils in the bloodstream produces leukocytosis” (Mitchell
1993). Valnet (1990) cites Novi who demonstrated the stimulant effect of
“essences of thyme, lavender, lemon, chamomile and bergamot on the white cor-
puscles by which curative leukocytosis is activated, enabling the body to combat
toxins and to resist infectious disease.” Roulier (1990) suggests clove, true ver-
bena, niaouli, and patchouli essential oils could help to balance the immune sys-
tem. However, no studies have measured the effect of aromatherapy on im-
munoglobulins in human blood or saliva—yet. Table 20-1 lists essential oils that
may assist immune function.
312 Section II Clinical Use of Aromatherapy
Table 20-1 h Essential Oils that May Help Immune Function
Common Name Botanical Name Reference
Clove Syzygium aromaticum Roulier 1990
Lemon verbena Lippia citriodora Roulier 1990
Niaouli Melaleuca viridiflora Roulier 1990
Thyme Thymus vulgaris CT thymol Valnet 1990
Lavender Lavandula angustifolia Valnet 1990
Lemon Citrus limon Valnet 1990
German chamomile Matricaria recutita Wagner 1985
Bergamot Citrus bergamia Valnet 1990
Patchouli Pogostemon patchouli Roulier 1990

Other essential oils thought to elevate levels of lymphocytes include Matri-
caria recutita (German chamomile), which increases the number of B lymphocytes
(Wagner 1985), and Citrus bergamia (bergamot), which is thought to be an
immune-system stimulant (Roulier 1990). Philippe Mailhebiau (1995) writes
that Thymus vulgaris CT thymol has strong immunostimulant properties and is
less hepatotoxic than Satureja montana CT thymol.
Perhaps two of the most common immunology problems encountered by
health professionals are rheumatoid arthritis and HIV/AIDS. Although there
is no suggestion that aromatherapy can “cure” rheumatoid arthritis or
AIDS/HIV, it may have a positive impact on immune function through the
feel-good factor. After all, Marette Flies, an eleven-year-old with lupus, was
able to produce the same physiologic response from smelling a rose as from re-
ceiving chemotherapy when she thought she was receiving both (Olness &
Ader 1992).
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic, symmetrical, inflammatory polyarthritis
that affects 3% of the adult population. The peak onset is between ages 25 and
55, and females are more affected than males. Juvenile RA commonly presents
between ages 1-3 years. In addition to arthritis, 20%-35% of patients also mani-
fest severe deformity of rheumatoid modules. These consist of a central area of
fibrinoid necrosis surrounded by macrophages and fibrous tissue containing
chronic inflammatory cells. The wrist subluxes and the radial head becomes
prominent. Extensor tendons in the hand may rupture and adjacent muscles
waste. RA is an autoimmune disorder affecting individuals with a genetic predis-
position who are exposed to an appropriate antigenic stimulus. Once started, the
disease appears to be self-perpetuating. Irreversible destruction of the joint occurs
when granulation tissue invades subchondral bone, tendons, and joint capsule
(Anthony & Thibodeau 1992). Conventional treatment is with nonsteroid anti-
inflammatory drugs, such as ibuprofen, dexamethasone drugs, and cytotoxins.
As rheumatoid arthritis affects specific joints, these areas of the body lend
themselves to the use of compresses. As well as being of great topical comfort and
focusing attention on the affected area of the body (unlike taking a pill), com-
presses allow essential oils to be absorbed through the skin directly to the site of
pain and inflammation. A combination of application methods is usually benefi-
cial, for example, a morning compress and evening bath (which can be a hand- or
foot-bath). It is important to choose the application method to suit the patient.
The whole process of preparing and treating an injured or painful area of the body
carries with it strong placebo effects and mind-body links, which may enhance
the efficacy of the treatment. Of course, some of the essential oil will also be in-
haled, producing a more instant effect. Using aromatherapy in this way we are as-
sisting the body’s own self-healing mechanisms by drawing on the antiinflamma-
tory and analgesic properties of essential oils, as well as their ability to reduce
stress and thereby impact the immune system.
Chapter 20 Immunology 313

Essential oils have some of their most poignant antiinflammatory effects
at the level of dermis and epidermis (Boyles 2000). Sawada et al (1980) explored
the activity of euglobal III in a hexane extraction of Eucalyptus globulus and found
it inhibited granulation tissue, which forms inappropriately in cases of RA.
Euglobal III has the structure of a bicyclic sesquiterpene, so Eucalyptus globulus
may be a useful essential oil to try. Inflammation in RA is caused by an increased
flow of blood to the affected area, bringing with it heat, swelling, and pain (Mills
1991). (For more information please see section of Chapter 12 on inflammation.)
I have found a mixture of essential oils that addresses each of these three symp-
toms can be helpful. Choose cooling, astringent, and analgesic essential oils, as
well as those that have antiinflammatory properties (Tables 20-2 and 20-3).
Sometimes heating inflammation can have a more soothing effect than cooling.
Some sesquiterpene lactones have powerful antiinflammatory properties because
they inhibit cellular response (Mazor et al 2000).
314 Section II Clinical Use of Aromatherapy
Table 20-2 h Antiinflammatory Components of Some Common
Essential Oils
Antiinflammatory
Common Name Botanical Name Component(s) Reference(s)
German Matricaria recutita Bisabolol, Carle & Gormaa
chamomile chamazulene 1992, Safayhi
et al 1994
Helichrysum Helichrysum italicum Italidiones Franchomme &
subsp. serotinum Penoel 1991
Rosemary Rosmarinus officinalis 1,8-cineole Juergens et al
CT cineole 1998
Black pepper Piper nigrum Beta-caryophyllene Tambe et al
1996
Table 20-3 h Analgesic Components of Some Common Essential Oils
Analgesic
Common Name Botanical Name Component(s) Reference
Lavender Lavandula Linalyl acetate, Re et al 2000
angustifolia linalool
West Indian Cymbopogon Myrcene Lorenzetti et al 1991
lemongrass citratus
Peppermint Mentha piperita Menthol Tyler et al 1988
Turkish oregano Origanum onites Carvacrol Aydin & Ozturk 1996
Brazilian mint Mentha X villosa Rotundifolene Almeida et al 1996

Rheumatoid arthritis may be eased by cooling or by heat. Patients will know
which they find most comforting. Using a cold (or hot) compress can augment
the effect of essential oils. If a patient says heat helps relieve the pain, add a drop
of an essential oil with vasodilatory properties such as Piper nigrum (black pep-
per) or clove to bring heat to the affected area. If the patient prefers a cooling ef-
fect, add Mentha piperita (peppermint) to cool the area. In all cases, it is impor-
tant to allow patients to choose the essential oils. Let them smell the mixture
before it is applied to their skin; after all, they will have to live with it! The “m”
technique can be a useful method of applying oils.
HIV and AIDS
The prevalence of human immunodeficiency virus (HIV) and acquired immune
deficiency syndrome (AIDS) continues to rise in the United States and in many
other parts of the world. In June 1999, the number of people living with
HIV/AIDS in the United States was 950,000 (UNAIDS 2001). It is estimated
that every minute, five people between the ages of 10 and 24 become infected
with HIV somewhere in the world (Sowell et al 1999). As HIV does not have
to be reported in many countries, the estimate is conservative (Beal & Nield-
Anderson 2000). Approximately 50% of people with HIV or AIDS are using
complementary and alternative medicine (CAM) to treat their illness (Dwyer et
al 1995). Initially, HIV-infected people or those who had progressed to AIDS
used CAM therapies thought to have immunostimulatory or antiviral properties
(Elion & Cohen 1997). However as antiretroviral drugs became more successful,
patients began choosing to add CAM to their conventional regimes for specific
symptom relief (Targ 2000). Commonly used therapies were acupuncture for pain
(Shlay et al 1998) and massage therapy (Ironson et al 1996) and herbal supple-
ments to boost immunity (Coss et al 1998). Although aromatherapy is a lesser-
known complementary therapy, it has much to offer in HIV/AIDS treatment in
terms of control of resistant infections, altering perceptions of pain, and the feel-
good factor.
There has been a tremendous increase in research into plants that could be
of value in the treatment of patients with HIV and AIDS. Some research has in-
volved specific plants that could inhibit reverse transcriptase production of spe-
cific tumours (Kusumoto et al 1992), while other research has concentrated on
additional antitumor and antiHIV agents (Cardellina & Boyd 1995). Many of
these studies have shown encouraging results, although the research is still in its
preliminary stages (Nakashima et al 1992; Mahmood et al 1993; De Tommasi et
al 1991; Schols et al 1991). Water and methanol extracts (not essential oil) of Rosa
damascena exhibited moderate antiHIV activity in a paper by Mahmood et al
(1996). Rosa damascena was found to reduce the maturation of the infectious
progeny virus due to selective inhibition of the viral protease. However, to date
it is aqueous extracts rather than the essential oils that have been investigated.
Yamasaki et al 1998 examined 45 aqueous herbal extracts from the Labiatae fam-
ily. Melissa officinalis, Mentha piperita var. crispa (grapefruit mint), Ocimum
Chapter 20 Immunology 315

basilicum var. cinnamon, and Satureja montana showed potent antiHIV activity (at
a dilution of 16 g/ml).
Hypericin and pseudohypericin, components of Hypericum perforatum (St.
John’s wort), were found to be effective against HIV in vitro (Meruelo et al 1988).
However, the 1999 phase-1 study of 30 HIV-infected people with CD4 counts
lower than 350 cells/mm
3
found 48% of the subjects could not tolerate the severe
phototoxic side effects (Gulick et al 1999). This could be because the two
chemical components (hypericin and pseudohypericin) had been isolated from
the whole plant. In the case of essential oils (and herbs in general), when a com-
ponent is removed from the whole plant and used on its own, the results can be
skewed. A clear example of this is lemongrass. Citral is an aldehyde that makes
up 85% of lemongrass. When citral is removed from lemongrass and used at 50%
dilution on the skin, it can cause erythema. However, if the whole essential oil is
used, a 50% dilution will not result in erythema. This is because lemongrass also
contains d-limonene, a terpene that appears to have a “quenching effect,” so no
burning occurs (Tisserand & Balacs 1995).
There is no published research on the effects of essential oil of Hypericum
perforatum on the AIDS/HIV, but the essential oil is being used for depression.
New studies contraindicate the use of St. John’s wort with protease inhibitors, and
the essential oil might also need to be avoided (Breckenridge 2000). However,
while the essential oil does not contain hypericin and pseudohypericin, it does
contain quercetin, a pentahydroxyflavone (Wells 2001) that gives the essential oil
its dark-red color. Quercetin is noted by Duke (1992) as having in-vitro antiHIV
properties (inhibitory concentration 1 g/ml), which indicates the essential
oil could be an interesting new avenue for antiretroviral research.
Opportunistic infections can cause morbidity and death in people with HIV
(Torres 1993), but there is in-vitro evidence that candidiasis, cryptococcosis, her-
pes simplex, and tuberculosis (TB) are sensitive to specific essential oils. Because
candidiasis, herpes, and TB have been covered in other sections, this section will
concentrate on cryptococcosis.
Remember, the strength of aromatherapy lies in its feel-good factor and its
ability to alleviate symptoms of HIV/AIDS and the side effects of conventional
medicine rather than any ability to cure the underlying disease.
Cryptococcosis
This yeast infection is spread from pigeon droppings and begins as a sporadic dis-
ease manifesting with lung infestation. From the lungs, yeast cells migrate to the
central nervous system and brain via the blood. Standard treatment is fluconazole,
itroconazole, or amphotericin B encapsulated in liposomes (Cordonnier 1993).
However, clinical resistance occurs fairly quickly.
Sixty percent of essential oils are known to possess antifungal properties
(Deans et al 1989), and aromatherapy is particularly suitable for lung treatment.
When essential oils are inhaled they directly target the affected area and do not
316 Section II Clinical Use of Aromatherapy

need to be digested as oral medication. Electrical or battery-operated diffusers and
nebulizers are the most effective ways of getting essential oils into the lungs. Neb-
ulizers are a very suitable method of treatment for lung infestations of yeast, fungi,
or bacteria as they fill the air with a very fine mist of micromolecules of essential
oil, and they can be programmed to come on and off at specific times. For recom-
mended distributors of essential oils and nebulizers, please see Appendix IV.
Effective Essential Oils
Voillon and Chaumont (1994) tested the susceptibility of a strain of Cryptococcus
neoformans isolated from the blood of a patient with AIDS to 25 essential oils and
17 separate chemical constituents found in essential oils. Antifungal activity was
tested by dilution method on solid Sabouraud dextrose agar DIFCO with chlo-
ramphenicol 0.005%. (The presence of chloramphenicol assured the inhibition of
possible pollution by bacteria that could confound the results.) Ten l of Cryp-
toccocus neoformans from the patient’s blood was spread on the culture. (A l is a
microliter or a millionth of a liter.) Cells were counted and the plates incubated
at 37° C for 48 hours. Then the minimum inhibitory concentration was measured.
Many of the essential oils used showed good fungistatic action. The best ef-
fects were from palma rosa, geranium, savory, sandalwood, thyme, marjoram, and
lavender. These are all common, inexpensive essential oils. What was interesting
about this study was that lavender and sweet marjoram, two essential oils previ-
ously been found to be ineffective against Cryptococcus neoformans on fungal
growth in vitro, were very effective when the fungus was isolated from infected
human tissue. This appeared to agree with the findings of Dr. Jean Valnet (1990),
who said the terrain of the patient is very important in control of infection.
Due to the high volatility, Voillon and Chaumont (1994) hypothesized es-
sential oils would be effective against pulmonary cryptococcosis, would easily
penetrate into the tissues due to their low molecular weight, and would easily
reach the cerebral spinal fluid in cases of meningitis. The researchers further hy-
pothesized essential oils would be less toxic than conventional drugs as they have
fewer side effects.
Lemongrass, Eucalyptus globulus, palma rosa, and peppermint were the most
effective essential oils tested against Cryptococcus by Pattnaik et al (1996). Lemon-
grass was effective not only against Cryptococcus but against 11 other fungi tested
in low dilutions. Minimum inhibitory concentration for each of the four essential
oils against Cryptococcus was 5l/ml
-1
. While the way essential oils work as fungi-
cides is not completely clear, it seems metabolism and growth of the fungus is in-
hibited, often with a breakdown in the lipid part of the membrane, resulting in
increased permeability and/or rupture (Larrondo & Calvo 1991). The main con-
stituent of lemongrass is citral, and Larrondo and Calvo (1991) have compared
the topical and inhaled action of citral to the systemic effects of clotrimazole.
Patchouli was found to be effective against Cryptococcus and 16 other patho-
genic fungi and commensal bacteria in a study by Yang et al (1996). In this in-
vitro study, essential oil of patchouli from three different countries, China, In-
Chapter 20 Immunology 317

donesia, and India was compared. Interestingly, only the Chinese patchouli was
effective against Cryptococcus neoformans. This was attributed to the higher con-
tent of patchouli alcohol (41%) as compared to 20%-23% in the Indonesian and
Indian essential oils. These findings underline the importance of knowing the
chemistry of the essential oil. In this case, the chemistry was directly related to
where the plant was grown.
Soliman et al (1994) tested essential oil of rosemary (Rosmarinus officinalis).
They investigated the essential oil distilled from two plants growing in different
climatic conditions. They found both rosemary essential oils were effective
against Cryptococcus neoformans in vitro and recommended either essential oil as
an effective treatment in AIDS patients with cryptococcal meningitis and pneu-
monia. While both rosemarys were effective, it could have been a different chem-
ical component in each oil that contributed to the success of the study.
Eugenol is a phenolic component found in several essential oils. An in-vitro
study found it to be effective against 33 strains of Cryptococcus neoformans using
isolates from human patients (Boonchild & Flegel 1982). The researchers con-
cluded eugenol would be effective against cutaneous mycoses, but toxicity tests
excluded the use of eugenol as a systemic agent. As a phenol, eugenol would not
be suitable for extensive use on the skin as it can be irritating and is hepatotoxic
(Schnaubelt 1999). Eugenol is found in clove and savory, two essential oils to be
used with caution on the skin but they could be used in small amounts in a neb-
ulizer. Table 20-4 lists essential oils used in the treatment of infections of Cryp-
tococcus neoformans.
318 Section II Clinical Use of Aromatherapy
Table 20-4 h Essential Oils for Treating Infections
of Cryptococcus neoformans
Common Name Botanical Name Reference
Rosemary Rosmarinus officinalis Soliman 1994
Palma rosa Cymbopogon martini Viollon 1994
Geranium Pelargonium graveolens Voillon & Chaumont 1994
Marjoram Origanum majorana Voillon & Chaumont 1994
Sandalwood Santalum album Voillon & Chaumont 1994
Lemongrass Cymbopogon citratus Voillon & Chaumont 1994
Eucalyptus Eucalyptus globulus Voillon & Chaumont 1994
Patchouli Pogostemon cablin Voillon & Chaumont 1994
Basil Ocimum basilicum Voillon & Chaumont 1994
Cypress lavender Santolina chamaecyparissus Suresh 1995

Patients with HIV and AIDS are especially appreciative of touch and smell.
I have found that Boswellia carterii (frankincense) is particularly useful. It seems
to help even the most defensive patient to open up, often with tears of release.
Citrus aurantium (neroli) and Rosa damascena (rose) both have wonderful aromas
that most patients like. However, if the aroma seems too flowery, Origanum mar-
jorana (sweet marjoram), Angelica archangelica (angelica root), or Santalum album
(sandalwood) are often acceptable alternatives.
Diarrhea is often a problem in the immune-compromised patient. Several
studies have indicated the oral use of essential oils might be one way of control-
ling this debilitating symptom. Hajihashemi et al (2000) found essential oil of Sa-
tureje hortentis (given orally) was effective against diarrhea in mice. Orafidiya and
Elujoba (2000) conducted a controlled, in-vivo study with mice and found Oci-
mum gratissimum (Holy basil) to be an effective agent against diarrhea. The es-
sential oil reduced fecal output in a dose-dependent manner, with the highest
dose of 7.91 g/ml similar to the action of the control, loperamide (an opioid that
inhibits perastalsis), but at a fraction of the cost.
In a study on humans, a British physician (Gravett 2001) found that oral
doses of essential oils were as effective as conventional medication (codeine phos-
phate 120 mg and Buscopan 20 mg) in high-dose chemoinduced diarrhea. Eighty
patients were randomly allocated into two groups. The experimental group took
an essential oil blend: 15 drops of geranium, 10 drops of German chamomile, and
10 drops of patchouli which were mixed with tumeric phytol and divided into
three portions. The three portions were blended into warm water and honey and
taken three times a day. There was no difference in overall duration of hospital-
ization but the diarrhea in patients who took the essential oils was marginally less.
The cost of the aromatherapy treatment was about 40 cents a day compared to
more than $4 a day for conventional treatment. Finally, Lavandula intermedia CT
grosso was found to be effective against nontubercular opportunistic mycobac-
terum in a sternal wound (Gabrielli et al 1988).
REFERENCES
Ader R, Cohen N, Felten D. 1995. Psychoneuroimmunology: interactions between the
nervous system and the immune system. Lancet. 345(8942) 99-103.
Alexander M. 2001. How Aromatherapy Works. Odessa, FL: Whole Spectrum Books.
Almeida R, Hiruma C, Barbosa-Filho J. 1996. Analgesic effect of rotundifolene in ro-
dents. Fitoterapia. 67(4) 334-339.
Beal M, Nield-Anderson L. 2000. Acupuncture for symptom relief in HIV positive
adults: lessons learned from a pilot study. Alternative Therapies in Health and Medi-
cine. 6(5) 33-42.
Berkarda B, Bouffard-Eyuboglu H, Derman U. 1983. The effect of coumarin derivatives
on the immunological system of man. Agents and Actions. 13(1) 50-52.
Boonchird D, Flegel T. 1982. In vitro activity of eugenol and vanillin against Candida albi-
cans and Cryptococcus neoformans. Canadian Journal of Microbiology. 28(11) 1235-1241.
Chapter 20 Immunology 319

Boyles J. 2000. The Basic Chemistry of Aromatherapeutic Essential Oils. Sydney, Aus-
tralia: Pirie Printers.
Breckenridge A. Important news from the committee on safety of medicine. Retrieved
March 28, 2003 from www.cascade-drugs.org.uk/.
Cardellina J, Boyd M. 1995. Pursuits of new leads to antitumour and anti-HIV agents
from plants. Proceedings of the Phytochemical Society of Europe. Oxford, UK: Ox-
ford Science Press, 81-93.
Carle R, Gormaa K. 1992. The medicinal use of Matricaria flos. British Journal of Phy-
totherapy. 2(4) 147-153.
Cohen S, Tyrrell D, Smith A. 1991. Psychological stress and susceptibility to the com-
mon cold. New England Journal of Medicine. 325(9) 606-612.
Cordonnier C. 1993. Les traitment preventifs et curatifs des mycoses en oncohematolo-
gie. In Euromedicine 1993. Monpelier-Le corum. Rencontres internationals de
recherches et de technologies medicales et pharmaceutiques. Paris: 10-13 November.
Coss R, McGrath P, Caggiano V. 1998. Alternative care: patient choices for adjunct
therapies within a cancer center. Cancer Practice. 6(3) 176-181.
De Tommasi N, De Simone F, De Feo V. 1991. Phenylpropanoid glycosides and ros-
marinic acid from Momardica balsamina. Planta Medica. 57(2) 201.
Deans S, Svoboda K, Kennedy A. 1989. Biological activity of plant volatile oils and their
constituents. Planta Medica. 55(1) 588.
Domar A, Seibel M, Benson H. 1990. The mind/body program for infertility. A new be-
havioural treatment approach for women with infertility. Fertility and Sterility. 53(2)
246-249.
Duke J. 1992. Handbook of biologically active phytochemicals and their activities. Boca
Raton, FL: CRC Press.
Dwyer J, Salvato-Schille A, Coulston A. 1995. The use of unconventional remedies
among HIV positive men living in California. Journal of the Association of Nurses in
AIDS Care. 6(1) 17-28.
Elion R, Cohen C. 1997. Complementary Medicine and HIV infection. Complemen-
tary and Alternative Therapies in Primary Care. 24(4) 905-919.
Gabrielli G, Loggini F, Cioni P, et al. 1988. Activity of lavandino essential oil. Pharma-
cological Research Communications. 20(Suppl. V) 37-41.
Glaser J, Glaser R. 1993. Mind and immunity. In Mind-Body Medicine. New York:
Consumer Report Books, pp. 39-59.
Gravett P. 2001. Treatment of gastrointestinal upset following high-dose chemotherapy.
International Journal of Aromatherapy. 11(2) 84-86.
Gulick R, McAuliffe V, Holden-Wiltse J, et al. 1999. Phase 1 studies of hypericin, the
active compound in St John’s Wort, as an antiretroviral agent in HIV-infected adults.
Annals of Internal Medicine. 130(6) 510-514.
Hajihashemi V, Sadraei H, Ghannadi A, et al. 2000. Antispasmodic and anti-diarrhoeal
effect of Satureja hortensis essential oil. Journal of Ethnopharmacology. 71(1-2)
187-192
Ironson G, Field T, Scafadi F, et al. 1996. Massage therapy is associated with enhance-
ment of the immune system’s cytotoxic capacity. Int Journal of Neuroscience. 84(1-4)
205-217.
Juergens U, Stober M, Schmidt-Schilling L, et al. 1998. Anti-inflammatory effects of
eucalyptol (1,8 cineole) in bronchial asthma: inhibition of arachidonic acid metabo-
lism in human monocytes ex vivo. European Journal of Medical Research. 2(9)
407-412.
320 Section II Clinical Use of Aromatherapy

Kiecolt-Glaser J, Glaser R. 1991. Stress and the immune system: human studies. In Tas-
man A, Riba M. (eds.), Annual Review of Psychiatry, Vol. 11. Washington, DC:
American Psychiatric Press, 169-180.
Kusumoto I, Shimada E. 1992. Inhibitory effects of Indonesian plant extracts on reverse
transcriptase of an RNA tumour virus. Phytotherapy Research. 6: 241-244.
Larrondo J, Calvo M. 1991. Effect of essential oils on Candida albicans: a scanning elec-
tron microscope study. Biomedical Letters. 46(184) 269-272.
Lewis T. 1974. The Lives of a Cell: Notes of a Biology Watcher. New York: Viking.
Mahmood N, Piacente S, Pizza C, et al. 1996. The anti-HIV activity and mechanism of
action of pure compounds isolated from rosa damascena. Biochemical and Biophysical
Research Communications. London: Academic Press. 229(1) 73-79.
Mailhebiau P. 1995. The thymus folder. Les Cahiers de l’Aromatherapie. 1: 38-60.
Mazor R, Menendez I, Ryan M, et al. 2000. Sesquiterpene lactones are potent inhibitors
of interleukin 8 gene expression in cultured human respiratory epithelium. Cytokine.
12(3) 239-245.
Meruelo D, Lavie G, Lavie D. 1988. Therapeutic agents with dramatic antiretroviral ac-
tivity and little toxicity at effective doses: Aromatic polycyclic diones hypericin and
pseudohypericin. Proceedings of the National Academy of Sciences. 85:5230-5234.
Mills S. 1991. Out of the Earth. London:Viking Arkana.
Mitchell S. 1993. Dementia. International Journal of Aromatherapy. 5(2) 20-23.
Nakashima H, Murakami T, Yamamoto N. 1992. Inhibition of human immunodefi-
ciency viral replications by tannins and related compounds. Antiviral Research. 18(1)
91-103.
Olness K, Ader R. 1992. Conditioning as an adjunct in the pharmacotherapy of Lupus
Erythematosus. Developmental and Behavioral Pediatrics 13(2) 127-127.
Panconesi E (ed.). 1984. Clinics in Dermatology, Vol. 2: Stress and skin diseases: psy-
chosomatic dermatology. Philadelphia: JB Lippincott.
Pattnaik S, Subramanyam V, Kole C. 1996. Antibacterial and antifungal activity of es-
sential oils in vitro. Microbios. 86(349) 237-246.
Penoel D. 1993. The immune system of mankind. In Aroma 93 Conference Proceedings.
Brighton, UK: Aromatherapy Publications.
Pert C. 2000. Molecules of Emotion. New York: Scribner.
Re L, Barocci S, Sonnino S, et al. 2000. Linalool modifies the nicotinic receptor-ion
channel kinetics at the mouse neuromuscular junction. Pharmacological Research.
42(2) 177-182.
Robinson F. 1999. Stress and HIV disease progression: psychoneuroimmunolgocial
framework. Journal of the Association of Nurses in AIDS Care. 10(1) 21-31.
Roulier G. 1990. Les Huiles Essentielles Pour Votre Sante. St Jean-de-Braye, France:
Dangles.
Rovesti P, Columbo E. 1973. Aromatherapy and aerosols. Soaps, Perfumery and Cos-
metics. 46: 49-54.
Safayhi H, Sabieraj J, Sailer E, et al. 1994. Chamzulene: an antioxidant-type inhibitor of
leukotriene B4 formation. Planta Medica. 60(5) 410-413.
Sawada T, Tozuka M, Komiya T, et al. 1980. A novel granulation inhibiting agent from
Eucalyptus globulus. Chemical & Pharmaceutical Bulletin. 28(8) 2546-2548.
Schnaubelt K. 1999. Medical Aromatherapy. Berkeley, CA: Frog Ltd., 179.
Schols D, Wutzler P, Klocking R. 1991. Selective inhibitory activity of polyhydroxycar-
boxylates derived from phenolic compounds against human immunodeficiency virus
replication. Journal of Acquired Immune Deficiency Syndrome. 4(7) 677-684.
Chapter 20 Immunology 321

Shlay J, Chaloner K, Max M. 1998. Acupuncture and amitriptyline for pain due to HIV
related peripheral neuropathy. Journal of the American Medical Association. 280(18)
1590-1595.
Sowell R, Moneyham L, Arnada-Naranjo B. 1999. The care of women with AIDS.
Nursing Clinics of North America. 34(1) 179-198.
Spieza M. 2002. Mission Statement. Retrieved October 10, 2001 from
www.spiezaorganics.org.
Tambe Y, Tsujiuchi H, Honda G, et al. 1996. Gastric cytoprotection of the non-
steroidal anti-inflammatory sesquiterpene, beta-carylophyllene. Plant Medica. 62(5)
469-470.
Targ E. 2000. CAM and HIV/AIDS: The importance of complementarity. Alternative
Therapies in Health and Medicine. 6(5) 30-31.
Tisserand R, Balars T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Torres G. 1993. Treatment issues. Gay Men’s Health Crisis: Newsletter of Experimental
AIDS Therapies. 7: 1-2.
Turk D, Nash J. 1993. Chronic pain. New ways to cope. In Goleman D, Gurin J, editors:
Mind-Body Medicine. New York: Consumer Reports Books. 111-131.
Tyler V, Brady L, Robbers J. 1988. Pharmacognosy. Philadelphia: Lea & Febiger.
113-119.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Viollon C, Chaumont J. 1994. Antifungal properties of essential oil components against
Cryptococcus neoformans. Mycopathologia. 128(3) 151-153.
Wagner H. 1985. Economic and medicinal plant research, Vol. 1. London: Academic
Press.
Wells C., Director, Essentially Oils Ltd., Chipping Norton, UK. 1991. Personal commu-
nication.
Yamasaki K, Nakano M, Kawahata T, et al. 1998. Anti-HIV-1 activity of herbs in Lami-
atae. Biological & Pharmaceutical Bulletin. 21(8) 829-833.
Yang D, Micehl D, Mandin D, et al. 1996. Antifungal and antibacterial properties in
vitro of three Patchouli essential oils of different origins. Acta Botanica Gallica. 143(1)
29-35.
322 Section II Clinical Use of Aromatherapy

W
323
21
Obstetrics and Gynecology
Aromatherapy is a relatively modern name for an ancient holistic practice.
Aromatherapy gives us something that is sometimes lacking in other alternative
practices: quite simply, it has the power to make us feel good.
Romy Rawlings (1999)
Healing Gardens
Aromatherapy and Pregnancy
The use of essential oils during pregnancy is controversial, but most fears are un-
founded (Guba 2002). Some aromatherapy schools condone the use of essential
oils in pregnancy during the first trimester, and some question their use at all.
Since the thalidomide tragedy, expectant mothers and their physicians have been
extra cautious of using anything that could have an adverse effect on the unborn
child or the security of the pregnancy. However, essential oils have been used
safely for hundreds of years by thousands of pregnant women in the form of per-
fumes, bath essences, and scented soap.
There are no records of abnormal fetuses or aborted fetuses due to the “nor-
mal” use of essential oils, either by inhalation or topical application. There are no
records of a few drops of essential oil taken by mouth causing any problems ei-
ther. However, there are a handful of records that link two specific essential oils,
pennyroyal and parsley seed, to abortion. The amount of essential oil (taken by
mouth) was extremely high—several milliliters at one time—which caused hepa-
totoxicity. This meant the body was unable to maintain the pregnancy. However,
there were two other cases recorded where the same amount of pennyroyal taken
by mouth did not result in the fetus being aborted, and the mothers recovered.
The amounts taken varied from 10 ml (in the case of pennyroyal) and 1.5-6 ml
for 8 consecutive days (parsley seed). This is between 100 to 200 times greater

than the normal amount of essential oil used in aromatherapy. (Usually only one
to five drops are applied topically to the skin or inhaled.) For internal use, the nor-
mal amount is 0.5-10 ml per day (Brinker 2000). The volume of one drop of es-
sential oil is equivalent to 0.05 ml. This works out to between 10 and 20 drops
per day. There are approximately 20 drops in a milliliter.
There is only one essential oil compound, sabinyl acetate, that has been
shown to have teratogenic effect in laboratory animals (Guba 2002). Sabinyl ac-
etate comprises 20% of savin (Juniperus sabina) and less than 10% of Spanish sage
(Salvia lavandulifolia). Both essential oils should be avoided in pregnancy and
have no aromatherapeutic use. More information on these oils is given in Chap-
ter 4.1 on toxicity.
There are several books available that cover the use of essential oils in preg-
nancy, including two good ones written by midwives: Aromatherapy in Midwifery
Practice by Tiran (1996) and Aromatherapy for the Mother and Baby by England
(1994). England attends 2500 deliveries annually, and Tiran is a lecturer in mid-
wifery at the University of Greenwich. In the United Kingdom, essential oils have
been used during pregnancy and delivery at many hospitals for approximately 15
years, and expectant mothers often appear at the delivery suite with their own box
of essential oils especially chosen for the birth of their child. Essential oils have
been used at Hinchingbrooke Hospital, Huntingdon, St John’s, and St Elizabeth’s
Hospitals in London and at the Radcliffe Infirmary in Oxford, England, since
1987. It would be expected that any adverse effects would have appeared by now.
However, it is always best to err towards caution, and there is no need to use large
amounts of essential oils. Nonetheless, when used correctly, essential oils are very
safe in pregnancy. These substances can give the expectant mother a sense of em-
powerment, reduce the annoying side effects of pregnancy, and can help make her
feel beautiful. If there is a choice between a synthetic chemical (with no studies on
long-term effects) or an essential oil (with hundreds of years of use) it would be
judicious to choose the latter. Aromatherapy can be helpful for many symptoms of
pregnancy: general tiredness, aches and pains, nausea, insomnia, and backache.
Some essential oils are thought to have emmenagogic actions, meaning they
cause tiny uterine contractions and can bring on a menstrual period early. How-
ever the hormonal and physical effects of pregnancy are quite different from those
of the menstrual cycle, and Guba (2002) suggests the topical or inhaled effect of
emmenagogic essential oils will not compromise a stable pregnancy. There is con-
flicting information on exactly which essential oils are emmenagogic. Some au-
thors believe Lavandula angustifolia is emmenagogic but also state it is safe to use
in the first trimester (England 1994).
It is extremely unlikely that a secure pregnancy will be compromised because
a mother has used an emmenagogic essential oil. Babies are difficult to dislodge in
a secure pregnancy. However, if the mother has had a previous miscarriage, it
would be prudent to avoid aromatherapy especially after the first trimester. Brinker
(2000) suggests avoiding angelica, Roman chamomile, cinnamon, any citrus,
myrrh, lemongrass, hyssop, lavender, German chamomile, melissa, peppermint,
324 Section II Clinical Use of Aromatherapy

basil, oregano, black pepper, rosemary, sandalwood, vetiver, and ginger. However, I
have several friends who used aromatherapy throughout their pregnancies. They
have all been uneventful and have produced beautiful babies.
One of the most significant medical events for a pregnant woman is the de-
velopment of pregnancy-induced hypertension (PIH) and its more severe com-
plications: preeclampsia and HELLP syndrome (hemolysis, elevated liver en-
zymes, and low platelets). The patient usually presents with epigastric pain and
blood pressure may or may not be elevated. HELLP is a variant of preeclampsia
and eclampsia.
Pregnancy-Induced Hypertension (PIH)
This condition occurs in 7%-10% of all pregnancies and causes 15% of maternal
deaths. Women who have a history of hypertension before pregnancy are twice as
likely to develop PIH. PIH can also lead to intrauterine fetal death through pla-
cental insufficiency. Orthodox treatment is bed rest with the feet elevated and in-
travenous magnesium sulphate. If the blood pressure does not come down to lev-
els below 150-110/110, labetalol, an alpha- and beta-adrenergic blocking agent,
is given. A blood pressure of 150-160/100-110 constitutes severe preeclampsia,
calling for antihypertensives (hydralazine or labetalol). Common side effects are
drowsiness, fatigue, pulse slower than 50 beats per minute, and nausea. The
mother is kept quiet in a darkened room. However, her mind is unlikely to be
quiet! At such a terrifying time, smell and touch can do much to help reassure a
woman, and reassurance can play an important role in this situation.
Nathan (2000), a midwife on Long Island, New York, used aromatherapy to
help a mother whose blood pressure remained above 200/100 despite intravenous
medication. The patient was continuously monitored for blood pressure and
pulse. Unable to control the hypertension, the attending physician asked Nathan
if she would try aromatherapy. After verbal consent from the patient, Nathan
used a 2% solution of Lavandula angustifolia in a hand “m” technique. Slowly the
blood pressure began to come down. After 15 minutes it was 150/85. The fetal
heart rate also improved, from mid 150s to mid 130s. Within 1 hour, the mother’s
blood pressure was 140/85. The patient was given 5 minutes of “m” technique
with dilute lavender every hour during the night, and her blood pressure was
maintained at 140/85. The mother was discharged 2 days later and went on to full
term. As a result of this case study, Nathan carried out a small project on eight
hypertensive patients in her maternity unit in 2000. Each patient chose rose or
lavender essential oil and received a 5-minute “m” technique on the hand. This re-
sulted in a measurable drop in blood pressure for each patient.
Essential Oils in Labor
Swingle (2001) carried out a study at the Newborn Family Center in Chenango
Memorial Hospital in Norwich, New York, on 25 laboring mothers. Four essen-
tial oils, lavender, geranium, frankincense, and clary sage, were used in 1% dilu-
tion. The oils were used from early labor through delivery. Each essential oil was
Chapter 21 Obstetrics and Gynecology 325

used for specific reasons. Lavender was used for relaxation, to relieve backache,
and to help expel the placenta, and was successful on all counts. Geranium was
used to decrease perineal swelling and to relieve hemorrhoids; it was also suc-
cessful. Clary sage was used to stimulate contractions but was not found success-
ful. Frankincense was used successfully for extreme anxiety between transition
and the second stage of labor. There were no side effects from any of the essen-
tial oils used and everyone commented on their nice aromas.
Adams (2000) carried out a controlled study on the use of lavender to reduce
patient anxiety when labor was induced at Desert Samaritan Hospital in Mesa,
Arizona. One or two drops of lavender were inhaled continuously, or at will, from
a cotton ball. Each of the 23 patients self-evaluated her anxiety level before the
lavender and 30 minutes after the lavender. The levels of evaluation were as fol-
lows: very nervous, nervous, OK, calm, and very calm. The lavender group had a
greater perception of reduced anxiety than the control group. Two subjects com-
mented that their headaches went away when they inhaled lavender. All had pos-
itive comments. The attending nurses’ comments ranged from “patient slept after
lavender,” to “more calm, much more mellow,” to “less anxious, physician very
pleased with effects of lavender.”
Burns et al (2000) evaluated the effect of aromatherapy on 8058 mothers
during an 8-year period (see Table 21-1 for a list of the essential oils used). Moth-
ers in labor were offered aromatherapy to relieve pain, anxiety, or nausea or to
strengthen contractions. Data from the unit audit were used to provide a com-
parison group of mothers not given aromatherapy (n 15.799). Aromatherapy
was offered by a core group of midwives who followed guidelines laid down by a
qualified aromatherapist.
326 Section II Clinical Use of Aromatherapy
Table 21-1 h Essential Oils Used in Burns et al (2000) Study
Common Name Botanical Name
Rose Rosa centifolia
Lavender Lavandula angustifolia
Jasmine Jasminum grandiflorum
Roman chamomile Chamaemelum nobile
Blue gum Eucalyptus globulus
Mandarin Citrus reticulata
Clary sage Salvia sclarea
Frankincense Boswellia carteri
Peppermint Mentha piperita
Lemon Citrus limonum

More than 50% of the mothers found aromatherapy useful. Only 14% of
mothers found it unhelpful. The number of adverse symptoms reported was low
(1%) and included symptoms commonly found in labor such as headache, nausea,
and itchy rash. Aromatherapy was typically used by mothers in established labor
(60%) or in the latent stage (29%). Of the women who used aromatherapy, 32% had
their labor induced. Fewer women needed pain relief in the aromatherapy group
than the control group, and fewer epidurals were given. During the 8 years of study,
the use of pethidine declined. In 1990, 13% of mothers used pethidine. By 1997,
use had dropped to less than 0.2%. Frankincense was found to be the most effec-
tive essential oil for pain. Rose was found to be the most helpful for anxiety (71%).
Peppermint was found to be the most effective for nausea (96%). Aromatherapy did
not appear to augment contractions. However, 70% of multigravidae in dysfunc-
tional labor did not require an oxytocin infusion, and 92% of the mothers went on
to spontaneous vaginal delivery. This is an unusually high figure. Only 36% of
women said they found aromatherapy helped strengthen their contractions, and the
most commonly offered essential oil for this was clary sage (87%).
Vaginal Infections
Yeast Infections
Vaginal yeast infection, caused by Candida albicans, is a common nuisance factor
in many women’s lives. It thrives in an acid environment and is sometimes the
side effect of antibiotics, or it may occur during pregnancy or when a woman is
immune compromised. It is often messy, uncomfortable, and embarrassing and
can reappear with depressing regularity. Antifungal drugs such as Terazol and
Femstat may only bring temporary relief. Other over-the-counter preparations
can be purchased, although some forms of this yeast infection have become resis-
tant to many of the orthodox preparations on the market (Goldway et al 1995).
Candidiasis is uncomfortable and often makes the sufferer feel powerless to cope
with it. However there is one essential oil that may eradicate this fungal infection
permanently and within only a few days (Belaiche 1985). It is called tea tree.
Belaiche (1985) wrote about its effect on vaginal infections 15 years ago.
Tea tree is the name of all species of Melaleuca, Leptospermum, Kunzea, and
Baeckea plants (Guenther 1972). In other words, specifying tea tree is not enough,
as it covers several hundred different plants. In New Zealand, Leptospermum
flavescens is also known as tea tree, but this is a completely different genus, al-
though it belongs to the same family (Myrtaceae) as tea tree. The tea tree needed
to treat vaginal infections is Melaleuca alternifolia. The Australian government has
set standards for the amount of terpineol (an alcohol) and 1,8-cineole (an oxide)
in tea tree. Some tea tree imitations are available that contain high levels of 1,8-
cineole. Occasionally oxides can be uncomfortable when applied to irritated or
abraded vaginal tissue. To avoid this, make sure the bottle of essential oil includes
the botanical name, and purchase it from a reliable source. The functional group,
Chapter 21 Obstetrics and Gynecology 327

alcohols, is kinder on abraded vaginal tissue. The levels of 1,8-cineole and terpi-
neol will show up on a gas chromatograph/mass spectrometer.
Mix two or three drops of Melaleuca alternifolia in 5 ml of cold-pressed veg-
etable oil, like oil of evening primrose or sweet almond oil. Roll a tampon in the
mixture and then insert into the vagina. The simplest method is to mix the es-
sential oil and vegetable oil on a saucer and then roll the tampon in the mixture
until it is saturated. The tampon should be changed three times a day for a new
tampon with a fresh dilution of carrier oil and tea tree. The tampon also needs to
remain in situ overnight. It will not lead to toxic shock syndrome. This is a very
safe and effective method of eradicating candidiasis and many other vaginal in-
fections, and there appear to be no adverse side effects. However, a word of cau-
tion should be given. If the yeast infection has exposed, raw areas in the vaginal
wall, Lavandula angustifolia diluted in vegetable oil should be used first. It can be
applied in exactly the same way, on a tampon, for 1 or 2 days until the excoriated
area has healed. This method has been used successfully in pregnancy with no ad-
verse effects to the mother or baby. Having suggested this treatment to many pa-
tients and colleagues over the last 10 years, I am confident Melaleuca alternifolia
should remove the infection within 3 days, regardless of how long the patient has
had the infection. Table 21-2 lists essential oils effective against Candida albicans.
328 Section II Clinical Use of Aromatherapy
Table 21-2 h Essential Oils Effective against Candida albicans
Common Name Botanical Name Reference
Melaleuca alternifolia
Mentha piperita
Cymbopogon martinii
Eucalyptus globulus
Cymbopogon citratus
Pelargonium graveolens
Pimenta racemosa
Vetiveria zizanoides
Santolina chamaecyparisus
Melissa officinalis
Rosmarinus officinalis
Lippia alba
Picea albies
Belaiche 1985, Pena 1962
Carson & Riley 1994
Pattnaik et al 1996
Pattnaik et al 1996
Pattnaik et al 1996
Pattnaik et al 1996
Chaumont & Bardy 1989,
Viollon et al 1993
Chaumont & Bardy 1989
Suresh et al 1997
Suresh et al 1997
Larrondo & Calvo 1991
Soliman et al 1994
Stiles et al 1995, Kartnig et al
1991
Tea tree
Peppermint
Palma rosa
Eucalyptus
Lemongrass
Geranium
Bay
Vetiver
Santolina
Melissa
Rosemary
Lippia
Austrian pine

Bacterial Infections
Bacterial Vaginosis
Bacterial vaginosis (BV) is a polymicrobial vaginal infection that affects
women of reproductive age (Cook et al 1992). Many of the bacteria, such as Pep-
tostreptococcus, are anaerobic and appear to replace the normally predominant Lac-
tobacilli. One of the main symptoms is copious, smelly discharge, often reducing
a woman to tears of frustration. The fishy smell is from the amine compounds
produced by anaerobes. There is no inflammatory reaction, so there are no white
blood cells in the discharge. Orthodox treatment is oral Metronidazole, which
usually results in normal flora and reduction of symptoms but often produces un-
pleasant side effects such as gastrointestinal upsets or unpleasant taste. A second
treatment is topical clindamycin cream (Cleocin). The cost of a tube of Cleocin
vaginal cream is high, approximately $50 for one-week supply. In 40% of cases
treated with oral Metronidazole, BV recurs within 3 months (Cook et al 1992).
Walsh and Longstaff (1987), Shapiro et al (1994), and Carson and Riley (1993),
tested tea tree against fusobacteria, Prevotella, and Peptostreptococcus bacteria by agar
and broth dilution, and all came up with comparable data. Whereas the previously
mentioned bacteria were susceptible, Lactobacilli were more resistant to tea tree, sug-
gesting that Melaleuca alternifolia could help restore the acid of the vagina and make
it more resistant to pathogenic bacteria. Blackwell (1991) treated a patient with BV
using Melaleuca alternifolia vaginal pessaries with good results. Self-medication with
alternative medicine is common among women with chronic vaginal symptoms
(Nyirjesy et al 1997), and diluted tea tree in cold-pressed carrier oil on a tampon can
be a very effective treatment. Diluted tea tree is pleasant to use and empowering to
the patient. It smells pleasantly antiseptic, and the tampon application makes the
vagina feel fresh. Usually, symptoms will disappear within one week.
Trichomonasas
Trichomonas vaginalis is a bacterial infection that causes inflammation of the
vaginal mucosa accompanied by an unpleasant, pungent discharge. The sufferer is
embarrassed and frequently complains of “feeling dirty.” Conventional treatment
is with systemic or cream Metronidazole. This is expensive. Humphrey suggested
tea tree for trichomonasas as long ago as 1930, and it was found effective by Pena
(1962). Diluted tea tree in cold-pressed carrier oil on a tampon is an effective
treatment. Usually, the bacteria will be gone within one week.
Because the vagina is situated closer to the urethra and essential oils are ab-
sorbed through the walls of the vagina, this is an excellent way of treating cysti-
tis. Essential oils can be absorbed systemically from vaginal application.
Dysmenorrhea
The menstrual cycle is delicately balanced and can easily be thrown out of
equilibrium by stress, illness, or a poor diet. Primary dysmenorrhea manifests
symptoms such as low-abdominal cramping that starts just before or with the
Chapter 21 Obstetrics and Gynecology 329

menstrual flow. This is often associated with nausea, vomiting, headache, and
faintness. Secondary dysmenorrhea usually affects older women who have symp-
toms of congestion and aching associated with low-abdominal cramps that typi-
cally start up to one week prior to menstruation (McFerren 1996). There are
two ways to approach dysmenorrhea using aromatherapy, physically and psycho-
logically.
To address physical symptoms, use a mix of essential oils known for their an-
tispasmodic, hormonal balancing, or analgesic properties (Table 21-3). Many es-
sential oils have antispasmodic properties. Roman chamomile contains more es-
ters than any other essential oil (up to 310 including those from angelic and tiglic
acid) and is thought to be one of the most antispasmodic essential oils available
(Evans 1994). It is also a recognized analgesic (Wren 1988). Han et al (2002) car-
ried out a placebo-controlled study on 85 nurses with dysmenorrhea, using rose,
clary sage, and lavender in 3% dilution applied to the abdomen. The mixture re-
duced the severity of symptoms significantly.
Some essential oils have topical analgesic effect (Table 21-4). Those that are
high in phenols such as clove may be too aggressive to apply to the skin of the
lower abdomen except in very low dilutions and are best avoided.
Geranium is thought to encourage regular ovulation (Belaiche 1979a) and
has been used for generations to balance fluctuating hormonal levels during
menopause through its action on the adrenal cortex (Holmes 1993). Add a few
drops of geranium (Pelargonium graveolens) to the mixture and rub it gently into
the lower abdomen and lumbar area. The best geranium oil comes from Reunion
Island and is usually called Bourbon. For optimum results, repeat the mixture
every hour until dysmenorrhea symptoms have subsided.
Compresses can bring great comfort when applied to the low abdomen. A
hot-water bottle has been an effective remedy for period pains for eons. Placed on
330 Section II Clinical Use of Aromatherapy
Table 21-3 h Antispasmodic Essential Oils for Dysmenorrhea
Common Name Botanical Name Reference
Roman chamomile
Petitgrain
Spearmint
Rosemary
Peppermint
Sage
Lavender
Summer savory
Franchomme & Penoel 1991
Reiter & Brandt 1985
Bulat et al 1999
Al-Sereiti et al 1999
Taddei et al 1988
Taddei et al 1988
Lis-Balchin & Hart 1999
Hajihashemi et al 2000
Chamaemelum nobile
Citrus amara fol
Mentha spicata
Rosmarinus officinalis
Mentha piperita
Salvia officinalis
Lavandula angustifolia
Satureja hortensis

top of an essential oil compress, it will encourage more rapid absorption of the
essential oils, as well as giving the added comfort of heat. This can really help
painful cramps. The whole process of tending a painful area topically brings with
it strong placebo and mind-body links that can only enhance the efficacy of the
therapy.
Psychologically relaxing essential oils can be given in a full body massage or
“m” technique. This will focus attention on the body and its state of relaxation
(unlike taking a tablet). Of course, some of the essential oil will also be inhaled,
producing a psychological effect. Severe dysmenorrhea sometimes brings with it
nausea. Inhaling a little essential oil of peppermint or spearmint will alleviate this.
Aromatherapy, used in this way, works along with the body’s own self-regulating
mechanisms.
REFERENCES
Adams A. 2000. Does Lavandula angustifolia reduce patient anxiety during induced la-
bor? Unpublished dissertation. Hunter, N.Y.: R J Buckle Associates.
Al-Sereiti M, Abu-Amer K, Sen P. 1999. Pharmacology of rosemary and its therapeutic
potential. Indian Journal of Experimental Biology. 37(2) 124-130.
Belaiche P. 1979a. Syndrome premenstruel. In Traite de Phytotherapie et d’Aromathera-
pie, Vol. 3. Paris: Maloine SA, 60-64.
Belaiche P. 1979b. Traite de Phytotherapie et d’Aromatherapie, Vol.1. Paris: Maloine
SA.
Belaiche P. 1985. Treatment of vaginal infections of Candida albicans with essential oil of
Melaleuca alternifolia. Phytotherapie. 15:13-15.
Blackwell R. 1991. Teatree oil and anaerobic (bacterial) vaginosis (letter). Lancet.
337(8736) 300.
Brinker F. 2000. The Toxicology of Botanical Medicine, 3rd ed. Sandy, OR: Eclectic
Medical Publications.
Bulat R, Fachnie E, Chauehan U, et al. 1999. Effect of spearmint on lower oesophageal
sphincter function and acid reflux in health volunteers. Alimentary Pharmacology &
Therapeutics. 13(6) 805-812.
Burns E, Blamey C, Ersser S, et al. 2000. An investigation into the use of aromatherapy
in intrapartum midwifery practice. The Journal of Alternative & Complementary
Medicine. 6(2) 141-147.
Carson C, Riley T. 1993. Antimicrobial activity of the essential oil of Melaleuca alternifo-
lia. Letters in Applied Microbiology. 16:49-55.
Chapter 21 Obstetrics and Gynecology 331
Table 21-4 h Analgesic Essential Oils for Dysmenorrhea
Common Name Botanical Name Reference
Lavender
Lemongrass
Peppermint
Ghelardini et al 1999
Viana et al 2000
Gobel et al 1994
Lavandula angustifolia
Cymbopogon citratus
Mentha piperita

Carson C, Riley T. 1994. The antimicrobial activity of teatree. Medical Journal of Aus-
tralia. 160:236.
Chaumont J, Bardy I. 1989. The in-vitro antifungal activities of seven essential oils. Fi-
toterapia. 60(3) 263-266.
Cook R, Redondo-Lopez V, Schmitt C, et al. 1992. Clinical, microbiological and bio-
chemical factors in recurrent bacterial vaginosis. Journal of Clinical Microbiology.
30(4) 870-877.
England A. 1994. Aromatherapy for the Mother and Baby. Rochester, VT: Healing Arts
Press.
Evans W. 1994. Trease and Evans’ Pharmacognosy, 13th ed. London: Bailliere Tindall.
Franchomme P, Penoel D. 1991. Aromatherapie Exactement. Limoges, France: Jollois.
Gobel H, Schmidt G, Soyka D. 1994. Effect of peppermint and eucalyptus oil prepara-
tions on neurophysiological and experimental algesimetric headache parameters.
Cephalagia. 14(3) 228-234.
Goldway M, Teff D, Schmidt R, et al. 1995. Multidrug resistance in Candida albicans.
Antimicrobial Agents and Chemotherapy. 39(2) 422-426.
Guba R. 2002. Toxicity Myths. International Society of Professional Aromatherapists.
London: Regents College. (Handout from conference presentation in March of 2002)
Guenther E. 1972. The Essential Oils. Melbourne, FL: Krieger Publishing.
Hajhashemi V, Sadraei H, Ghannadi A, et al. 2000. Antispasmodic and anti-diarrhoeal
effect of Satureja hortensis. Journal of Ethnopharmacology. 71(1-2) 187-192.
Han S, Hur M, Buckle J, et al. 2002. Randomized controlled trial on the effect of aro-
matherapy on menstrual cramps in college students. Unpublished dissertation. Seoul,
Korea: School of Nursing.
Holmes P. 1993. The Energetics of Western Herbs. Berkeley, CA: NatTrop.
Humphrey E. 1930. A new Australian germicide. Medical Journal of Australia.
1:417-418.
Kartnig T, Still F, Reinthaler F. 1991. Antimicrobial activity of the essential oil of young
pine shoots (Picea albies). Journal of Ethnopharmacology. 35(92) 155-157.
Larrondo J, Calvo M. 1991. Effect of essential oils on Candida albicans: a scanning elec-
tron microscope study. Biomedical Letters. 46(184) 269-272.
Lis-Balchin M, Hart S, Roth G. 1997. The spasmolytic activity of the essential oils of
scented Pelargoniums. Phytotherapy Research. 11(8) 583-583.
Lis-Balchin M, Hart S. 1999. Studies on the mode of action of essential oil of lavender,
Lavandula angustifolia. Phytotherapy Research. 13(6) 540-542.
McFerren T (ed.). 1996. Oxford Dictionary of Nursing, 2nd ed. Oxford, UK: Oxford
University Press.
Nathan E. 2000. Aromatherapy for pregnancy induced hypertension. Unpublished dis-
sertation. Hunter, NY: R J Buckle Associates.
Nyirjesy P, Weitz M, Grody M, et al. 1997. Over-the-counter and alternative medicines
in the treatment of chronic vaginal symptoms. Obstetrics & Gynecology. 90:50-53.
Pattnaik S, Subramanyam V, Kole C. 1996. Antibacterial and antifungal activity of es-
sential oils in vitro. Microbios. 86(349) 237-246.
Pena E. 1925. Melaleuca alternifolia oil. Its use for trichomanal vaginitis and other vagi-
nal infections. Proceedings of the Royal Society of Medicine. New South Wales, Aus-
tralia. 60:167-170.
Pena E. 1962. Melaleuca alternifolia oil. Its use for trichomonal vaginitis and other vagi-
nal infections. Obstet Gynecol. 19(6) 793-795.
332 Section II Clinical Use of Aromatherapy

Rawlings R. Healing Gardens. Minocqua, WI: Willow Creek Press, 125.
Reiter M, Brandt W. 1985. Relaxant effect on the trachea and ilea of smooth muscle of
the guinea pig. Arzneimittel-Forschung Drug Research (Aulendorf ). 35:408-414.
Shapiro S, Meier A, Guggenheim B. 1994. The antimicrobial acitivy of essential oils and
essential oil components towards oral bacteria. Oral Microbiology and Immunology.
9:202-208.
Soliman F, El-Kashoury E, Fathy M, et al.1994. Analysis and biological activity of the
essential oil of Rosmarinus officinalis from Egypt. Flavour and Fragrance Journal.
9:29-33.
Stiles J, Sparks M, Ronzio B, et al. 1995. The inhibition of Candida albicans by oregano.
Journal of Applied Nutrition. 47(4) 96-102.
Suresh B, Siram S, Dhanarj S, et al. 1997. Anticandidal activity of Santolina chamaecy-
parisus volatile oil. Journal of Ethnopharmacology. 55:151-159.
Swingle J. 2001. Use of essential oils in intrapartum care. Unpublished dissertation.
Hunter, N.Y.: R J Buckle Associates.
Taddei I, Giachetti E, Taddei P. 1988. Spasmolytic activity of peppermint, sage and rose-
mary essences and their major constituents. Fitoterapia. 59(6) 463-468.
Tiran D. 1996. Aromatherapy in Midwifery Practice. London: Bailliere Tindall.
Viana G, Vale T, Pinho R, et al. 2000. Antinociceptor effect of the essential oil from
Cymbopogon citratus in mice. Journal of Ethnopharmacology. 70(3) 323-327.
Viollon C, Leger D, Caumont J. 1993. The antagonistic properties in vitro of specified
natural volatile compounds with respect to the germs of the vaginal flora. Plantes
Medicinales et Phytotherapie. 16(1) 17-22.
Walsh L, Longstaff J. 1987.The antimicrobial activity of an essential oil on selected oral
pathogens. Periodontology. 8:11-15.
Wren R. 1988. Potter’s New Cyclopaedia of Botanical Drugs and Preparations. London:
Churchill Livingstone.
Chapter 21 Obstetrics and Gynecology 333

334
W
22
Oncology
If one learns from others but does not think, one will be bewildered. If on the other
hand, one thinks but does not learn from others, one will be in peril.
Confucius
Analects, Book II
C
ancer affects approximately one person in three (Stevenson 1996) and is
the general term applied to a series of malignant diseases that may affect
different parts of the body (Dewick 1989). The possible causes of cancer
are many and range from electromagnetic and chemical pollution to genetic pre-
disposition and severe stress. According to the American Cancer Society, approx-
imately 550,000 Americans die each year from cancer (Lam 2001). At least half
of them are thought to suffer symptoms such as pain, nausea, and emotional dis-
tress that conventional medicine either does not or cannot treat (Okie 2001).
Cancer has been around for a million years; traces of it were found in mummies
from the Great Pyramid at Giza (Lewis & Elvin-Lewis 1977). Humans do not
have a monopoly on the disease, as higher-order animals also suffer from cancer.
The three main orthodox treatments for cancer are surgery, radiation, and
chemotherapy agents. These treatments have saved lives but have been hard to
endure. Now, some of those treatments are being questioned. On May 17, 1999,
bone-marrow transplants received controversial press following an announcement
at the annual meeting of the American Society of Clinical Oncology in Georgia
that a multinational research program found “no evidence that bone marrow
transplants were any more beneficial than chemotherapy in breast cancer” (Porter
1999). Five hundred twenty-five women in Scandinavia, 154 in South Africa, 553
in Philadelphia PA, and 61 in France took part in the randomized studies. The

researchers found that survival after bone-marrow transplants was 40%, not much
higher than a placebo.
Cancer-drug research has also had its share of bad publicity. Barlow (2001)
of the British Financial Times, wrote “clinical research into cancer drugs was
found to be eight times more likely to reach a positive conclusion when funded
by a drug company than when publicly funded.”
Aromatherapy and Cancer Treatment
Many plants and plant materials have been used to treat malignant diseases for
centuries. It is fascinating how the same plants keep being cited all over the world
for the treatment of cancer. For example, Dr. Fell completed a study of 25 cases
of breast cancer using the herb bloodwort at the Middlesex Hospital in London
in 1857. He chose bloodwort (Sanguinaria canadensis) because he learned it had
been used by American Indians for hundreds of years. Fell found all his cases
went into remission (Fell 1857). It is difficult to establish whether this really hap-
pened, although Sanguinaria also has a long history of use in Russia for the treat-
ment of cancer (Lewis & Elvin-Lewis 1977).
Madagascan periwinkle (Catharanthus roseus) contains the alkaloids vinblas-
tine and vincristine, which have been useful in treating cancer (Dewick 1989).
More recently, Centella asiatica, sometimes called gotu kola or South African Pen-
nywort, was featured in an in-vitro study of cultured cancer cells. Centella appeared
to destroy 100% of the cultured cancer cells. When the study was conducted on
mice, Centella doubled the life span of mice with tumors. Centella has virtually no
toxic effect on normal human lymphocytes (Foster 1995). Centella asiatica can also
be obtained as an infused oil (phytol). Phytols are often used in aromatherapy and
are supplied by many essential-oil distributors.
Some essential oils, or components found within essential oils, have been
found to have antitumoral activity. Sclareol, a diterpenol in Salvia sclarea (clary
sage), was found to kill cell-lines of human leukemia and had an inhibitory con-
centration of lower than 20 (g/ml) (Dimas et al 1999). Delora et al (1994) found
myrrh had an anticarcinogenic effect on tumors induced in mice. Bergamottin, a
furanocoumarin found in bergamot (5%) and lemon (0.2%) was one of several
coumarins found to inhibit in-vitro tumor promoters (Miyake et al 1999).
Limonene is metabolized into perillyl alcohol by the body. Perillyl alcohol, a
monoterpenol also found in lavandin, peppermint, and spearmint, inhibited more
than 80% of all chemically induced breast cancers in animal studies (Haag &
Gould 1992) and was also found to regress pancreatic, mammary, and liver tu-
mors (Belanger 1998). Perillyl alcohol was found to have chemopreventative ac-
tivity against colon, skin, and lung cancer and to revert tumor cells to a differen-
tiated state. However, preliminary human trials have not demonstrated tumor
regression as of yet, but this could be because only part of an essential oil has been
used in isolation. It would be interesting to run the study using the complete es-
sential oil.
Chapter 22 Oncology 335

Treating Conventional Side Effects
The side effects of some conventional treatments for cancer can be very hard to
endure. Several of my friends are cancer survivors. I also had a small aromather-
apy private practice in England. My patients came by doctor’s referral or word of
mouth. Almost half of them had cancer, and the role of aromatherapy in their
treatment was one of support. The cancer patients were mainly undergoing
chemotherapy and radiation therapy following surgery and, without exception,
they found the going very tough. Many expressed their despair that conventional
medicine did not adequately address the unpleasant side effects of the cancer
treatment.
Several years ago, there was some controversy about the use of massage on
cancer patients, with the suggestion that massage could actually spread the dis-
ease (Goodman 1995). However, a study and rigorous review of the published lit-
erature indicates massage should not be contraindicated (McNamara 1994).
Bernie Siegel, MD, also states massage therapy is not contraindicated in a cancer
patient (Siegel 1996). Deep massage is rarely requested by an oncology patient.
What oncology patients usually prefer is a very light touch, more like stroking.
The “m”’ technique can be really valuable, particularly as it is so quick to learn and
to do and could be taught to family members and friends who are eager to help
but don’t know how.
Conrad (2000) investigated the effects of aromatherapy on a cancer support
group to see if diffused essential oils could decrease anxiety and encourage commu-
nication. Ten to 12 cancer patients met weekly. The preponderance was women, but
there were some men in the support group. Some individuals were receiving
chemotherapy or radiation therapy and some were 3- to 10-year survivors. Three es-
sential oils were chosen for their ability to calm and soothe. The study took six weeks.
During weeks one and two no essential oils were diffused, although the diffuser was
placed in the room and switched on. During weeks three and four, two drops of a
mixture of six drops lavender and four drops mandarin were diffused. During weeks
five and six, six drops of lavender and four drops of frankincense were diffused. The
diffuser was an AromaStream electric fan. Questionnaires were given to each of the
support group members with five simple questions. The questions ranged from
whether they could smell anything to whether they found communication more or
less difficult. A Likert scale was used to tally the responses. The facilitator did not
know when the essential oils were being diffused or which ones were being used.
However the facilitator noticed major changes in the group when the essential oils
were diffused. During the lavender/mandarin week, there was more laughter and
sharing. The sessions seemed more fluid and effortless. During the lavender/frank-
incense week, the group seemed more emotional and labile. There were more tears
than usual, and the group was challenging to facilitate. The participants recorded
they felt more relaxed when talking about difficult subjects during the aromatherapy
weeks, particularly when the lavender/mandarin mixture was diffused.
336 Section II Clinical Use of Aromatherapy

Gravett (2001) reported on the effects of topically applied essential oils to an
infected Hickman arterial line. He used tea tree, Eucalyptus globulus, and lavender
(Lavandula angustifolia) in a 10% cream applied to the site twice a day. The con-
trol group received Povidone iodine spray, which is the standard treatment for an
infected line. Gravett notes that chemical antiseptic sprays can lead to cutaneous
sensitivity as well as to direct chemical damage and resistant organisms. Gravett
found that economically the essential-oil treatment was preferable and appeared
to work as well as the Povidone spray.
Researchers at Memorial Sloane Kettering Cancer Center in New York
used aromatherapy to reduce anxiety attacks of patients undergoing magnetic
resonance imaging. They diffused heliotropin and found it relieved anxiety
(Castleman 1996). Heliotropin is a close relative to vanilla. A pilot survey con-
ducted in 1995 showed a wide variety of cancer patients sought complementary
care therapy (Clover et al 1995). In a study involving two London hospitals, 16%
of patients who had received complementary therapies said they had wanted
them to gain emotional support and hope (Downer et al 1994). Perhaps aro-
matherapy can help during the “dark times,” and enhance the quality of care as
well as quality of life.
Nausea, constipation, depression, exhaustion, shooting pains, “feeling my
bones might break,” lymphedema, postradiation burns, hair loss, and insomnia are
possibly the most common side effects of radiation therapy and chemotherapy. Of
these symptoms, nausea, postradiation burns, hair loss, and lymphedema have
been selected for discussion in this chpater. As Dobbs, a British nurse, wrote
“complementary therapies may enrich our interventions and bring comfort and
better health to patients with cancer” (Dobbs 1985).
Nausea
The cytotoxic drugs used in chemotherapy for cancer have two well-known
side effects: nausea and immune supression (Bovbjerg et al 1990). One-third of
patients with cancer experience nausea and vomiting (Finlay 1995). Nausea is
common during radiation or chemotherapy treatment, and 24%-75% of patients
develop anticipatory nausea and vomiting during the course of repeated
chemotherapy (Bovbjerg et al 1990). Patients frequently report that everything
tastes different. They also say they are very sensitive to odors, often smelling
something they had not noticed before or feeling great distaste for a smell that
had not bothered them previously. While conventional medicine can be used in
the form of antiemetics, there are also essential oils that can reduce nausea. See
Table 22-1 for suggestions.
Just a few drops of one of the oils in Table 22-1 on a tissue can bring relief.
Sipping hot water with a sliver of ginger root can also frequently bring relief from
nausea and is a well-known remedy for morning sickness during pregnancy. A
more in-depth review of essential oils for nausea can be found in Chapter 11 on
nausea.
Chapter 22 Oncology 337

Patients receiving bone-marrow transplants frequently have to endure the
smell of dimethyl sulfoxide (DMSO). DMSO causes differentiation of malignant
bone-marrow cells (Toren & Rechavi 1993) and can help deliver anticancer sub-
stances to the site of the cancer (Wilner 1994). It also seems to enhance the ef-
fects of various cytotoxic agents while simultaneously reducing the toxicity of
conventional medication (Pommier et al 1988). Citrus essential oils such as lemon
and grapefruit are being used successfully to hide this aroma at Columbia Pres-
byterian Medical center in New York, according to my students. The essence of
oranges is a traditional treatment in Sicily for sea sickness.
Postradiation burns
Although most radiologists request nothing be put on the skin during
radiation, this is mainly to ensure the marks for radiation will not be removed
(Sheppard-Hanger 2000). It is extremely important that nothing should disturb
the marks. Maiche et al (1990) conducted their study (see following description)
throughout irradiation by applying a cream to the area before and after each ra-
diation treatment.
Before the area is marked, the skin can be prepared with undiluted naiouli
(Melaleuca viridiflora). This seems to toughen the skin and results in fewer and less
severe burns. Apply naiouli to the area three times a day for a week. Roulier (1990)
and Penoel and Franchomme (1990) both suggest using 50% naiouli immediately
before each radiation session and 50% in a St. John’s wort-infused oil or rosehip car-
rier oil after each session. Sheppard-Hanger (2000) also used spritzers of everlasting
(Helichrysum italicum) and blue tansy (Tanacetum annum) immediately following
each radiation treatment. Blue tansy is dark blue in color and high in chamazulene,
an antiinflammatory. Do not mistakenly use Tanacetum vulgare, another species of
Tanacetum. Tanacetum vulgare is yellow to pale blue and contains 60% thujone, a ke-
tone, and is not recommended for use in oncology or aromatherapy in general.
My patients have used tansy and everlasting in spritzers and also spritzers of
lavender and rose with good results. Yarrow and blue chamomile are also good
choices. Table 22-2 lists essential oils that can be used in post-radiation spritzers.
338 Section II Clinical Use of Aromatherapy
Table 22-1 h Essential Oils for Nausea
Common Name Botanical Name Reference
Peppermint
Ginger
Cardamom
Patchouli
Spearmint
Briggs 1993, Williams 1998,
Williamson & Evans 1988
Mowry 1982
Nadkarani 1992, Cabo &
Crespo 1986
Yang et al 1999
Buckle 1997
Mentha piperita
Zingiber officinale
Elettoria cardamomum
Pogostemon cablin
Mentha spicata

To make a spritzer, add 4 ml of essential oils to 4 oz of water and put in a spray
bottle. Shake well before using. Anything to be used topically that has been stored
in an aluminum container or contains aluminum (such as antiperspirants) cannot
be used during radiation therapy as aluminum can interfere with the treatment.
When radiation therapy is finished, apply a compress. Mix antiinflammatory
essential oils like German chamomile, frankincense, or rose into a base of either
aloe vera gel or tamanu (Calophyllum inophyllum). An infused oil of gotu kola
(Centella asiatica) or comfrey (Symphytum officinale) can also bring rapid relief and
help promote healing.
Maiche et al (1990) carried out a controlled, single-blind study on 50 women
ages 30-79 who had been operated on for breast cancer and who had received
radiation therapy. Kamillosan Ointment, a proprietary cream containing chamo-
mile that is widely available in Europe, was applied 30 minutes before radiation
and just before bed. Measurements were made by a physician using a four-point
scale (no change through moist desquamation). A comparison between the con-
trol group and the Kamillosan group showed no statistical significant changes
overall, but skin deterioration appeared to happen later in the Kamillosan group,
and there were fewer patients who presented with Grade 2 (dark erythema) reac-
tions. In a further controlled study on leg ulcers, Kamillosan appeared to enhance
standard treatment of corticosteroids and antihistamines (Nasemann 1975).
Hair loss
In a randomized, double-blind, controlled study, hair loss due to alopecia re-
sponded well to topically applied essential oils (Hay et al 1998). Eighty-six pa-
tients took part in the study. The active group massaged thyme, rosemary, laven-
der, and cedarwood in a mixture of jojoba and grapeseed oil into their scalps daily.
The control group massaged their scalps with vegetable oils only. Measurement
Chapter 22 Oncology 339
Table 22-2 h Spritzers for Postradiation Burns
Common Name Botanical Name Reference
Lavender
German chamomile
Roman chamomile
Rose
Everlasting
Blue tansy
Yarrow
Tisserand 1993
Maiche et al 1990,
Williamson & Evans 1988
Maiche et al 1990,
Grieve 1931
Brud & Szydlowska 1991
Sheppard-Hanger 2000
Sheppard-Hanger 2000
Sheppard-Hanger 2000
Lavandula angustifolia
Matricaria recutita
Chamaemelum nobile
Rosa damascena
Helichrysum italicum
Tanacetum annum
Achillea millefolium

was taken three ways: through a standardized, professional photograph taken ini-
tially, and then again after 3 and 7 months. Measurement was on a four-point
scale and with a map of the alopecia traced onto transparent film. This was con-
verted into a computerized image so exact calculations could be made. Nineteen
(44%) of the 43 patients in the active group showed improvement compared with
six (15%) of the control group (p 0.008).
When chemotherapy stops, usually the patient’s hair begins to grow again,
often more luxuriantly.
Lymphedema
Lymphedema occurs frequently following mastectomy but is also fairly com-
mon following lumpectomy if there has been removal of lymph glands. It stands
to reason that the lymph system will have more difficulty returning excess inter-
stitial fluid to the blood if there has been a reduction in the number of lymph
pathways. The large, lymphatic vessel walls are contractile (so progress is in one
direction only), and when one or more of the lymph glands has been removed via
surgery or damage, lymph accumulates in the subcutaneous tissue causing the af-
fected limb to become swollen and tender (Badger 1995).
Lymph contains large protein molecules, and build-up of protein in the tis-
sue leads to chronic inflammation and, over a period of time, thickened, leathery
looking skin. After the initial phase of soft skin and pitting, chronic lymphedema
is characteristically nonpitting. Because of chronic inflammation, local immunity
is compromised, with subsequent bouts of cellulitis and poor resistance to insect
bites or minor cuts.
Lymphatic drainage should be carried out regularly, as there is no pumping
action by the lymph system itself. Normal lymphatic drainage relies on muscular
activity during exercise to move the lymph in the right direction. When this no
longer happens, the lymph needs a little extra help. However, because the prob-
lem occurs at a subcutaneous level, the pressure needed is extremely light and only
in the direction of the lymph. This is one instance where normal massage is con-
traindicated. The pressure of an ordinary massage can cause spasm in the lymph
vessels, temporarily suspending the lymphatic flow (Idoux 1996), and most mas-
sage strokes are not suitable.
Lymphatic drainage is a completely different technique and needs to be
learned. Perhaps the most famous and accepted method is the Vodder method,
which was developed in Austria 50 years ago. Rather than a massage stroke,
which tends to be a two- directional movement with both hands working in op-
posite directions, lymphatic drainage works in one direction only: the direction of
flow of the lymph, which is toward the main lymph ducts, away from the periph-
eries, and toward the thoracic duct. Regular sessions, daily if possible, can reduce
the size of a lymph-enlarged limb quite dramatically. The limb will feel lighter
and the skin more supple. The elbow (or other joint) will become more clearly
defined, and there will be more tactile sensation. I have had success using
“tramlines,” running my fingers gently, slowly, and repeatedly in the direction of
the lymph. With a bit of practice it was possible to feel the lymph move.
340 Section II Clinical Use of Aromatherapy

Aromatherapy can play an important role when the skin loses its elasticity
and infections become more frequent. However, it is unlikely that essential oils
could help the lymph to move. Table 22-3 lists carrier and infused oils used in the
treatment of lymphedema.
Essential oils can be useful to protect the engorged limb from bacterial or
fungal infection (Table 22-4). Choose an essential oil the patient likes, and avoid
those with an astringent action like Cupressus sempervirens (cypress).
Kirshbaum (1996) carried out a small study with eight patients with lym-
phedema using diluted lavender in a massage. She found aromatherapy massage
reduced pain and swelling and improved movement, a finding that seems to con-
tradict the conclusion of Idoux (1996). Casley-Smith (1999) found topically ap-
plied coumarins reduced edema, but not as effectively as when taken orally.
Benefits of Aromatherapy for Cancer Patients
Aromatherapy is often used to enhance the quality of life of cancer patients. In a
study at the Marie Curie Center in Liverpool, England, patients received a massage
with or without Roman chamomile. The group that received the aromatherapy mas-
sage was found to have statistically significant improved quality of life and reduced
anxiety (Wilkinson 1995). In another study conducted to assess the acceptability of
using aromatherapy in palliative care, doctors, nurses, paramedics, and volunteers
were reported to be extremely enthusiastic about the concept (Arnold 1995).
Corner et al (1995) used a premade mixture of lavender, rosewood, lemon, rose,
and valerian in their randomized controlled study of 52 patients with a variety of
cancers. Just over half of the patients received chemotherapy, radiation, or surgery
during the 8-week study. Patients were randomly assigned to a group to receive a
weekly massage with or without essential oils. A matching control group was se-
lected from patients who were unable to attend the 8-week course of massage. The
Chapter 22 Oncology 341
Table 22-4
h Skin-Friendly Essential Oils with Antibacterial
or Antifungal Actions
Common Name Botanical Name Reference
Lavender Lavandula angustifolia Valnet 1991
Frankincense Boswellia carterii Duwiejua et al 1993
Sweet marjoram Origanum majorana Ross et al 1980
Table 22-3 h Carrier and Infused Oils for Treating Lymphedema
Common Name Botanical Name Reference
Gotu kola
Oil of evening primrose
Passionflower
Price et al 1999
Earle 1991
Earle 1991
Centella asiatica
Oenothera biennis
Passiflora incarnata

results showed a statistical difference in anxiety between the two groups receiving
massage, but pain and mobility showed almost equal improvement.
Evans (1995) conducted an audit into aromatherapy massage in cancer pa-
tients in a palliative-care setting. The study lasted 6 months and involved 69 pa-
tients. Participants were offered an aromatherapy session with an aromatherapy
massage and therapist advice on symptom control using aromatherapy. Eighty
percent of the patients felt they benefited, although it is difficult to assess whether
this was due to the essential oils, massage, or the one-on-one care. Everson (2002)
found that while her white-blood-cell (WBC) count fell with each chemother-
apy treatment, the WBC rebounded faster when she added bergamot to her daily
regimen. Table 22-5 lists isolates believed to have anticarcinogenic properties.
Essential Oils to Avoid in Oncology
Recent studies have indicated that phytoestrogens, once thought to be con-
traindicated in cancer, may actually reduce the risk of cancer and could therefore
be beneficial. However, as the jury is still out and until more definite information
emerges, it might be prudent to avoid essential oils with estrogen-like properties
in tumors that are estrogen dependent. Estrogen-dependent cancers are breast,
uterine, and ovarian. It is extremely unlikely that the tiny amounts of estrogen-
like compounds used in aromatherapy would impact cancerous growth. As early
as 1938, Zondeck and Bergmann wrote about the estrogenic properties of phenol
methyl ethers. Essential oils thought to have an estrogen-like effect include fen-
nel and aniseed as they contain anethole (Albert-Puleo 1980). Anethole is a phe-
342 Section II Clinical Use of Aromatherapy
Table 22-5 h Isolates Thought to Have Anticarcinogenic Properties
Isolate Source Botanical Name Reference
Sclareol Clary sage Salvia sclarea Dimas et al 1999
Bergamottin Bergamot Citrus bergamia Miyake et al 1999
Perillyl alcohol Peppermint Mentha piperita Belanger 1998
Spearmint Mentha spicata
Lavandin Lavandula intermedia
D-limonene, Lemongrass Cymbopogon citratus Zheng et al 1993
geraniol
Carvone, Dill Anethum graveolens Zheng et al 1991
anethufuran,
limonene
Carvone, Caraway Carum carvi Zheng et al 1991
anethufuran,
limonene

nol methyl ether. Scareol (found in clary sage) and viridifloral (found in niaouli)
are other components of essential oils that have structures similar to estrogen
(Franchomme & Penoel 1991). Therapists using aniseed and fennel on a daily ba-
sis found that their periods came earlier than usual. The link to geranium and rose
is really too tenuous, and both essential oils should be fine to use in estrogen-
dependent tumors.
In-vitro studies on rat skin indicated that some essential oils enhance the
penetration of 5-fluorouracil (5FU) (Abdullah et al 1996). Peppermint increased
penetration by 46 times, and Eucalyptus globulus increased penetration by 60
times. It might be advisable to avoid using these two essential oils topically near
the intravenous site during chemotherapy with 5FU.
Conclusion
In summary, aromatherapy is a way to “enrich interventions and bring comfort
and better health to patients with cancer” (Penson & Fisher 1995). Such actions
demonstrate caring. Perhaps this is the caring referred to by the nursing theorist
Orem as “a moral idea of nursing” (Leddy & Pepper 1993). However, caring is a
moral issue for all health-care professionals.
REFERENCES
Abdullah D, Ping Q, Liu G. 1996. Enhancing the effect of essential oils on the penetra-
tion of 5-fluorouracil through rat skin. Yao Xue Xue Bao. 31(3) 214-221.
Albert-Puleo M. 1980. Fennel and anise as estrogenic agents. Journal of Ethnopharma-
cology. 2(4) 337-344.
Arnold L. 1995. The use of aromatherapy and essential oils in palliative care: risk versus
research. Positive Health. 32-34.
Badger C. 1995. Lymphoedema. In Penson J, Fisher R (eds.), Palliative Care for People
with Cancer. London: Edward Arnold, 81-90.
Barlow T. 2001. When the devil invites you to dine. Financial Times. May 26/27, 11.
Belanger J. 1998. Perillyl alcohol: applications in oncology. Alternative Medicine Review.
3(96) 448-457.
Bovbjerg D, Redd W, Maier L, et al. 1990. Anticipatory immune suppression and nau-
sea in women receiving cyclic chemotherapy for ovarian cancer. Journal of Consulting
and Clinical Psychology. 58(2) 153-157.
Briggs C. 1993. Peppermint: medicinal herb and flavouring agent. Canadian Pharmaceu-
tical Journal. 126:89-92.
Cabo J, Crespo M. 1986. The spasmolytic activity of various aromatic plants from
Granada: the activity of the major components of their essential oils. Plantes Medici-
nales et Phytotherapie. 20(3) 213-218.
Casley-Smith J.1999. Benzo-pyrones in the treatment of lymphedema. International
Journal of Angiology. 18(1) 31-41.
Castleman M. 1996. Aromatherapy: Nature’s Cures. Emmaus, PA: Rodale Press, 39.
Clover A, Last P, Fisher P. 1995. Complementary cancer therapy: a pilot study of patients,
therapies and quality of life. Complementary Therapies in Medicine. 3(3) 129-133.
Chapter 22 Oncology 343

Conrad P. 2000. Aromatherapy and the cancer support group. Unpublished dissertation.
Hunter, N.Y.: R J Buckle Associates.
Corner J, Cawley N, Hildebrand S. 1995. An evaluation of the use of massage and es-
sential oils on the well being of cancer patients. International Journal of Palliative
Nursing. 1(2) 67-73.
Delora P, Luceri C, Gherlandini C, et al. 1994. Anticarcinogenic effect of Commophora
momol on solid tumors induced by Ehrlich carcinoma cells in mice. Chemotherapy.
40:337-347.
Dewick P. 1989. Tumour inhibitors from plants. In Evans W (ed.), Trease and Evan’s
Pharmacognosy, 13th ed. London: Bailliere Tindall, 634-656.
Dimas K, Kokkinopoulos D, Demetzos C, et al. 1999. The effect of sclareol on growth
and cell cycle progression of human leukemic cell lines. Leukemia Research. 23(3)
217-234.
Dobbs B. 1985. Alternative health approaches. Nursing Mirror. 160:41-42.
Downer S, Cody M, McCluskey P. 1994. Pursuit and practice of complementary thera-
pies by cancer patients receiving conventional treatment. British Medical Journal.
309(6947) 86-89.
Duwiejua M, Zeitlin I, Waterman P, et al. 1993. Anti-inflammatory activity of resins
from some species of the plant family Burseraceae. Planta Medica. 59(5) 12-16.
Earle L. 1991. Vital Oils. London: Vermilion.
Evans B. 1995. An audit into the effects of aromatherapy massage and the cancer patient
in palliative and terminal cancer. Complementary Therapies in Medicine. 3(4) 239-241.
Everson C. 2002. Personal communication.
Fell J. 1857. A Treatise on Cancer and Its Treatment. London: J & A Churchill.
Finlay I. 1995. The management of other frequently encountered symptoms. In Penson
J, Fisher R (eds.), Palliative Care for People with Cancer. London: Edward Arnold,
57-80.
Foster S. 1995. Anti-cancer effects of Gotu Kola (Centella asiatica). HerbalGram.
36:17-18.
Franchomme P, Penoel D. 1990. Aromatherapie Exactement. Limoges, France: Jollois.
Gattefosse R. 1937. (Translated in 1993 by R. Tisserand.) Aromatherapie: Les Huile
Essentielles-Hormones Vegetales (Gattefosse’s Aromatherapy.) Saffron Walden, UK:
CW Daniels, 89.
Goodman S (ed.). 1995. Book review: Massage for People with Cancer. Positive Health. 26.
Gravett P. 2001. Aromatherapy treatment for patients with Hickman line infection fol-
lowing high-dose chemotherapy. Int J of Aromatherapy. 11(1) 18-20.
Grieve M. 1931. A Modern Herbal. Harmondsworth, UK: Penguin Books.
Haag J, Gould M. 1992. Mammary carcinoma regression induced by perillyl alcohol, an
hydroxylated analog of d-lmonene. Cancer Chemother Pharmacog. 34(6) 477-483.
Hay I, Jamieson M, Ormerod D. 1998. Randomized trial of aromatherapy: successful
treatment for alopecia areata. Archives of Dermatology. 134(11) 1349-1352.
Idoux M. 1996. Treatment for lymphoedema following mastectomy or lumpectomy.
Holistic Nurses’ Association Newsletter. 3:4-5.
Kirshbaum M. 1996.Using massage in the relief of lymphedema. Professional Nurse.
11(4) 230-232.
Lam M. 2001. Annual cancer deaths in USA. Retrieved March 17, 2003 from
www.LamMD.com.
Leddy S, Pepper J. 1993. Conceptual Bases of Professional Nursing. Philadelphia:
Lippincott.
344 Section II Clinical Use of Aromatherapy

Lewis W, Elvin-Lewis M. 1977. Medical Botany. New York: Wiley Interscience.
Maiche A, Grohn P, Maki-Hokkonen H. 1990. Effect of chamomile cream and almond
ointment on acute radiation skin reaction. Acta Oncologica. 30(3) 395-396.
McNamara P. 1994. Massage for People with Cancer. London: Wandsworth Cancer
Support Centre.
Miyake Y, Murakami A, Sugiyama Y, et al. 1999. Identification of coumarins from lemon
fruit (Citrus limon) as inhibitors of in vitro tumor promotion and superoxide and nitric
oxide generation. Journal of Agricultural and Food Chemistry. 47(8) 3151-3157.
Mowrey D. 1982. Motion sickness, ginger and psychophysics. Lancet. 1(8273) 655-657.
Nadkarni K. 1992. Indian Material Medica, Vol. 1. Prakashan, India: Bombay Popular.
Nasemann T. 1975. Kamillosan therapy in dermatology. Z Allgemeinmed. 25:1105-1106.
Okie S. 2001. Report faults priorities of cancer care in the US. Albany, N.Y.: Times
Union, A5.
Penson J, Fisher R. 1995. Palliative Care for People with Cancer. London: Edward
Arnold.
Pommier RF, Woltering EA, Milo G, 1988. Cytotoxicity of DMSO and antineoplastic
combinations against human tumors. American Journal of Surgery. 155(5) 672-675.
Porter C. 1999. Business thrives on unproven care, leaving science behind. New York
Times. CXLIX A1.
Price L, Smith I, Price S. 1999. Carrier Oils. Stratford-upon-Avon, UK: Riverhead.
Ross S, El-Keltaw N, Megella S. 1980. Antimicrobial activity of some Egyptian aromatic
plants. Fitoterapia. 51:201-205.
Roulier G. 1990. Les Huiles Essentielles Pour Votre Sante. St. Jean-de-Braye, France:
Dangles.
Siegal B. 1996. Letter to the editor. Massage Therapy Journal. 35:12-13.
Sheppard-Hanger S. 2000. Use of essential oils and natural extracts to help counter side
effects of radiation during cancer treatment. Proceedings of the 3rd Scientific Wholis-
tic Aromatherapy Conference. San Francisco. Nov 10-12, 174-191.
Stevenson C. 1996. Disease. In Vickers A (ed.), Massage and Aromatherapy. London:
Chapman & Hall, 193-202.
Toren A, Rechavi G. 1993. What really cures in autologous bone marrow transplanta-
tion? A possible role for dimethylsulfide. Medical Hypotheses. 41(6) 495-498.
Weil A. 1998. Complementary Care for Cancer. Dr. Andrew Weil’s Self- Healing. 1, 6.
Wilkinson S, Aldridge J, Salmon I. 1999. An evaluation of Aromatherapy massage in
palliative care. Journal of Palliative Medicine. 13(5) 409-417.
Williamson E, Evans F (eds.). 1988. Potter’s New Cyclopedia of Botanical Drugs and
Preparations. Saffron Walden, UK: CW Daniels.
Wilner J. 1994. DMSO. The Cancer Solution. Boca Raton, FL: Peltec Publishing.
Yang Y, Kinoshita K, Koyama K, et al. 1999. Anti-emetic principles of Pogostemon cablin.
Phytomedicine. 6(2) 89-93.
Zheng G, Kenney P, Lam K. 1991. Anethofurna, carvone and limonene: Potential cancer
chemopreventive agents from dill weed oil and caraway oil. Planta Medica. 58(4)
338-341.
Zheng G, Kenney P, Lam K. 1993. Potential anticarcinogenic natural products isolated
from lemongrass oils and galanga root oil. Journal of Agricultural and Food Chem-
istry. 41(2) 153-157.
Zondeck B, Bergmann E. 1938. Phenol methyl ethers as estrogenic agents. Biochemical
Journal. 32:641-645.
Chapter 22 Oncology 345

346
W
23
Pediatrics
And when you crush an apple with your teeth, say to it in your heart:
“Your seeds shall live in my body.
And the buds of your tomorrow shall blossom in my heart.
And your fragrance shall be my breath,
And together, we shall rejoice through all the seasons.”
Kahil Gibran
The Prophet
T
here is a Chinese saying that “Children get sick easily, and sickness can
quickly become serious,” and another saying that “Children easily ill, eas-
ily cured.” There is no doubt that children in the hospital are very vulner-
able. They do indeed deteriorate or improve rapidly, and they need a tremendous
amount of love and support, particularly if their families cannot visit. Although
children are more adaptable than adults and often face very intimidating proce-
dures with wide-eyed interest and no apparent fear, many do display behavioral
problems just because they have become institutionalized.
Some of the most distressing aspects of hospitalization are the invasive med-
ical procedures, like venipuncture and the placing of nasogastric tubes. Aro-
matherapy can help soothe the child prior to these interventions. A few moments
of hand or face “m” technique can help relax children while you explain what is
going to happen, how long it will last, and how it will help them. Anxiety about
being hurt has been identified as one of a child’s greatest fears (Kurfit Stephens
et al 1999). Sweet orange oil was found to be helpful in the induction of 120 un-
premedicated children aged 5-14 years in a study by Mehta et al (1998). Children
in the essential oil group were significantly more likely to say they would like to
have a similar anaesthetic technique again in the future (p⬍0.05). As nausea is

frequently a symptom of fear in children, lavender might be another useful es-
sential oil to use. Lavender straw (the discarded by-product of stream distillation)
still retains some aroma and was found to alleviate stress and travel sickness in 40
pigs being transported by road (Bradshaw et al 1998).
Aromatherapy is a natural thing to a child, whose early life revolves around
smell and touch. Babies identify their mothers through the mother’s smell
(Russell 1976). This is easy to understand when one realizes that babies are born
with structurally mature olfactory systems (Humphrey 1940). Young children up
to the age of 5 years are not repelled by smells that most adults dislike, such as fe-
ces. However, by the age of seven, many children are beginning to establish sim-
ilar “tastes” in smells to adults (Engen 1974). Children also display the facility of
“learned memory” early on, gravitating toward the smell of a perfume worn by
their mother, rather than another unknown perfume (Schleidt & Genzel 1990).
Therefore, familiar smells are more acceptable to children than other smells. This
is particularly important in the case of children from other cultures, who may re-
spond to exotic aromas with which Western children might not identify, such as
spices. Children can be extremely sensitive to smell. Schilcher (1997), head of the
Institute of Pharmaceutical Biology at Berlin’s Independent University, suggests
inhalation of volatile oils is an excellent method of choice for pediatrics.
Most of us find it an instinctive action to cuddle and stroke a child. Aro-
matherapy takes that instinct a little further and adds some extra therapeutic
value. Parents and relatives can be taught very easily how to use the “m” technique
on a sick child, and they relish the feeling of being empowered to do something
in a situation most parents fear. This experience of empowerment can be made
more potent by the addition of an aroma with which both mother or father and
child are familiar and which they both like. Gentle aromas can soothe a child, but
the emphasis is on gentleness. It is necessary to use only half the normal number
of drops of an essential oil required for an adult. Please see Table 23-1 for dosage
recommendations for children.
Bear in mind that some children may have been subjected to abuse and will
not be receptive to touch, finding it more threatening than comforting. If this is
Chapter 23 Pediatrics 347
Table 23-1 h Doses for Children and Babies
Premies Floral waters only N/A
Newborn-6 months 1 drop in 20 ml 0.25%
6 months-2 years 1 drop in 10 ml 0.5%
2-5 years 1 drop in 5 ml 1%
5-10 years 1-2 drops in 5 ml 1-2%
More than 10 years 1-5 drops in 5 ml 1-5%
*unless treating specific infections, for example onychomycosis (toenail fungus) or hair lice.

the case, merely using the appropriate aroma can still be beneficial. Children quite
like to be involved in choosing an aroma, especially if the choice is small. More
than four essential oils will demand too much effort from a sick child. Sometimes
a choice of just two will make aromatherapy acceptable, whereas if only one smell
is offered it might be refused. However, it is important never to insist; children
are patients with patients’ rights, no matter how old they are.
Of the possible problems that might be helped by aromatherapy, hyperactiv-
ity, attention deficit hyperactivity disorder (ADHD), and head lice have been
chosen for discussion in this chapter. Clinical aromatherapy has an important role
in pediatrics alongside orthodox medicine. Aromatherapy can also bring comfort
to both child and parent and give a sense of empowerment to staff. Caring for sick
children is an emotionally draining experience, and caring for a dying child is one
of the most daunting tasks faced by any health professional (Hodson 1985).
Hyperactivity
Hyperactivity in children who have become hospitalized is common. This form
of excitable behavior is different from attention deficit/hyperactivity disorder
(ADHD), which is a recognized mental disorder and will be covered in a later
section (McFerran 1996).
Every child will have a unique response to being hospitalized. Some children
become withdrawn, some become placatory, and others become hyperactive. It is
the hyperactive children who can become a source of irritation to staff and other
children. Aromatherapy can often help. The cause underlying the behavior may be
the strange environment and smells, which make the child feel threatened. Hy-
peractivity may be a means of asking for more attention or a means of communi-
cating a child’s sense of ill ease. The “m” technique with a familiar smell (Table 23-
2) may soothe a child and reduce hyperactivity. Sometimes mixing aromas to
produce a new but faintly familiar aroma can be beneficial (Worwood 2000).
348 Section II Clinical Use of Aromatherapy
Table 23-2 h Essential Oils to Relax a Hyperactive Child in the Hospital
Common Name
Roman chamomile
Mandarin
Lavender
Neroli
Rose
Geranium
Sweet marjoram
Botanical Name
Chamaemelum nobile
Citrus reticulata
Lavandula angustifolia
Citrus aurantium flos
Rosa damascena
Pelargonium graveolens
Origanum majorana

A foot or hand “m” technique is usually acceptable to a sick child. Teaching
parents to help their sick children is one of the most rewarding things I have ever
done. A mother’s touch, no matter how unfamiliar she is with any technique or
stroke, is what a child will usually recognize and respond to. Gentleness and slow
strokes are what matters. This is particularly important to remember if the child
is unconscious. If the mother wears a lot of bracelets, do not ask her to remove
them, as her child will remember how they sounded and how they felt.
Sometimes the smallest amount of a compound in an essential oil can have a
profound effect. One example is the smell of rose caused by an oxide present at a
concentration of only 0.1 parts per million. Another example is a compound
called indole present at trace levels in citrus oils, honeysuckle, and jasmine (Collin
& Hoeke 1993). In large amounts, indole smells vile and would make most peo-
ple gag because it contributes to the smell of rotting meat! However, indole has a
remarkable relationship with tryptophan and appears to aid its synthesis (Clark
1995). Tryptophan is found in various foodstuffs like chicken, milk, bananas, and
rice and is the chemical precursor of serotonin, the “feel-good” neurochemical
(Parish 1991). Using an essential oil containing a trace of indole may help a child
relax.
Attention Deficit/Hyperactivity Disorder
ADHD is a combination of inattention, hyperactivity, and impulsive behavior
that is classified as a disorder when these behaviors are severe. ADHD is thought
to be a developmental failure in the brain circuitry that underlies inhibition and
self control (Tucker 1999). During the last 10 years, an increasing number of chil-
dren have been diagnosed with ADHD. It is the most commonly diagnosed be-
havioral disorder in children and the fastest growing disorder in adults. Since
1990, the number of children in the United States diagnosed with ADHD has
increased from 900,000 to more than 5.5 million. ADHD is thought to affect 5-
10% of all school-aged children. One and a half million adults also have been di-
agnosed with ADHD.
Charles Bradley first noticed that amphetamine (Benzedrine) calmed hyper-
active children in 1937 (Gainetdinov & Caron 2001). Numerous studies carried
out since that time have shown that stimulants such as amphetamines interact
with plasma-membrane monoamine transporters (dopamine, serotonin, and nor-
epinephrine transporters) (Gainetdinov et al 1999). The current treatment for
ADHD is with a stimulant medication such as Ritalin. Sales of Ritalin have in-
creased 700% since 1990 (Haislip 2002). Little is known about the long-term ef-
fect of stimulants on brain chemistry, and there is increasing concern about the
long-term use of Ritalin (Breggin 1998).
Some research on ADHD suggests many different contributing factors are
involved, including sensitivity to the yellow dye tartrazine. However, no definite
cause for the disorder has been found. Recent research at Harvard and Massa-
chusetts General Hospital shows adult subjects with longstanding ADHD have
Chapter 23 Pediatrics 349

an abnormal elevation in their number of dopamine transporters. Ritalin was
thought to work by altering levels of dopamine. However, studies with rats sug-
gest Ritalin works by boosting serotonin levels in the brain. The researchers con-
cluded that ADHD may occur when the chemical balance between dopamine
and serotonin is thrown off (Caron 1999).
I have found that children with ADHD become more stimulated with seda-
tive essential oils such as Roman chamomile and lavender. So, I tried essential oils
with stimulant properties and found they had a relaxing effect. Because of this
finding, two of my students carried out two separate studies on ADHD using two
different essential oils. The first study, by Sorenson (1999), was very simple and
involved observing four children with ADHD who were attending piano lessons.
When lavender (Lavandula angustifolia) was diffused into the air, all four children
became more inattentive and restless. When rosemary (Rosmarinus officinalis) was
diffused into the air, three of the four children became more attentive and less
restless.
Sptizer (2000) carried out a study on 10 children (aged 7-9 years) attending
a school for children with special needs. Children who were prone to seizures
were excluded from the study. Two occupational therapists conducted the exper-
iment at the school and used a Likert scale for analysis. Baseline data were
recorded for four separate visits. This included the number of times the children
got out of their chairs, the number of times the children needed directions re-
peated, the number of times the children engaged in self stimulation (rocking),
and the number of minutes the children sustained attention to a particular task.
During the experimental stage, two drops of Rosmarinus officanalis were placed on
an aromastone before each of the four occupational therapy sessions. (An aroma-
stone is a ceramic stone that uses electricity to gently heat a few drops of essen-
tial oil placed on the stone.)
As each child was so different, the data were discussed individually. In the
best case scenario, child six managed to focus with rosemary and sustained atten-
tion for up to 23 minutes, instead of 18 without the oil. Child one sustained fo-
cused attention for 9 minutes instead of 3 minutes. Child three was able to re-
main seated longer. Child four, who was prone to tantrums, did not have any
tantrums during the aromatherapy sessions. Child five did not have any self-
regulating problems, and therefore there was no room for improvement. Three
other children had slight improvements overall, two children had no difference,
and one child performed worse. Although this study is inconclusive, both occu-
pational therapists felt the findings warranted further study.
Pitman (2000) invited a group of 11 children with ADHD to choose three
essential oils from a selection of 15 oils that included stimulant and sedative es-
sential oils. The three were then mixed together, diluted in vegetable oil, and ap-
plied to the children’s wrists. The same mixture was sometimes used at home in
a bath or diffused into the air. The oils appeared to relax the children, increase
their concentration in class, and decrease disruptions, and the children all ap-
peared calmer. The parents agreed the essential-oil mixtures had helped their
350 Section II Clinical Use of Aromatherapy

children calm down. However, one parent said the child became hyperactive
when a citrus aroma was vaporized for too long.
Pediculosis (Head lice)
Head-louse infestation is common worldwide. In developed countries the infesta-
tion rate is increasing, especially in the 4- to 13-year-old age group (Mumcuoglu
1999). This increased infestation could be due to the incorrect use of effective
agents that has led to lice strains becoming resistant to insecticides. Compounds
such as Permethrin, malathion, and DDT are no longer sucessful (Combescot et
al 1996). Izri and Briere (1995) report on the first case of resistant head lice in
France in Paris and Tours, citing that resistance had already occurred in the
United Kingdom. Most pediculicides are only partially ovicidal, resulting in an-
other batch of new lice after 10 days. It is important that a special lice comb is
used and all the eggs are removed after treatment, as some nits can remain glued
to the hair for several months, even if they are dead. Suffocating agents such as
olive, soya, or sunflower vegetable oil can be effective if used for more than 12
hours. While some studies have shown that essential oils can be pediculicidal,
there is no evidence that essential oils repel lice (Mumcuoglu 1999).
Veal (1996) tested seven essential oils and three blends (by Shirley Price) in
vitro. Aniseed, oregano, cinnamon leaf, red thyme, and tea tree all performed well
when tested in an alcoholic solution using overnight exposure. Veal concluded it
would be important to use the same essential oil in the rinse that was contained
in the original application. She recommended using an essential oil, vinegar, and
water solution but alcohol and water could also be effective. Phenols and pheno-
lic ethers, ketones, and 1,8-cineole appeared to be the compounds most likely to
kill lice.
Laurent et al (1997) reported that linalol, menthone, menthol, and limonene
were also effective larvicides and ovicides. Gauthier et al (1989) showed that a-
pinene was another effective compound against head lice in his study on the ef-
fectiveness of Myrtle.
Lahlou et al (2000) investigated the effectiveness of 24 essential oils and 15
of their isolated compounds against human head lice in vitro using microatmo-
sphere and direct application. Mentha pulegium (pennyroyal), Thymus broussonetti,
Chenopodium ambrosioides (American wormseed), and Ruta chalepensis were found
to be the most effective. Unfortunately, these essential oils are not the most suit-
able for children. (It was interesting that they did not include tea tree in their
study.) The lice died within 15 minutes of direct application by the essential oils.
However, the nits were a little more difficult. At a 1:4 dilution of Thymus brous-
sonettii applied directly, 20% of the nits hatched. Of the isolated compounds, phe-
nols and phenolic ethers, ketones, and 1,8-cineole were the most effective.
Oladimeji et al (2000) investigated the effects of Lippa multiflora essential oil
on head and body lice and scabies and found it effective. In the study, 0.02 ml of
a 25% solution of Lippia in liquid paraffin was sufficient to kill head lice within
Chapter 23 Pediatrics 351

2 hours. (The lice had been removed from the children to a petri dish.) Lippia
multiflora was more effective than benzyl benzoate at the same concentration, but
not as effective as kerosene.
REFERENCES
ADD/ADHD research. Jan. 11, 2001. ADD/ADHD Online Support Group.
www.adders.org.
Bradshaw R, Marchant J, Meredith M, et al. 1998. Effects of lavender straw on stress
and travel sickness in pigs. Journal of Alternative & Complementary Medicine. 4(3)
271-275.
Breggin P. 1998. Report to the plenary session of the NIH consensus conference on
ADHD and its treatment. www.breggin.com.
Caron M. 1999. Role of serotonin in the paradoxical calming effect of psychostimulants
on hyperactivity. Science. 283:397-401.
Clark G. 1995. An aroma chemical profile: indole. Perfumer & Flavorist. 20(2) 21-31.
Collin G, Hoeke H. 1993. Ullman’s Encyclopedia of Industrial Chemistry, Vol. 14, 5th
ed. Weinheim, Germany: VCH.
Combescot C, Combescot-Lang C, Remy-Kristensen A, et al. 1996. Tests for evaluating
the effectiveness of pediculicides: importance and limitations. Bulletin de l’Academie
Nationale de Medecine. 180(6) 1315-1323.
Engen T. 1974. Method and theory in the study of odor preferences. In Johnston J (ed.),
Human Response to Environmental Odors. New York: Academic Press, 121-141.
Gainetdinov R, Wetzel W, Jones S, et al. 1999. Role of serotonin in the paradoxical
calming effect of psychostimulants on hyperactivity. Science. 283(5400) 397-401.
Gainetdinov R, Caron M. 2001. Genetics of Childhood Disorders: XXIV, Part 8: Hy-
perdopaminergic mice as an animal model of ADHD. Journal of the American Acad-
emy of Child Psychiatry. 40(3) 380-382.
Gauthier R, Agoumi A, Gourai M. 1989. Activite d’extraits de Myrtus communis contre
Pediculus humanis capitis. Plantes Medicinales et Phytotherapie. 23(2) 95-108.
Haislip G. 2002. Ritalin: the smart drug? www.vanderbilt.edu/AnS/psychology. Accessed
September 2002.
Hodson D. 1995. The special needs of children and adolescents. In Penson J, Fisher R
(eds.), Palliative Care for People with Cancer, 2nd ed. London: Edward Arnold,
198-229.
Howard Hughes Medical Institute News ( Jan 15, 1999 newsletter). Nov. 4, 1999. Sero-
tonin may hold key to hyperactivity disorder. www.hhmi.org/news/caron2.html.
Humphrey T. 1940. The development of the olfactory and the accessory olfactory forma-
tions in human embryos and fetuses. Journal of Comparative Neurology. 73:431-468.
Izri M, Briere C. 1995 First cases of resistance of Pediculus capitis Linne 1758 to
malathion in France. La Presse Medicale. 24(31) 1444.
Kurfit Stephens B, Barkey M, Hall H. 1999. Technique to comfort children during
stressful procedures. Advances in Mind-Body Medicine. 15(1) 49-60.
Lahlou M, Berrada R, Agoumi A, et al. 2000. The potential effectiveness of essential oils
in the control of human head lice in Morocco. International Journal of Aromatherapy.
10(3/4) 108-123.
352 Section II Clinical Use of Aromatherapy

Laurent D, Vilaseca L, Chantraine J, et al. 1997. Insecticidal activity of essential oils on
Triatoma infestans. Phytotherapy Research. 11(4) 285-290.
McFerran T. 1996. A Dictionary of Nursing, 2nd ed. Oxford, UK: Oxford University
Press.
Mehta S, Stone D, Whitehead H. 1998. Use of essential oil to promote induction of
anesthesia in children. Anaesthesia. 53(7) 720-721.
Mumcuoglu K. 1999. Prevention and treatment of head lice in children. Pediatric Drugs.
1(3) 211-218.
Oladimeji F, Orafidlya O, Ogunniyi T, et al. 2000. Pediculocidal and scabicidal proper-
ties of Lippia multiflora essential oil. Journal of Ethnopharmacology. 72(1-2) 304-311.
Parish P. 1991. Medical Treatments: The Benefits and Risks. Harmondsworth, UK:
Penguin Books.
Pitman V. 2000. Aromatherapy and children with learning difficulties. Aromatherapy
Today. 15:20-23.
Russell M. 1976. Human olfactory communication. Nature. 260:520-522.
Schleidt M, Genzel C. 1990. The significance of mother’s perfume for infants in the first
weeks of their life. Ethology and Sociobiology. 11(1) 145-150.
Schilcher H. 1997. Physiotherapy in Pediatrics. Stuttgart, Germany: Medpharm.
Sorenson K. 1999. Effects of aroma with poor attention span in music lessons. Unpub-
lished dissrtation. Hunter, N.Y.: R J Buckle Associates.
Sptizer H. 2000. Special needs children and aromatherapy: rosemary oil. Unpublished
dissertation. Hunter, N.Y.: R J Buckle Associates.
Tucker S. 1999. Attention deficit hyperactivity disorder. Journal of the Royal Society of
Medicine. 92(5) 217-219.
Veal L. 1996.The potential effectiveness of essential oils as a treatment for headlice,
Pediculus humanus capitis. Complementary Therapies in Nursing & Midwifery. 2(4)
97-102.
Worwood V. 2000. Aromatherapy for the Healthy Child. Navato, CA: New World
Library.
Chapter 23 Pediatrics 353

354
W
24
Psychiatric Care
The use of scents is not practiced in modern physic but might be carried out with
advantage seeing that some smells are so depressing and others so inspiring and
reviving.
Sir William Temple (1701)
Essay on Health and Long Life
A
nyone who believes scent does not have a profound impact on the human
psyche should read Perfume: The Story of a Murderer (Suskind 1987). The
novel is set in 18th-century France, and Grenouille, the lead character, is
born with a heightened sense of smell but without body odor himself. These two
factors rule his life and impact those around him with devastating consequences.
Pickover (1998) quotes Hippocrates, who wrote, “Men ought to know that from
nothing else but the brain come joys, delights, laughter and sports, and sorrows,
griefs, despondency and lamentations.”
Wiener (1966) of the New York Medical College suggested our bodies have
an internal and external communicating system that uses our nervous system
without alerting us to its existence. Such a system is made up of chemicals and
interacts with the other systems in the body by means of odor. He further sug-
gests that if someone had the ability to communicate consciously in this system
it could be distressing. Subsequent to this theory was the discovery that schizo-
phrenics give out a persistent aroma discernible to dogs and rats. This aroma be-
comes more pronounced when they are in crisis (Smith & Sines 1960).
Certainly there is a link between depression and the inability to smell (anos-
mia) (Douek 1988). Aristotle noted that pleasurable aromas could contribute to
the well being of humans, and both malodors and bad odors impact on our health.
Stand next to a garbage dump downwind for just a few moments and you get a

good sense of this! Malaria literally means “bad air” as it was believed that odor
emanating from marshes caused the disease (King 1988).
The use of psychoactive products evolved along two related paths: for reli-
gious or recreational pursuits and to modify normal behavior (Alexander 2001).
The effects of aromas on the brain were first tested by Moncrieff (1966) using an
electroencephalograph to monitor changes in brainwave patterns. He found that
basil, black pepper, cardamom, and rosemary induced mainly beta patterns and
that jasmine, neroli, and rose induced mainly delta patterns (Moncrieff 1977).
Beta brain patterns (13-40 cycles per second) are concerned with attention and
alertness. Delta brain patterns (0-4 cycles per second) are concerned with eupho-
ria and calmness (Mureriwa 2001). Dodd and Van Toller (1983) compared the ac-
tion of chemical components found in essential oils to the action of psychotropic
drugs such as antidepressants. Torii et al (1988) reported on the electrical changes
of the brain and the similarities between emotion and the sense of smell. King
(1988) postulated the relation between odor and olfaction was probably a two-
way relationship.
A report in the Journal of the American Medical Association suggests a study of
smell could shed light on some of the symptoms of schizophrenia. Dr. Daniel
O’Leary from the University of Iowa Hospitals and Clinics exposed 18 people
with schizophrenia and 15 healthy volunteers to a pleasant smell (vanilla) and an
unpleasant smell (O’Neil 2001). An imaging device was used to track blood flow
to different areas of the brain, and subjects were asked to rate each smell. The
mental imaging showed big differences between the two groups in the mental
processing of the unpleasant smell. The limbic system appeared to be highly ac-
tive in healthy subjects but largely unused with people with schizophrenia. The
latter depended more on frontal cortical areas usually reserved for functions such
as decisionmaking. This misuse of brain circuits could play a role in paranoia.
Insanity or mental illness is an area of fear for many people, and yet almost
everyone has experienced insanity at some time in their life: a crazy decision, a
wrong choice, a mad moment, a dark time. I remember when my son went miss-
ing. He was only 2 years old and my daughter was a newborn. One moment he
was there next to the cheese counter in the supermarket, and the next moment he
was gone. During the following 2 hours I experienced a sense of insanity and all
reality appeared put on hold.
During times like this, one’s link with reality can seem blurred as sensory
perception becomes skewed and basic physical needs are forgotten. This is when
familiar smells and reassuring touch may help find a way out of the fog and back
to reality. Patients with mental-health problems are a constant reminder just how
fragile sanity is.
Aromatherapy and Mental Illness
“Components within essential oils that alter brain chemistry and relieve psychi-
atric symptoms have brought great hope and help to many people” (Alexander
Chapter 24 Psychiatric Care 355

2001). Sugano (1992) suggests natural fragrances can provide a cost-effective and
efficient alternative to many common drug treatments, especially stimulants and
sedatives. Tisserand (1988) suggests olfactory “ecstasy” was discovered by man at
a very early age, and that aromatics can be perceived as drugs. Alexander (2001)
suggests that “EOs [essential oils] for the brain that have antidepressant, mood-
balancing, anxiolytic and hormone regulating properties are nourishment at the
biochemical level.”
Most synthetic psychotropic medications have limited efficacy and signifi-
cant side effects, and preliminary findings suggest several treatments based on
natural substances are as effective and safe as the synthetic pharmaceuticals in
current use (Lake 2000). Lake’s review article on the use of herbs for neurologi-
cal problems is a must-read. However, the number of herbs he covers is limited
by space. The Napralert database (which I have used extensively for this book)
contains more than 1000 citations on herbs useful for psychiatry.
Many health professionals working in psychiatric units have been grateful for
strong sedatives when patients have become psychotic and unmanageable. How-
ever, there are some people who are may just have a poor ability to cope with life.
This could be due to genetics, environmental issues, or just one of those unex-
plainable things. However, with the demand for a cure, or at least medicine, seems
to be a growing group of people who take antidepressant drugs but who are not
clinically depressed. They are just life depressed. In the words of Patch Adams,
MD (1997), “Prozac has replaced a hug.” It is this shadowy area in which aro-
matherapy may help. While all the hi-tech advances in the world cannot rewire
the brain, something as simple as an essential oil can enable the brain to reregu-
late itself (Alexander 2001).
Addiction
Today’s society is an addictive one, and it often rewards socially acceptable addic-
tions like workaholism, in addition to accepting shopaholics and nicotine addic-
tion, condoning alcohol addiction, and prosecuting drug addiction. Yet the ethos
behind addiction—instant gratification—is at the very core of today’s society.
People want things instantly. Large portions are required even if they cannot be
eaten. Everything must be big. It is as though people feel too small in a world that
undervalues them. Reassurance of worth is sought from external sources rather
than from within. It is as though people have a hole in their wholeness and are
hungry for anything that will stop the feeling of emptiness. Health professionals
are often presented with evidence of a sick society in which individuals who do
not fit in or are unable to cope are isolated, ridiculed, or forgotten.
A few detoxification programs have included herbal treatment protocols for
the management of acute benzodiazepine or opiate withdrawal with positive ef-
fects (Rasmussen 1996). But there is scant if any published literature on the use
of essential oils for alcohol or benzodiazepine withdrawal. However, some anec-
dotal success with weaning patients from antidepressants and night sedation us-
ing both nontouch modality (diffusers at night and face tissues during the day)
356 Section II Clinical Use of Aromatherapy

and the “m” technique has been achieved. The process was very gradual and un-
der physician control. This is not recommended unless physician support is given.
Limited success with helping reduce the cravings of women withdrawing from al-
cohol has also been achieved using specific inhaled essential oils (Lundgren
1999). A protocol that has been used is shown in Table 24-1.
The idea that an olfactory stimuli might reduce craving for nicotine was in-
vestigated by Seyette and Parrott (1999). They found that both negative and pos-
itive aromas decreased cravings against a nonodoriferous control in nicotine ad-
diction. The sense of smell is lessened in a heavy smoker; nevertheless,
aromatherapy has achieved some modest success. DaCosta (1999) explored in-
haling essential oil as a means to reduce the craving of nicotine withdrawal. The
three essential oils tested were lavender (Lavandula angustifolia), Helicrysum
italicum, and Angelica archangelica. Four male subjects who smoked at least 10 cig-
arettes a day and had tried to stop smoking in the past were recruited. The period
immediately after breakfast, lunch, and supper were chosen as those were the
hardest times to abstain from smoking. The normal period the test subjects could
wait before smoking (baseline) was minimal, less than 2 minutes. Each essential
oil was then tested separately for 5 consecutive days, divided by a dry-out period
of 2 days, and the subjects timed how long they could last without a cigarette. An-
gelica root appeared to be the most helpful, with subjects able to wait an average
of 53 minutes before having a cigarette. This was considerable improvement on 2
minutes, although inhaling angelica did not prevent them from smoking after 53
minutes.
Chapter 24 Psychiatric Care 357
Table 24-1
h Protocol for Coming Off Benzodiazepine or Night Sedation
with Aromatherapy
Week 1 Choose aroma(s) from a selection of six.
Choose touch or nontouch application. Apply oil in office.
Give written instructions on when and how to use aromatherapy.
Week 2 Reduce medication by
1
⁄
4
.
Week 3 Reduce medication by further
1
⁄
4
.
Week 4 Remain on
1
⁄
2
medication .
Week 5 Reduce medication to
1
⁄
4
.
Week 6 Remain on
1
⁄
4
medication.
Week 7
1
⁄
4
medication alternate days.
Week 8 Remain on
1
⁄
4
alternate days.
Week 9
1
⁄
4
medication twice a week.
Week 10
1
⁄
4
medication once a week.

Rose and Behm (1994) used black pepper essential oil as an aid in a smoking-
cessation program. They hypothesized that clients needed to experience the res-
piratory-tract sensations that accompany cigarette smoking to quit successfully,
and they believed black pepper essential oil could simulate those sensations. They
found “the vapor of black pepper essential oil, when inhaled, partially reproduces
the respiratory tract sensations experienced when smoking, thereby reducing the
craving for cigarettes.”
Newsham (2001) explored the effect of aromatherapy as an adjunct to auric-
ular acupuncture for drug detoxification at Yonkers General Hospital in New Jer-
sey. This was a study compared to a historical control. Two hundred eighty-two au-
ricular treatments (some subjects received more than one treatment) were given
with ambient odor of lavender in the room. The comparison group received 230
auricular treatments without lavender. Two standard aromatherapy diffusers were
used to diffuse a room of approximately 400 square feet. Twenty drops of lavender
were placed in the nebulizer. All patients routinely completed a short questionnaire
before and after treatment. Analysis was done to see if there was any difference be-
tween the aromatherapy group and the comparison group. Fifty percent of patients
did not complete the full 21 days of treatment. The actual treatment range was
1-14 with an average of 4. Data were collected monthly and aggregate data were
used. Questions ranged from “How are you feeling right now?” to “How would you
rate any cravings you have right now?” The choice of answers was on a 0-5 scale.
There was no difference between the aromatherapy group and the compari-
son group in the number of patients who said they felt “very good” physically or
emotionally after the treatment. There was a difference in those who felt “good”
physically and emotionally. Physically, there was 6% change in the comparison
group and a 24.8% change in the aromatherapy group. Emotionally, there was
4.6% change in the comparison group and a 24.9% change in the aromatherapy
group. However, there seemed to be no difference in the cravings. More than half
the patients said they were unable to smell the essential oils diffused into the room.
Caldwell (2001) explored the effects of ylang ylang (Cananga odorata) in a
small, controlled study of 10 women suffering from cravings following with-
drawal of substance abuse. All women were taking orthodox medication. The par-
ticipants were randomly split into two groups: an experimental group and a con-
trol group. The experimental group was given essential oil of Cananga odorata
(ylang ylang) to inhale, and the control group received plain almond oil. Both
groups were told that they were using ylang ylang oil. The participants were self-
selecting and limited to women dealing with chemical addiction. All 10 partici-
pants had either stopped using and were still experiencing cravings, or were try-
ing to stop using and were experiencing cravings.
Each participant put two drops of the oil on a cotton square and put the
square in her pillowcase every night for seven nights. The participants were also
asked to put two to three drops of oil on a cotton hanky, carry the hanky with them
for seven days, and smell it if they experienced a craving. The participants were
asked to record the number of cravings, their intensity, and any other comments.
358 Section II Clinical Use of Aromatherapy

The results showed the number of cravings for the essential oil group went
down more than for the control group. However, ylang ylang did not prevent
cravings completely. Four out of 5 women in the experimental group believed
“smelling the oil relieved the stress and anxiety of that moment.” None of the par-
ticipants using the almond oil expressed this feeling. Caldwell (2001) notes that
ylang ylang’s positive effect might be enhanced by using a diffuser at night.
Olfactory loss is common in alcoholics (Shear et al 1992), cocaine users
(Schwartz et al 1998), and heroin addicts (Perl et al 1997). Loss of smell is not
thought to affect the transfer of the volatile molecules unless there is damage to
the olfactory nerve. Loss of smell in addicts is thought to be due to damage to the
cortical and subcortical brain regions (Shear et al 1992), but it is possible there is
nerve damage due to snorting or sniffing cocaine, heroin, and glue.
Bipolar Disorder
Approximately 2.5 million Americans are thought to be affected with bipolar dis-
ease. Originally named manic-depression, the disease was discovered by German
psychiatrist Emil Kraepelin after carefully observing many patients in the 19th
century (DRADA 2001). Kraepelin found many patients had spontaneous re-
mission of symptoms that could last for months or years before relapsing and that
patients who had suffered episodic periods of illness in their 20s were more likely
to have them in their 40s. Psychiatrists today conclude that bipolar disease is a re-
lapsing illness that may recur more frequently as the patient ages. Bipolar disease
is thought to run in families, and recent research is concentrating on chromosome
18 in an attempt to locate the gene responsible (Stine et al 1995). However, bipo-
lar disease is quintessentially a disease of the Western world. The World Health
Organization conducted studies over a 25-year period and found that in under-
developed countries, psychotic disorders such as bipolar were fewer, less severe,
and resolved more rapidly (Sartorius 1990).
People, and in particular scientists, have a fascination with putting things in
categories. Since manic-depressive disorder became bipolar disorder, bipolar has
been divided into seven subcategories:
1. Pure mania;
2. Mixed mania (symptoms of mania and depression appearing simultane-
ously);
3. Rapid cycling (four or more episodes a year);
4. Secondary mania (appearance of mania after another illness);
5. Bipolar disorder with coexisting substance abuse;
6. Bipolar disorder type II (mildly manic states); and
7. Cyclothymia (chronic mood cycles with depression or mania too mild to
be classified).
Because mental illness is thought of as a brain disorder, magnetic resonance
imaging is frequently used as a diagnostic tool (DRADA 2001), although there
are inconsistent findings. The areas of the brain examined are the amygdala, the
entorhinal cortex, and the asymmetries—areas of the brain bigger on one side
Chapter 24 Psychiatric Care 359

than the other. In the brain of a normal, right-handed person, the brain area for
language is much bigger on the left side (Pearlson 1996). Pearlson also found
schizophrenic patients had greatly shrunken entorhinal cortexes and striking re-
versal of some key brain asymmetries. In bipolar patients these structures looked
normal, although the amygdala was slightly shrunken. In mood-disorder patients,
the amygdala was significantly shrunken on the left side.
Many neurological problems are a function of altered brain pattern and a
change in neurochemicals. Conventional drug treatment is with Lithium, dival-
proex (Depakote), and carbamazepine (Tegretol). However, all three have signif-
icant side effects. Bowden (1996) suggests Lithium has a narrow band of effec-
tive blood levels before reaching toxicity. However, Purol-Hershey (2002), a
psychiatric nurse and teaching professor, states that the band 0.5-1.2 mg is pretty
broad for lithium. The information on Tegretol suggesting precautions for “emo-
tional or mental problems” could be perceived as rather strange as the drug is pre-
scribed for bipolar disorder (Winter Griffith 1997). However, Tegretol is also an
antiseizure medication with mood-stabilizing features. Table 24-2 has been cre-
ated from information in Treatment Options in Bipolar Disorder by Bowden (1996)
360 Section II Clinical Use of Aromatherapy
Table 24-2 h Commonly Used Medications for Bipolar Disorder:
Benefits and Common Side Effects
Lithium
Depakote
Carbamazepine
Pure mania, history of
depression, family his-
tory of bipolar disor-
der, previous favorable
response to Lithium,
few previous episodes,
full relief between
symptoms
Mixed mania, nonfa-
vorable response to
Lithium, mood swings,
adverse effects less se-
vere, attention deficit
hyperactivity disorder,
substance abuse
No family history of
bipolar disorder, bipo-
lar disorder is a sec-
ondary condition, lack
of response to other
medication
May correct
chemical imbal-
ance in brains’
transmission of
nerve impulses
that influence
mood and be-
havior
Increases gamma
aminobutyric
acid, which in-
hibits nerve
transmission to
parts of the brain
Analgesic, anti-
convulsant
Weight gain, dry
mouth, confusion,
poor concentra-
tion, shakiness,
tremor, increased
urination
Loss of appetite,
nausea, diarrhea,
tremor, unusual
weight gain (or
loss), menstrual
changes
Dizziness, blurred
vision, headaches,
back-and-forth
eye movement
(nystogmus)

and the Complete Guide to Prescription and Nonprescription Drugs (Winter Griffith
1997).
The human body is controlled by extremely delicate mechanisms that rely on
hormonal and chemical communication. Each person has a slightly different body
chemistry that requires different things to achieve homeostasis. Like herbs, es-
sential oils are therapeutically multifaceted. Therefore, the components within an
essential oil may produce a different reaction in one person than in another, de-
pending on the availability of receptor sites (Mills 1991). For example, an essen-
tial oil may work to reduce blood pressure (acting as a hypotensor) if that is what
is required for homeostasis, or it may not if the blood pressure is normal for that
person. When a plant has the ability to change function it is called adaptogenic.
Many essential oils also have a balancing effect on the emotions.
Various antipsychotic agents have antagonistic interactions toward a whole se-
lection of receptor sites including serotoninic, adrenergic, and histaminic. There-
fore their ongoing effects on the autonomic nervous system are complex and un-
predictable (Alexander 2001). This is the case with each of the hundreds of
components in essential oils that interact with many receptor sites. While antide-
pressants work by making the neurotransmitter serotonin linger in the gaps be-
tween brain cells, essential oils are thought to work as serotonin agonists, which
can push the serotonin system into overdrive. This makes the brain more sensitive,
rather like turning up the volume on a radio so very weak stations can be heard.
There is no suggestion that bipolar patients should give up medication in fa-
vor of aromatherapy. There is little if anything published on bipolar disorder and
aromatherapy. However, essential oils may enhance orthodox medication so
dosages may be kept sufficiently low and reduce side effects. However, a few psy-
chiatric nurses who were my students have had some success with stabilizing pa-
tients using aromatherapy. As these were case studies it is difficult to say whether
the patients’ stability would have happened anyway. Other case studies by psychi-
atric nurses have indicated aromatherapy may help reduce the need for orthodox
medication and still retain stability (Table 24-3).
A set ritual or protocol is useful when working with bipolar patients. This is
worked out in detail with the patient: the when, where, and how of treatment. Es-
sential oils need to be experienced for the first time in a stable, calm, balanced sit-
uation with supervision. When this pattern is well established, the essential oils
can be experienced in the patient’s own setting. This is akin to preparing a “psy-
chological comfort blanket.” This setting of a psychological trigger is similar to
Bett’s research (1994) with epilepsy. He found massage with ylang ylang set a
precedent so strong that ultimately patients had only to think about the aroma of
ylang ylang to prevent a seizure occurring.
Tisserand and Balacs (1995) suggest several essential oils should be avoided
with patients who are prone to seizure. It might be a good idea to avoid them in
bipolar patients as well. These oils are listed in Table 24-4.
The flowers of Matricaria recutita (German chamomile) contain apigenin,
which can completely inhibit central nervous system benzodiazepine binding
Chapter 24 Psychiatric Care 361

without sedation. There are no known negative side effects (Viola et al 1995).
Apigenin occurs in the CO
2
extract but not in the steam-distilled extract of Ger-
man chamomile. Valerian root (Valeriana officinalis) has been shown to reduce
mild to moderate anxiety and may be useful in substance withdrawal (Brown
1994). Essential oil of valerian root is available and could be combined with
Melissa officinalis essential oil for an enhanced sedative effect. Valerian is safe
to inhale in pregnancy, and long-term use does not produce dependency. The
362 Section II Clinical Use of Aromatherapy
Table 24-3 h Balancing Essential Oils that May Be Useful in Cases
of Bipolar Disorder
Table 24-4 h Essential Oils to Avoid in Bipolar Disorder
Essential Oil Suspect Component Amount (approximate)
White camphor Camphor 30%-50%
Hyssop Pinocamphone 70%
Nutmeg Myristicin, Elemicin 3%-14%
0.1%-4.6%
Pennyroyal Pulegone 55%-95%
Tansy Thujone 66%-81%
Botanical Name
Pelargonium graveolens
Lavandula angustifolia
Santalum album
Angelica archangelica
Rosa damascena
Pogostemon cablin
Cananga odorata var. genuina
Valeriana fauriei
Vetiveria zizanoides
Nardostachys jatamansi
Melissa officinalis
Citrus bergamia
Salvia sclarea
Common Name
Geranium
Lavender
Sandalwood
Angelica root
Rose
Patchouli
Ylang ylang
Valerian
Vetiver
Spikenard
Melissa
Bergamot
Clary sage

therapeutic effects are thought to be through gamma-aminobutyric acid-antago-
nistic action (Lake 2000).
Lake (2000), a board-certified psychiatrist, reports the oral intake of St John’s
wort (Hypericum perforatum) is effective in certain mild depression, seasonal af-
fective disorder, and other neurological malfunctions. Essential oil of Hypericum
perforatum offers a more concentrated version that so far has not shown any of the
photosensitivity problems connected with the oral intake of St. John’s wort. This
could be an interesting area for further research.
REFERENCES
Adams P. 1997 (June). Lecture at AHNA conference, Burlington, VT.
Alexander M. 2001. How Aromatherapy Works. Odessa, FL: Whole Spectrum Books.
Bett T. 1994. Sniffing the breeze. Aromatherapy Quarterly. 40:19-22.
Bowden C. 1996. Treatment of bipolar disorder. The American Psychiatric Press Text-
book of Psychopharmacology. Chapter 29:603-614.
Brown D. Fall 1994. Valerian root: non addictive alternative for insomnia and anxiety.
Review of Natural Medicine. 221-224.
Caldwell N. 2001. Effects of ylang ylang on cravings of women with substance abuse.
Hunter, N.Y.: R J Buckle Associates.
DaCosta R. 1999. Nicotine withdrawal and aromatherapy. Unpublished dissertation.
Hunter, N.Y.: R J Buckle Associates.
DePaulo JR. Sept. 4, 2001. Recent findings in the genetics of bipolar disorder, Smooth
Sailing, 1996. Depression and Related Affective Disorders Association.
www.med.jhu.edu/drada.
Dodd G, Van Toller S. 1983. The biology and psychology of perfumery. Perfumer &
Flavorist. 8:1-14.
Douek E. 1988. Abnormalities of smell. In Van Toller S, Dodd G (eds.), Perfumery: The
Psychology and Biology of Fragrance. London: Chapman and Hall, xvii-3.
King J. 1988. Anxiety reduction using fragrances. In Van Toller S, Dodd G (eds.), Per-
fumery: The Psychology and Biology of Fragrance. London: Chapman and Hall,
147-167.
Lake J. 2000. Psychotropic medications from natural products: a review of promising re-
search and recommendations. Alternative Therapies in Health & Medicine. 6(3)
36-60.
Lundgren W. 1999. Clary sage for withdrawal cravings in alcoholic women. Unpublished
dissertation. Hunter, N.Y.: R J Buckle Associates.
Mills S. 1991.Out of the Earth. London: Viking Arkana.
Moncrieff R. 1966. Odor Preferences. New York: Wiley.
Moncrieff R. 1977. Emotional response to odors. Soap, Perfumery and Cosmetics.
50:24-25.
Mureriwa J. Jan. 2001. EEG Biofeedback. Retrieved March 17, 2003, from
www.biofeedback.co.2a/biofeedback-eeg.htm
Newsham G. 2001. Lavender for auricular acupuncture support in detoxification. Un-
published dissertation. Hunter, N.Y.: R J Buckle Associates.
O’Neil J. Jan. 2001. Smells used to explore schizophrenia. www.schizophrenia.com.
Chapter 24 Psychiatric Care 363

Pearlson G. Sept. 4, 2001. Excepts from schizophrenia vs. mood disorder: a puzzle
solved. Smooth Sailing, 1-2, 1996. Depression and Related Affective Disorders Asso-
ciation. www.med.jhi.edu/drada/pearlson.html.
Perl E, Shufman E, Vas A, et al. 1997. Taste and odor reactivity in heroin addicts. Israel
Journal of Psychiatry and Related Sciences. 34(4) 290-299.
Pickover C. 1998. Strange Brains and Genius. New York: Plenum.
Purol-Hershey S. Sept., 2002. Personal communication.
Rasmussen P. 1996. A role for phytotherapy in the treatment of benzodiazepine and opi-
ate drug withdrawal. European Journal of Herbal Medicine. 3(1) 12-21.
Rose J, Behm F. 1994. Inhalation of vapor from black pepper extract reduces smoking
withdrawal symptoms. Drug and Alcohol Dependence. 34(3) 225-229.
Sartorius N. 1990. Cultural factors in the etiology of schizophrenia. In Stefanis C (ed.),
Psychiatry: A World Perspective, Vol. 4. New York: Elsevier Science, 33-40.
Schwartz R, Estroff T, Fairbanks D, et al. 1998. Nasal symptoms associated with cocaine
abuse during adolescence. Archives of Otolaryngology-Head & Neck Surgery. 115(1)
63-64.
Seyette M, Parrott D. 1999. Effects of olfactory stimuli on urge reduction in smokers.
Experimental and Clinical Psychopharmacology. 7(2) 151-159.
Shear P, Butters N, Jernigan T, et al. 1992. Olfactory loss in alcoholics: correlations with
cortical and subcortical MRI indices. Alcohol. 9(3) 247-255.
Smith K, Sines J. 1960. Demonstration of a peculiar odor in the sweat of schizophrenic
patients. Archives of General Psychiatry. 2:184.
Stine O, Xu J, Koskela R, et al. 1995. Evidence for linkage of bipolar disorder to chro-
mosome 18 with a parent-or-origin effect. American Journal of Human Genetics.
57(6) 1384-1394.
Sugano H. 1992.Psychophysical studies of fragrances. In Dodd G, Van Toller S (eds.),
Fragrance: The Psychology and Biology of Perfume. London: Elsevier Science, 227.
Suskind P. 1987. Perfume: The Story of a Murderer. London: Penguin Books.
Temple W. 1701. Essay on Health and Long Life, 1701. In Cornaro L, 1915, The Art
of Living Long, Kessinger Publishing, www.kessinger-publishing.com.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
Tisserand R. 1988. Essential oils as psychotherapeutic agents. In Van Toller S, Dodd G
(eds.), Perfumery: The Psychology and Biology of Fragrance. London: Chapman and
Hall, 167-180.
Torii S, Fukada H, Kanemoto H, et al. 1988. Contingent negative variation (CNV) and
the psychological effects of odor. In Van Toller S, Dodd G (eds.), Perfumery: The
Psychology and Biology of Fragrance. London: Chapman and Hall, 107-118.
Viola H, Wasowski C, Levi de Stein M. 1995. Apigenin. A component of Matricaria re-
cutita flowers that is a central benzodiazepine receptor ligand with anxiolytic effects.
Planta Medica. 61:213-216.
Wiener H. 1966. External chemical messengers I. New York State Journal of Medicine.
66:3153.
Winter Griffith H. 1997. Complete Guide to Prescription and Nonprescription Drugs.
New York: Berkeley Publishing.
364 Section II Clinical Use of Aromatherapy

W
365
25
Respiratory Care
Scent has a persuasive power stronger than words, appearances, feelings and wishes.
There is no defense against the persuasive power of scent; it looks into us, like the air
we breathe enters our lungs, it fulfils us perfectly and there is no antidote to it.
Patrick Suskind (1987)
Perfume: The Story of a Murderer
O
f all the clinical specialties, perhaps respiratory care is the most obvious
candidate for aromatherapy, for when we inhale to smell, we inhale to
breathe as well. Why bother with digesting essential oils and “first pass”
(metabolizing them via the liver) when inhaled oils may work as well? Falk et al
(1990) noted the high solubility of ␣-pinene in human volunteers. Alpha pinene
(22%) is found in rosemary essential oil, camphor chemotype. Falk et al found
60% of ␣-pinene was absorbed through inhalation, but only 8% was exhaled. The
rest was excreted in the urine, suggesting inhaled essential oils could also treat
cystitis. Some essential oils taken by mouth are exhaled. Some essential oils given
rectally are excreted through respiration. Pulmonary excretion of 1,8-cineole,
menthol, and thymol was demonstrated following rectal application in rats, al-
though the percentage exhaled was extremely small (Grisk & Fischer 1969).
Air pollution has become more prevalent, especially in cities and especially
during the summer. Inner-city air seems to contain less and less oxygen and more
and more environmental toxins. In fact, for more than 30 years, environmental in-
fluences have been linked to chest problems (Cruz-Coke 1960). Environmental
pollutants range from dust mites to cockroaches and latex to second-hand smoke.
Cases of asthma and chronic bronchitis doubled between 1982 and 1994, and
more than 14 million Americans are now diagnosed with asthma (Weil 1997).
Three in 10 people consult their doctor at least once a year about a respiratory

disease, with the most common complaint being upper-respiratory tract infection
(Newman-Taylor 1995). In the United Kingdom, 10% of all prescriptions are for
drugs to treat respiratory problems (Lung and Asthma Information Agency
1995), and one in seven children has asthma. In 1995, 5600 deaths in the United
States were attributed to asthma (Weil 1997).
While some kinds of asthma could be exacerbated by essential oils, other
kinds can be greatly ameliorated. Eucalyptus radiata and Styrax benzoin (benzoin)
have been used by health professionals to treat respiratory infections for many
years (Stevenson 1995). Essential oils to avoid in asthma are those high in alpha-
and beta-pinene or delta-3-carene, as they were found to cause airway and
breathing discomfort during a study by Filipsson (1996) on turpentine. Bowles
(2000) also notes that inhalation of pinene-rich essential oils could cause this
problem in asthma. Alpha-pinene is found in Scotch pine (Pinus sylvestris), at a
level of 42%.
There are two chronic respiratory problems becoming endemic in the United
States, namely recurrent bronchitis and tuberculosis. These will be discussed in
this chapter.
Chronic Bronchitis, Asthma, and Sinusitis
Recurrent chest infections, or chronic bronchitis, are on the increase. Each out-
break of the disease begins with a dry cough followed by a mucolytic stage with
a productive cough. The underlying problem may be infection, viral or bacterial,
or it may be chronic inflammation similar to an allergy.
Essential oils have been used in cough medicines for many years (Boyd
1954). The expectorant action of a cough medicine is mainly due to the local ac-
tion of aromatics on the lining of the respiratory tract during exhalation, after the
medicine has been swallowed (Boyd & Sheppard 1970). Boyd (1967) found sys-
temic expectorants (including glyceryl guaiacolate) have little pharmacological
expectorant action. but some inhaled expectorants, such as cedar leaf, have an ef-
fect, even at a subliminal level (Boyd and Sheppard 1968). Kendig et al (1967)
found water vapor (steam) to be the most effective means of liquefying secretions,
and Boyd and Sheppard conclude in their 1970 paper that “inhaled expectorants
may be superior to systemic expectorants.” This certainly opens the way for aro-
matherapy as a useful modality for upper-respiratory infections.
Boyd and Sheppard (1970) found the expectorant effect of inhaled nutmeg
oil was due to its high camphene content (60%). However, the amount of cam-
phene may be adversely affected if the nutmeg has been irradiated (Wilmers &
Grobel 1990). According to The Merck Index (Budavari 1996) camphene is
found (to a lesser degree) in the oils listed in Table 25-1.
An ointment containing camphene and menthol was found to be effective in
reducing bronchospasms by 50% when it was insufflated through the respiratory
system of laboratory animals, but it was only slightly effective when applied cu-
taneously (Schaefer & Schaefer 1981). Applying essential oils to an airway with
366 Section II Clinical Use of Aromatherapy

nasal ointment has also been shown effective in stimulating airway secretary
glands and reducing mucus. However, caution is needed in pediatrics. In another
study, children were mistakenly given nosedrops that contained menthol or euca-
lyptol (constituents of essential oils) instead of saline drops. Adverse effects
ranged from irritated mucous membrane to tachycardia (Melis et al 1989).
In a randomized trial involving 182 institutionalized patients, “essence” drops
containing mint, clove, thyme, cinnamon, and lavender appeared to reduce the
frequency of bouts of chronic bronchitis (Ferley et al 1989). The essential oils
most effective in this study were clove, lavender, lemon, marjoram, mint, niaouli,
pine, rosemary, and thyme. This could be because some essential oils are known
to destroy airborne Staphylococcus aureus and Streptococcus pyogenes within hours,
and these would be an effective way of preventing ailments such as bronchitis
(Bardeau 1976). Other essential oils frequently used to treat chest infections are
Boswellia carterii (frankincense) and Pinus sylvestris (Scotch pine) (Sheppard-
Hanger 1995; Abdel Wahab et al 1987).
Charron (1997) carried out an exploratory study on 40 patients with
bronchial and sinus congestion. Patients inhaled two drops of Spike lavender
floating in a bowl of hot water. All patients cleared their mucus immediately with
results lasting from 20 minutes to 2 hours. Some patients who had been on yearly
repeat antibiotics no longer needed them.
A 3% solution of frankincense, Spike lavender, and lavender was used in an
exploratory study of eight patients with asthma (Spear 1999). Application was
topical to chest and back. The age of patients ranged from 14-70 years. Four pa-
tients registered a moderate improvement in their peak-flow meters, and three
registered a substantial improvement. Six patients noticed a change in their emo-
tional attitude, and the same six felt their sleep was much improved. No patient
became worse, but one patient noticed no improvement.
Lockhart (2000) used inhaled essential oil of Frankincense on eight subjects
(20-52 years of age), five females and three males, throughout a period of 6 weeks.
Following patch testing and assessment for allergies, the subjects were given a
bottle of pure essential oil from the same supplier (same batch number) and asked
to inhale it when they felt an asthma attack coming. A Likert scale was used at
Chapter 25 Respiratory Care 367
Table 25-1 h Essential Oils Containing Camphene
Common Name
Neroli
Citronella
Bergamot
Cypress
Ginger
Botanical Name
Citrus aurantium
Cymbopogon nardus
Citrus bergamia
Cupressus sempervirens
Zingiber officinale

the end of 6 weeks. All subjects felt their anxiety levels decreased when they in-
haled the frankincense, and all subjects decreased the use of their normal inhalers.
Pitcher (2001) studied the effects of inhaled Mentha piperita on 20 adult pa-
tients (age range 18-90) with chronic sinusitis. Five of the 20 patients had a his-
tory of medically diagnosed asthma. Four patients used inhalers daily. No patients
were using prescription decongestants daily, although 12 patients used over-the-
counter decongestants as necessary. Smokers were excluded from the study. Undi-
luted peppermint was inhaled for 10 minutes at a time. A small cushion with two
drops of peppermint on it was kept by the bedside to assist with night breathing.
Measurements of nasal congestion, sense of smell, headache, and postnasal drip
were taken. There was a significant improvement in all symptoms. Inhaler users
reported a decline in the number of times they used their inhaler. No side effects
were reported. When the symptoms returned at a later date, each participant
reached for the peppermint bottle again!
Machon (2001) carried out a controlled study to evaluate the effects of a mix-
ture of Eucalyptus globulus, Ravansara aromatica, Pinus sylvestris, and Mentha
piperita essential oils on sinus infections. Eight subjects (five females and three
males) used three drops of the mixture in a steam inhalation for 10 minutes, three
times a day for 5 days. Three subjects (both male and female) acted as controls
and received only steam inhalation. Baseline measurements of pain, sense of well-
ness, color of mucus, and amount of mucus were taken using a visual analog scale
of 0-10. The essential-oil group was consistently more improved with three of the
five members completely clear of congestion and two nearly free. By the fifth day,
their mucus was clear. In the control group, the congestion remained the same,
and the mucus remained green in color.
Rudansky (2000) used Eucalyptus globulus to good effect to aid expectoration
in a patient with cystic fibrosis. The subject, a 36-year-old woman, had pneumo-
nia and plural edema and was being treated with intravenous antibiotics (6 weeks
on and 3 weeks off ). She was also dependent on an oxygen-concentrator ma-
chine. Her mucus was thick, dense, and flecked with blood. Working with the
woman’s physician, Rudansky was able to increase the subject’s lung elasticity
causing a measurable reduction in pulse and oxygen demand. She used regular in-
halations and body treatments to help the woman relax. The cycle of intravenous
antibiotics was reduced, and at the time of writing the patient had received no an-
tibiotic cover for 2 months and was doing well. The patient felt the heaviness in
her lungs had decreased substantially, and she was sleeping better.
Mattys et al (2000) carried out a randomized, double-blind study to explore
the effects of myrtol. Myrtol is a standardized distillate marketed under the brand
name Gelomyrtol and contains ␣-pinene, 1,8-cineole, and d-limonene. Six hun-
dred seventy-six patients were divided into four groups. The experimental group
received myrtol orally (4 ⫻ 300 mg daily) for two weeks. The two control groups
received either cefuroxine (2 ⫻ 250 mg daily) or ambroxol (a mucolytic agent),
and the fourth group received placebo capsules (four daily) for 14 days. Patients
368 Section II Clinical Use of Aromatherapy

receiving myrtol experienced a significant reduction in coughing. Lung ausculta-
tion improved significantly. Myrtol was found to be comparable to the other med-
ications (and superior to the placebo) and carries no risk of causing bacterial re-
sistance.
Essential oils with expectorant properties may be unable to fight the infec-
tion causing the problem, in which case the cause of the symptom is not being
addressed. An aromatogram would be needed to culture the bacteria and find out
to which essential oil it was sensitive. There are laboratories that can do this (see
Appendix 3 and Chapter 7 on infections for more details). In many instances
the infection may linger in sinuses (Belaiche 1979a). Some infections that are re-
sistant to antibiotics can be alleviated with the use of the correct essential oil
(Carson et al 1995). Table 25-2 lists essential oils I have used to treat respiratory
problems.
Belaiche (1979a) found thyme (Thymus vulgaris) and cinnamon (Cinnamo-
mum zeylanicum) were effective against Streptococcus aureus and lavender (Lavan-
dula angustifolia), marjoram (Origanum majorana), and winter savory (Satureja
montana) effective against Staphylococcus aureus (Belaiche 1979). Eucalyptus globu-
lus (2%) will kill 70% of ambient Staphylococcus aureus within hours. Duke writes
that in Cuba essential oil of Eucalyptus globulus is used to treat all lung ailments
(Duke 1985).
Chapter 25 Respiratory Care 369
Table 25-2 h General Respiratory Aid Essential Oils Used by the Author
Common Name
Ravansara
Gully gum
Spike lavender
Sweet marjoram
Lavender
Niaouli
Scots pine
Rosemary
Thyme
Tea tree
Blue gum
Cypress
Botanical Name
Ravansara aromatica
Eucalyptus smithi
Lavandula latifolia
Origanum majorana
Lavandula angustifolia
Melaleuca viridiflora
Pinus sylvestris
Rosmarinus officinalis CT cineole
Thymus vulgaris CT linalol, CT thujanol
Melaleuca alternifolia
Eucalyptus globulus
Cupressus sempervirens

Tuberculosis
Tuberculosis (TB) is a mycobacterial disease spread by droplet infection. Primary
TB is usually pulmonary. A peripheral lesion forms, and its draining nodes are in-
fected, so there is early spread of the bacillus throughout the body. Immunity
rapidly develops, and the infection becomes quiescent at all sites. The most com-
mon nonpulmonary primary infection is in the ileocecal junction and associated
lymph nodes (Hope et al 1993). Postprimary TB occurs when any form of im-
munocompromise allows reactivation. The lung lesions progressively fibrose, par-
ticularly in the upper lobe. Sometimes the bacilli can spread to other parts of the
body, setting up nodular lesions called tubercules (McFerran 1996). Sometimes
bone, brain, or genitourinary tract is involved.
TB was relatively well controlled in the Western world by Bacille Calmette-
Guerin (BCG) vaccine, and infection numbers fell to 10 in 100,000 people
by the end of the 1980s (MacSween & Whaley 1992). In 1996, the Centers for
Disease Control recommended the BCG vaccine be used only for health workers
in whom there was a high likelihood of multiple drug-resistant (MDR) TB. The
incidence of the disease has increased quite dramatically throughout the last 15
years. This trend is directly related to immigrant communities who were not vac-
cinated in their country of origin, and also to the spread of AIDS.
One-third of the world’s population is infected with TB. Annual global
deaths are approximately one million, and TB is the leading cause of death due to
an infectious agent in the world (NIAID 2002). Recently, MDR TB has ap-
peared. Outbreaks have occurred in hospitals, correctional institutions, residen-
tial-care facilities, and homeless shelters. In the United States, several hundred
people have contracted TB at their workplace. TB has also caused concern in the
aviation industry as commercial pilots and crew have been infected by passengers
(WHO 1998).
Although there still are antibiotics to treat MDR TB, these medications are
expensive, have side effects, and are slowly becoming ineffective. MDR TB is
more difficult to treat than TB, as it requires expensive second-line drugs to be
taken for at least 18 months compared with cheaper, first-line drugs taken for
only 6 months in cases of TB. The cost of first-line treatment is approximately
$120 for a 6-month course. The cost of second-line treatment is approximately
$10,000 (Davies 2001).
Before the advent of para-aminosalicylic acid and isoniazid, patients with TB
were sent to sanatoriums, often located high in the mountains and frequently
close to pine forests, because it was thought that breathing mountain air laced
with pine essence would aid recuperation. Sanatorium windows contained no
panes of glass so air could flow freely through the facility.
There is no suggestion that aromatherapy should replace conventional treat-
ment for TB. However, essential oils can enhance a patient’s quality of life. Some
essential oils have been found effective against TB in vitro, and some have been
found to increase the potency of orthodox medicines. Valnet (1993) was one of the
370 Section II Clinical Use of Aromatherapy

first physicians to document the use of aromatherapy in the treatment of TB. He
found essential oil of hyssop neutralized the TB bacillus at a concentration of 0.2
parts per 1000 (Valnet 1993). This finding was similar to that of Hilal et al (1980).
Hilal found the volatile oil of hyssop was effective using different chromatograph
and spectral methods. Hyssop is eliminated through the lungs. Due to the high
percentage of the ketones iso-pinocamphone and pinocamphone (70%), this es-
sential oil should not be taken orally and many feel it is contraindicated in epilepsy.
It also has a pronounced hypertensive action (Valnet 1990). However, in view of
Valnet’s findings of hyssop’s effectiveness as such a very low percentage (0.002%),
hyssop could play a part in TB control if used in low dosages.
Despite the fact that most of the research on TB and essential oils has been
conducted on animals, there are a few papers that suggest essential oils might be
effective against TB in humans. A Russian paper reports the results of a 2-month
study on the effects of inhaled essential oils. The symptoms of 81.8%-95.6% pa-
tients disappeared, and their body masses increased (Petrosian et al 1999). Un-
fortunately, only the abstract is in English and the name of the essential oil is not
given. TB is rampant in Russian correctional facilities where a virulent, resistant
strain is endemic.
Lall and Meyer (1999) found that 14 out of 20 South African-plant ex-
tracts (extracted with acetone) were effective against isoniazid- and riampin-
resistant strains of TB at 0.5mg/ml using the agar-plate method. A further rapid-
radiometric method often used for drug susceptibility testing confirmed in-
hibitory activity. Eight of the plants showed activity against the resistant strain at
1.0mg/ml. One of the plants belonged to the Helichrysum genus (spp. melanacme),
although the other plants were unfamiliar. Gupta and Viswanathan (1955) re-
ported on the tuberculostatic activity of Occimum sanctum (Holy basil) and Piper
betle (betle juice). In a further paper they found that Occimum canum inhibited the
growth of TB in dilution of 1: 50,000 (Gupta & Viswanathan 1955a).
Kufferath and Mundualgo (1954) found Eucalyptus globulus enhanced the
activity of streptomycin, isoniazid, and sulfetrone in the treatment of TB
(Kufferath & Mundualgo 1954). Schaubelt (1994) wrote that Cupressus semper-
virens (cypress) and Pinus sylvestris (Scotch pine) are also effective against TB.
The essential oils should be diffused continuously over several months and
are best used in rotation. Steam inhalation and/or use of a nebulizer will help get
the essential oils deep into the lungs. Sputum tests will indicate if the infection is
being contained. Hopefully further in-vitro research will show that other essen-
tial oils also have TB activity, and these can be added to a general mix of four es-
sential oils. It might be helpful to add Lavandula angustifolia and/or tea tree to
enhance immune function. In addition, the patient should take steam inhalations
with four drops of the essential oil mix three times daily to get the essential oils
deep inside the lungs. Adding an antiinflammatory essential oil such as Helichry-
sum italicum, German chamomile, or frankincense will help soothe the mucous
membrane. Table 25-3 lists inhaled essential oils of use in the treatment of pul-
monary TB.
Chapter 25 Respiratory Care 371

REFERENCES
Abdel Wahab S, Adoutabl E, El-Zalabani S, et al. 1987. The essential oil of Olibanum.
Planta Medica. 53(4) 382-384.
Bardeau F. 1976. Use of essential aromatic oils to purify and deodorise the air. Le
Chirurgien-Dentiste de France. 46:53.
Belaiche P. 1979. Traite de Phytotherapie et d’Aromatherapie, Vol.1. Paris: Maloine SA.
Belaiche P. 1979a. Traite de Phytotherapie et d’Aromatherapie, Vol. 2. Paris: Maloine
SA.
Boyd E. 1954. Expectorants and respiratory tract fluid. Pharmacological Review.
6:521-542.
Boyd E, Sheppard E, Boyd C. 1967. The pharmacological basis of the expectorant action
of glyceryl guaiacolate. Applied Therapies. 9(1) 55-59.
Boyd E, Sheppard E. 1968. The effect of steam inhalation of volatile oils on the output
and composition of respiratory tract fluid. Journal of Pharmacology and Experimental
Therapeutics. 163(4) 250-256.
Boyd E, Sheppard P. 1970. Nutmeg and camphene as inhaled expectorants. Archives of
Otolaryngology (Chicago). 92:372-378.
Budavari S (ed). 1996. The Merck Index, 12th ed. Whitehouse Station, NJ: Merck &
Co Ltd.
Carson C, Cookson B, Farrelly H, et al. 1995. Susceptibility of MRSA to the essential
oil of Melaleuca alternifolia. Journal of Antimicrobial Chemotherapy. 35(3) 421-424.
Centers for Disease Control and Prevention. 1996. Notifiable diseases and deaths in se-
lected cities. Morbidity and Mortality Weekly Report. 45(4) 1-27.
www.cdc.gov/mmwr.
Charron J. 1997. Use of Lavandula latifolia as an expectorant. Journal of Alternative &
Complementary Medicine. 3(3) 211.
Cruz-Coke R. 1960. Environmental influences and arterial blood pressure. Lancet.
2(345) 295-296.
Davies P. 2001. Drug resistant tuberculosis. Journal of the Royal Society of Medicine.
94(6) 261-263.
Duke J. 1985. Handbook of Medicinal Herbs. Boca Raton, FL: CRC Press.
372 Section II Clinical Use of Aromatherapy
Table 25-3 h Inhaled Essential Oils to Use with Pulmonary TB
Botanical Name Common Name Reference
Blue gum Eucalyptus globulus Kufferath & Mundualgo 1954
Niaouli Melaleuca viridiflora Kufferath & Mundualgo 1954
Marjoram Origanum majorana Valnet 1993
Holy basil Occimum sanctum* Gupta & Viswanathan 1955
Hyssop Hyssopus officinalis Hilal et al 1978
Juniper Juniperus communis Duke 1985
* low doses; suggested amount below 0.5%

Falk A, Gullstrand E, Lof A. 1990. Liquid/air partition coefficients of four terpenes.
British Journal of Industrial Medicine. 47(1) 62-64.
Ferley J, Poutignat N, Mirou D. 1989. Prophylactic aromatherapy for supervening infec-
tions in patients with chronic bronchitis. Statistical evaluation conducted in clinics
against a placebo. Phytotherapy Research. 3(3) 97-100.
Filipsson A. 1996. Short term inhalation exposure to turpentine, toxicokinetics and acute
effects in men. Occupational and Environmental Medicine. 53(2) 100-105.
Grisk A, Fischer W. 1969. On the pulmonar excretion of cineole, menthol and thymol in
rats following rectal application. Zeitschrift fur Arztliche Fortbilding. 63(4) 233-236.
Gupta K, Viswanathan R. 1956. A short note on antitubercular substance from Occimum
sanctum. Antibiotics and Chemotherapy. 6(3) 247.
Gupta K, Viswanathan R. 1956a. Antitubercular substances from plants. Antibiotics and
Chemotherapy. 6(2) 194-195.
Kendig E, Chernick V (eds.). 1983. ed 4. Disorders of the Respiratory Tract in Children.
Philadelphia: WB Saunders.
Kufferath F, Mundualgo G. 1954. The activity of some preparations containing essential
oils in TB. Fitoterapia. 25:483-485.
Lall N, Meyer J. 1999. In vitro inhibition of drug-resistant and drug-sensitive strains of
Mycobacterium tuberculosis by ethnobotanically selected South African plants. Journal
of Ethnopharmacology. 66(3) 347-354.
Lockhart N. 2000. Inhalation of frankincense and its affect on asthmatics. Unpublished
dissertation. Hunter, N.Y.: R J Buckle Associates.
Lung and Asthma Information Agency. 1995. Factsheet. London: Department of Public
Health Sciences, St. George’s Hospital Medical School.
Machon L. 2001. Use of four essential oils in the treatment of sinus infections. Unpub-
lished dissertation. Hunter, N.Y.: R J Buckle Associates.
MacSween R, Whaley K (eds.). 1992. Muir’s Textbook of Pathology. London: Edward
Arnold.
Mattys H, de Mey C, Carls C, et al. 2000. Efficacy and tolerability of myrtol. Standard-
ized in acute bronchitis. A multi-centre, randomised, double-blind, placebo-controlled
parallel group clinical trial vs. cefuroxime and ambroxol. Arzneimittel-Forschung
Drug Research. 50(8) 700-711.
McFerran T. 1996. A Dictionary of Nursing, 2nd ed. Oxford, UK: Oxford University
Press.
Melis K, Bochner A, Hanssens G. 1989. Accidental nasal eucalyptol and menthol instil-
lation. European Journal of Pediatrics. 148(8) 786-788.
National Institute of Allergy and Infectious Diseases. 2002. One third of the world’s
population has tuberculosis bacterium. Oct., 2002. NIAID News, 2002. www.
hivandhepatitis.com.
Newman-Taylor A. 1995. Environmental determinants of asthma. Lancet. 345(8945)
296-299.
Petrosian F, L’vov S, Levchenko G. 1999. The methods of traditional medicine in the
treatment of tuberculosis. Voenno-Meditsinskii Zhurnal. 320(10) 45-48.
Pitcher L. 2001. The Effects of Mentha piperita on chronic upper respiratory symptoms
in adults. Unpublished dissertation. Hunter, N.Y.: R J Buckle Associates.
Rudansky R. 2000. Eucalyptus globulus and cystic fibrosis: a case-study. Unpublished dis-
sertation. Hunter, N.Y.: R J Buckle Associates.
Chapter 25 Respiratory Care 373

Schafer D, Schafer W. 1981. Pharmacological studies with an ointment containing men-
thol, camphene and essential oils for broncholytic and secretolytic effects. Arzneimit-
telforschung. 31(1) 82-86.
Schnaubelt K. 1993. Aromatherapy Course, Part 3. San Rafael, CA: Pacific Institute of
Aromatherapy.
Sheppard-Hanger S. 1995. The Aromatherapy Practitioner Reference Manual, Vol. 11.
Tampa, FL: Atlantic Institute of Aromatherapy.
Spear B. 1999. Essential oils and their effectiveness in the relief of symptoms of asthma.
Unpublished dissertation. Hunter, N.Y.: R J Buckle Associates.
Stevenson C. 1995. Aromatherapy. In Rankin-Box D (ed.), The Nurses’ Handbook of
Complementary Therapies. London: Churchill Livingstone, 52-58.
Suskind P. 1987. Perfume: The Story of a Murderer. London: Penguin Books.
Valnet J. 1990. The Practice of Aromatherapy. Saffron Walden, UK: CW Daniels.
Varga E, Hajdu Z, Veres K, et al. 1998. Investigation of variation of the production of
biological and chemical compounds of Hyssopus officinalis L. Acta Pharm Hung
May. 68(3) 183-188.
Wagner T. 1999. Looking to make death a little less painful. Times Union. B1.
Weil A. 1997. Breathing Easier with Asthma. Dr. Andrew Weil’s Self-Healing. 6-7.
Wilmers K, Grobel W. 1990. Chemometric evaluation of GC/MS profiles for the detec-
tion of g-irradiated spices as exemplified by nutmeg. Deutsch Lebensen. Rundsch. 86:
344-348.
World Health Organization. 2002. Tuberculosis and air travel: guidelines for prevention
and control. Oct. 2002 WHO Press Release, 1998. www.who.int/inf.pr.
374 Section II Clinical Use of Aromatherapy

W
375
Appendix I
Education
M
ost aromatherapy courses on the market are intended for the lay public
and have a recreational or esthetic approach, such as making perfumes,
soaps, or cosmetics, or the aromatic content of the science of food addi-
tives. While these courses are interesting, they are not relevant to clinical practice.
Certification
Certification can mean one of two things: the student has attended a course (al-
though he or she may not have learned anything) or the student has attended a
course and passed the required examination.
The term certified usually implies a student has passed the required examina-
tion and is therefore, in the mind of the certifying body (which may or may not
be the school that set the examination), competent in that subject. A certified per-
son is often described as licensed to use that training, as in the case of a certified
lawyer or accountant. However, in the field of aromatherapy, there is no licensing
body either in the United States or United Kingdom that can license an aro-
matherapist. The closest thing in the United Kingdom is a self-regulating body
called the Aromatherapy Organization Council (AOC), which sets a core cur-
riculum for aromatherapy training for lay people.
Choices of Training
There are three types of aromatherapy training: professional, academic, or within
a specific discipline such as nursing. Any of these courses could have an esthetic
or clinical focus.
Professional
National Association for Holistic Aromatherapy
The National Association for Holistic Aromatherapy (NAHA) is the largest
aromatherapy organization in the United States with just under 1000 members.
As NAHA is a membership organization, it cannot offer certification itself. How-
ever, NAHA does set guidelines for a national curriculum and approves schools

and educational programs that heed these guidelines. A list of NAHA-
approved schools and programs can be obtained from their Web site: www.naha.org.
NAHA-approved training is divided into Level One and Level Two. Level
One requires 30 hours of training and covers a minimum of 10 essential oils. Level
Two requires 200 hours of training, but the number of essential oils to be covered
is not stated. Level Two also includes “the clinical science of at least five common
ailments for each system covered.” The systems listed are reproductive, circulatory,
nervous, endocrine, lymphatic, musculoskeletal, and digestive. Students must write
a 5-10 page research paper, complete 10 case histories, and pass an examination of-
fered by the school. NAHA does not inspect schools or approve the exam.
Aromatherapy Registration Council
The Aromatherapy Registration Council (ARC), a not-for-profit organization in
the United States, was set up in 2000 to mirror the work of the AOC in England.
The ARC has a curriculum and national examination. The exam is held four
times a year in different locations and is run by the Professional Testing Corpo-
ration (PTC). The curriculum content is available from the PTC. Areas covered
on the examination are given as follows: 20% basic concepts of aromatherapy, 30%
scientific principles, 35% administration, and 15% professional issues. There are
no prerequisites to the examination but “a completion in a program of aro-
matherapy or one year of full-time experience in aromatherapy is recommended.”
For more information, see www.aromatherapycouncil.org.
PTC runs certification tests for different modalities. For information on the
PTC, please see their Web site: www.ptcny.com. At the time of writing, the aro-
matherapy exam does not involve any specific clinical questions because the exam
is open to lay people. I am an active and supportive member of ARC and helped
set the ARC exam. It is hoped that in time the exam will include an optional clin-
ical section specifically for licensed health professionals.
Academic Training
University Programs
Academic credit is given for some aromatherapy courses. One credit is equivalent
to 11-15 hours of class at a particular level. The level at which the learning occurs
will also be taken into account (undergraduate versus postgraduate) and will be
reflected in the cost of each credit. Some aromatherapy courses are in the process
of being accredited by a university. My own course, Aromatherapy for Health
Professionals, is at the time of writing this book (2002) in the accreditation
process. Several universities are beginning to look at creating aromatherapy pro-
grams. Academic training may concentrate on theory or research review and have
wonderful library access, but unless the instructors are clinicians with years of ex-
perience and the students are given sufficient hands-on training, academic courses
may not produce clinically qualified practitioners. The curriculum may or may not
conform to ARC guidelines. Look for a well-rounded course with lots of hands-
on practice directed by experienced instructors. An added bonus in a university
program is the chance to carry out research.
376 Appendix I Education

The University of Minnesota began a four-credit program in 2001 aimed at
“providing foundational knowledge in therapeutic uses of essential oils for health
science students and professionals, including skills in critiquing the aromatherapy
research literature. The focus is on 33 specific essential oils as well as general prin-
ciples and chemistry.” This is a Web-based course sequence with 2 days each se-
mester on campus. Grading criteria include participation (including online dis-
cussion assignments), a written exam, case studies, and a report on an essential oil.
Other universities that offer aromatherapy courses include Washington State
University, University of Indiana, The College of New Rochelle, Bastyr Univer-
sity, and New York University.
State-Approved Schools
While it is encouraging that some schools teaching aromatherapy are state ap-
proved, this does not mean the content of the aromatherapy courses taught at that
school is approved. State approval usually only means the school complies with
regulations regarding safety and insurance.
Distance Learning
Discussing theory and analyzing research is excellent, but practical experience is
irreplaceable—particularly with a therapy that involves smell and touch. However,
distance-learning courses are an excellent way to begin and acquire base knowledge,
and I have created a short home-study and on-line course myself (www.rjbuckle.com).
Education within a Specific Discipline (relevant to licensed
health-care professionals)
Courses are being set up in complementary medicine for many health-care disci-
plines. These may or may not include separate training in aromatherapy.
Clinical Competency
To show clinical competency, licensed health professionals need to have com-
pleted an educational program recognized by their licensing body. Ideally, this
should involve a course endorsed by a professional body or that at least gives
continuing-education units (CEUs) for their professional modality.
Testing should be via a method that demonstrates clinical competency. Because
clinical competency is involved, the instructor should be someone recognized as a
health professional. To ensure fair and objective marking, the examination or test-
ing should involve someone other than the person who taught the course.
Endorsed Programs
This means that the course content has been approved by an external accrediting
body such as the American Holistic Nurses Association. One example is my
course, which is a 250-hour CEU program endorsed by the American Holistic
Nurses Association. For details on training in United States, Australia, Korea, and
Japan, please visit www.rjbuckle.com, which is listed in resources. Training in
South America, Korea, and Australia is expected to start in 2004.
Appendix I Education 377

Approved Providers
An approved provider means that the educational organization creating the aro-
matherapy course is approved by an accrediting body to give CEUs to physicians,
nurses, massage therapists, pharmacists, and so on. One CEU is equivalent to 50
minutes of classroom teaching. There are several training programs that provide
nursing or massage therapy CEUs, such as The Institute of Integrative Aro-
matherapy, The Institute of Dynamic Aromatherapy, The Atlantic Institute of
Aromatherapy, The Pacific Institute of Aromatherapy, The Australasian College
of Aromatherapy, and my company, R J Buckle Associates, among others. Some
hospital groups approve specific educational providers to teach aromatherapy to
their employees. R J Buckle Associates is an approved educational provider to the
Planetree Hospital Group.
Specific Training for Nurses
The Royal College of Nursing (RCN) in England issued guidelines for nurses
wanting to use aromatherapy. These state that a nurse “should know his/her sub-
ject and have received training.” There is no requirement that the aromatherapy
course should be nursing based. However, if aromatherapy is to be used to en-
hance nursing, the instruction probably should be clinically based and nurse cen-
tered. Nurses in the United Kingdom who use aromatherapy are part of nursing
care are covered under RCN insurance for up to £3 million. To date, no claims
have been made.
The guidelines for using aromatherapy issued by the RCN include the fol-
lowing:
• Supervised practice;
• Anatomy, physiology, pathology, and pharmacology;
• Practical and theoretical examination;
• Holistic approach;
• Supervised clinical practice;
• Counseling/communication and self-development skills training;
• Appropriately qualified teachers;
• Support for the trainee therapist;
• A sensible tutor/pupil ratio (Royal College of Nursing 1993).
REFERENCES
Royal College of Nursing. 1993. Choosing a complementary therapy. London: Comple-
mentary Therapies in Nursing Special Interest Group, Royal College of Nursing De-
partment of Nursing Policy and Practice.
378 Appendix I Education

379
W
Appendix II
Policies, Protocols,
and the Occupational
Safety and Health
Administration (OSHA)
Sample Hospital Patient Care Policy and Procedure
Most health facilities require a health-safety policy in place. If aromatherapy is to
be integrated into a facility, this is the first thing that needs to happen. I am ap-
preciative of the hospitals that worked with me to create policies and protocols
and to those facilities that shared their documentation with me.
Purpose
To outline the management of patients receiving aromatherapy treatment.
Definitions
Clinical aromatherapy is the controlled use of essential oils to enhance health
and well being, which targets a specific symptoms.
Topical application refers to the “m” technique, light massage, a compress
with water, carrier oil, or gel (spore or bacteria free) on cotton squares directly
over the affected area, or a bath (hand, foot, sitz, or full).
Inhalation can be indirect or direct, differentiated as follows:
• Direct inhalation means applying two to five drops of essential oil to a tissue
and breathing normally for up to 15 minutes, applying two to five drops of es-
sential oil on a cotton ball placed under the pillowcase, or floating two to five
drops of essential oil on a bowl of hot water and inhaling the aroma for up to
10 minutes. Patients should remove spectacles and keep eyes closed.
• Indirect inhalation means using an electric nebulizer or battery-operated dif-
fuser to diffuse fine particles of essential oil within a room.
Carrier oil is a cold-pressed vegetable oil. The most frequently used is sweet
almond oil. Carrier oils have specific properties. Culinary oils are not suitable.

Patch testing is the process used to determine if a person is sensitive to po-
tential allergens in an essential oil. Two drops of the mixture at double the con-
centration to be used are put on an adhesive bandage, attached to the patient’s up-
per arm, and left for 12 hours.
Goals
• To promote a sense of well being
• To promote relaxation and reduction of stress
• To reduce or alleviate physical, emotional or spiritual symptoms
Indications
• Stress and related disorders
• Anxiety, depression, sadness, grief, anger
• Insomnia
• Digestive disorders, cramping, nausea
• Pain
• Muscular problems
• Inflammation
• Infection
• Mental agitation
• Premenstrual syndrome, menopausal problems
• Slow wound healing
Contraindications
• Use with caution in pregnancy, epilepsy, hypertension, estrogen-dependent tu-
mors, and patients with sensitivities and allergies.
Policy
• Essential oils should be used in a clinical setting by a licensed health profes-
sional trained in the use of essential oils. Such training should be clinical and
should be acceptable to the establishment where the health professional works.
Such training should cover safety precautions, potential side effects, and con-
traindications related to the use of each essential oil (see Table A2-2 and Box
A2-2).
• Treatments should be offered after consultation with the patient and after re-
ceiving their verbal consent or that of their family when applicable.
• Aromatherapy does not require medical order except for perceived prescriptive
use. Nurses need to check with their Board of Nursing (see Chapter 6).
• Treatment will vary according to each patient and his or her needs (see Table
A2-1).
• Essential oils used should be limited to the attached list (see Table A2-3).
• Full botanical name will be used.
• Aromatherapy will be offered in addition to conventional treatments.
• The dignity of the patient will be respected at all times.
380 Appendix II Policies, Protocols, and OSHA

• A Material Safety Data Sheet (MSDS) and Gas Chromatography/Mass Spec-
trometry (GCMS) is available for each essential oil used (see Box A2-1).
A health professional using aromatherapy as part of patient care will do the
following.
• Check with patients about skin reactions to nuts, essential oils, perfumes, cos-
metics, or pharmaceuticals
• Know how to take a proper case history to decide if the patient has a condition
or is taking a drug that might contraindicate specific essential oils
• Know how to perform a patch test and use this in appropriate cases
• Ensure all undiluted essential oils (singles or mixtures) used by patients are ad-
equately labeled and in bottles with integrated drop dispensers
• Advise patients not to ingest essential oils (except as part of specified treatment
given by a person with prescription authority)
• Have sufficient knowledge of clinical practice to know when to avoid a partic-
ular procedure and when to obtain further medical assistance
Appendix II Policies, Protocols, and OSHA 381
Table A2-1 h Sample Protocol and Policy
Procedure Important Points
Assess patient
Obtain history, including allergies,
medications, skin integrity, and liked
and disliked aromas.
Explain the procedure.
Select essential oil and identify
method to be used. Advise about
photosensitivity when relevant.
Ensure patient privacy. Provide
treatment.
If a skin reaction occurs, remove
essential oil with milk or carrier oil,
wash the area with unscented soap
and water, pat dry, and leave in open
air for 10 minutes.
Evaluate the patient’s response and
document the treatment in the
medical records.
Be aware of patient sensitivities: see
safety guidelines.
Provide information about aro-
matherapy.
Effects of inhalation are rapid; topical
action is slower. Choice to be deter-
mined by patient’s condition and tar-
geted outcome.
Be sensitive about others in the room.
Complete an occurrence report and
notify the appropriate staff. Provide
follow-up care.
Documentation includes assessment,
choice of essential oil, method, and
outcome.

Practitioner Safety
Practitioner safety measures should include the following.
• Maintain good ventilation in treatment areas.
• Air the treatment room between treatment sessions.
• Wash hands before and after patient contact.
• Take a minimum of 5 minutes to breathe fresh air after each treatment.
An algorithm can be a simple and clear way to explain a thought process.
Please see Fig. A2-1 for an algorithm exploring the use of lavender as a sleep aid.
382 Appendix II Policies, Protocols, and OSHA
BOX A2-1 Sample Material Safety Data Sheet (MSDS)
Individual Safety Data Form for Specific Essential Oil
HP’s name Patient’s name Date Time
Florence Nightingale John Doe 11/11/96 3 p.m.
Essential oil: Melaleuca alternifolia CT terpineol
Number of drops: 1-5
Known Hazards Risks
Xn: Cat 3 carcinogen R10/22/38
LD
50
190 mg/kg Flammable, harmful if swallowed, not
irritating to the skin
Safety Other safety data
S24/25 No sensitization (Ford 1988)
Avoid contact with skin and eyes No phototoxicity (Ford 1988)
Nonirritant
Emergency Treatment:
• If swallowed, drink full-cream milk and seek medical attention.
• If in eye, irrigate with vegetable oils or full-cream milk followed by water,
then seek medical attention
Application Method Contraindications Precautions
Topical, inhalation — Avoid using teatree with high
1,8-cineole content
Other Information:
• Can be used neat on insect bites/stings/zits
• Can be used in gargle and mouthwash (1–2 drops)
• Can be used vaginally diluted in carrier oil
• Insoluble in water: dissolve in alcohol/milk
• Ensure correct chemotype low cineole. Cineole can be a mucous-
membrane irritant.
Sources: AMA Council on Medical Service Report “Growing Nursing Shortage in the
USA.” South Florida Business Journal; California Nurses Association

Appendix II Policies, Protocols, and OSHA 383
Table A2-2 h Accident Procedures
Problem Answer
Essential oil in the eye Irrigate the eye with milk or carrier oil, then
with water. Keep the bottle to show which
essential oil was being used. Seek medical as-
sistance.
Used an undiluted essential oil Dilute with carrier oil, then wash with non-
(high phenols), skin burned perfumed soap and water and dry. Seek med-
ical assistance.
5 ml (or more) essential oil Give milk to drink, and keep the bottle.
taken orally Seek medical assistance. Essential oils, when
taken in amounts greater than 5 ml by
mouth, should be treated as poisons.
Bottle of essential oil dropped Use a paper towel to soak up essential oil and
and broken, essential oil and collect the glass. Put mixture in more paper.
glass on floor Dispose in double-sealed plastic bag.
BOX A2-2 General Safety
Storage
All essential oils should be stored as follows:
• Locked up
• Out of reach of children
• In a cool place
• In tightly closed containers
• Away from food, drink, or animal feed
• Away from heat
• Away from naked flames
Labeling
All bottles containing essential oils should be clearly marked with indelible
labels that include the following:
• Full botanical name
• Relevant safety information
• Quantity of oil
• Company name and address
Packaging
• All essential oils should be packaged in colored glass bottles that include
an integral dropper of standard (20 drops per ml) size.
Continued

384 Appendix II Policies, Protocols, and OSHA
BOX A2-2 General Safety—cont’d
Procedures
• Essential oils should only be used in a clinical setting by a member of the
staff or an outside contractor qualified in aromatherapy and who has per-
mission to use them.
• Whenever possible, essential oils should be used in enclosed areas to pre-
vent the aromas from spreading.
• All essential oils used should be documented in the patient-care plan.
• The positive and negative effects of essential oils should be evaluated and
noted.
• Use topically in 1%-5% dilution, except in specific situations as recom-
mended by safety guides.
• When used in a bath with the elderly or small children, essential oils
should be dissolved in a small amount of milk to avoid possible corneal
damage during splashing.
• Essential oils that carry a high risk should be avoided. They are listed in
safety guides (Tisseland, Balass 1995). A suggested list of safe oils can be
found in Table A2-3.
Clothing
• No special clothing is required, but some essential oils such as German
chamomile may leave stains.
Disposal
Essential oils are highly flammable and carry intense aromas. They should be
disposed of in a sealed, polythene bag.
Table A2-3 h Some Essential Oils Suitable for a Clinical Setting
Common Name Botanical Name
Yarrow Achillea millefolium
Angelica Angelica archangelica (root)
Frankincense Boswellia carteri
Ylang ylang Cananga odorata
Roman chamomile Chamomelum nobile
Bergamot Citrus bergamia
Mandarin Citrus reticulata
Neroli Citrus aurantium var. amara flos
Petitgrain Citrus aurantium var. amara fol
Myrrh Commiphora myrrha

Appendix II Policies, Protocols, and OSHA 385
Table A2-3 h Some Essential Oils Suitable for a Clinical Setting—cont’d
Common Name Botanical Name
Cypress Cupressus sempervirens
Palma rosa Cymbopogon martini var. motia
Lemongrass Cymbopogon citratus
Blue gum Eucalyptus globulus
Gully gum Eucalytpus smithi
Lemon gum Eucalyptus citriodora
Fennel Foeniculum vulgare
Everlasting flower Helichrysum italicum
Juniper Juniperus communis
True lavender Lavandula officinalis
Spike lavender Lavandula latifolia
Lavandin Lavandula hybrida CT grosso
German chamomile Matricaria recutita
Tea tree Melaleuca alternifolia
Melissa Melissa officinalis
Peppermint Mentha piperita
Basil Ocimum basilicum (European)
Marjoram Origanum majorana
Geranium Pelargonium graveolens
Black pepper Piper nigrum
Rose Rosa damascena
Rosemary Rosmarinus officinalis
Clary sage Salvia sclarea
Sandalwood Santalum album
Clove bud (only use diluted) Syzygium aromaticum
Thyme Thymus vulgaris CT linalol
Vetiver Vetiveria zizanioides
Ginger Zingiber officinale

Client Complaint: Sleeping Problem
Perform history and physical examination
(Rule out and treat contributing causes, such as pain, GI upset,
psychiatric conditions, medication interactions, and poor sleep
habits. Rule out and treat medical conditions).
Persistent sleep problem
(psychotropic medication usually considered here)
Discuss traditional
treatments
Client allergy or dislike
of lavender oil?
Would client consider aromatherapy via inhalation?
Yes No
Institute aromatherapy and sleep educationConsider alternative
essential oils or
traditional treatments
Provide client with sleep diary
Reevaluate client sleep
and review sleep diary
Sleep improved?
Begin treatment: One drop of essential oil of
lavender at bedtime, placed on pillow case
or on cotton ball then placed in pillow case
Yes No
Reevaluate: history and physical exam;
contributing factors of sleep problems;
correct use of lavender oil
Continue aromatherapy
as needed and continue
to evaluate sleep
Consider continued aromatherapy trial
or discuss traditional treatments
Yes No
Figure A2-1 Nonpharmacological Approach to Sleep Problems in the Elderly. Kindly
supplied by Sherry Simpson (2001).

Regulations and Health
In the United States, the two most important groups of regulations aromatherapy
needs to address are those proposed by OSHA and JCAHO. For more informa-
tion about JCAHO, see their Web site at www.jcaho.com. The most interesting
part of the site for aromatherapy is the section on mind/body, spirituality, cultural,
and psychosocial needs of patients.
OSHA is concerned with the transport, storage, and spillage of quantities of
hazardous material. Essential oils fall into this category, particularly in large
amounts. OSHA requirements go well beyond those normally required for aro-
matherapy use. However they are presented here in the unlikely event they might
be needed. The people most likely to use this chapter are those preparing the
MSDS for various essential oils.
The latest information on OSHA can be obtained from their Web site:
www.osha.gov. A wide variety of materials including standards, interpretations,
directives, and more can be purchased on a CD-ROM from the US Government
Printing Office. To order, apply to
Superintendent of Documents
PO Box 371954
Pittsburgh, PA 15250-7954.
OSHA is divided into 10 regions. OSHA requires that MSDS be completed
for any substance used on or with the public. Their toll-free compliance-
assistance number is 1-800-321-OSHA(6742) or (202) 693-2100. Alternatively,
a contact number may be sent to OSHA and their Compliance Assistance Phone
Service will contact you, if you are located in the United States. To send a day-
time contact number, forward your message to [email protected].
A formal letter describing the particulars of the workplace and question also
can be mailed to:
Department of Labor—OSHA
200 Constitution Avenue NW
Room N3603
Washington, DC 20210
OSHA
OSHA was created for the following purposes.
• Encourage employers and employees to reduce workplace hazards and to
implement new, or improve existing, safety and health programs
• Provide for research in occupational safety and health to develop innova-
tive ways of dealing with occupational safety and health problems
• Establish “separate but dependent responsibilities and rights” for employ-
ers and employees for the achievement of better safety and health condi-
tions
• Maintain a reporting and recordkeeping system to monitor job-related in-
juries and illnesses
Appendix II Policies, Protocols, and OSHA 387

• Establish training programs to increase the number and competence of oc-
cupational safety and health personnel
• Develop mandatory job safety and health standards and enforce them ef-
fectively
• Provide for the development, analysis, evaluation, and approval of state oc-
cupational safety and health programs.
OSHA does not cover self-employed people, farms that only employ family
members, or working conditions regulated by other federal agencies. OSHA is
concerned with safety and risk management of potentially hazardous substances
in the workplace. Hazardous substances include essential oils, as they are flam-
mable and in some cases are skin irritants or sensitizing. The object of OSHA for
aromatherapy is to assess and evaluate risk, thereby reducing the possibility of
harm for those using essential oils either directly or indirectly. Risk and safety
phrases to be used are listed in the material safety data sheet (MSDS). By stan-
dardizing them in this way, anyone looking at an OSHA document on an essen-
tial oil will immediately recognize its potential risk. MSDSs are required by
OSHA. Some parts of the documentation may help health professionals and
health administrators make an informed judgment about the safety of each es-
sential oil in a clinical setting. However, much of the data involves estimates, not
actual exact evidence.
OSHA assessment requires the person wanting to use essential oils to be
aware of any potential hazards and risks involved. Essential oils that are defined
as dangerous (corrosive, irritant, or toxic), need to be clearly identified as to the
maximum exposure limit and the occupational exposure limit of any given essen-
tial oil. This will indicate the toxicity of an essential oil. Toxicity is measured by
the oral dose needed to kill 50% of experimental animals (LD
50
). It is expressed
in milligrams per kilogram of body weight (mg/kg). The dose needed to kill 50%
of experimental animals when taken other than orally is the lethal concentra-
tion(LC
50
). Degrees of toxicity are listed in Table A2-4.
Essential oils are classified simply with a T (for toxic) hazard sign. An essen-
tial oil classified in this way will also have specific risk phrases on its labeling such
388 Appendix II Policies, Protocols, and OSHA
Table A2-4 h Degrees of Toxicity
Extremely toxic Up to 1 mg
Highly toxic 1-50 mg
Moderately toxic 50-500 mg
Slightly toxic 0.5-5 g
Virtually nontoxic 5-15 g
Relatively harmless Up to 15 g

as “toxic if inhaled, toxic if swallowed, toxic if in contact with the skin,” or “harm-
ful if inhaled, harmful if swallowed, harmful if in contact with the skin,” and spe-
cific safety phrases. Lists of essential oil classifications/guidelines are available
that grade essential oils by giving them hazard symbols and acceptable risk (R)
and safety (S) phrases. Some essential oils, such as cedarwood, clary sage, and
geranium, have no hazard symbol or R and S number. Some, like grapefruit and
lemongrass, have no hazard symbol and no safety phrase but carry a risk phrase
such as R10, which means flammable, or R38, which means irritating to the skin.
An MSDS identifies potential hazards of transporting and storing essential oils
and is intended to warn people of any risk factors. It will include the features
listed in Box A2-3. A list of organizations that give registration numbers is in
Table A2-5.
Essential oil product identification includes the plant material, physical con-
stants, registrations (usually in the form of numbers), and safety and toxicity con-
siderations such as the flash point (the temperature at which an essential oil will
ignite). This information should be available from the essential-oil dealer. Sam-
ple MSDS is shown in Box A2-4.
Flavor and Extracts Manufacturers Association
The Flavor and Extracts Manufacturers Association (FEMA), the oldest and
largest national association of the flavor industry, produces many data sheets
on essential oils (as well as flavor data sheets). They can be obtained in sets. The
Appendix II Policies, Protocols, and OSHA 389
BOX A2-3 Information Found on Material Safety Data Sheets
(MSDSs)
1. Identification of the substance/preparation and company
2. Composition/information on ingredients
3. Hazards identification
4. First-aid measures
5. Fire-fighting measures
6. Accidental-releases measures
7. Handling and storage
8. Exposure controls/personal protection
9. Physical and chemical properties
10. Stability and reactivity
11. Toxicologic information
12. Ecologic information
13. Disposal considerations
14. Transport information
15. Regulatory information
16. Other information

BOX A2-4 Sample Material Safety Data Sheet (MSDS)
for Tea Tree
Product Identification
Name Tea tree
Botanical name Melaleuca alternifolia
Chemotype Terpineol
FEMA number
CAS number 68647-73-4
Extraction Steam distillation of the leaves
Specifications
Odor Fresh, eucalyptus type, herbaceous, antiseptic
Origin Australia
Appearance Clear to faintly yellow
Analytical Data
(1) Physical constants Specific gravity: 0.895–0.905 g
Optical rotation: @ 20°C 6.59.5
Refractive index: @ 20°C 1.476 to 1.481
Solubility: 1 vol of oil in 0.75 vol of 85% ethanol
(2) Chemical composition See GLC
Toxicity
Low cineole content 6% (as used for medicinal and dental purposes) re-
ported to be nonirritant. LD
50
400 mg (Ford 1988)
Flash Point
57–61°C
Table A2-5 h Organizations that Give Registration Numbers
CAS Chemical Abstracts Service
EINECS European Inventory of Existing Chemical Substances
FEMA Flavor and Extracts Manufacturers Association
IFRA International Fragrance Association
RIFM Research Institute for Fragrance Materials
CTFA Cosmetic Toiletry and Fragrance Association
INCI International Nomenclature of Cosmetic Ingredients
EFFA European Flavor and Fragrance Association
IOFI International Organization of the Flavor Industry
FDA Food and Drug Administration
AIS Association Internationale de la Savonnerie et de la Detergence
USES Uniform System for the Evaluation of Substances

Research Institute for Fragrance Materials (RIFM) was established in 1966 and
is a not-for-profit. The expert panel is independent of any manufacturing inter-
ests. RIFM collects and researches raw perfumery materials. The information is
submitted to the International Fragrance Association (IFRA) (established in
1973). The IFRA produces guidelines for individual fragrance ingredients and is
involved in risk management. IFRA publishes a “banned list” of 50 substances,
and a further 58 have limitations for use. Some essential oils have many more
regulatory numbers. Other important fragrance organizations are in Table
A2-6. Opdyke’s monographs on fragrance raw materials (1978) are also a good
source of information.
Risk phrases give an indication as to how flammable an essential oil may be,
if it is harmful when swallowed, if there is a risk of eye damage, if it may cause
birth defects, etc. Safety phrases provide an indication of how to store the oil and
dispose of it and what it will mix with. Both phrases are expressed as numbers.
Mandarin has risk phrase number R10 (flammable) and safety phrase number S3
(keep in a cool place). R65 relates to the potential of a substance to cause lung
damage after swallowing and is concerned with substances that contain more
than 10% of aliphatic, alicylic, or aromatic hydrocarbons. This is a relatively new
risk hazard that only came into being in May 1988. An example of the different
numbers given to one essential oil is in Table A2-7.
Some essential oils are not on the list of any of the fragrance organizations
mentioned. Ravensara is one such example. When an essential oil is not listed, it
should be possible to evaluate its risk and safety issues based on the chemical
components within the essential oil. Therefore the simplest thing is to look them
Appendix II Policies, Protocols, and OSHA 391
Table A2-6
h Other Important Organizations within the Fragrance
Industry
IFEAT International Federation of Essential Oils & Aroma Trades
COLIPA The European Cosmetic, Toiletry and Perfumery Association
NAFFS National Association of Flavors and Food-Ingredient Systems
FF Fragrance Foundation
Table A2-7 h Example: Citrus reticulata blanco Regulatory Numbers
REFM 250
FEMA 2657 (GRAS)
FDA 182.20
CAS 8008-31-9

up in a phytochemical database or a reference book such as Essential Oil Safety.
(Tisserand & Balacs 1995). While this section has gone into tremendous detail,
the important thing to remember is essential oils are safe when used correctly.
REFERENCES
Burfield T. 2001. Toxicity myths. www.aroma-science.com. Sept. 2002.
Ford R. 1988. Tea tree oil. Food and Chemical Toxicology. 26: 407.
Opdyke D. 1978. Monographs on fragrance raw materials. Food and Cosmetics Toxicol-
ogy. 16: 783-784.
Simpson S. 2001. Personal communication.
Tisserand R, Balacs T. 1995. Essential Oil Safety. London: Churchill Livingstone.
392 Appendix II Policies, Protocols, and OSHA

393
W
Appendix III
The White House Commission
on Complementary
Alternative Medicine Policy
T
he White House Commission on Complementary Alternative Medicine
Policy (WHCCAMP) was created on March 8, 2000, by executive order.
The 2-year commission will ultimately report to the president with leg-
islative and administrative recommendations to ensure US public policy will max-
imize the benefits of complementary and alternative medicine (CAM) (Gordon
2002). The commission includes 20 members who represent a diverse range of ex-
perts in biomedical, medical, and CAM fields. The chair, James Gordon, MD, is
helped by the following commissioners.
Bernier, George, MD Kerr, Charlotte, RSM, RN, MAC
Bresler, David, PhD Larson, Linnea, LCSW
Chappell, Thomas Low Dog, Tieraona, MD
Chow, Effie, PhD Ornish, Dean, MD
DeVries III, George Paz, Conchita, MD
Fair, William, MD Pizzorno, Joseph, MD
Fins, Joseph, MD Rolin, Buford
Guttierrez Veronica, DC Scott, Julia
Jonas, Wayne, MD Tian, Xiaoming, MD
Warren, Donald, DDS
The National Center for Complementary Alternative Medicine (NCCAM),
which is part of the National Institutes of Health (NIH), divides CAM is divided
into five categories. These categories are alternative medical systems, mind-body
interventions, energy therapies, manipulative and body-based methods, and bio-
logically based treatments (see Table A3-1).
Testimony indicated that coverage of CAM had been included by some em-
ployer-sponsored health plans as a direct response to employee requests. The
commission held meetings in Washington DC, Seattle, San Francisco, New York,
and Minneapolis, and spoke positively about encouraging rigorous research ($220
million was allocated for 2002).
The commission reported on four key areas:
1. Education and training of health care practitioners
2. Research to increase training of health care practitioners
3. Provision of health care professionals and the public with reliable infor-
mation
4. Guidance in appropriate access to and delivery of CAM
The report was filed after 14 meetings lasting over 18 months, in which sub-
missions were heard from 1700 people and organizations from groups as diverse
as the National Heart Lung and Blood Institute, the National Cancer Institute,
the Food and Drug Administration, Blue Cross/Blue Shield, and the Journal of
the American Medical Association, as well as many CAM practitioners and their
organizations. It has 29 recommendations and 100 action items—too many to list
here. But the response to the commission’s recommendation by Dr Tieraona Low
Dog MD and Joseph Fin MD is available at www.whccamp.hhs.gov/sfc.html.
Nurse Practice Acts
While the use of complementary therapies, including aromatherapy, has increased in
the last few years, there is little reference in any published articles to the state prac-
tice laws and how they impact the professional use of CAM. However, licensure laws
do affect the use of CAM. Sparber (2001) reports on a study of state Boards of Nurs-
ing (BON) policy conducted for WHCCAMP, the National Center for Comple-
mentary Alternative Medicine, and the Health and Human Services Bureau of
Health Professions. The study found that liberalization of licensure laws to practice
CAM has been associated with a significantly increased use by physician and non-
physician CAM providers. CAM was viewed as representative of the “integrative na-
ture of nursing practice rather than as an alternative method of care.”The report sug-
gests nurses are in a unique position to bridge the gap between orthodox, Western
health care and CAM.
394 Appendix III The White House Commission
Table A3-1 h Categories of Complementary Alternative Medicine
Alternative Medical Systems: Acupressure, biologically based therapies, orien-
tal massage, diet and nutrition (not herbs)
Mind-Body Interventions: Art, biofeedback, focused breathing, holistic nurs-
ing, humor, meditation, music, visual imagery, yoga
Manipulative and Body-Based Systems: Aromatherapy, cranial-sacral, deep-
muscle massage, effleurage, Esalen, feldencras, friction, Heller work, infant mas-
sage, Lomilorri, lymphatic drainage, myofascial, neuromuscular, petrissage, re-
flexology, shiatsu, structural integration, Swedish massage
Energy Therapies: Healing touch, Reiki, therapeutic touch
Biologically Based Systems: Herbs

The Louisiana BON www.lsbn.state.la.us defines CAM as a “broad domain
of healing resources that allow registered nurses to promote and/or enhance care
supportive to or restorative of live and well being.” Sparber (2001) has written an
important document that clarifies the situation for many nurses. BONs are re-
quired to monitor the scope of practice issues and protect the public through li-
censure and practice acts. Employers also have a role in safe practice. Anecdotal
reports indicate that although some nurses may consider certain complementary
therapies to be questionable, professional nurses who use these therapies report
their patients do experience an “increased level of comfort and well being”(Spar-
ber 2001). The fifth WHCCAMP category was not included in the article as it
is concerned with the prescriptive authority for herbal and other natural products.
However, some boards did have recommendations for advanced nursing practice.
At the time of writing, 47% of BONs had taken a position that allows nurses
to practice a range of complementary therapies. Thirteen percent were in the
process of deciding on their policy, and 40%, although they did not have any for-
mal policy, did not discourage nurses from using complementary therapies as part
of their care (Table A3-2). Some states, noticeably Minnesota, have recently
passed policies that cover the use of CAM by nonlicensed health professionals
(www.minnesotanatucalhealth.org). Sturn and Unutzer (2001) write that the exis-
tence of a practice act that gives nonphysicians specific rights to deliver CAM is
likely to increase the supply of persons practicing CAM.
The first state BON to issue a formal statement on CAM was Arizona (1991).
This BON states that a nurse may hold dual professional licensure/certification, but
the nurse will be held to the standard of the highest nursing credential he or she
holds. “A professional, practical or advanced practitioner who has acquired or de-
veloped a specialized knowledge base in complementary therapies will be held to
the standard of care for the nursing credential” (www.azboardofnursing.org). Ken-
tucky followed in 1996, after several inquiries from nurses wanting to know if
they could use their complementary-therapy skills to enhance nursing care
(www.kbn.state.ky.us). In 1997, Massachusetts (www.state.ma.us/reg/boards/rn)
and Pennsylvania (www.dos.state.pa.us) made general-position statements describ-
ing complementary therapies as being “within the scope of nursing practice” but
noting that “the nurse had responsibility for safe practice.”
Most BONs agree that the very nature of nursing lends itself to a framework
that welcomes these noninvasive, complementary practices, and that much of the
thinking behind nursing is similar to that underlying complementary therapies
(Sparber 2001). What has come out of the WHCCAMP report is the need for
documented training that clearly shows skills, knowledge, and competency in a
CAM discipline. Credentialing is recommended to ensure safe practice and to in-
dicate to other health professionals that nurses have learned another discipline. It
is suggested that nurses do not use titles such as “nurse massage therapist” unless
they are certified in massage. However, some states disagree with this. The New
York BON says nurses “cannot hold themselves out to be nurse reflexologists—
but they can say that reflexology is a service included as part of their overall
care” (O’Brien 2001). New York requires nurses who wish to use CAM to have
Appendix III The White House Commission 395

Board of Nursing is Deliberating Practice of CAM
Delaware
District of Columbia
Georgia
“received special training or education in this area and have received a certificate
of competency” (O’Brien 2001). The Oregon BON has stated that “complemen-
tary therapies fit within the definition of the practice of nursing” (Amdell-
Thompson 2001). For up-to-date information on all State Boards of Nursing, see
the web site of the National Council of State Boards of Nursing (www.ncsbn.org/
public/regulation/boards_of_nursing_board.htm).
According to the WHCCAMP report, aromatherapy is accepted as part
of nursing care in over half the states in the United States. What is also clear is
that while there are many types of touch, there only appears to be one kind of
aromatherapy, and that is the one associated with topical applications. This is a little
strange as much of the psychological impact of essential oils will be from inhalation.
396 Appendix III The White House Commission
Table A3-2 h CAM Policies of Individual US States and Territories
Board of Nursing Has Issued Statement Permitting Practice of CAM
Arizona
Arkansas
California
Connecticut
Illinois
Iowa
Kansas
Louisiana
Maine
Maryland
Massachusetts
Mississippi
Missouri
New Hampshire
New York
Nevada
North Carolina
North Dakota
Minnesota
New Jersey
New Mexico
Ohio
Oregon
Pennsylvania
South Dakota
Texas
Vermont
West Virginia
Washington
Board of Nursing Has No Formal Position, but Does Not Necessarily
Discourage CAM
Alabama
Alaska
Colorado
Florida
Georgia
Hawaii
Idaho
Indiana
Tennessee
Utah
Virginia
Virgin Islands
Washington
Wisconsin
Wyoming
Kentucky
Michigan
Montana
Oklahoma
Puerto Rico
Rhode Island
South Carolina

The American Holistic Nurses Association (AHNA) has for many years
been the standard bearer for a more holistic approach to nursing care and more
recently has embraced complementary therapies in nursing. In 1994, the AHNA
approached me and asked me to create a course in clinical aromatherapy for
nurses in the USA. The course, Aromatherapy for Health Professionals was en-
dorsed by the AHNA in United States. In 2000, I worked with the AHNA to
produce the following statement on complementary therapies in nursing:
Nursing Complementary and Alternative Modalities (NCAM) offer therapies that
supplement conventional nursing care. NCAM encompasses a broad range of heal-
ing resources that allow registered nurses to integrate such therapies into the nurs-
ing process, which can interface with traditional medical and/or surgical therapies
in order to enhance and promote preventive, supportive, or restorative care.
AHNA is an organization of professional nurses dedicated to the promotion
of health and healing of the whole person: body, mind, emotions, behavior, and
spirit. Holistic nurses utilize nursing interventions that can impact body, mind,
emotions, behavior, and spirit. Holistic nurses integrate nursing theory and prac-
tice models for health care that:
1. Promote and enhance health and well being, or support peaceful dying so
that the person is as independent as possible
2. Manage prescribed care directed toward the prevention and complications
of illness
3. Guide the healing of self and others.
For further information, see the AHNA Standards of Holistic Nursing Practice by
Frisch et al (2000) and Holistic Nursing: A Handbook for Practice (Keegan et al 1999).
The AHNA believes in the integration of NCAM into conventional nursing
care so the client can derive benefit from the best of all interventions available.
The National Institute of Health Center on Complementary and Alternative
Medicines groups CAM practices into five major domains (National Center for
Complementary and Alternative Medicine 2000):
1. Alternative medical systems are complete systems of theory and practice
developed outside the Western biomedical approach (examples include
acupuncture and Oriental medicine).
2. Mind-body–based modalities include behavioral, psychological, social,
and spiritual approaches to health.
3. Biologically based modalities include natural and biologically based prac-
tices and holistic nursing interventions, such as special diets/nutrition, bio-
chemical monitoring, and aromatherapy.
4. Manipulative and body-based methods
5. Energy therapies
The AHNA recognizes the major domains of CAM as modalities that fall
within the realm of holistic nursing practice, except for Alternative Medical
Systems, which may require additional preparation to practice. The AHNA be-
lieves nurses must fulfill the educational and licensing/certification qualifications
required by those disciplines.
Appendix III The White House Commission 397

The AHNA believes the integration of CAM into conventional practice of-
fers opportunities for a higher quality of care. However, the AHNA does not
equate the practice of a CAM modality with holistic care. Rather, holistic care is
defined as the interventions built upon basic nursing practice. Nursing practice is
defined and built upon by three standardized languages for classifying what and
how nurses practice nursing. They are as follows.
1. Nursing Interventions Classification (NIC): is a comprehensive stan-
dardized nomenclature describing treatments nurses perform: more than
486 direct and indirect interventions (McCloskey & Bulechek 1999).
2. Nursing Diagnoses Definitions & Classifications (NANDA Associa-
tion, 2000)
3. Nursing Outcomes Classification contains treatment outcomes repre-
senting all nursing-practice settings and clinical specialties (260 nursing-
sensitive patient outcomes organized in seven domains and 29 classes)
Federal law governing the practice of nursing requires registered nurses to prac-
tice within the scope appropriate to their educational level, knowledge, skill, and
abilities. It allows registered nurses to perform additional acts (such as NCAM) rec-
ognized within the standards of nursing practice and that are authorized by the
nurse’s state BON. Furthermore, registered nurses may employ and initiate such
therapies as part of an overall plan of nursing care to meet nursing and patient goals
(provided the patient has granted informed consent). Goals for the patient include
pain reduction, improved comfort, relaxation, improved coping mechanisms, reduc-
tion or moderation of stress, modification of unhealthy behaviors, and enhancing a
sense of well being. In all practice settings, the registered nurse must have written
policies and procedures in place that guide the performance of such modalities. For
more general questions on nursing, complementary therapies, and their legality,
contact www.legalnurse.com.
REFERENCES
Amdell-Thompson M. 2001. State boards of nursing (BONs)—Oregon. Retrieved April
2, 2003 from Mary.AMDELL-[email protected].us
Frisch N, Dossey B, Guzzetta C, et al. 2000. AHNA Standards of Holistic Nursing
Practice. Gaithersburg, MD: Aspen.
Gordon J. 2002. Interim Progress Report. Alternative Therapies. 7(6) 32-40.
McCloskey J, Bulechek G. (eds). 1999. Nursing Interventions Classification (NIC).
London: Harcourt.
National Center for Complementary and Alternative Medicine. 2000. Five-Year Strate-
gic Plan. June 26. Retrieved October 2001 from http://www.niccam.nih.gov.
O’Brien L. 2001. State boards of nursing (BONs)—New York. Retrieved April 2, 2003
from Lobr[email protected].
Sparber A. 2001. State Boards of Nursing and Scope of Practice of Registered Nurses
Performing Complementary Therapies. Online Journal of Issues in Nursing. August
13. Retrieved October 2002 from http://www.nursingworld.org/ojin/topic15.
Sturn R, Unutzer J. 2001. State legislation and the use of complementary and alternative
medicine. Inquiry 37:423-429.
398 Appendix III The White House Commission

W
Appendix IV
Recommended Essential-Oil
Distributors
T
here are many essential oil distributors that sell good essential oils, and it
would be impossible to list them all. Instead I have listed a few companies
I have used for many years. There are the five companies I use in my cer-
tification program and others I use for my courses.
Companies Used in Certification Program
Florial France
42 Chemin Des Aubepine
06130 Grasse, France
www.florihana.com
US Distributors:
Lisa Roth
2653 Blackhoof Train
Milford, OH 45150
Tel: 513-576-9944
Email: danannscrossing@yahoo.com
and
Kari Morford
9418 14th Avenue SW
Seattle, WA 98106
Tel: 206-768-2568
Email: [email protected]
Fragrant Earth Ltd.
Orchard Court, Magdelene Street
Glastonbury, Somerset BA6 9EW UK
www.fragrant-earth.co.uk
Northwest Essence
Director: Cheryl Young
PO Box 428
Gig Harbor, WA 98335 USA
Tel: 253-858-0777
Email: [email protected]

Scents & Scentsibility Ltd.
Director: Debbie Freund
PO Box 8013
Bridgewater, NJ 08807 USA
Tel: 908-369-4537
www.scentsibility.com
Nature’s Gift
1040 Cheyenne Boulevard
Madison, TN 37115 USA
Tel: 615-612-4270
www.naturesgift.com
Companies Used for Other Courses
Essentially Oils Ltd.
8-10 Mount Farm, Junction Road
Churchill, Chipping Norton, OX7 6NP UK
www.essentiallyoils.com
Elizabeth Van Buren, Inc.
PO Box 7542
Santa Cruz, CA 95061 USA
Tel: 800-710-7759
www.evb.aromatherapy.com
Therapeutic Essentials
5 Michelle Court
Edgewood, NM 87015
Tel: 505-281-9547
Email: [email protected]
Springfield Aromatherapy
Unit 2, 2 Anella Avenue
Castle Hill, NSW 2154
Australia
(2)9894-9934
www.springfieldsaroma.com
Enfleurage
321 Bleeker Street
New York, NY 10014 USA
888-387-0300
www.enfleurage.com
400 Appendix IV Recommended Essential-Oil Distributors

401
W
Appendix V
Useful Addresses, Databases,
and Web sites
A
search on www.google.com or using one of the following databases is a
great way to begin a search for studies on aromatherapy. For botanical
sites, use an individual essential oil, either botanical or common name, as
your search term is likely to bring up more studies than using aromatherapy. For
more information on databases please see Wootton’s Directory of databases for
research into alternative & complementary medicine (1997) in the Journal of Al-
ternative & Complementary Medicine. One of the best places to start for aro-
matherapy searches is Bob Harris’s database, www.aromatherapy.database.com.
This is a privately owned database you can subscribe to that has abstracts of over
800 studies and is excellent value.
Databases
Agricola (National Agricultural Library database) www.nal.usda.gov
American Indian Ethnobotany Database www.umd.umich.edu
Biosciences Information Service of Biological Abstracts www.csfs.ca
Current Awareness Topics/Alternative & Allied Medicine Database
(CATS/AMED) www.bl.uk
Cumulative Index to Nursing and Allied Health (CINAHL) www.cinahl.
com
EMBASE/Excerpta Medica Secondary Publishing Division http://library.
dialog/bluesheets/html
EthnobotDB (Dr. Duke’s Phytochemical Ethnobotanical database) www.
ars.grin.gov
Focus on Alternative & Complementary Therapies (FACT); follow links
through www.pubmed.com
Food Science & Technology Abstracts www.ifis.org
Herb Research Foundation www.herbs.org
IBIS: The Interactive BodyMind Information Service www.ibismedical.com

The Indian Medicinal Plant Distributed Database Network (INMED-
PLAN); access through www.rosenthal.hs.columbia.edu/databases
International Pharmaceutical Abstracts (IPA) www.csa.com/csa
Journal of National Herbalists published by the National Institute of Med-
ical Herbalists www.ejhm.co.uk
Medline National Library of Medicine www.ncbi.nim.nih.gov/PubMed
Medicinal Plants of Native America Database (MPNADBP) www.ars-grin.
gov/duke
NAPRALERT (NAtural PRoducts ALERT) www.ag.uiuc.edu/~ffh/
rapra.html
National Library of Medicine www.nim.nih.gov
Occupational Therapy Index/AMED www.bl.uk/services/information/
amed.html
Phytodok (index of worldwide scientific journals) www.phytopharm.org/en/
science.html
Pubmed www.ncbi.nim.nih.gov/PubMed
Review of Aromatic & Medicinal Plants Journal www.cabi-publishing.org
Science Citation Index; follow links from www.isinet.com
Social Science Citation Index; follow links from www.isinet.com
World Research Foundation www.wrf.org
Planetree Medical Centers and Facilities
Planetree facilities are patient-centered and use complementary therapies includ-
ing aromatherapy in all their facilities. My company, R J Buckle Associates, is an
approved educational provider in aromatherapy and the “m” technique for the
Planetree Hospitals. For a list of their 45 facilities in the United States, go to
www.planetree.org.
REFERENCES
Wootton J. 1997. Directory of Databases for Research into Alternative & Complemen-
tary Medicine. Journal of Alternative & Complementary Medicine. 3(2) 179-190.
402 Appendix V Useful Addresses, Databases, and Web sites

W
403
Appendix VI
Hospitals and Other
Institutions Employing
Aromatherapy in Treatment
USA
Desert Samaritan Medical Center,
Mesa, Arizona
Fountain Valley Hospital, Fountain
Valley, California
Orange Coast Memorial Hospital,
Fountain Valley, California
Saddleback Medical Center, Laguna
Hills, California
Midway Hospital, Los Angeles, Cali-
fornia
Children’s Hospital and Health Cen-
ter, San Diego, California
San Diego Hospice, San Diego, Cali-
fornia
California Pacific Medical Center,
San Francisco, California
O’Connor Hospital, San Jose, Cali-
fornia
Aspen Valley Hospital, Aspen, Col-
orado
Memorial Hospital, Colorado
Springs, Colorado
St. Anthony Hospitals, Centura
Health, Englewood, Colorado
Gunnison Valley Hospital, Gunni-
son, Colorado
Griffin Hospital, Derby, Connecticut
St. Francis Medical Center, Hartford,
Connecticut
Windham Community Memorial
Hospital, Willimantic, Connecti-
cut
Holy Cross Hospital, Sunrise,
Florida
Northside Hospital, Atlanta, Georgia
North Hawaii Community Hospital,
Kamuela, Hawaii
Advocate Good Shepherd Hospital,
Barrington, Illinois
St. James Health and Wellness Insti-
tute, Chicago, Illinois
Advocate Heathcare, Oakbrook, Illi-
nois
Deaconess Hospital Evansville Indi-
ana
Riverview Hospital, Noblesville, In-
diana
Memorial Health System, South
Bend, Indiana

Charlton Health System, Fall River,
Massachusetts
St. Luke’s Health Care System, New
Bedford, Massachusetts
Morton Hospital and Medical Cen-
ter, Taunton, Massachusetts
Tobey Health Systems, Wareham,
Massachusetts
Barbara Ann Karmanos Cancer In-
stitute, Detroit, Michigan
Bronson Methodist Hospital, Kala-
mazoo, Michigan
Mercy Hospital Group, Port Huron,
Michigan
St. John’s Health, Warren, Michigan
Children’s Hospital, St. Paul, Min-
nesota
Regions Hospital, St. Paul, Min-
nesota
St. Peter Community Hospital St Pe-
ter, Minnesota
Woodwinds Health Campus, Wood-
bury, Minnesota
Barnes-Jewish Hospital, St. Louis,
Missouri
St Luke’s Hospital. Chesterfield,
Missouri
Bergen Mercy Medical Center, Om-
aha, Nebraska
St Rose Dominican Hospital, Hen-
derson, Nevada
Wentworth-Douglas Hospital,
Dover, New Hampshire
Cooper Hospital/University Medical
Center, Camden, New Jersey
St. Barnabas Health Care System,
Hackensack, New Jersey.
Mountainside Medical Center,
Montclair, New Jersey
Bellevue Women’s Hospital. Albany,
New York
St Peter’s Medical Center, Albany,
New York
Northern Westchester Hospital Cen-
ter, Mount Kisco, New York
Columbia Presbyterian Medical Cen-
ter,New York,New York
Bellevue Women’s Hospital,
Niskayuna, New York
Morgan Stanley Children’s Hospital,
New York, New York
New York-Weill Cornell Children’s
Hospital, New York, New York
Hugh Chatham Memorial Hospital,
Elkin, North Carolina
Iredell Memorial Hospital,
Statesville, North Carolina
Children’s Hospital Medical Center,
Akron, Ohio
Alliance Community Hospital, Al-
liance, Ohio
Cleveland Clinic Health System,
Chagrin Falls, Ohio
UHHS Bainbridge Health Center,
Chagrin Falls, Ohio
University Hospitals’ Health System,
Cleveland Ohio
Mercy Health Center, Oklahoma
City, Oklahoma
St. Charles Medical Center, Bend,
Oregon
Mid-Columbia Medical Center, The
Dalles, Oregon
Elk Regional Health Center, Elk,
Pennsylvania
St. Peter’s Hospital, Jeanette, Penn-
sylvania
Windber Medical Center, Windber,
Pennsylvania
404 Appendix VI Hospitals Employing Aromatherapy

Highline Community Hospital
Burien, Washington
Elmbrook Memorial Hospital, Brook-
field, Wisconsin
St. Michael Hospital, Milwaukee,
Wisconsin
Shawano Medical Center, Shawano,
Wisconsin
Canada
Children’s Hospital of Western On-
tario. London, Ontario
Toronto Hospital, Toronto, Ontario
Trinity Health Center, Windsor, On-
tario
UK
BUPA Hospital Group, nationwide
London
Edgware Hospital, Edgware, London,
Guy’s and St Thomas’ Hospital NHS
Trust London
Hammersmith Hospital NHS Trust
London
King’s College Hospital Caldecot
Centre, London
London Bridge Hospital, London
The Royal London Homoeopathic
Hospital, London
St George’s Hospital, London
St Thomas’ Hospital, London
University College Hospital NHS
Trust, London
Northern England
Bolton NHS Trust, Bolton, Lan-
cashire
Bridlington Hospital, Bridlington,
East Yorkshire
Hereford Hospitals NHS Trust,
Hereford, Herefordshire
Leeds General Infirmary, Leeds,
Yorkshire
Liverpool & Broadgreen University
Hospitals NHS Trust, Liverpool
Newcastle General Hospital, Newcas-
tle, Durham
Nottingham City Hospital NHS
Trust, Nottinghamshire
Smallwood Day Hospital, Redditch,
Worcestershire
The Queen Elizabeth Hospital, Birm-
ingham
Southern England
Crowborough War Memorial Hospi-
tal, Crowborough, Sussex
Heatherwood Hospital, Ascot, Berk-
shire
Moorgreen Hospital, Southampton,
Hampshire
Mount Vernon Hospital, Northwood,
Middlesex
Musgrove Park Hospital, Taunton,
Devon
Poole Hospital, Poole, Dorset
Royal Surrey Country Hospital NHS
Trust, Guildford, Surrey
Royal South Hants Hospital,
Southampton, Hampshire
Southend Hospital NHS Trust,
Southend, Essex
Swanage Hospital, Swanage, Dorset
West Suffolk Hospital HNS Trust,
Suffolk
Dorset Cancer Centre, based at Poole
Hospital, Dorset
Queen Victoria Hospital NHS
Chartham, Kent
Scotland
Borders Community Hospital Group
thru-out Scotland
Western General Hospital, Edin-
burgh,
Appendix VI Hospitals Employing Aromatherapy 405

Western General Hospital in Edin-
burgh
Northern Ireland
Thompson House Hospital, Lisburn,
Antrim, Northern Ireland
St Francis Private Hospital,
Mullingar, Co Westmeath,
Northern Ireland
Ireland
Galway University College Hospital,
Galway
Stewarts Hospital, Dublin
Australia
Calvary Health Care, Kogarah, New
South Wales
Prince of Wales, Randwick, New
South Wales
St Vincent’s Hospital, Sydney, New
South Wales,
Mater Private Hospital, Brisbane,
Queensland
Royal Brisbane Hospital, Brisbane,
Queensland
St Andrew’s Hospital, Toowoomba,
Queensland
Cabrini Hospital, Malvern, Victoria
Myrtleford Hospital, Myrtleford, Vic-
toria
St. Vincents & Mercy Private Hospi-
tal, Melbourne, Victoria
Swinburne Hospital, Swinburne, Vic-
toria
406 Appendix VI Hospitals Employing Aromatherapy

W
407
Index
A
Abies balsamea, 17
Abortificant, pennyroyal as, 80
Abortion, 323
Abuse, substance, 357-359
Acetaminophen, 93, 215
Achilla millifolium, 42t
Acquired immunodeficiency disease (AIDS), 315-316
Active ingredient, isolation of, 18
Acute pain, 214
Acyclovir for herpes, 287
Addiction, 356-359
Adenosine triphosphate, 67
Adrenaline, 233
Aging, 107, 270
Alantolactone, 52, 52t
Alcohol abuse, 359
Alcohol of essential oil, 46, 47t, 48, 48t
Aldehyde of essential oil, 49-50, 49t
Allelopathy, 70
Allergic reaction, 85-87
Alpha-bisabolol, 47t
Alpha-eudesmol, 48
Altered comfort as nursing diagnosis, 121-125
Alzheimer’s disease, 261
Amygdala, 30, 111
Analgesic essential oil, 151t, 314t, 331t
Androsterone, 111
Anemia, sickle cell, 223
Anethole, 53-54
Anethum graveolens, 45
Angelica archangelica
dreaming and, 111
for nicotine withdrawal, 357
Animal testing of essential oil, 80-81
Anosmia, 31
Anthemis nobilis for inflammation, 223
Antibacterial essential oil, 130-131, 172-178
aromatogram for, 179-180, 179f
for lymphedema, 341t
research on, 173-178
Antibiotic, 167, 169-172
resistance to, 169, 170f, 171-172
in tuberculosis, 370
Anticarcinogenic essential oil, 335, 342t
Anticholinergic drug, 208
Anticholinergic essential oil, 211
Anticoagulant, 90-91, 256
Antidepressant drug, 361
Antifungal agent, 289-291
essential oils as, 317-319, 318t
Eucalyptus globulus as, 122
for lymphedema, 341t
Antiinflammatory agent
chamazulene as, 41
eczema and, 285-286
essential oils as, 223-224, 314t
for low back pain, 151t
for pain, 215-216
for postradiation burn, 339
Antimicrobial essential oil, 281t
Antiparasitic essential oil, 190-192
Antipsychotic drug, 360-361, 360t
Antiretroviral therapy, 182
Antispasmodic essential oil, 222t, 300t, 330
Antiviral agent, synthetic, 181-182
Anxiety
aromatherapy and, 242-243
in child, 346-347
myocardial infarction and, 250-251, 251t
Apium graveolens, 189
Arabia, 15-16
Aroma, 64-65, 70, 73
Aromatherapy Organisation Council, 75
Aromatherapy Registration Council, 137
Aromatogram, 177-178, 179-180, 181f
Artemisia dracunculus, 42t, 175
Artemisia parviflora, 187
Artemisia, 190-191
Artemisia annua, 70
Artemisia caerulescens, 219
Artemisia cina, 192
Arthritis
osteoarthritis, 152, 269-271
rheumatoid, 313-315, 314t
Aspergillosis, 185, 187-188, 189
Asthma, 365-369, 368t
Athlete’s foot, 289-291
Attention deficit/hyperactivity disorder, 348-351
Autoimmune disorder, 313-315
Avicenna, 15-16
AZT, 180, 182
Note: Page numbers followed by f indicate figures; those followed by t indicate tables.

B
B-asarone, 91
B-mycene, 90
Bacilli, 166f
Bacillus subtilis, 174
Bacterial vaginal infection, 329
Barbiturate
b-myrcene interacting with, 90
for insomnia, 202-203
Bark, cinnamon, 95
Barrier to pain management, 216-217
Bay laurel, 183
Bedsores
in critical care patient, 279-281, 280t, 281t
in elderly, 267-269
essential oils for, 178
Benzaldehyde, 189
Benzene ring in phenol, 48-49
Benzodiazepine, 202, 208, 357t
Benzoin, skin reaction to, 85
Bergamot, 39, 87-88, 254
Beta-caryophyllene, 46t
Bilharziasis, 191
Binding of drug, 90
Biosynthesis, 43f, 65-71, 67t
Bipolar disorder, 359-363, 361t, 362t
Bitter fennel, 95
Black cumin, 172, 204
Black pepper oil, 152
Blood pressure, 95, 105
Blue gum eucalyptus, 92
Boldo leaf, 95
Bone marrow transplant, 334-335, 338
Borderline hypertension, 247-250
Borneol, 221-222
Boswellia carteri
for cryptococcosis, 318
for eczema, 286
for low back pain, 150
Bronchitis, 365-369, 368t
Bulinus truncatus, 191
Burn
essential oil for, 173
phototoxicity and, 87
postradiation, 338-339
Bypass surgery, depression after, 252-255, 253t
C
Calamus, 95
Calophyllum inophyllum, 279
Camphene, 366-367, 367t
Camphor, 50, 70, 95
Campylobacter enteritis, 164
Cananga odorata, 46t, 358-359
Cancer
end-of-life care in, 303-307
essential oils in, 341-342, 342t
contraindicated, 95, 342-343
for treatment side effects, 336-341
hair loss in, 339-340
lymphedema in, 340-341
“m” technique for, 153-154
nausea in, 337-338
postradiation burn in, 338-339, 339t
Candida albicans, 185
antifungal essential oils for, 188-189
nail infection with, 189
vaginal infection with, 124, 327-328, 328t
Cannabinoid, 208
Capsaicin, for pain, 221
Carbamazepine, 360t
Carbon dioxide extraction, 60t, 63-64
Carbon dioxide in photosynthesis, 67
Cardamom, 209
Cardiac surgery, 236, 255
Cardiology, 247-256, 251t, 253t
Carrier for lymphedema, 341t
Carvacrol, 48t, 49
Carvone, 25
Cassia, 95
Catharanthus roseus, 335
Catnip, lactones of, 52, 52t
Cedar for eczema, 286
Cedarwood, 93
Cedrus atlantica, 286
Cellulitis, 141
Centella asiatica, 335
Central nervous system disorder, 207-208
Ceylon cinnamon, 183
Chamaemelum nobile
allergy to, 86
drug interactions with, 92
for eczema, 286
for insomnia, 204-205
for pain, 220
taxonomy and properties of, 40-41, 40t
Chamazulene, 41, 46t
Chamomile
German. See German chamomile
for inflammation, 223
for insomnia, 204-205
Moroccan, 40-41, 40t
for postradiation burn, 339
for pressure sore, 279
properties of, 40
Roman. SeeRoman chamomile
taxonomy of, 40-41
Chemistry of essential oils, 43-54. See also Essential
oil, chemistry of
Chemoreceptor trigger zone, 208
Chemotherapy
nausea and vomiting in, 209-211, 337, 338t
study on, 140
Chemotype, 42
Chenopodium ambrosioides, 191-192
Children
cellulitis in, 141
diarrhea in, 141
essential oil doses for, 347t
hyperactive, 348-351
overdose of essential oil in, 79
pediculosis in, 351-352
China, 13
Chiropractic, 149-152, 151t
Chronic bronchitis, 365-369, 368t
Chronic pain, 127, 214
Chronic pain syndrome, 217
Chronic stress, 230-231, 231f
Chronic toxicity, 88
Cigarette smoking, 357
408 Index

1,8-Cineole
as antiviral, 182-183
properties of, 51, 51t
in transdermal therapeutic system, 283
Cinnamaldehyde, 49, 49t
Cinnamomum zyelanticum, 49, 49t
Cinnamon
as antiviral, 183
drug interactions with, 93
overdose of, 78
trichlorophenol and, 85
Cinnamon bark, 42, 95
properties of, 42
Ciprofloxacin, resistance to, 171
Citral, 86
Citronella, 78t, 80, 105
Citronellal, 49, 49t. 204
Citrus aurantium, 275
Citrus bergamia, 39
Citrus limon, 254
Citrus peel oil, 85
Clary sage, 299, 300, 325-326
Closed ventilation system, 130-131
Clostridium, 178
Clove
contraindicated, 95
for herpes, 289
for nausea and vomiting, 211
overdose of, 78t
Clove bud oil, 183, 221-222
Cocaine abuse, 359
Cocoa, 17
Codeine, 215
Cohobation, 62
Commiphora momol
as antiparasitic, 190
for pain, 220-221
Common thyme, 42
Complementary and alternative medicine, 4-6
Compress, 178, 314-315, 330-331
Conduction, galvanic skin, 105
Constipation in elderly, 267, 267t
Contact dermatitis, 85-87
Contraindications for essential oils, 94-96
Coriandrum sativum, 223
Coronary artery bypass surgery, 252-255, 253t
Corticosteroid for nausea and vomiting, 208
Cotton ball, direct inhalation via, 32
Coumarin, 52-53, 53t, 256
Cramp, menstrual, 329-330
Critical care, 274-281
Cross-infection, 193
Cryptococcosis, 185
essential oils for, 186-187, 317-319, 318t
in HIV/AIDS, 316-319, 318t
Cupressus sempervirens, 183
Cymbopogon citratus, 45
aldehydes of, 49, 49t
as antibacterial, 176
for low back pain, 150
for onychomycosis, 290-291
for osteoarthritis, 270
Cymbopogon martini, 47t, 50, 50t
Cymbopogon nardus, 219
Cyperus scariosus, 286
Cypress, 183, 299
Cystic fibrosis, 368
Cystitis, study on, 140-141
D
d-pulegone, 91
Decubitus ulcer
in critical care patient, 279-281, 280t, 281t
in elderly, 267-269
essential oils for, 178
Degenerative joint disease, 269-271
Dementia, 261, 264-266, 266t
Depakote, 360t
Depression, 108-111
bergamot for, 254
postpump, 252-255, 253t
Dermal lethal dose of essential oil, 81
Dermatitis, contact, 85-87
Dermatology, 283-291, 285t, 287t, 288t
Dermatophyte infection, 289-291
Detoxification, 356-357, 357t
Diabetes, 300
Diagnosis, nursing, 119-122
Diazepam, 30, 31
Dicoumarol, 53, 93
Dilution, 25, 74, 138
Distillation, 59, 60t, 61-62, 61f, 84
Diterpene, 46
Drainage, lymphatic, 340
Dressing, 26
Dronabinol, 208
Drop, size of, 138
Drug interaction with essential oil
cellular receptors and, 89-90
changing action or potency, 90-94
pharmacokinetics and, 88-89
taking multiple drugs and, 86
Drug-resistant bacteria, 177-178, 370
Duct, secretory, 69
Dysmenorrhea, 329-331, 330t, 331t
E
Eczema, 284-286, 285t
Egypt, 12-13
Elderly, 260-271
constipation in, 267, 267t
dementia in, 264-266, 266t
insomnia in, 262-264
mood and, 110
osteoarthritis in, 269-271
wound healing in, 267-269, 268f, 269t
Elettaria cardamomum, 209
Elimination, drug, 89
Emergency room, 130
Emmenagogic agent, 324
End-of-life care, 305-307
Endocrine system, 294-300, 295t, 298t, 299t
Endorphin, 239-240
Enfleurage, 60t, 63
English approach to aromatherapy, 77
Enzyme, drug interactions and, 92
Epidermal absorption, 26-27
Epidermal cell, 69
Epilepsy, 95
Index 409

Essential oil
absorption of, 22-23, 24f, 25-28
for aging, 270
in Alzheimer’s disease, 264-265
antibacterial, 130-131, 172-178
anticarcinogenic, 342t
antimalarial, 190-191
antimicrobial, 281t
antiparasitic, 190-192
aroma intensity of, 64-65
in asthma, 366
availability of, 137
biosynthesis of, 65-71, 67t
in bipolar disorder, 361-363, 362t
blood pressure and, 248-249
for burn, 173
buying of, 73-75
camphene in, 366-367, 367t
chemistry of, 43-54
chemotypes of, 42t
in chiropractic, 149-152
for constipation, 267
contraindications for, 94-96
in critical care, 275-277
for depression, 109
for diarrhea, 319
dilution of, 138
drug interactions with, 88-94
for dysmenorrhea, 330, 330t
electroencephalography and, 236-237
expression of, 60t, 62
extract versus, 60f
extraction of, 59-62
for extubation, 277-278
for herpes, 122
homeopathy and, 94
for hyperactive child, 348t
immune function and, 312t
for inflammation, 223-224
inhalation of, 29, 32-33
for insomnia, 203-205, 262-264, 263t
in labor and delivery, 325-327, 326t
for lice, 351-352
for lymphedema, 341t
“m” technique with and without, 153
material safety data sheet for, 74
in menopause, 298-300, 298t
for muscle spasm, 222, 222t
for nausea and vomiting, 209-211
olfaction and, 29-32
oral administration of, 28-29
overdose of, 78t
for pain, 218t
for postpump depression, 253t
for premenstrual syndrome, 297-298, 297t
for pressure sore, 279-281, 280t
purity testing of, 72-73
quality of, 71, 71t
for rheumatoid arthritis, 313-315, 314t
skin reaction caused by, 85-88
storage of, in plant, 68-70
toxicity of, 76-98. See also Toxicity
for tuberculosis, 370-371
uses of, 7-8, 71, 72t
Essential Oil Safety, 95
Essential Oils Trade Association, 74-75
Ester, 41, 50t
Estragole, 53-54
Estrogen, forms of, 296
Estrogen-like effect, 342-343
Ether, 53-54, 54t
Ethical issues, 132
Eucalyptol, 87, 92, 182-183
Eucalyptus, 78t, 79-80, 174, 183
Eucalyptus citriodora, 49t, 291, 300
Eucalyptus globulus
in cystic fibrosis, 368
for extubation, 277-278
for herpes, 122
oxide of, 51t
in tuberculosis, 371
Eugenia caryophyllata, 189, 211
Eugenol
in cinnamon bark, 42
for cryptococcosis, 318
drug interactions with, 93
for herpes, 289
properties of, 48t, 49
Euglobal III for rheumatoid arthritis, 313-314
Europe, aromatherapy in, 16, 17-19
Evening primrose oil for wound healing, 268
Expectorant, 366, 369
Expression of essential oils, 60t, 62
External method of aromatherapy, 77
Extraction, 63-64, 85
Extubation, 277-278
F
Farnesol, 47t
Fatty acid, polyunsaturated, 270
Fear
amygdala and, 111
in critical care, 278
in extubation, 277-278
Female reproductive system, 294-300, 299t
Fennel, 54t, 95, 223
Fetal abnormality, 323-324
Fibromyalgia syndrome, 146-149, 148t, 149t
Fibrosis, cystic, 368
Flavonoid, plant, 223
Floral waters267-268, 280t, 306
Florasol process, 64
Foeniculum vulgare, 54t, 223
Fragrance, allergy to, 85, 87
France, 12
Frankincense
in asthma, 367
for cryptococcosis, 318-319
dreaming and, 111
for eczema, 286
in labor, 325-326
for low back pain, 150
French approach to aromatherapy, 77
French marigold, allergy to, 86
Fungal infection, 184-189
Fungus, plant metabolites and, 70
Furanocoumarin, 53, 87-88
phototoxicity of, 87-88
G
Gamma-aminobutyric acid, 202
Garlic, 184
410 Index

Gas chromatography of essential oil, 72-73
Gastrointestinal disorder, 207
Gastrointestinal worm, 191-192
GCMS, 72-73
Gelatin capsule, 77, 139, 140
Gentamicin, resistance to, 171
Geraniol, 47t, 49t, 289
Geranium
for diarrhea, 141
for dysmenorrhea, 330
in labor, 325-326
in menopause, 300
Geranyl acetate, 50, 50t
German chamomile
allergy to, 86
in bipolar disorder, 361-362
for eczema, 285-286
for inflammation, 223
taxonomy and properties of, 40-41, 40t
Ginger, 210, 221
Glandular trichome, 69
Glucose-6-phosphate dehydrogenase, 93
Glutathione, 93
Gram-negative cocci, 166, 166f, 167
Gram-positive cocci, 166, 166f, 167
Greece, 14-15
Griseofulvin, 289-290
Group A Streptococcus, 164-165
Guaiacwood oil, 87
Guba’s wound-healing cream, 268-269, 269t
Gully gum oil, 182
Gynecology, 327-331
H
Hair loss, 339-340
Head lice, 351-352
Healing in elderly, 267-269, 268f, 269t
Heart disease, 247-256, 251t, 253t
Heart surgery, 236
Hedonic mechanism, 102
Helichrysum picardii, 175
Helichrysum italicum, 270, 357
Heliotropin, 106
HELLP syndrome, 325
Helminth infestation, 191-192
Herbal medicine, 7, 77-78, 359
Heroin addiction, 359
Herpes infection
antiviral essential oils for, 184
case study of, 122
essential oils for, 286-289, 287t, 288t
Hexose, 67t
Hibi oil, 110
HIV infection, 315-316
Holism, 118-119
Holistic aromatherapy, 11
Holy basil, 188
Homeopathy, 94
Honey, 140
Hood, direct inhalation via, 32
Hormone replacement therapy, 298
Hospice, 303-307
Hospital-acquired infection, 162-166, 163f, 163t, 176
Hospital staff, stress and, 237
Hot-pepper cream for pain, 221
Houttynia cordata, 184
Human study of antibacterial essential oils, 177-178
Hybrid, antibacterial, 175t
Hydrocortisone, 93
Hyperactivity, 348-351
Hypericum perforatum, 316, 363
Hypertension
borderline, 247-250
essential oils contraindicated in, 95
pregnancy-induced, 325-327, 326t
Hyssop, 78t
I
Immune system, 311-313, 312t
Immunoglobulin G, 312
Immunology, 234-235, 310-319
Incense, 110
India, 13-14
Indirect inhalation, 32-33
Infection
antibiotics for, 167, 169-172
aromatogram and, 179-180
bacterial classification of, 166-167, 166f, 167f
cross-infection, 193
essential oils for, 172-178
fungal, 184-189
in HIV/AIDS, 316
hospital-acquired, 162-166, 163f, 163t
parasitic, 189-192
spread of, 163t
vaginal, 124-125, 327-328, 327-329, 328t
viral, 180-184, 181f
Inflammation, 222-224
Informed consent, 132
Infrared test, 73
Ingestion, 7, 78-80
Inhalation
direct, 31-32
of essential oils, 29, 32-33
for insomnia, 204
for sinusitis, 368
toxicity of, 82
Insect, plant metabolites affecting, 69-70
Insomnia, 201-205
in elderly, 262-264, 263t
Insurance, 139
Integrative medicine, 5-6
Internal administration of essential oils, 28-29, 77,
136-144
anomalies about use of, 137-138
oral use versus, 137-138
Inula graveolens, 52, 52t
Iraq, 12
Irrigation, wound, 267-268, 268t
Irritation, 84-85
Isoborneol, 184
Isoprene unit, 44-45
J
Jasmine, 104
Joint Commission on Accreditation of Healthcare Or-
ganizations, 214-215
Joint disease, degenerative, 269-271
Juniper, 85-86, 183, 223
Juniperus communis, 223
Index 411

K
Kallmann’s syndrome, 31
Kanuka, 176
Ketoconazole, 289
Ketone, 50-51, 51t
Ketosis, 50
Khella, 53
Khellin, 52-53
Killer T cell, 311
Klebsiella, 164-165
Kunzea ericoides, 176
L
Labeling, 74-75, 85
Labiatae, 39-40
Labor and delivery
aromatherapy for, 242-243
essential oils in, 96, 325-327, 326t
Lactone, 52-53, 52t, 53t
Lamiaceae family, 39-40, 70, 176
Lavandin, 39-40, 275-276
Lavandula, 39-40, 40t, 175t
Lavandula angustifolia, 39-40
alcohols of, 47t
in Alzheimer’s disease, 265
as antiparasitic, 192
in chiropractic, 150
in critical care, 276
drug interactions with, 91
eczema and, 285
in end-of-life care, 307
esters of, 50, 50t
examination stress and, 106-107
for extubation, 278
for insomnia, 203, 262-263, 263t, 264
for nicotine withdrawal, 357
in pregnancy-induced hypertension, 325
quality of essential oil of, 71
sedative effect of, 30
toxicity of, 79
in tuberculosis, 371
for vaginal yeast infection, 328
for wound healing, 268
Lavandula intermedia, 210, 275-276
Lavandula latifolia, 39-40
as antiparasitic, 192
blood pressure and, 249
for extubation, 277-278
toxicity of, 79
Lavandula spicas, 40
Lavandula stoechas, 40, 79
Lavender. See also Lavandula entries
absorption of, 22, 25
in Alzheimer’s disease, 264-265, 265
as antibacterial, 172, 175t
as antiparasitic, 192
in asthma, 367
blood pressure and, 248-249
in chiropractic, 150
contingent negative variation and, 31
in critical care unit, 275
in drug detoxification, 358
drug interactions with, 91
eczema and, 285
examination stress and, 106-107
for hospitalized child, 346-347
Lavender (Continued)
for insomnia, 203, 262-263, 264t
in labor, 325-326
“m” technique with, 153
memory test and, 107
mood and, 110
for nausea and vomiting, 210
in nicotine withdrawal, 357
for osteoarthritis, 152
overdose of, 79
physiologic changes with, 105
psychological associations of, 104
for skin condition, 123
taxonomy of, 39-40
in tuberculosis, 371
for vaginal yeast infection, 328
for wound healing, 268
Lemon, 110
Lemon balm, 182
Lemon oil for postpump depression, 254
Lemongrass
as antibacterial, 176
as antifungal, 187
for cryptococcosis, 317
for low back pain, 150
for onychomycosis, 290
for osteoarthritis, 270
Leptospermum flavescens, 327
Leptospermum scoparium, 176
Lethality of essential oil, 28-29, 80-81
Lice, 351-352
Limbic system, 30-31
Lime blossom, 204
Limonene, 45, 283, 335
Linalol, 47t, 80
Linalyl acetate, 50, 50t
Lipid solubility, 25, 89
Lippia alba, 188
Lippia citriodora, 188-189
Lippia multiflora, 351-352
Lippia sidoides, 48t
Lithium, 360t
Litsea cubeba, 285
Liver disease, 80, 191
Long pepper, 188
Low-back pain, 149-152, 151t
Lupulon, 173
Lymphedema, 340-341
M
“m” technique, 131, 132, 152-154, 254
for cancer patient, 336
in critical care, 276-277
in end-of-life care, 307
for extubation, 276-277
fear and, 278
in pregnancy-induced hypertension, 325
Madagascan periwinkle, 335
Magnetic resonance imaging, 337, 359-360
Malaria, 48, 190-191
Manic-depressive disorder, 359-363
Manipulation, chiropractic, 149-152
Manual therapy, 145-154
Manuka, 176
Marigold, French, 86
Mass spectrometry, 72-73
412 Index

Massage, 145-146
aromatherapy linked with, 7
cancer and, 336
chiropractic and, 149
for constipation, 267
foot, in critical care unit, 275
“m” technique versus, 152-153
Material safety data sheet, 74
Matricaria recutita
allergy to, 86
in bipolar disorder, 361-362
chemotypes of, 42t
eczema and, 285-286
for inflammation, 223
for pressure sore, 279
properties of, 46t
taxonomy and properties of, 40-41, 40t
Melaleuca alternifolia
alcohols of, 47t
for cystitis, 140-141
for vaginal yeast infection, 124, 327-328
for vaginosis, 329
Melissa, 265, 287-288
Melissa officinalis, 182, 261
Memory, 104-107, 254
Menopause, 298-300
Menstrual period, 296-298, 297t, 324
Mental illness, 354-355
Mentha longifolia, 91, 249
Mentha piperita, 51t, 209, 314-315, 368
Mentha rotundifolia, 91, 220, 249
Menthofuran, 80
Menthone, 51t
Mesopotamia, 12
Metabolic disorder, 208
Metabolism, drug, 89-91
Metabolite68, 69
Metastatic cancer, 153-154
Methicillin, resistance to, 171
Methicillin-resistant Staphylococcus aureus, 164, 176-178
Methyl salicylate, 90-91
Metronidazole for vaginosis, 329
Mevalonic pathway, in essential oils, 44
Mind/body connection, 106-108
Mint, drug interactions and, 91
Monarda didyma, 39
Monoterpene, 45
Monoterpenic alcohol, 46
Mood, odor affecting, 109-110
Moroccan chamomile, 40-41, 40t
Mourning, 304
Mugwort, 95
Multiple-drug resistant tuberculosis, 370
Muscle spasm, 150, 222, 222t
Mustard, 94, 95
Mycobacterium avium, 174
Myocardial infarction, 250-251
Myrcene, 45, 222
Myristica fragrans, 174, 223
Myrrh, 220-221
Myrtol, 368-369
N
Nail infection, 189, 289-291
Nardostachys jatamansi, 263
National Association for Holistic Aromatherapy, 75
Native American medicine, 17
Nausea and vomiting, 207-211
in cancer patient, 337-338, 338t
central nervous system causes of, 207-208
conventional approaches to, 208-209
essentials oils for, 209-211
gastrointestinal causes of, 207
metabolic causes of, 208
Nebulizer, 33
Nepeta caesarea, 52, 52t, 219
Nepetalactone, 52, 52t
Neral, 49, 49t
Neroli, 204, 275
Nerolidol, 48
Neurologic disorder, 207-208
Neuropathic pain, 213
Nicotine withdrawal, 357
Nigella sativa, 172, 174, 204
Night sweats, 299
Non-insulin-dependent diabetes, 300
Nonopioid analgesic, 215
Nonphysician clinician, prescriptive license for, 142-
144, 143t
Nonsteroidal antiinflammatory drug, 215-216
Nontoxic ketone, 51
Noradrenaline, 233
North American Nursing Diagnosis Association, 119-
120
Nucleoside analogue for herpes, 287
Nursing practice, 116-133
case study of, 122-129, 126f
nursing diagnosis in, 119-121
Nursing shortage, 116, 117
Nutmeg, 223
O
Obstetrics and gynecology, 323-329, 328t
Occlusive dressing, 26
Ocimum basilicum, 42t
Ocimum sanctum, 188
Odor
brain mapping and, 31
of essential oil, 64-65
pheromones and, 103
pollination and, 70
relaxing versus stimulating, 104
Olfaction, 29-32
Olfactory dysfunction, 264, 359
Olfactory response, 102
Oncology, 334-343
end-of-life care, 303-307
essential oils in, 341-342, 341t
contraindicated, 95, 342-343
for treatment side effects, 336-341
hair loss in, 339-340
lymphedema in, 340-341
“m” technique for, 153-154
nausea in, 337-338
postradiation burn in, 338-339, 339t
Onychomycosis, 289-291
Open-heart surgery, 236
Operating theatre, 130-131
Oppor
tunistic infection in HIV/AIDS,
316
Oral administration, 136-144
of essential oil, 28-29, 77
Oral lethal dose of essential oil, 80-81
Index 413

Oregano, 95, 183, 193
Oregano officinalis, 176
Organ transplant, 236
Origanum majorana, 178, 265
Origanum tyttanthum, cross-infection and, 193
Origanum vulgare, 48t, 174, 193
Ormenis mixta, 40-41, 40t
Ormenis multicaulis, 40-41, 40t
Osteoarthritis, 152, 269-271
Osteomyelitis, 177
Overdose of essential oil, 78t
Overgrowth, Candida, 185
Oxide of essential oil, 51-52, 51t
P
Pain, 213-222
aromatherapy for, 217-222
chronic, case study of, 127
in labor and delivery, 327
“m” technique for, 154
orthodox approach to, 214-217
physiology of, 213-214
relaxation and, 239-240
Palliative care, 304-305
Panic attack, 106
Parasitic infection, 189-192
Parsley seed, abortion and, 323-324
Patch test, 84
Patchouli, 47t, 317
Pathogen, classification of, 168f
Pediculosis, 351-352
Pelargonium graveolens, 39, 174, 330
Penicillinase-resistant Staphylococcus, 171
Pennyroyal, abortion and, 80, 323-324
Pentobarbital, 90, 91
Pentose, 67t
Pepper
black, 152, 174
long, 188
Peppermint
blood pressure and, 249
in menopause, 299
for muscle spasm, 222
for nausea and vomiting, 209-210
for pain, 221
for rheumatoid arthritis, 314-315
sleep and, 111
Peppermint oil, 88, 140
Pharmacokinetics, 25, 88-89
Phenol, 48-49, 48t, 81-82
Phenylethyl acetate, 204
Phenylpropane, 43-44, 43f
Pheromone, 103
Phototoxicity, 53, 87-88
Physical symptoms of stress, 233-234
Phytoestrogen, 342
Phytol, 280t
Picea glauca, 17
Pigmentation, 53
Pine, Scotch, 107-108
Pink root, 192
Pinus pumilio, 92
Piper longum, 188
Piper nigrum, 174, 270
Plant flavonoid, 223
Plasma protein, 90
Pleasure memory, 254
Pneumococcus, 167
Poisoning, 78-80. See also Toxicity
Polymyxin B nonapeptide, 174
Polyunsaturated fatty acid, 270
Portable distillation of essential oils, 62
Postpump depression, 252-255, 253t
Postradiation burn, 338-339
Potency, drug, 90-91
Povidone spray, 337
Pregnancy, 95-96, 210, 323-327
Premenstrual syndrome, 296-298, 297t
Prescriptive license, 142-144, 143t
Pressure sores
in critical care patient, 279-281, 280t, 281t
in elderly, 267-269
Prostaglandin, 216, 294-297
Protein binding in drug interaction, 90
Protocol in bipolar disorder, 361
Pseudomonas aeruginosa, 164, 174
Psoriasis, 123
Psychiatric care, 354-363
Psychoaromatherapy, 103-105
Psychological stress, 233
Psychology, 102-112
Psychoneuroimmunology, 240-244, 311-312
Pulegone, 50-51
Purity of essential oil, 72-73
Q
Quasipharmacologic mechanism, 102
R
R-R interval, changes in, 105
Radiation burn, 338-339
Rapid eye movement sleep, 111-112, 201-202
Red thyme, 95
Refractive index, 73
Relaxation, 7, 238-244
Remission, spontaneous, 243-244
Reproductive system, female, 294-300
Resinoid, 65
Resistance, antibiotic, 169, 170f, 171-172
Respiratory care, 365-371, 372t
Rheumatic disease, 150
Rheumatoid arthritis, 313-315, 314t
Ritalin, 349
RNA virus, 180
Roman chamomile
allergy to, 86
drug interactions with, 92
for dysmenorrhea, 330
for eczema, 286
for inflammation, 223
for insomnia, 204-205
taxonomy and properties of, 40-41, 40t
Root, valerian, 362-363
Rosa damascena, 127
Rosa rubiginosa,
268, 279
Rose oil,
107
for insomnia, 205
in menopause,
299
for pain, 127
for spiritual distress, 128
Rosehip for pressure sore, 279
414 Index

Rosemary
in Alzheimer’s disease, 266
as antifungal, 187
blood pressure and, 248-249
for cryptococcosis, 318-319
in diabetes, 300
drug interactions with, 93
examination stress and, 106-107
for hyperactive child, 350
memory test and, 107
physiologic changes with, 105
Rosmarinus officinalis
in Alzheimer’s disease, 266
blood pressure and, 248-249
for cryptococcosis, 319
in diabetes, 300
examination stress and, 106-107
for hyperactive child, 350
Royal College of Nursing, 137
Rue, 95
S
Sabinyl acetate, 324
Safety, of essential oils, 96
Safety labeling, 75
Sage
as antibacterial, 175t
clary
in labor, 325-326
in menopause, 299, 300
St. John’s wort, 316, 363
Salmonella, 174
Salvia elegans, 261
Salvia officinalis, 42t, 174
Sandalwood, 87, 183-184
Santolol, 48
Sassafras, 95
Satureja, 175t
Satureja hortensis, 270, 319
Savory, 175t
Scabies, 191
Sarcoptes scabii, 191
Sclareol, 48, 335
Scopolamine, 208
Scotch pine, 107-108
Secondary metabolite, 69-70
Secretory structure of plant, 69-70
Sedative, 201-205, 357t
Sedative essential oil for hyperactive child, 350
Selective serotonin reuptake inhibitor, 296-297
Semantic mechanism, 102
Sensitivity, 85-87
Serotonin agonist, 209
Serratia marcescens, 164-165
Sesquiterpene, 45-46
Sesquiterpenol, 4, 47t, 48
Sexually transmitted disease, drug resistant, 172
Shigella, 172, 174
Shikimic pathway, 44
Sickle cell anemia, 223
Sinusitis, 366-369, 368t
Skin
absorption of essentials oils from, 23, 24f, 25-28
lavender for, 123
Skin disorder, 283-291, 285t, 287t, 288t
Skin reaction, 81-82, 85-88
Skin ulcer
in critical care patient, 279-281, 280t, 281t
in elderly, 267-269
essential oils for, 178
Sleep
aroma affecting, 104
in elderly, 262-264, 264t
insomnia and, 201-205
rapid eye movement, 111-112
Smell, sense of, 29-32. See also Odor
age affecting, 107
in Alzheimer’s disease, 264
in child, 347
loss of, 359
pheromones and, 103
psychologic effects of, 354-355
as purity test, 73
Smoking cessation, 357-358
Solubility in drug interactions, 88
Solvent, irritation caused by, 85
Solvent extraction of essential oils, 60t, 63
Spearmint, 210
Spigelia marylandica, 192
Spike lavender
in asthma, 367
blood pressure and, 249
for eczema, 285
properties of, 40t
taxonomy of, 40
Spray, povidone, 337
Spritzer for postradiation burn, 338-339, 339t
Staphylococcus, 167, 171
Staphylococcus aureus, 164, 174
Steam, direct inhalation via, 32
Steam distillation, 59, 61, 62, 84
Steam inhalation for sinusitis, 368
Steroid, antiinflammatory, 216
Stimulant essential oil for hyperactive child, 349-350
Stoechas, 40
Storage of essential oil, 68-70, 96-98
Stratum corneum, 25-26
Streptococcus, 164-165, 167
Streptomyces, 173
Stress, 228-244
aroma affecting, 106-107
definition of, 229
immunology and, 234-235
physical responses to, 232-233
psychoneuroimmunology and, 240-244
Selye’s list of, 230-232, 231f
topical absorption and, 26
Substance abuse, 357-359
Substance P, 214
Sugar, types of, 67t
Summer savory, 270
Suppository, 141
Suppressor cell, 311
Susceptibility, antibacterial, 170f
Sweet birch, 90
Sweet marjoram, 178, 188, 204-205, 265
Synthetic antiparasitic, 190
Synthetic antiviral, 181-182
Synthetic fragrance, allergy to, 85
Synthetic oil, concern about, 132
Syzgium aromatica , 48t, 289
Index 415

T
Tagetes patula, 86
Tanacetum, 338
Tansy, 95
Tarragon, 175
Taxonomy, 39-41, 40t
Tea, pennyroyal, 80
Tea tree
as antibacterial, 176, 177
as antifungal, 189
as antiparasitic, 192
for bacterial vaginosis, 329
for cancer patient, 337
for onychomycosis, 290
for vaginal yeast infection, 327
Tea tree oil
allergic reaction to, 87
for cystitis, 140-141
overdose of, 79
Pseudomonas aeruginosa and, 174
for vaginal yeast infection, 124
Teratogen, 323-324
Terminal patient, 303-307
Terpene, 43-46, 44t, 45t, 70
Terpenic alcohol, 4, 47t, 48
Terpenoid, definition of, 44-45
Terpinen-4-ol, 47t
Terpineol, 93
Testosterone, methol and, 93
Theobroma cocao, 17
Thujopsis dolabrata, 110
Thyme, 42, 95, 175t
Thyme oil, sensitivity to, 87
Thymol, 48t, 248
Thymus vulgaris
as antibacterial, 174
blood pressure and, 248
chemotypes of, 42
thymol in, 48t
Tibet, 14
Tinea ingium, 289-291
Tinea pedis, 289-291
Toenail infection, 289-290
Tonsillitis, 141
Topical application, of essential oils, 23-28
Touch
aromatherapy with, 131
for child, 349
for hospitalized patient, 238
in palliative care, 304
relaxation and, 239
Toxicity
chronic, 88
ingestion reactions in, 78-80
inhalation, 82
of ketones, 50-51
measuring of, 80-81
skin reaction in, 81-82
Trachyspermum ammi, 188, 248
Transanethole, 54t
Transdermal therapeutic system, 289
Transplant, organ, 236
Trichlorophenol, 85
Trichome, glandular, 69
Trichomonas vaginalis, 191, 329
Trichophyton mentagrophytes, 188, 290-291
Triose, 67t
True lavender, 40. See also Lavandula angustifolia
Tuberculosis, 370-371, 372t
U
Ulcer, skin, 267-269, 279-281, 280t, 281t
essential oils for, 178
United Kingdom, 19
Urticaria, 87
V
Vaginal infection
bacterial, 191, 329
yeast, 124-125, 327-328, 328t
Vaginosis, bacterial, 191, 329
Valerian root, 362-363
Valeriana officinalis, 263, 362-363
Valve repair, cardiac, 255
Vancomycin, resistance to, 171
Vaporized essential oil, antibacterial, 193
Vedic medicine, 13
Ventilation system, closed, 130-131
Ventilator-dependent patient, 153-154
Ventilatory weaning response, dysfunctional, 125, 126f
Virola surinamensis, 48
Virus, plant metabolites and, 70
Visitor, stress and, 237-238
Visnagin, 52-53
Vomiting. See Nausea and vomiting
W
Warfarin, 53t, 90-91
Water-and-steam distillation, 59
Water distillation, 59
Weaning response, dysfunctional ventilatory, 125, 126f
Wintergreen, 90-91, 95
Worm infestation, 191-192
Wormseed lavant, 192
Wormwood, 95
Wound healing in elderly, 267-269, 268f, 269t
Wound infection, 178
Y
Yeast infection
Candida albicans, 185
cryptococcosis, 185
essential oils for, 186-187, 317-319, 318t
in HIV/AIDS, 316-319, 318t
vaginal, 124-125, 327-328, 328t
Ylang ylang, 250, 358-359
Z
Zidovudine, 180, 182
Zingiber officinale, 210-221
416 Index
