
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
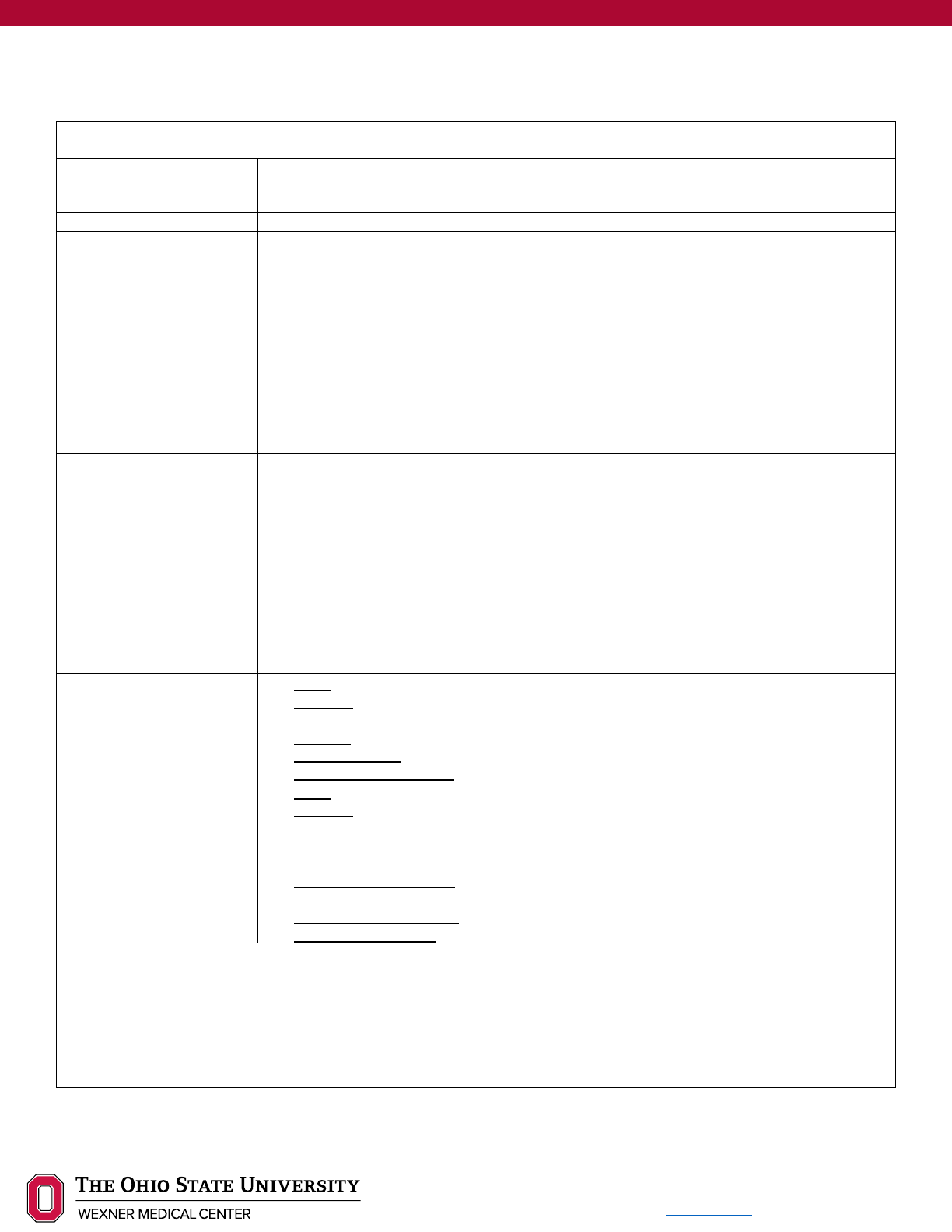
TROCHLEOPLASTY
Background
A trochleoplasty is a surgical procedure that corrects the femoral trochlea to allow for normal (or more normal)
movement of the patella within the trochlear groove during knee flexion and extension. It has been found that
85% of patients with recurrent patellar instability also have trochlear dysplasia, and this procedure is indicated
for patients with both of these deficits. Trochlear dysplasia involves an abnormality in the shape and depth of
the trochlear groove, which creates inadequate patellar tracking during knee flexion. There are 3 main types of
surgical procedures that will address this issue and they are as follows:
• Lateral Facet Elevation
• Sulcus Deepening
• Recession Wedge
Lateral Facet Elevation is indicated in patients with decreased lateral facet height, causing the patella to
translate laterally during knee motion. This type of procedure involves removing bone in the lateral facet and
compaction of the underlying cancellous bone. A bone graft is then implanted into this space, creating a
mechanical block that limits lateral patellar translation.
Sulcus Deepening involves the removal of a strip of cortical bone followed by the removal of a strip of
cancellous bone. This area is then covered by a flap of bone that is shaped to create a V-shaped wedge in the
groove. This process creates a deeper groove in which the patella will glide and demonstrate more appropriate
tracking mechanics.
Recession Wedge Trochleoplasty focuses on reduction of a supratrochlear spur that causes the patella to
move laterally during knee flexion/extension. This technique creates an even surface for patellar gliding, but
does not change the groove depth or the wide sulcus angle that could be present in patients with patellar
instability.
Disclaimer
Progression is time and criterion-based, dependent on soft tissue healing, patient demographics, and clinician
evaluation. Contact Ohio State Sports Medicine at 614-293-2385 if questions arise.

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Summary of Recommendations
Expectations
• Return to sport: 9-15 months
Risk Factors
• Trochleoplasty requires extensive rehabilitation and can often exhaust insurance approved PT visits.
Consider decreasing initial visit frequency, use of home NMES unit and daily self-ROM.
• Long-term quadriceps strength deficits typically present >1 year post-operatively.
Concomitant
Procedures
• MPFL reconstruction is typically always performed with trochleoplasty: Do not change protocol based
on concurrent MPFL reconstruction
• If trochleoplasty is performed in conjunction with osteotomy, rehab progression will be slower and
RTS may be delayed. Refer to operative note or contact physician directly for protocol deviations
Weight
Bearing
Progression
• Phase 1 (weeks 0-4): 25-50% BW – Brace locked at 10-15°, wear brace at all times
• Phase 2 (weeks 4-6): 50-75% BW with brace unlocked to patient’s available flexion ROM (90-120°)
• Phase 3 (weeks 6-8): 75% - Full BW with completely unlocked brace. Consider discharging crutches
at weeks 6-8 (see criteria to discharge assistive device below)
• Phase 4 (weeks 8-12): Full BW – Brace discharge at 8-10 weeks pending appropriate quadriceps
control and normal gait mechanics. May continue brace as needed for adverse weather conditions or
ambulation on uneven ground x12 weeks
• Phase 5 (weeks 12-16): Full BW, no brace
• Phase 6 (weeks 16 – RTS): Full BW, no brace
Range of
Motion
Progression
• Phase 1 (weeks 0-4): 0-90°
• Phase 2 (weeks 4-6): Symmetrical hyperextension - 120° of flexion
• Phase 3 - 6 (weeks 6 - RTS): Full AROM
Functional
Testing
• Isometric testing: 5 months
• Isokinetic testing: 6, 9, 12 months and discharge
• Hop testing (Appropriate after 80% symmetry achieved on isokinetic testing)
o SL hop for distance
o Triple hop
o Cross over hop
o Timed 6m hop
*Functional strength testing and hop testing should be reserved for patients returning high-level activity*
Patient
Reported
Outcomes
Collect the Lower Extremity Functional Scale at each visit
Consider addition one of the following at initial evaluation, every 6 weeks and discharge. Be consistent
with which outcome tool is collected.
• Knee Injury and Osteoarthritis Outcome Score (KOOS)
• International Knee Documentation Committee (IKDC)
Criteria to
Discharge
Assistive
Device
1. ROM: Full active knee extension; no pain on passive overpressure
2. Strength: Able to perform strong quad isometric with full tetany and superior patellar glide and able to
perform 2x10 SLR without quad lag
3. Effusion: 1+ or less is preferred (2+ acceptable if all other criteria are met)
4. Weight Bearing: Demonstrates pain-free ambulation without visible gait deviation
*Patients should be PWBing until week 6, and should continue brace compliance until week 8-10*
Criteria to
Initiate
Running and
Jumping
*No running until the patient is 6 months post-op and meets the criteria listed below*
1. ROM: full, pain-free knee ROM, symmetrical with the uninvolved limb
2. Strength: Isokinetic testing 80% or greater for hamstring and quad at 60º/sec and 300º/sec
3. Effusion: 1+ or less
4. Weight Bearing: normalized gait and jogging mechanics
5. Neuromuscular Control: Pain-free hopping in place
Criteria for
Return to
Sport
1. ROM: full, pain free knee ROM, symmetrical with the uninvolved limb
2. Strength: Isokinetic testing 90% or greater for hamstring and quad at 60º/sec and 300º/sec
3. Effusion: No reactive effusion ≥ 1+ with sport-specific activity
4. Weight Bearing: normalized gait and jogging mechanics
5. Neuromuscular control: appropriate mechanics and force attenuation strategies with high level agility,
plyometrics, and high impact movements
6. Functional Hop Testing: LSI 90% or greater for all tests
7. Physician Clearance

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
RED/YELLOW FLAGS
Red flags are signs/symptoms that require immediate referral for re-evaluation. Yellow flags are
signs/symptoms that require modification to plan of care.
Red Flags
• Signs of DVT (Refer directly to ED)
o Localized tenderness along the distribution of deep venous system
o Entire LE swelling
o Calf swelling >3cm compared to asymptomatic limb
o Pitting edema
o Collateral superficial veins
• Mechanical block or clunk (Refer to surgeon for re-evaluation)
• Lack of full knee extension by 4-6 weeks (Refer to surgeon for re-evaluation)
Yellow Flags
• Persistent reactive pain or effusion following therapy or ADLs
o Decrease intensity of therapy interventions, continue effusion management
and provide patient education regarding activity modification until reactive
symptoms resolve
PHASE 1 (Weeks 0-4)
In this phase, goal is to maintain joint mobility and muscle tone while adhering to all post-operative precautions.
Emphasis is placed on ensuring proper wound healing and effusion management.
Precautions
No OKC knee extension
Range of Motion
0-90°
Achieved though AAROM/AROM
• Extension ROM: Seated towel stretch, prone hang, bag hang
• Flexion ROM: heel slides, wall slides
•
Goal: early AROM though safe range
Weight Bearing
25-50% BW – Brace locked at 10-15°, wear brace at all times
Suggested Interventions
• Ankle pumps
• Quadriceps, hamstring and gluteal isometrics
• SLR in knee brace
• Diaphragmatic breathing
• Effusion management strategies, including RICE
• NMES (with biofeedback as needed)
NMES Parameters
• NMES pads are placed on the proximal and distal quadriceps
• Patient: Seated with the knee in at least 60º flexion, shank secured with strap and
back support with thigh strap preferred. The ankle pad/belt should be two finger
widths superior to the lateral malleoli
• The patient is instructed to relax while the e-stim generates at least 50% of their max
volitional contraction against a fixed resistance OR maximal tolerable amperage
without knee joint pain
10-20 seconds on/ 50 seconds off x 15 min
Criteria to Progress to
Phase 2
By the end of week 4:
• Pain-free knee flexion of 90°
• Pain-free and full passive knee extension
• Proficient heel-to-toe gait with 50% BW
• Compliance with brace at all times
• Reduced and well-controlled post-operative pain and edema
• Ability to perform a strong isometric quadriceps contraction (full tetany and
superior patellar glide)
• Proficiency with home-exercise program

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
PHASE 2 (WEEKS 4-6)
During Phase 2, the patient should achieve full and pain-free knee extension. Focus is placed on increasing LE
strength, proper mechanics and effusion management.
Precautions
No OKC knee extension
Range of Motion
Symmetrical hyperextension - 120°of flexion
Achieved though AAROM/AROM
• Extension ROM: Seated towel stretch, prone hang, bag hang
•
Flexion ROM: heel slides, wall slides
Weight Bearing
50-75% BW with brace unlocked to patient’s available flexion ROM (90-120°)
Suggested Interventions
• Continue phase 1 interventions as needed
• Prone TKE
• SLR-4 way – without brace if quadriceps lag is not present
• Double leg CKC interventions with brace
o Shuttle press
o Mini-squats
o Bridges
o Sit to stands
o Side steps
o Wall sit
• Patellar mobilization in superior and inferior directions only
o Initiate medial and lateral patellar glides at 6 weeks
• Gait training
• Upright cycling- for ROM only
• Trunk stability interventions
o TrA isometric progression
o Prone/side planks
• Continue effusion management and NMES (seated with tibia fixed at 60° of knee
flexion)
Criteria to Progress to
Phase 3
By the end of week 6:
• Pain-free Symmetrical hyperextension - 120°of flexion
• Proficient heel-to-toe gait with 75% BW with brace unlocked to 120°of flexion
• Reduced and well-controlled post-operative pain and edema
• Ability to perform SLR without quadriceps lag without knee brace
• Proficiency with home-exercise program

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
PHASE 3 (WEEKS 6-8)
During Phase 3, the patient works toward movement independent of ambulation devices. Full ROM should be achieved
and balance/proprioception interventions are initiated. Progression towards SL CKC interventions is appropriate during
Phase 3.
Precautions
No OKC knee extension
Range of Motion
Full AROM
Weight Bearing
75% - Full BW with completely unlocked brace. Consider discharging crutches at weeks
6-8 (see criteria to discharge assistive device)
Suggested Interventions
• Continue Phase 1 and 2 interventions
• SLR-Flexion progressions
o Semi-reclined or seated
o Add ER
o Perform with eyes closed (cortical training)
o Speed
o Isometric holds at end-range
• Initiate single leg CKC interventions with brace on
o Single leg sit to stand
o Single leg wall sit
• Initiate SL balance and proprioceptive interventions
• Upright cycling for strength and endurance
• Continue effusion management strategies and NMES (seated with tibia fixed at 60° of
knee flexion)
Criteria to Discharge
Assistive Device
1. ROM: Full active knee extension; no pain on passive overpressure
2. Strength: Able to perform strong quad isometric with full tetany and superior patellar
glide and able to perform 2x10 SLR without quad lag
3. Effusion: 1+ or less is preferred (2+ acceptable if all other criteria are met)
4. Weight Bearing: Demonstrates pain-free ambulation without visible gait deviation
Criteria to Progress to
Phase 4
By the end of week 8:
• Pain-free full AROM
• Pain-free gait with full BW with unlocked brace
• Discharged crutches, pain-free ambulation without visible gait deviation
• Proficiency with home exercise program

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
PHASE 4 (WEEKS 8-12)
During Phase 4, the majority of patients return to work either on a part-time or full-time basis. Patients should continue
skilled physical therapy to progress functional, CKC strengthening (DL and SL).
Precautions
No running or impact activities
Range of Motion
Full AROM
Weight Bearing
Full BW – Brace discharge at 8-10 weeks pending appropriate quadriceps control and
normal gait mechanics. May continue brace as needed for adverse weather conditions or
ambulation on uneven ground x12 weeks
Suggested Interventions
• Continue Phase 2 and 3 interventions
• Continue ROM interventions until symmetrical ROM is achieved
• Continue to progress single leg interventions per patient’s tolerance
• Progress proprioceptive and core interventions per patient’s tolerance
• Multi-angle isometrics
• SAQ
• Unresisted LAQ
• Continue NMES (seated with tibia fixed at 60° of knee flexion)
• Continue effusion management strategies as needed
Criteria to Progress to
Phase 5
By week 12:
• Full and pain-free active ROM
• Pain-free ambulation without visible gait deviation
• Full and pain-free ADLs (including stair negotiation), with proper technique
• Able to perform single leg balance x60 seconds without complaints of pain
• Able to perform x5 single leg squats 60-90°
• Proficiency in home exercise program
PHASE 5 (WEEKS 12-16)
During Phase 5, patient progresses OKC interventions and can initiate cardio training via elliptical or stair stepper. Full
return to unrestricted IADLs and vocational duties should be achieved during this phase.
Precautions
No running or impact activities. Continued emphasis on mechanics to avoid patellofemoral
pain.
Range of Motion
Full AROM
Weight Bearing
Full BW, no brace
Suggested Interventions
• Continue Phase 3 and 4 interventions
• Continue to progress single leg interventions per patient’s tolerance
• Progress proprioceptive and core interventions per patient’s tolerance
• Bridging
• Resisted OKC quadriceps strengthening
o Partial ROM (90-45°) – weeks 12-13
o Full ROM – weeks 14-16
• Lunges
• Step Ups
• Heel Taps
• Elliptical/stair stepper
• Outdoor cycling if desired
• Rowing ergometry as tolerated
• Continue NMES until 80% symmetry is obtained (seated with tibia fixed at 60° of knee
flexion)
• Continue effusion management as needed
Criteria to Progress to
Phase 6
By 4 months:
• Ability to negotiate stairs and mild gradients without pain or reactive effusion
• Return to work, depending on the demands of the job
• Ability to perform 3x10 heel tap on 6” step with neutral frontal and sagittal plane
alignment
• Proficiency in home exercise program
For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
PHASE 6 (WEEKS 16 - RTS)
In Phase 6, strength assessments are utilized to determine readiness to return to running/jumping. Care is taken to
emphasize mechanics and functional movement patterns to safely transition back to sport.
Precautions
Running should not be initiated until 6 months post-op. The surgeon must provide final
clearance for RTS
Range of Motion
Full AROM
Weight Bearing
Full BW, no brace
Suggested Interventions
• Continue phase 2-5 interventions
• Progress and increased difficulty of OKC exercises
• Continue to progress SL eccentric strengthening through body weight and
machine interventions
• Once strength criteria have been met:
o PBW jumping on the shuttle
o Step-hold progression to SL hop progressions
o Walk-jog program
o Sports-specific training
o Agility
o Plyometric training
Strength Testing
Isometric testing is appropriate at 5 months
Isokinetic testing is appropriate at 6, 9 and 12 months, and RTS
SL hop testing battery (appropriate once the patient has achieved 80% LSI on isokinetic
testing)
• SL hop for distance
• Triple hop for distance
• Cross over hop for distance
• 6m timed hop
*Functional strength testing and hop testing should be reserved for patients returning
high-level activity*
Criteria to Initiate
Running
and Jumping
1. ROM: full, pain-free knee ROM, symmetrical with the uninvolved limb
2. Strength: Isokinetic testing 80% or greater for hamstring and quad at 60º/sec and
300º/sec
3. Effusion: 1+ or less
4. Weight Bearing: normalized gait and jogging mechanics
5. Neuromuscular Control: Pain-free hopping in place
Criteria to Return to
Sport
1. ROM: full, pain free knee ROM, symmetrical with the uninvolved limb
2. Strength: Isokinetic testing 90% or greater for hamstring and quad at 60º/sec and
300º/sec
3. Effusion: No reactive effusion ≥ 1+ with sport-specific activity
4. Weight Bearing: normalized gait and jogging mechanics
5. Neuromuscular control: appropriate mechanics and force attenuation strategies with
high level agility, plyometrics, and high impact movements
6. Functional Hop Testing: LSI 90% or greater for all tests
7. Physician Clearance
Most patients who undergo this procedure have limited sports goals and have not routinely engaged in jumping and
pounding sports. Define patient goals and expectations upfront, and work with the surgeon to modify protocol
accordingly.
Full RTS expected between 9-15 months post-operatively

For OSUWMC USE ONLY. To license, please
contact the OSU Technology Commercialization
Office at https://tco.osu.edu.
Author: Caroline Brunst, PT, DPT, SCS, AT; Megan McCabe, SPT
Reviewers: Mary Montalto, PT, DPT; Vickie Otto, PT, DPT; Robert Magnussen, MD, MPH; David Flanigan, MD
References:
Balcarek, P., & Zimmermann, F. (2019). Deepening trochleoplasty and medial patellofemoral ligament reconstruction
normalize patellotrochlear congruence in severe trochlear dysplasia. The Bone & Joint Journal, 101–B(3), 325–330.
https://doi.org/10.1302/0301-620X.101B3.BJJ-2018-0795.R2
Camathias, C., Speth, B. M., Rutz, E., Schlemmer, T., Papp, K., Vavken, P., & Studer, K. (2018). Solitary Trochleoplasty
for Treatment of Recurrent Patellar Dislocation. JBJS Essential Surgical Techniques, 8(2), e11.
https://doi.org/10.2106/JBJS.ST.17.00039
DeJour, D., & Saggin, P. (2010). The sulcus deepening trochleoplasty—the Lyon’s procedure. International Orthopaedics,
34(2), 311. https://doi.org/10.1007/S00264-009-0933-8
Duncan, S. T., Noehren, B. S., & Lattermann, C. (2012). The role of trochleoplasty in patellofemoral instability. Sports
Medicine and Arthroscopy Review, 20(3), 171–180. https://doi.org/10.1097/JSA.0b013e31826a1d37
Hiemstra, L. A., Peterson, D., Youssef, M., Soliman, J., Banfield, L., & Ayeni, O. R. (2018). Trochleoplasty provides good
clinical outcomes and an acceptable complication profile in both short and long-term follow-up. Knee Surgery, Sports
Traumatology, Arthroscopy. https://doi.org/10.1007/s00167-018-5311-x
Laidlaw, M. S., & Diduch, D. R. (2017). Current Concepts in the Management of Patellar Instability. Indian Journal of
Orthopaedics, 51(5), 493–504. https://doi.org/10.4103/ortho.IJOrtho_164_17
Laidlaw, M. S., Feeley, S. M., Ruland, J. R., & Diduch, D. R. (2018). Sulcus-Deepening Trochleoplasty and Medial
Patellofemoral Ligament Reconstruction for Recurrent Patellar Instability. Arthroscopy Techniques, 7(2), e113–e123.
https://doi.org/10.1016/j.eats.2017.08.061
McGee, T. G., Cosgarea, A. J., McLaughlin, K., Tanaka, M., & Johnson, K. (2017). Rehabilitation After Medial
Patellofemoral Ligament Reconstruction. Sports Medicine and Arthroscopy Review, 25(2), 105–113.
https://doi.org/10.1097/JSA.0000000000000147
Nolan, J. E., Schottel, P. C., & Endres, N. K. (2018). Trochleoplasty: Indications and Technique. Current Reviews in
Musculoskeletal Medicine, 11(2), 231–240. https://doi.org/10.1007/s12178-018-9478-z
Weber, A. E., Nathani, A., Dines, J. S., Allen, A. A., Shubin-Stein, B. E., Arendt, E. A., & Bedi, A. (2016). An Algorithmic
Approach to the Management of Recurrent Lateral Patellar Dislocation. The Journal of Bone and Joint Surgery,
98(5), 417–427. https://doi.org/10.2106/JBJS.O.00354
