
### Related CR ####
Page 1 of 10
Overview of the Patient Driven Groupings Model
MLN Matters Number: SE19027
Article Release Date: November 25, 2019
Related CR Transmittal Number: N/A
Related Change Request (CR) Number: N/A
Effective Date: January 1, 2020
Implementation Date: January 1, 2020
PROVIDER TYPES AFFECTED
This special edition MLN Matters® article is intended for physicians that order home
health services.
PROVIDER ACTION NEEDED
This article provides information on the implementation of the new Home Health Prospective
Payment System (HH PPS) case-mix adjustment methodology named the Patient-Driven
Groupings Model (PDGM). The PDGM will be implemented for home health periods of care
starting on and after January 1, 2020.
BACKGROUND
Medicare home health services are available to eligible Medicare beneficiaries. To be eligible
for Medicare home health services, a physician must certify that a patient:
1. Is confined to the home;
2. Needs skilled services (intermittent skilled nursing, physical therapy, speech-
language pathology services, or a continuing need for occupational therapy after the
need for skilled nursing, physical therapy and/or speech language pathology
services have ceased);
3. Is under the care of a physician;
4. Receives services under a plan of care established and reviewed by a physician; and
5. Had a face-to-face encounter with a physician or allowed non-physician practitioner.
Section 1814(a) and Section 1835(a) of the Act specify that an individual is considered
“confined to the home” (homebound) if the following two criteria are met:

MLN Matters SE19027 Related CR N/A
Page 2 of 10
First Criteria
One of the following must be met:
Second Criteria
Both of the following must be met:
1. Because of illness or injury, the individual
needs the aid of supportive devices such as
crutches, canes, wheelchairs, and walkers; the
use of special transportation; or the assistance
of another person to leave their place of
residence.
1. There must exist a normal
inability to leave home.
2. Have a condition such that leaving his or
her home is medically contraindicated.
2. Leaving home must require
a considerable and taxing
effort.
The aged person who does not often travel from home because of frailty and insecurity brought
on by advanced age would not be considered confined to the home for purposes of receiving
home health services unless they meet the above conditions.
The patient may be considered homebound (that is, confined to the home) if absences from the
home are:
• Infrequent;
• For periods of relatively short duration;
• For the need to receive health care treatment;
• For religious services;
• To attend adult daycare programs; or
• For other unique or infrequent events (for example, funeral, graduation,
trip to the barber).
Medicare covered home health services include:
• Skilled nursing (SN) care (other than solely venipuncture for the purposes of
obtaining a blood sample) on part-time or intermittent basis;
• Home health aides on a part-time or intermittent basis;
• Physical therapy (PT);
• Occupational therapy (OT);
• Speech-language pathology (SLP);
• Medical social services;
• Routine & non-routine medical supplies (for example, catheters, catheter care supplies,
ostomy bags, and ostomy care supplies);
• Durable Medical Equipment (paid separately from the home health prospective payment);
• Injectable osteoporosis drugs (reimbursed on a reasonable cost basis and the patient must
meet certain criteria); and
• Negative pressure wound therapy using disposable devices.

MLN Matters SE19027 Related CR N/A
Page 3 of 10
Changes to Home Health Payment
Since October 2000, Home Health Agencies (HHAs) have been paid under a Home Health
Prospective Payment System (HH PPS) for 60-day episodes of care that include all covered
home health services. The 60-day payment amount is adjusted for case-mix and area wage
differences. The case-mix adjustment under this system included: a clinical dimension; a
functional dimension; and a service dimension, in which payment would increase if certain
thresholds of therapy visits were met.
The Bipartisan Budget Act of 2018 (BBA of 2018) includes several requirements for home
health payment reform, effective January 1, 2020. These requirements include the elimination of
the use of therapy thresholds for case-mix adjustment and a change from a 60-day unit of
payment to a 30-day unit of payment. The mandated home health payment reform resulted in
the Patient-Driven Groupings Model, or PDGM. The PDGM removes the current incentive to
overprovide therapy, and instead, is designed to focus more heavily on clinical characteristics
and other patient information to better align Medicare payments with patients’ care needs.
The Importance of Diagnosis Reporting and Physician Documentation
under the PDGM
Under the Medicare home health benefit, the patient must be under the care of a physician and
must be receiving home health services under a plan of care established and periodically
reviewed by a physician. Physicians play an important role in the provision of home health
services and HHAs rely on documentation from the certifying physician (and/or the acute/post-
acute care facility) to confirm home health eligibility, substantiate diagnoses that are populated
on the home health claim and factor into the payment amount, and to help demonstrate the
medical necessity of the home health services provided.
The principal diagnosis code on the home health claim will assign the home health period of
care to a clinical group that explains the primary reason the patient is receiving home health
services. For example, if the reported principal diagnosis is a “stage 2 pressure ulcer of the left
heel”, the home health period of care would be assigned to the “wound” clinical group, meaning
the primary reason for home health services is for wound care. Payment varies between each of
the clinical groups to account for the differences in resource use associated with the primary
reason for home health care.
There are certain diagnoses that are vague, unspecified, or not allowed to be reported as a
principal diagnosis by ICD-10 coding guidelines that will not be assigned into a clinical group. If
a home health claim is submitted with a principal diagnosis that would not be assigned to a
clinical group under the PDGM, the claim would be returned to the HHA for more definitive
diagnosis coding. The top 5 diagnoses reported on home health claims that would not be
assigned to a clinical group are:
• M62.81, Muscle weakness, generalized
• R26.89 Other abnormalities of gait and mobility
• M54.5, Low back pain
• R26.81, Unsteadiness on feet
• R53.1, Weakness

MLN Matters SE19027 Related CR N/A
Page 4 of 10
For example, if a patient has been referred to home health with a principal diagnosis of “muscle
weakness, generalized” (M62.81), this would not be assigned to a clinical group because this is
a vague code that does not clearly support a rationale for skilled services. If the underlying
etiology of the generalized muscle weakness is unknown by the time a home health referral is
made, a more definitive principal diagnosis is warranted in order to justify the need for skilled
services and appropriate treatment. Further, if the original condition is resolved, but the resulting
muscle weakness persists as a result of the known original diagnosis, we anticipate that a more
specific code exists that accounts for why the muscle weakness is on-going, such as muscle
wasting or atrophy. So, if M62.561, “muscle wasting and atrophy of the right lower leg” is
reported as the principal diagnosis, the home health period of care would be assigned to the
“Musculoskeletal Rehab” clinical group, meaning the primary reason for home health services is
for therapy.
Additionally, if reported as a principal diagnosis, most symptom diagnoses will not be assigned
to a clinical group under the PDGM. Clinically, it is important for HHAs to have a clear
understanding of the patients’ diagnoses in order to safely and effectively furnish home health
services. Interventions and treatment aimed at mitigating signs and symptoms of a condition
may vary depending on the cause. For example, if a patient has been referred to home health
with a diagnosis of ‘‘other abnormalities of gait and mobility’’ (R26.89), it is important for the
home health clinician to know what is precipitating the abnormality. For instance, a plan of care
for a gait abnormality related to a neurological diagnosis (such as Parkinson’s disease, G20) is
likely to be different from a plan of care for a gait abnormality due to a fracture or injury (such as
a fracture of the head and neck of femur, S72.0).
There are other, more specific ICD-10-CM diagnosis codes that could be used as the principal
diagnosis instead of symptom codes to ensure that a home health period of care is accurately
assigned to the appropriate clinical group reflecting the patient’s home health care needs.
Symptom codes can be reported as secondary diagnoses, as appropriate, to more fully explain
patient characteristics.
Reported secondary diagnoses (that is, comorbidities) also factor into the case-mix adjustment
methodology under the HH PPS. For example, if there is a reported secondary diagnosis of
“heart failure,” home health payment is increased for the period of care to account for the
additional resource needs associated with this condition. Additionally, HHAs can report up to 24
secondary diagnoses that may be eligible for additional payment under the PDGM.
Complete, accurate, and specific diagnosis reporting by physicians, along with clinical
documentation supporting all diagnoses, is important to make sure that patient characteristics
are fully captured under the PDGM. However, this does not mean that the certifying physician
would be required to perform additional diagnostic testing solely to certify a patient for home
health services or establish a home health plan of care. Complete and comprehensive
documentation of the patient’s diagnoses and other clinical conditions by the physician will help
to ensure that such diagnoses support medical necessity and Medicare payment aligns with
your patient’s home health resource needs.
30-Day Periods of Care under the PDGM:
While the unit of payment for home health services will be a 30-day period starting on January
1, 2020; there are no changes to timeframes for re-certifying eligibility and reviewing the home

MLN Matters SE19027 Related CR N/A
Page 5 of 10
health plan of care, both of which still need to occur every 60-days (or in the case of updates to
the plan of care, more often as the patient’s condition warrants). Physicians are separately paid
by Medicare for certification and recertification for home health services.
Because the unit of payment is now 30-days, instead of 60-days, HHAs may have more
frequent contact with the certifying physician to communicate any changes in the patient’s
condition to ensure that home health payment is adjusted to account for those changes.
Furthermore, the certification and the home health plan of care must be signed timely by the
certifying physician because HHAs will submit a final claim with each 30-day period of care and
need this important signed documentation in order to bill for home health services.
Home health services are not limited to a single 30-day period of care. An individual can
continue to receive home health services for subsequent 30-day periods as long as the
individual continues to meet home health eligibility criteria.
Overview of the Patient-Driven Groupings Model:
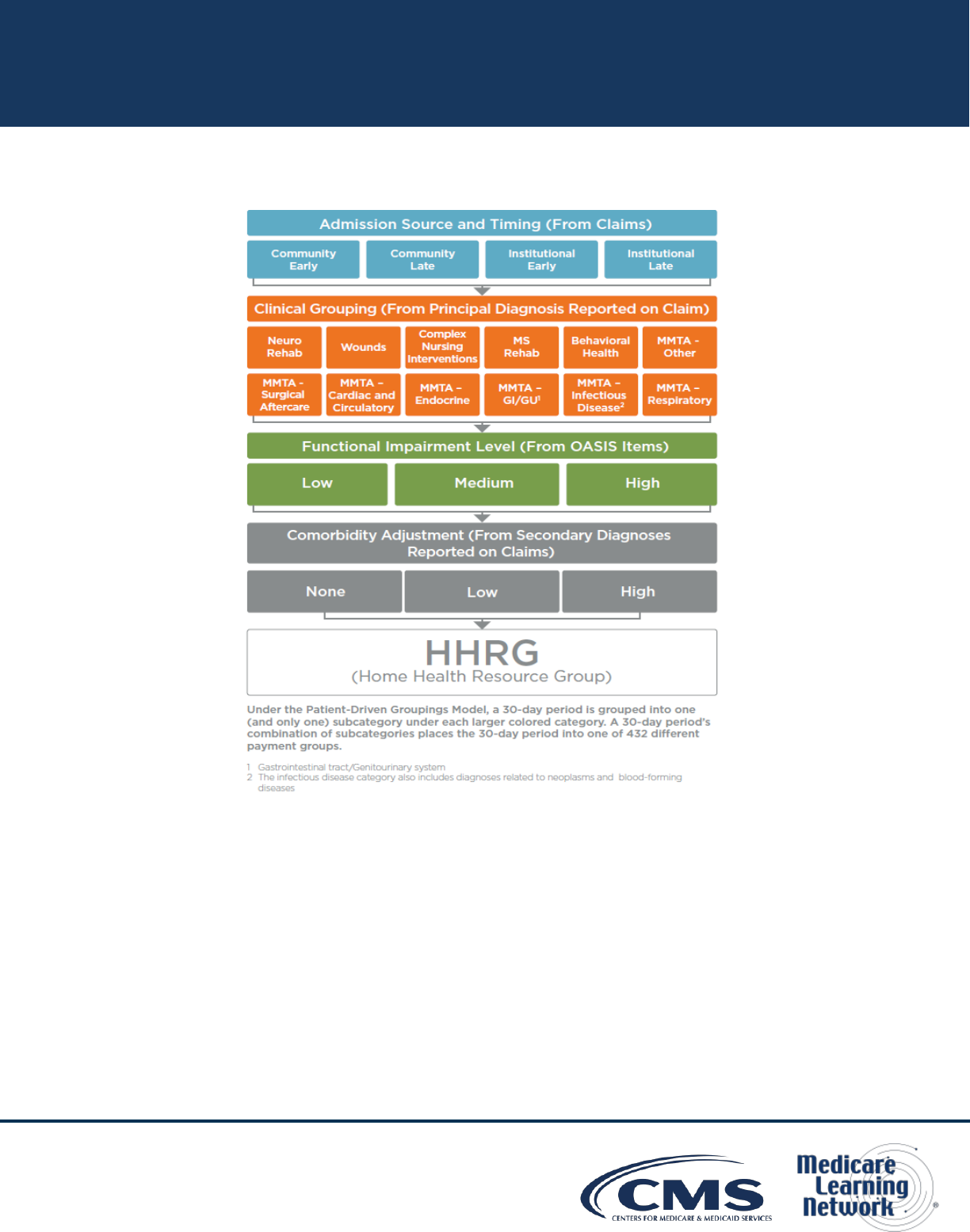
Figure 1 below provides an overview of how 30-day periods are categorized into 432 case-mix
groups for the purposes of adjusting payment under the PDGM. In particular, 30-day periods are
placed into different subgroups for each of the following broad categories:
• Admission source (two subgroups): community or institutional admission source
• Timing of the 30-day period (two subgroups): early or late
• Clinical grouping (twelve subgroups): musculoskeletal rehabilitation; neuro/stroke
rehabilitation; wounds; Medication Management, Teaching, and Assessment (MMTA)
- surgical aftercare; MMTA - cardiac and circulatory; MMTA - endocrine; MMTA -
gastrointestinal tract and genitourinary system; MMTA - infectious disease,
neoplasms, and blood-forming diseases; MMTA - respiratory; MMTA- other;
behavioral health; or complex nursing interventions
• Functional impairment level (three subgroups): low, medium, or high
• Comorbidity adjustment (three subgroups): none, low, or high based on secondary diagnoses.
In total, there are 2*2*12*3*3 = 432 possible case-mix adjusted payment groups.
MLN Matters SE19027 Related CR N/A
Page 6 of 10
Figure 1: Structure of the Patient-Driven Groupings Model
Admission Source:
Under the PDGM, each 30-day period is classified into one of two admission source categories
– community or institutional – depending on what healthcare setting was utilized in the 14 days
prior to home health admission. Late 30-day periods are always classified as a community
admission unless there was an acute inpatient hospital stay in the 14 days prior to the late home
health 30-day period. A post-acute stay in the 14 days prior to a late home health 30-day period
would not be classified as an institutional admission unless the patient had been discharged
from home health prior to a post-acute stay.
Timing of the 30-Day Period:
Under the PDGM, the first 30-day period is classified as early. All subsequent 30-day periods
(second or later) in a sequence of 30-day periods are classified as late. A sequence of 30-day
periods continues until there is a gap of at least 60-days between the end of one 30-day period

MLN Matters SE19027 Related CR N/A
Page 7 of 10
and the start of the next. When there is a gap of at least 60-days, the subsequent 30-day period
is classified as being the first 30-day period of a new sequence (and therefore, is labeled as
early).
Clinical Groups:
Under the PDGM, each 30-day period is grouped into one of twelve clinical groups based on the
patient’s principal diagnosis as reported on home health claims. The reported principal
diagnosis provides information to describe the primary reason for which patients are receiving
home health services under the Medicare home health benefit. Table 1 below describes the
twelve clinical groups. These groups are designed to capture the most common types of care
that Home Health Agencies (HHAs) provide.
Table 1: PDGM Clinical Groups
Clinical Groups
The Primary Reason for the Home Health
Encounter is to Provide:
Musculoskeletal
Rehabilitation
Therapy (physical, occupational or speech)
for a musculoskeletal condition
Neuro/Stroke
Rehabilitation
Therapy (physical, occupational or speech)
for a neurological condition or stroke
Wounds – Post-Op
Wound Aftercare and
Skin/Non-Surgical Wound
Care
Assessment, treatment & evaluation of a
surgical wound(s); assessment, treatment &
evaluation of non-surgical wounds, ulcers,
burns, and other lesions
Behavioral Health Care
Assessment, treatment & evaluation of
psychiatric conditions, including substance
use disorder
Complex Nursing
Interventions
Assessment, treatment & evaluation of
complex medical & surgical conditions
including IV, TPN, enteral nutrition, ventilator,
and ostomies
MLN Matters SE19027 Related CR N/A
Page 8 of 10
Clinical Groups
The Primary Reason for the Home Health
Encounter is to Provide:
Medication Management, Teaching
and Assessment (MMTA)--
• MMTA –Surgical Aftercare
• MMTA – Cardiac/Circulatory
• MMTA – Endocrine
• MMTA – GI/GU
• MMTA – ID/Neoplasms/ Blood
Diseases
• MMTA –Respiratory
• MMTA – Other
Assessment, evaluation, teaching, and
medication management for a variety of medical
and surgical conditions not classified in one of
the above listed groups. The subgroups
represent common clinical conditions that require
home health services for medication
management, teaching, and assessment.
While there are clinical groups where the primary reason for home health services is for therapy
(for example, Musculoskeletal Rehabilitation) and other clinical groups where the primary
reason for home health services is for nursing (for example, Complex Nursing Interventions),
these groups represent the primary reason for home health services during a 30-day period of
care, but not the only reason for home health care. Home health remains a multidisciplinary
benefit and payment is bundled to cover all necessary services identified on the individualized
home health plan of care.
Functional Impairment Level:
The PDGM designates a functional impairment level for each 30-day period based on
responses to the OASIS items in Table 2 below:
Table 2: OASIS Items Used for Functional Impairment Level in the PDGM
Item # Description
M1033 Risk for Hospitalization
M1800 Grooming
M1810 Current ability to dress upper body safely
M1820 Current ability to dress lower body safely
M1830 Bathing
M1840 Toilet transferring

MLN Matters SE19027 Related CR N/A
Page 9 of 10
Item # Description
M1850 Transferring
M1860 Ambulation and locomotion
Responses that indicate higher functional impairment and a higher risk of hospitalization are
associated with higher resource use and are therefore assigned higher points. These points are
then summed, and thresholds are applied to determine whether a 30-day period is assigned a
low, medium, or high functional impairment level.
Comorbidity Adjustment:
The PDGM includes a comorbidity adjustment category based on the presence of certain
secondary diagnoses (for example, congestive heart failure) associated with increased resource
use. Depending on a patient’s secondary diagnoses, a 30-day period may receive no
comorbidity adjustment, a low comorbidity adjustment, or a high comorbidity adjustment. Home
health 30-day periods of care can receive a comorbidity adjustment under the following
circumstances:
• Low comorbidity adjustment: There is a reported secondary diagnosis that is
associated with higher resource use, or;
• High comorbidity adjustment: There are two or more secondary diagnoses that
are associated with higher resource use when both are reported together compared
to if they were reported separately. That is, the two diagnoses may interact with one
another, resulting in higher resource use.
• No comorbidity adjustment: A 30-day period would receive no comorbidity
adjustment if no secondary diagnoses exist or none meet the criteria for a low or high
comorbidity adjustment.
With the implementation of the PDGM in CY 2020, the physician continues to play an invaluable
role in making sure that needed home health services are provided to eligible Medicare
beneficiaries through accurate, specific diagnosis reporting, developing a patient-specific home
health plan of care identifying all services and disciplines to provide care, and communicating
with home health agencies in a timely-fashion to ensure that all Medicare requirements are met.
RESOURCES
Read MLN Matters Article SE19028 for current information on the PDGM.
HHA Center Webpage at: https://www.cms.gov/Center/Provider-Type/Home-Health-Agency-
HHA-Center.html
PDGM Webpage at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-
Payment/HomeHealthPPS/HH-PDGM.html
Medicare Benefit Policy Manual, Chapter 7, Home Health Services at:
https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c07.pdf

MLN Matters SE19027 Related CR N/A
Page 10 of 10
DOCUMENT HISTORY
Date of Change Description
October 25, 2022 We revised the Article to add a link to SE19028 for current information
on the PDGM. All other information is the same.
November 25, 2019 Initial article released.
Disclaimer: Paid for by the Department of Health & Human Services. This article was prepared as a service to the public and is not
intended to grant rights or impose obligations. This article may contain references or links to statutes, regulations, or other policy
materials. The information provided is only intended to be a general summary. It is not intended to take the place of either the
written law or regulations. We encourage readers to review the specific statutes, regulations and other interpretive materials for a full
and accurate statement of their contents. CPT only copyright 2018 American Medical Association. All rights reserved.
Copyright © 2013-2019, the American Hospital Association, Chicago, Illinois. Reproduced by CMS with permission. No portion of
the AHA copyrighted materials contained within this publication may be copied without the express written consent of the AHA. AHA
copyrighted materials including the UB-04 codes and descriptions may not be removed, copied, or utilized within any software,
product, service, solution or derivative work without the written consent of the AHA. If an entity wishes to utilize any AHA materials,
please contact the AHA at 312-893-6816. Making copies or utilizing the content of the UB-04 Manual, including the codes and/or
descriptions, for internal purposes, resale and/or to be used in any product or publication; creating any modified or derivative work of
the UB-04 Manual and/or codes and descriptions; and/or making any commercial use of UB-04 Manual or any portion thereof,
including the codes and/or descriptions, is only authorized with an express license from the American Hospital Association. To
license the electronic data file of UB-04 Data Specifications, contact Tim Carlson at (312) 893-6816. You may also contact us at
ub04@healthforum.com
The American Hospital Association (the “AHA”) has not reviewed, and is not responsible for, the completeness or accuracy of any
information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the
analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent
the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
