
NATIONAL HEALTHCAREER
ASSOCIATION
Certified Patient Care Technician
Study Guide
This document is property of the
National Healthcareer Association.
This cannot be reproduced for any
reason without written consent of the
National Healthcareer Association.

2
TEST INSTRUCTIONS AND PROTOCOLS:
Please take note of the following test protocols that will be in effect the day of your exam:
1. USE ONLY A #2 PENCIL.
2. Your full name, test ID and social security number must be clearly printed on the answer sheet in the
appropriate boxes, as well as on the sign in sheet along with your complete mailing address. We must
have a complete mailing address or we cannot process your exam and certifications.
3. Do Not write on the test booklet write only on the answer sheet. Anyone caught writing in the test
booklet will be fined and risks being removed from the exam!
4. Please refrain from eating or drinking in the testing room.
5. Use of: beepers, radios, cellular phones, watch alarms, translators, dictionaries and all other electronic
devices are prohibited in the testing room. Please turn all electronic communications OFF.
6. Cheating of any kind will not be tolerated, including but not limited to: consulting text books, notes or
web sites; discussing or reviewing any items on the exam with anyone else during the exam period; and
talking to other students during the exam. If the exam monitor suspects anyone of talking or cheating
during the exam, the monitor has the right to remove you from the testing room. You will have to retake
the exam and be responsible to pay full price again to retest.
7. You should answer every question on the exam. If you are unsure of the correct answer, try to eliminate
incorrect answers and take your best guess.
8. Test results will be sent to you via mail. Please do not call the office for results; the NHA will not
release grades on the telephone. Please allow approximately 30 days after the test date.
9. In order to achieve National Certification, you must receive a minimum grade of 70%. If you earn a
grade below 70%, you will be required to retake the exam. You will be notified via mail of the next
available testing dates and locations.
10. The monitor will not answer any questions once the exam begins.
11. Please use the restroom facilities before the exam begins, you will not be allowed to leave the test room
again until you complete the exam.
SPECIAL ACCOMMODATIONS
Special exam accommodations are available for persons with disabilities or other special needs. The
participants or their representatives can submit a request, in writing, to the National Healthcareer Association.
The request should include an explanation of the disability and the participants‟ specific requirements. Special
accommodations may include additional testing time, use of a private room or physical assistance in completing
the examination. If you have questions about special accommodations, please call the NHA‟s Corporate Office
at 1-800-499-9092. Requests for special accommodations must be submitted to the NHA at least 45 days prior
to the exam date and may be sent via certified mail or faxed to our corporate offices.
EXAM CHALLENGES:
If you believe a question on an exam was misleading, unfair or contained errors, you may submit an exam
question challenge. Any challenges to exam questions must be submitted in writing to NHA‟s Corporate
Office. Challenges to exams must be submitted within 5 business days of the completion of the exam. No
action can be taken on exam challenges submitted after that date, and no challenge will be considered viable
unless submitted in writing to our Corporate Office. This policy allows everyone to benefit from any legitimate
challenges before grades are posted, while avoiding any unreasonable delays in the NHA‟s ability to process
and deliver participants‟ grades.
The NHA does not provide individual responses to challenges; however, every challenge is considered and
acted on accordingly. Exam challenges may be faxed to NHA, Attn.: Cynthia Orr, (973) 644-4797, or may be
sent via overnight courier to the following address:
National Healthcareer Association Attn.: Cynthia Orr7 Ridgedale Avenue, Suite 203 Cedar Knolls, NJ 07927

3
TABLE OF CONTENTS
Topic
Page
Instructions to the Exam Taker
2
Medical Terminology
4
Anatomy and Physiology
5
Ethics and Legal Considerations
6
OSHA and Infection Control
7
General Patient Care
9
Medical History and Patient Interview
9
Physical Examination and Vital Signs
11
Assisting in a Medical Facility
15
Elimination and Sample Creation
17
Oxygen and Respiratory Assistance
18
Surgical Patient and Wound Care
19
Anatomy of the Heart
20
Basic Concepts in EKG Recording
26
Phlebotomy – Duties and Responsibilities
41
Special Phlebotomy Procedures
48
PRACTICE EXAM BEGINS
50 Questions – Multiple Choice – Necessary to Study for Exam
50
Answer key for practice exam
60-61
4
Thank you for choosing the NATIONAL HEALTHCAREER ASSOCIATION as your certifying agency. The
Certified Patient Care Technician exam consists of 200 multiple-choice questions. The Certified Patient Care
Technician exam will include competencies in Patient Care, Phlebotomy, EKG, Terminology/Anatomy, and
some ethical or legal considerations.
The following study guide is meant to assist you in focusing on concepts tested in the certification exam. It is
not intended to replace instruction and/or experience necessary for successfully completing the exam. Should
you find that a lot of the information shown below is not information you feel you are sufficiently prepared in,
or you cannot find answers to a lot of the questions below, you may want to purchase and utilize the “Review
Classes” as shown on a prior page in this packet, which gives a more in depth discussion on the concepts.
Part 1 -General Medical Information
A. Medical Terminology
Medical Terminology derives from Greek and Latin words. These words are formed by four main
components (Root, Prefix, Suffix and Links). The root is the most important part of the medical word (a
noun or a verb). Prefixes are small words placed in front of the root defining it as an adjective or an adverb.
Suffixes are small words at the end of the root that modify the root. All these elements are connected with
vowels (o, e, u, etc) called links.
Important Prefixes:
1. A, An = No, none 10. Inter = Between
2. Auto = Self 11. Brady = Slaw
3. Dia = Complete, through 12. Tachy = Fast
4. Endo = Inside 13. Dys = Bad, painful
5. Exo = Outside 14. Hemi = Half
6. Epi = Supra = Above 15. Pre = Before
7. Sub = Infra = Below 16. Retro = Behind
8. Hyper = More than normal
9. Hypo = Less than normal
Important Suffixes:
A. Diagnostic Suffixes: B. Surgical Suffixes:
1. –opsy = direct visualization 1. –centesis = puncture = piercing
2. –scopy = observing with a machine 2. –tomy = cision = cut
3. –graphy = record with an image 3.-ectomy = excision = cut & remove
4. –gram = record with a pen 4. –stomy = opening of a mouth like
5. –lysis = destruction, break down
6. –plasty = repair
7. –rrhaphy = suture = stitches
Important Pathology Suffixes:
1. –algia = -dynia = pain 6. –megaly = enlargment
2. –pathy = disease 7. –malacia = softening
3.-itis = inflammation 8. –osis = condition
4. –oma = tumor 9. –penia = deficiency
5. –carcino = malign tumor 10. –sclerosis = hardening
5
D. Important Abbreviations:
1. FUO = Fever of Unknown Origin 13. GTT = Glucose Tolerance Test
2. H & H = Hematocrit / Hemoglobin 14. MI = Myocardial Infarction
3. IV = Intravenous 15. I & D = Incision and Drainage
4. C & C = Clean Catch urine 16. I & O = Intake and Output
5. RBC = Erythrocytes 17. NPO = Nothing by mouth
6. WBC = Leukocytes 18. NPT = New Patient
7. BP = Blood Pressure 19. NYD = Not Yet Diagnosed
8. CDC = Center of Disease Control 20. S/R = Suture removal
9. CHF = Congestive Heart Failure 21. STAT = Immediately
10. CPE = Complete Physical Exam 22. UA = Urinalysis
11. CBC = Complete Blood Cell Count
B. Anatomy and Physiology
Anatomy is the science that studies the structure of the human body. Physiology is the science that studies
the function of the human body. Cell is the basic structural and functional unit of the human body. There are
three main features of the cell: Membrane, a double layer of phospholipids that protects the cell and
exchanges substances with the environment. Cytoplasm, the inner matrix, where all the chemical reactions
occur and and a nucleus, which is a safe for the DNA and genes used for reproduction and reconstruction of
the cell itself. Tissue is defined as a group of similar cells performing a specific function. There are four
tissues in the human body:
a. Connective tissue: The universal organ glue and the connection used by other tissues. It includes
tendons, cartilages, bone, etc. Blood is a connective tissue.
b. Epithelial tissue: The coverage of all hollow organs, including blood vessels and the heart, as well other
organs such as glands, liver, pancreas etc.
c. Muscular tissue: The tissue of movement and contraction. There are three types of muscular tissue.
Skeletal striated muscle that voluntarily moves bones. Cardiac muscle that contracts and circulates
blood. Smooth muscle that moves blood and food by involuntary periodic contractions.
d. Nervous tissue: The tissue that transmits analyzes and coordinates electrical impulses in response to the
changes of the outside environment.
An organ is a combination of different tissues, performing complicated and specialized functions. A group
of similar organs form a system. The cardiovascular system includes heart and blood vessels (arteries,
capillaries, and veins). The respiratory system includes pharynx, trachea, bronchi and lungs. All the systems
of the human body work in harmony and coordination is realized by the nervous system and the endocrine
system.
Homeostasis is a complex set of processes continuously working to maintain the stability of the inner body
environment (blood and tissues), despite the changes imposed from the outside environment. Homeostasis
includes the maintenance of temperature, blood pH, blood glucose levels, blood‟s electrolyte levels and the
body fluid volume and concentration. Diseases change and disrupt this homeostasis.

6
Important Positional and Directional Terms: Main Regions of the Human Body
1. Anterior = Front 1. Capitis (head)
Posterior = Back 2. Cervical (neck)
3. Upper Limbs
2. Superior = Above 4. Thorax (chest)
Inferior = Below 5. Abdomen (belly)
6. Pelvic (basin)
3. Proximal = Close to the point of attachment 7. Lumbar (flank)
Distal = Far from the point of attachment 8. Lower Limbs
9. Sacral (birth canal bone)
4. Medial = Close to the midline 10. Coccygeal (tail)
Lateral = Close to the side
5. Dorsal = Back
Ventral = Prone = Belly
C. Ethics and Legal Considerations .
Ethics are standards of right and wrong that regulate the behavior of any professional in their daily activities and
communication. PCTs are required to have the highest ethical standards.
Law is defined as a regulation or action enforced by a controlling authority, such as local, state and federal
government. A tort is defined as a civil wrong committed against a person or property that causes damage or
deprives someone of his or her personal liberty and freedom. Torts are punishable by law.
Some intentional torts are:
Assault: an open threat of bodily harm to someone
Battery: any body contact made without permission
False imprisonment: unlawful restraint or confinement of one person from another
Invasion of privacy: an interference with the person‟s right to be left alone
Negligence is an unintentional tort. Negligence is charged when a health care professional fails to provide ordinary
and standard care and the patient suffers injuries. As a tort, negligence is punishable by law.
Patient’s Bill of Rights was created in 1973 and revised in 1993. Patient‟s Bill of Rights is a list of standards that a
patient can expect from any health care provider. Preserving the confidentiality of a patient is one of the main
requirements of the Patient‟s Bill of Rights. Patient‟s Confidentiality is also at the foundation of HIPAA (Health
Insurance Portability and Accountability Act).
HIPAA is a US law designed to provide privacy standards to protect patients‟ medical records and other health
information provided to health insurance agencies, doctors, hospitals and other health care providers, while
transmitted or recorded by electronic or other media.
Informed Consent involves the patient‟s right to receive complete information and understanding relative to his or
her condition and the obligation to make decisions and cooperate in his or her treatment based on this knowledge.
The person that signs the informed consent must be legally and mentally healthy and responsible.
Implied Consent is a self-understood action of permission not expressed in words or in writing. Extending an arm
for blood withdrawal, to a health care provider, is an example of the implied consent.
Advance Directives or Advanced Health Care Directives are instructions given by individuals specifying what
actions should be taken for their health in the event that they are no longer capable to make the proper decisions due
to an illness or incapacitating condition. A living will and Power of Attorney are also forms of advance directives

7
and usually cover specific directives as to the treatment provided by caregivers. Abuse of any person who is
incapable of self-protection is punishable by law. It may include children, adults or the elderly. Abuse could be
physical, psychological or sexual. A patient‟s confidential rights are waived when a report of abuse is made. If you
suspect a child or any individual is abused, neglected or maltreated, relay your suspicion to the physician.
Chain of Custody reflects a timed written record of different individuals who have custody of a test or item from its
initial acquisition until its final deposition in court as evidence.. For medical test results the chain is maintained until
there is an official disclosure of the results.
D. OSHA Regulations and Infection Control
1. OSHA (Occupational Safety and Health Administration) requires basic safety practices to protect any
employee in the working place from different types of hazards
Biological Hazards: damage caused by infectious agents such as bacteria, viruses, fungus, or
other parasites. Allergic reactions are part of the biological hazards and can be caused by different
allergens. Latex sensitivity can cause allergic reactions ranging from simple dermatitis to
anaphylaxis.
Chemical Hazards: damage is caused by different chemicals used in the medical laboratory.
There is possible exposure to toxic, carcinogenic or caustic substances in the medical lab and
offices. All chemicals and reagents, containing hazardous ingredients in a concentration greater
than 1%, must have a Material Safety Sheet (MSDS) on file in the laboratory. The MSDS contains
information on physical and chemical characteristics; fire, explosion, reactivity, and health
hazards; primary routes of entry, exposure limits and carcinogenic potential; precautions for safe
handling; clean-up and emergency first aid information.
Radiological Hazards: damage caused by radiating X-rays or atomic particles. Radiation is used
widely in the medical field for diagnostic and therapeutic purposes. Radiation it is not recognized
by the senses and must be detected by specialized equipment.
Electrical Hazards: high-voltage equipment can cause burns and shock. Simple steps, such as
avoiding extension cords, grounding and maintaining electrical equipment, drying hands before
using electrical equipment and positioning electrical devices away from sinks, faucets and other
sources of water can prevent electrical injuries.
Fire or explosive Hazards: Bunsen burners, oxygen and chemicals can cause burns or
dismemberment. To prevent damage from fire you should know and follow the policies of the
office. You should know the routes of exit and evacuation and remember the word RACE (R =
Rescue persons immediately in danger, A = Alarm the nearest fire alarm, C = Confine the fire
closing doors and windows, and E = Extinguish a small fire and stop it from spreading).
Physical Hazards: wet floors, heavy lifting can cause falls, sprains and strains. To avoid
physical injury you should wear proper attire, walk do not run in the office or laboratories
unless it is an emergency, do not overextend your reach, use the transportation belt while
transporting a patient, lift with your legs when lifting heavy objects, etc.
2. Infection, Body Protection and Infection Control
Infectious diseases are damages to the tissues or organs resulting from the activity or presence of living
micro-organisms. Infection is a result of the interaction between the human body‟s defense mechanisms and
the microorganisms. A pathogen is defined as a disease causing microorganism Infections acquired in a
medical environment are called nosocomial infections. The goals of infection control are to limit or prevent
the presence of infectious agents, to create barriers against transmission and to reduce the risk to other
individuals of being infected.

8
The chain of infection is as follows:
Agent ---------Reservoir Host-------- Mode of transmission ------- Susceptible host
: :
: :
Portal of exit Portal of entry
Agents- are infectious microorganisms.
Reservoir Host-is the person that keeps the disease alive and transmits it to others. Sick individuals are
the most common reservoir host.
Portal of exit- the method by which an infectious agent leaves its reservoir. Standard Precautions and
Transmission-Based Precautions are control measures aimed at preventing the spread of the disease as
infectious agents exit the reservoir.
Mode of transmission- specific ways in which microorganisms travel from the reservoir to the
susceptible host. The direct way of transmission is from one person to another. The indirect way of
transmission is from a person to an animal (vector) to a thing (fomite) to another person.
Portal of entry- allows the infectious agent access to the susceptible host. Common entry sites are broken
skin, mucous membranes, and body systems exposed to the external environment such as the respiratory,
gastrointestinal, and reproductive.
Susceptible host- the infectious agent enters a person who is not resistant or immune. Control at this
level is directed towards the identification of the patients at risk, treat the underlying condition of their
susceptibility, or isolate them from the source of infection.
Immune system is the main body defense mechanism against infection.
To prevent the spreading of infectious diseases to large populations the CDC (Center for Disease
Control and Prevention) has issued a number of guidelines that have enabled health care professionals to
practice responsible infection control. The CDC has developed isolation categories for patients with
known infectious diseases. This category system includes strict isolation, respiratory isolation to prevent
air borne (droplet) spread of infection, protective isolation, enteric precautions, wound and skin
precautions, and discharge precautions.
Universal Precautions (Universal Blood and Body Fluid Precautions) are infection control practices used
to prevent blood borne infections.
Standard Precautions intend to protect all health care providers, patients and their visitors or family
members from infectious diseases. Following is a summary of CDC‟s Universal Precautions and
guidelines for control of blood borne infectious diseases (Hepatitis B, HIV etc):
Some of most important Universal Precautions guidelines are:
1. Consider all the body fluids from any patient as if they are infected or contaminated.
2. Wash your hands for up to 2 min before wearing, and after removal, of gloves used in a procedure
with body fluid contact. The best way to prevent any infection is through proper hand washing.
3. Always wear gloves when handling body fluids, body tissues, mucous membranes, damaged skin or
contaminated equipment. If gloves are damaged immediately wash your hands and wear a new pair
before you continue the procedure.
4. Wear PPE equipment in cases of a high risk of splashing or exposure to droplets from body fluids.
5. Never recap a needle. Always cover the used needle with the protective device and dispose it
immediately into a biohazard sharp container.
6. In cases of body fluid spills spray the spill first with a disinfectant or most frequently with 10% bleach.
7. Always properly dispose soiled soft materials into biohazard bags or boxes.
8. Properly report needle stick injuries, splashes, and wound secretion contact and contamination
9. Health care workers with open wounds or lesions, dermatitis or other infectious diseases should avoid
direct contact with the patients.

9
10. All the health care workers in contact or at risk of body fluid contamination should be vaccinated for
Hepatitis B virus.
3. Personal Protective Equipment (PPE): includes gloves, eye and facial protection, protective clothing
and resuscitation equipment.
a. Gloves: are used to protect against contact with infected body fluids, mucous membranes, non
intact or damaged skin, contaminated surfaces, equipment and instruments or when performing vascular
access procedures such as phlebotomy.
b. Mask and Facial Protection are required whenever there is a potential of splashing, spraying or
splattering of contaminated body fluids, such as centrifugation (equipment used to divide particles by
spinning and on their weight).
c. Protective Clothing must be worn whenever splashing or splattering to skin or clothing may
occur. They include hats, gown and boots (shoe coverage).
Part II - General Patient Care
1. Patient Identification:
Patient Identification is the process of verifying patient‟s identity and is the first and most important
step of any medical examination, procedure or specimen collection. Misidentifying a patient can be
ground for dismissal or can be lead to a malpractice law suit. There are three important ways of
identifying a patient:
a. Verify the name and Date of Birth (DOB): Ask the patient to state his or her full name and/or
date of birth. Ask “What is your name”, and never ask “Are you Mr. Smith?”.
b. Checking Identification Bracelets (ID Band, Wrist Band): In patients usually are required to
wear and ID band on the wrist. The typical ID bracelet contains patient‟s name and DOB and
hospital/facility ID number or Medical Record (MR) number. The patient Name, DOB, MR
number, and ID number must always match the information on the chart or test requisite.
c. 3-Way ID: This is a way to avoid identification errors or mislabeling, in which the patient is
identified by three means: the patient‟s verbal identification, check of the ID band, and a visual
comparison of the labeled specimen with the patient‟s ID band before leaving the patient‟s
bedside.
d. Emergency Room (ER) ID Procedures: This is a common procedure used for unconscious
patients or for those without identification. The procedure involves attaching a special three-part
identification band, such as Typenex Blood Recipient ID Band (Federal Laboratory a division of
Travenol Laboratories, Deerfield, IL) to the unidentified patient. All the three part contain the
same ID number. The first part becomes the patient‟s ID band, the second part is attached to the
specimen, and the third part is used if the patient needs a transfusion and is attached to the unit of
blood.
2. Medical History and Patient Interview
Interviewing the patient to obtain his or her medical history is the primary step of the medical
examination. The information from the medical history together with the Physical Examination data
enables the physician to form a diagnosis and a treatment plan for the patient.
Symptom: is a relevant complaining of the patient. It is a sensation that is only perceived by the patient.
Clinical Signs: is a finding or a change detected by the doctor or medical personnel during a physical
examination.
Chief Complaint: the patient states as the reason for seeking medical care. Chief complaint is a
symptom.

10
History of Present Illness (HPI): is a detailed in time description of detailed changes of the chief
complaint.
Past Medical History: any and all health problems present and in past, including procedures or taken
medication.
Family History: health history of the family members (Mother, father, brother aunt, etc).
Social and Occupational History: includes marital status, sexual behaviors and orientation, occupation,
hobbies, use of chemical substances, etc.
Review of Systems (ROS): is the part completed by a physician and is a review of all and each of the
body systems.
Etiology: the cause and the origin of the disease
Diagnosis: the process of identifying the nature and the cause of a disease.
Differential Diagnosis: a list of potential causes of the disease.
Prognosis: a prediction of the probable course and outcome of a disease.
3. Recording the Patient’s Medical History (Interview) When recording the patient‟s
medical history you must do more than just fill out the form. You must review, organize and determine
the importance of the information and document the facts. The “PQRST” is a good example interview
technique based on the chief complains:
P = Provoke: provoke the patient to reveal the cause of the main symptom.
Q = Quality: describe the nature of the complaint, its features, rate in a scale.
R = Region: where the complaint is located, where it spreads.
S = Signs Associated: complains associated with CC (nausea, vomiting etc).
T = Time: time of the onset of the CC, intermittent (comes and goes) or continuous,
the lasting time,etc.
b. 6 Cs of Charting: Clint’s words: record the exact words of the patient.
Clarity: use the precise medical terminology.
Completeness: record all the important information.
Conciseness: cover as much information in few words.
Chronological: arrange the information in timely manner.
Confidentiality: Protect the patient‟s private information.
c. Methods of Charting:
1. SOAP: defines the steps in Charting of the patient‟s information.
Subjective: Patient interview
Objective: Physical examination and test results
Assessment: defining the diagnosis from both the above findings
Plan: planning the treatment options, consultations, other lab examinations, etc.
2. Methods of Chart Recording:
a. SOMR (Source Oriented Medical Records): information recorded based on who provided the data,
patient, physician, nurse, paramedic, etc.
b. POMR (Problem Oriented Medical Records): used in large medical facilities when the patient is
seen by more than one physician. It includes a problem list designated to each of the patient conditions,
a treatment plan, and progress notes.
c. Computerized Medical Records: is a combination of SOMR and POMR methods and provides
accessibility to other health professionals beside physicians.

11
3. Physical Examination and Vital Signs
Physical Examination is the objective evaluation of the human body to determine its state of health or
diseases. It is a complete and through investigation for signs of diseases. Physical exam together with
the medical history help to formulate a differential diagnosis (a list of potential symptoms‟ causes and
diseases) laying the foundation for the definitive diagnosis.
Complete Physical Examination: includes vital signs and body measurements, examination of all
the body systems. It starts at the head and proceeds all the way to the toes.
Examination Methods:
a. Inspection: visual examination of the body by using eyes or lighted instruments.
b. Palpation: examination of the body using the sense of touch. There are two types of palpation: light
or superficial and deep.
c. Percussion: tapping with the fingers to obtain information from body organs and parts through the
returning sound produced by them. Used to evaluate heart, lungs and abdominal organs.
d. Auscultation: listening directly (ears) or with the help of an instrument (Stethoscope) of the body
sounds. Auscultation is used to evaluate heart, vessels, lungs and abdominal organs.
e. Manipulation: movement of extremities and other body parts for diagnostic purposes. Mainly used
to check the musculo-skeletal system.
f. Mensuration: the process of measuring different body parts and extremities. Used to assess height,
weight, head circumference, limbs circumference and etc.
Examination Equipment:
Gloves,Tongue depressor,Anoscope,Speculum,Thermometer,Otoscope,Ophthalmoscope,
Stethoscope, Tuning fork, Laryngeal mirror, Examining Light, Tape meter and a
Sphygmomanometer
Patient Positioning is crucial in placing the patient or his or her body part in a position that could be
better and comfortably examined.
1. Sitting Position: The patient is sitting at the edge of the examination table without any support. This
position is used for examinations of head, neck, chest and upper extremities.
2. Supine Position (recumbent): The patient is lying flat on the back, face looking upward. This
position is used for examinations of the head, neck, chest, upper and lower limbs.
3. Dorsal Recumbent Position: The patient is lying on the back, face up, flexed knees, with feet soles
flat on the table. It is an abdominal muscle relaxing position, but is also used for the examination of
chest, arms and lower extremities.
4. Lithotomy Position: The patient lying on the back, knees flexed and legs are placed above the chest
on stirrups and wide apart. This position is used to examine vaginal and perineal areas.
5. Fowler’s Position: The patient is lying on the back. The table head part is tilted usually in 45 degree
angle (can be tilted up to 90 degree angle). This position is used to examine head, neck, chest and
extremities, but is mostly used for patients experiencing dyspnea (difficult and painful breathing) or
with lower back injuries.
6. Trendelenburg’s Position: The patient is lying supine (on the back) on a tilted table with the head
positioned lower than the legs. Is mostly used to tread hypovolemia (low blood volume), hypotension
(low blood pressure) or shock, and in some surgical procedures.

12
7. Sims’ Position (Lateral/ on the side): The patient is resting on the left side, with left leg slightly bent
at the knee and thigh levels, and the left arm bent toward the head. The patient weight is supported by
the chest and both left limbs.
The right (opposite leg) is bent in a 90 degree angle and ensures a large base of support. This position is
used for examinations of pelvic and perineal areas.
8. Prone Position: The patient is placed on the belly, face down and turned on the side; arms are placed
on the side of the body or bent at the elbow and placed under the chest. This position is used to examine
the back of the patient.
9. Knee-Chest Position: The patient rests on the knees and the chests, with thighs slightly separated and
face looking on the side. This position is usually used for rectal and perineal examinations. A fenestrated
drape is used and should cover under the arms up to the knees.
10. Proctologic Position: The patient is bent at the hips at 90 degree angle. The head is placed on the
side, and the arms are placed on the side of the body. This position is used for rectal and perineal
diagnostic and surgical procedures.
4. Vital signs
Vital signs measure body‟s most basic functions. They show the function of most important body systems
(brain, heart, vessels and lungs). Vitals signs are the first to change during diseases and injuries. They also
provide important clues about the patient progress and healing. Vital signs include Temperature, Respiratory
rate, Pulse and Blood pressure. Vital signs are closely related to each other so if one of them changes the others
change too.
1. Temperature: Body temperature is a balance between heat production and heat loss. The center of
temperature control is located in a part at the base of the brain called Hypothalamus. Thermometers are used
to measure temperature using the Fahrenheit and Centigrade or Celsius scales. Temperature sites are the
following: mouth, rectum, ear (tympanic membrane), and the axilla (armpit). Normal temperatures measured in
different regions are as follows:
Site Normal Range
Rectal 98.6 F to 100.6 F (37.0C to 38.1C)
Oral 97.6 F to 99.6 F (36.5C to 37.5C)
Axillary 96.6 F to 98.6 F (35.9C to 37.0C)
Tympanic membrane 98.6 F (37C)
Fever: is an increase of body temperature above normal rage (98.6 degree F or 37 degrees C), a defense
mechanism that increases the body defense, kills many microorganisms and promotes healing. Very high fever
can have damaging consequences for the brain and the body, especially in children. Besides infection fever can
be caused by heat stroke, brain damage, neoplasms, allergies, etc.
Pyrexia: Is a fever above 104 degrees F (38 degree C)
Hyperpyrexia: is a fever above 105 degree F (41 degree C). Fever above this limit is generally fatal.
Hypothermia: is a body temperature lower than 97 degree F (36 degree C).
Afebrile: having normal body temperature.
Febrile: having fever.
Types of fever are:
Intermittent: fluctuating fever that returns to or below baseline, then rises again.
Remittent: fluctuating fever that remains elevated; it does not return to baseline temperature.
Continuous: a fever that remains fairly constant above the baseline; it does not fluctuate.

13
Oral temperature is the most common method of measurement; however it is not taken from non cooperating
patients (under 6 years‟ old children, convulsion and hemiplegic patients), and patients with facial surgery,
receiving oxygen, or with nasogastric tubes.
Rectal temperature is taken when oral temperature is not feasible. However, it is not taken from the following
patients with lower gastro intestinal problems (rectal surgery or disorders, patients with diarrhea, etc) as well in
patients with cardio-pulmonary disorders that will be aggravated by the position. Rectal temperature is
considered by the majority of the physicians as the most accurate method of temperature measurement.
Axillary temperature is the least accurate and is taken only when no other temperature site can be used.
Tympanic temperature is useful for children and confused patients because of the speed of operation of the
tympanic thermometer. A covered probe is gently inserted into the ear canal and temperature is measured
within seconds (1 – 3 seconds). It is not used if the patient has an ear infection, disorder or ear drainage.
2. Respiration: is the act of breathing, inhaling and exhaling of gases for energy. When measuring respiration,
respiratory characteristics such as rate, rhythm, and depth are taken into account. The control center for
breathing is in the medulla oblongata.
The ways to check the respiration are by watching the movement at the patient‟s chest, back, abdomen, or
shoulders, by palpation placing the hands over the patient back and feel the movement of the chest, and by
listening with a stethoscope of the respiratory sounds.
Rate (RR) is the number of respirations per minute. The normal range for adults is 12 to 20 per minute. One
inhalation and one exhalation counts for one respiration. It is counted for 30 seconds multiplied by two or for a
full minute.
Some rate abnormalities are the following:
Apnea – this is a temporary complete absence of breathing which may be a result of a reduction in
the stimuli to the respiratory centers of the brain.
Tachypnea – this is a RR rate of greater than 40/min. It is transient in the newborn and maybe
caused by the hysteria in the adult.
Bradypnea – is a decrease in numbers of respirations. This occurs during sleep. It may also be due
to certain diseases.
Depth of respiration refers to the amount of air that is inhaled and exhaled during each respiration. Some
abnormalities in the depth of respirations may include the following:
Hypoventilation: Slow and shallow respiration.
Hyperventilation: Rapid and deep breathing.
Dyspnea: Difficult and painful breathing
Orthopnea: difficulty in breathing when lying down.
Respiratory rhythm refers to the pattern of breathing. It can vary with age: infants have an irregular rhythm
while adults have regular. Cheyne-Stokes is a type of abnormal respiratory rhythm with an irregular breathing
rate.
3. Pulse: is defined as the rhythmical throbbing of arteries produced by the regular contractions of the heart, that
helps propel the blood toward the tissues and reducing the vascular resistance.
Pulse rate: the number of times the artery beats in a minute. The normal adult pulse rate ranges between 60 and
100 beats per minute. Many factors influence the pulse rate, such as age, sex, body size, exercise, anxiety,
malignancy, pregnancy, and medications.
Tachycardia: is a pulse rate above 100 beats per minute (bpm).
Bradycardia: is a pulse rate below 60 bpm.
Besides the pulse rate the pulse measure can provide some information about the blood volume and pressure as
well as information about the arterial wall consistency.
Pulse site: the most commonly used pulse sites
14
Temporal artery: in front of the ear.
Carotid artery: in front of sternocleidomastoid muscle on the neck.
Apical pulse: located on the chest in the crossing of 5
th
intercostals and midclavicular line. It is the most
accurate pulse; it is heard by using the stethoscope. Apical pulse is used for patients with irregular heart rates
and for infants and small children.
Brachial artery: on the medial side of the arm above cubital fossa and is also used to measure blood pressure.
Radial artery: found in the groove on the thumb side of the wrist. It is the most common pulse rate measuring
site.
Pulse deficit: the difference between the apical and radial pulse rate.
Method of pulse evaluation: the pulse is felt with the first two or three fingers (never with the thumb) and
usually taken for 30 seconds multiplied by two to get the rate/minute. If he rate is unusually fast or slow,
however, count it for 60 seconds.
When the rhythm is irregular, the rate should be evaluated by cardiac auscultation because beats that occur
earlier than others may not be detected peripherally and the pulse rate can thus be seriously underestimated.
4. Blood Pressure
Blood pressure is the force of the blood pushing against the walls of the arteries. Blood pressure is produced by
heart contraction and blood volume. Arteries close to the heart have higher blood pressure than those far from
heart. Blood pressure is measured in millimeters (mm) of mercury (Hg). The measurement consists of two
components: the highest (systole) measuring the force of the heart muscle contraction, and lowest (diastole)
amount of pressure exerted during the cardiac rest and is related to blood volume before contraction.
Normal blood pressure depends on age as it is listed below:
Newborn 50/25
6 – 9 years 95/65
10 – 15 years 100/65
Young adult 118/76
Adult 120/80
Pulse pressure: is the difference between the systolic and diastolic pressure readings.
Heart Sounds: The first heart sound is produced by systole (heart contraction time) sounding like “Lubb” is
dull, firm and prolonged. The second produced during diastole (heart resting time), when the heart valves are
closed, is shorter and sharper “Dubb”.
Korotkoff’s or Blood Pressure Sounds: are the sound heard over the brachial artery after a complete
occlusion of the artery from the blood pressure cuff, when the pressure is released and the blood circulation is
restored.
Blood Pressure Equipment: A stethoscope and sphygmomanometer of either aneroid or the mercury type are
used to take the measurement.
Sphygmomanometer: is the instrument used to measure the blood pressure. It is build by a manometer (a scale
that registers the actual blood pressure reading), inflatable rubber bladder, cuff and a bulb. There are three types
of sphygmomanometer: mercury, aneroid and electronic. The mercury one is the most accurate, but because of
the mercury toxicity is not used frequently. The size of the cuff of the sphygmomanometer will depend on the
circumference of the limb and not the age of the patient. The width of the inflatable bag within the cuff should
be about 40% of this circumference – 12 cm to 14 cm in an average adult. The length of the bag should be
about 80% of this circumference – almost long enough to encircle the arm.
Cuff placement: The inflatable bag is centered over the brachial artery with the lower border about 2.5 cm
above the antecubital crease. The cuff is positioned at heart level. If the brachial artery is much below the heart
level the blood pressure will appear falsely high. If the brachial artery is much above heart level, blood pressure
will appear falsely low.

15
Method of measuring BP: Blood pressure is taken by determining first the palpatory systolic pressure over the
brachial artery. Inflate the cuff until there is no more pulse palpated over radial artery. The first beat of pulse
felt while releasing the pressure is the approximate systolic blood pressure. After completely release the
pressure of the cuff place the bell of the stethoscope over the brachial artery, the cuff is inflated again to about
30 mm Hg above the palpatory systolic pressure and deflated slowly, allowing the pressure to drop at a rate of
about 2 to 3 mmHg per second. Note the level at which you hear the sounds of at least two consecutive beats or
the first strong heart sound. This is the systolic pressure. Then deflate the cuff rapidly to zero. The
disappearance point, which is usually only a few mmHg below the muffling point, marks the generally accepted
diastolic pressure. Both the systolic and diastolic pressure levels are read to the nearest 2 mmHg.
Common errors in blood pressure measurements:
Improper cuff size: Cuffs that are too short or narrow may give falsely high readings. Using a regular
cuff on an obese arm may lead to a false diagnosis of hypertension. For an obese arm, select a cuff with
a larger than standard bag.
The arm is not at heart level. If the brachial artery is much below the heart level, the blood pressure
will appear falsely high. Conversely, if the artery is much above heart level, blood pressure will appear
falsely low. Cuff is not completely deflated before use.
Deflation of the cuff is faster than 2-3 mmHg per second. Rapid deflation will lead to underestimation of
the systolic and overestimation of the diastolic pressure.
The cuff is reinflated during the procedure without allowing the arm to rest for 1-2 minute between
readings. Repetitive inflation of the cuff can result in venous congestion which could make the sound
less audible producing artificially low systolic and high diastolic pressure.
Improper stethoscope placement.
Defective equipment.
A bag that balloons outside the cuff leads to falsely high readings.
5. Measuring the Human Body (Mensuration): most commonly measures the weight, height and head
circumference for infants. These measurements provide baseline data or normal data for the actual patient‟s
condition.
Part III - Assisting in a Medical Facility
a. Patient Admission, Transfer and Discharge
The medical record is a written account of a patient‟s condition and response to treatment and care. It is a
permanent legal document should be carefully recorded and updated according to law.
1. Admission: is the official entry of a patient into a health care facility. The admission process involves the
following important steps:
a. Completion of the admission records and patient identification.
b. Preparation of the room (open the bed; prepare the patient supply, etc.)
c. Completion of the Admission Check List: this is a standard form that provides a baseline assessment of the
new patient. The nurse is responsible for completing this checklist. This checklist includes three main areas of
information: patient‟s personal information; patient‟s condition on admission (disabilities, physical and mental
status, etc.); Baseline medical information (vital signs, list of medications).
The Graphic Sheet: is a special spread sheet used to record measurements and observations made every shift
or 3-4 times a day. Recorded are blood pressure, temperature, pulse, respirations, weight, I & O, and doctor‟s
visits.
Progress Notes: a record of the care given to the patient and contains:
Signs and symptoms

16
Special treatments/medications, procedures performed by the physician
Patient or resident teaching and counseling
Visits by other health care member
Flow sheets: are used to record frequent measurements or observations. Examples of these are: bedside I & O
and record of BP taken every 15 minutes.
Kardex is a type of card file that summarizes information found in the medical record such as diagnosis,
treatments, medications, routine care measures, and special needs.
Reporting is the oral account of care and observations.
Recording, known as charting, is the written account of care and observations.
Recording time: When military or international time is used, the terms a.m. and p.m. are dropped. Time is
recorded as multiples of 24 hours. The hour is the same for the morning, but when referring to the afternoon or
evening, 12 is added to the clock time. For example when referring to 3:00 pm, the correct recorded time is
15:00 or 1500 (read as 15 hundred hours)
2. Transferring is a procedure carried out according to the policies of the health care facility. These policies
ensure that there is no interruption in the patient care. A transferring form is a document that provides doctor‟s
authorization of the transfer and ensures that the patient‟s care plan is understood and well executed by the
medical personnel.
3. Discharge is a patient‟s authorized release form from a health care facility. A doctor‟s order is required for
any patient to be discharged. If a patient leaves the facility without the permission of a doctor, you should
immediately notify the nurse.
Discharging Plan is a document that outlines the ongoing patient care following the discharge. The plan
includes instructions and arrangements for home health care, physical therapy, special meals, and other services.
A nurse is responsible for the entire discharge process.
Discharge Instruction: is a written document that outlines the information about the continuing care. This form
summarizes the discharge plan, both the patient and the nurse are required to sign the instructions in duplicate to
verify that the information was explained and that the patient understands them. A copy of the instructions
remain in the patient‟s chart.
b. Bedding
Bath Blanket is a light weight blanket used to provide warmth and privacy when changing the bed while the
patient is in the bed.
Draw sheet is a small sheet that is placed over the middle of the bottom sheet that is used to lift or move the
patient in bed. When plastic is used, a cotton draw sheet must be used over the plastic. The plastic sheet should
never come in contact with the patient‟s skin, because it can cause sores.
Bed pads: are absorbent pads placed over the bottom sheet to protect the linen from becoming wet or soiled.
Disposable pads provide better infection control.
c. Patient Positioning, Draping, and Transfer
Positioning is a periodical changing in the patient‟s position to ensure physical comfort and general well-being.
It promotes better circulation, improves respiration, improves better drainage of the respiratory pathways, and
prevents deep vein clotting. It is also used in different procedures performed at the patient‟s bedside. (See the
different positions page)
Moving Patient’s Safely: The following are some of the most important guidelines to safely move or transport
the patients:
Know when to get assistance.
Use the proper body mechanics to lift patients. Never twist your body when lifting a patient.
Take your time to move slowly and carefully
Explain the procedure to the patient and ask for his or her cooperation.

17
Always maintain the patient„s privacy.
Make sure that there are no obstacles in the way during the transfer.
Make sure the wheels of the bed or wheelchair are locked.
Place one hand under the shoulder and the other under the thigh to safely lift and reposition the patient,
with the patient or another person‟s help.
Preventing Orthostatic Hypotension: Orthostatic Hypotension is a sudden drop in blood pressure when the
patient changes the position from a lying to sitting or standing up, with signs of dizziness or fainting. Bed rest
is the common cause of the orthostatic hypotension, but is also caused by diseases and medications. To prevent
this type of hypotension, assist the patient to slowly and gradually change the position, first from lying into
sitting, and after a while from sitting into standing up, allowing the body to adjust.
d. Elimination and Sample Collection
Besides helping and assisting the patient with elimination of urine and feces, the patient care technician should
also observe and report the changes of these excrements.
Urine observations include:
o color (normally pale or dark yellow);
o odor (normally slight urine odor, but fruity or sweet in diabetes, foul in infection)
o sediment (normally none or a little in female urine)
o clarity (normally clear, cloudy in proteinuria or infection)
o quantity
Stool observation include:
o color (normally dark brown, but tarry stools are a consequence of gastrointestinal hemorrhage or
melena)
o odor (normally a mild special odor)
o consistency (normally formed, watery in diarrhea)
o amount small, moderate or large.
The main rule on assisting a patient during elimination is to provide as much privacy as possible.
1. Assisting an Incontinent Patient
Incontinence is the inability of the patient to control his or her urination or defecation process. It is caused by
physical injuries (spinal cord injuries, perineal area damage), as well mentally by stress and anxiety. Patient
Care Technicians assist the patients to control and manage their incontinence and support their self-esteem and
dignity.
2. Assisting with Catheters
A catheter is a tube used to drain fluids into or out of the body. A urinary catheter is a tube used to drain
urine out of the bladder. A nurse or a doctor inserts the catheter through the urethra into the bladder. The urine
drains in a special bag. The catheter is secured by a balloon or a strap or adhesive tape to keep it in place.
Intermittent catheters are used to drain urine time to time, while permanent catheters are left in place for days
and weeks. When caring for a patient with catheters:
Always follow universal precautions and OSHA regulations
Make sure there are no kinks in the catheter or tubing that will prevent drainage.
The urinary bag should always be placed at a lower level than the bladder.
Never attach the bag to a movable part of the bed.
Provide perineal and catheter care to prevent infection. Always clean from the urethral exit to 4 inches
down on the catheter.
Avoid moving or pulling the catheter out.
Record the data periodically and accurately.

18
3. Collecting and Testing Urine and Fecal Samples
Routine Random Urine Sample: is collected from every patient entering the medical facility at any time and
without any special preparation.
Clean-Catch Urine Sample: is collected at midstream (voiding the first portion) and after the perineal area is
clean and disinfected properly. The patient should fill ¾ of the container. It is used for urine microbiology
studies.
24 Hour Urine Sample: it measures the urine production of the patient in 24 hours. A preservative is added to
the accumulated urine to prevent microbial growth. The patient voids the first urine in the morning before the
test to begin with an empty bladder. All portions of urine produced in 24 hours are added to the collection
container.
Stool samples are most frequently tested for presence of blood, fat, microorganisms, and parasites. Fecal
Occult Blood Test (FOBT) is a test used to detect the presence of hidden blood in stools. Patient Care
Technicians take a portion of some stools with a wooden spatula and places the sample into the specimen
container. Some specimens – especially those tested for parasites or their eggs – require warming to ensure
accurate test results.
e. Oxygen and Respiratory Assistance
Oxygen treatment and respiratory assistance are needed when a patient has the signs of hypoxia (the patient can
not maintaining the normal blood levels of oxygen).
Signs of hypoxia are:
Disorientation and confusion, fatigue and anxiety.
Increase in pulse and respiratory rate.
Bluish color seen in the lips, nose, ears, fingers and toes.
Difficult or painful breathing (dyspnea).
Some of the respiratory test most frequently used in hospitals and medical facilities to diagnose respiratory
problems or dyspnea are:
Chest X-Rays (CXR): studying the lungs‟ structure by using x-rays.
Lung Scans: evaluating the lungs‟ function and blood supply by using radioactive gases or injecting radioactive
substances into the venous blood.
Bronchoscopy: examining the respiratory pathways by using a special lighted tube.
Thoracocentesis: piercing the chest cavity with a needle and examining or evacuating the pleural fluid.
Collecting sputum specimen: is the process of collecting the mucus secreted from the respiratory pathways.
Pulmonary Function Tests: measuring the amount of air moving into or out of the lungs (spirometer).
Arterial Blood Gases (ABGs): a nurse or a respiratory therapist inserts a needle into an artery and collects and
analyzes the levels of oxygen in blood.
Pulse Oxymetry: measures the quantity of oxygen contained in the hemoglobin (RBCs oxygen transporting
protein). Normal values range from 95% to 100%. Values under 90 percent are considered hypoxia. To properly
measure the oxygen levels, the sensor of the machine should not be placed over swollen, damaged skin or part
of the limbs with a poor blood circulation. In children, the saturation levels are measured over the palms, fingers
or earlobes. For elderly patients the test is usually measured over the earlobes. In home care settings, this test is
measured and recorded together with the vital signs.
f. Assisting with Fluid and Electrolyte replacement
An adult needs minimum 1500 ml and up to 2500 ml a day to completely replenish his or her fluid losses. The
fluid and electrolyte daily requirements increase with hot weather, exercise, fever, illness, diarrhea etc. The
doctor orders the amount of fluid a patient requires during 24 hours.
Encourage Fluids: the person intakes an increased amount of fluid.
Restrict Fluids: fluids are limited to a certain amount. The fluids are offered in small amounts and in small
containers. The water pitcher is removed from the room or is kept out of sight. Intake records are kept and

19
placed in the patient chart. The patient needs frequent oral hygiene to keep the mucous membranes and mouth
moist and clean.
Nothing by Mouth: (Non Per OS NPO): it is usually ordered before and after procedures and treatments for
certain illnesses. NPO sign is posted in the room.
Intake and Output Records (I & O): The doctor or the nurse orders the intake and output measurements. This
is used to evaluate the fluid balance and the kidney function. All the fluids taken by mouth are measured,
including foods that melt at room temperature, such as ice-cream, puddings, gelatins etc. The body fluid out-put
such as urine, vomit, diarrhea and wound drainage are recorded, too. An I & O record is kept at the bedside,
every amount is recorded in the correct column, amounts are totaled at the end of the shift and placed in the
patient‟s chart.
IV Therapy: is giving fluids through a needle or a catheter inserted into a vein. Doctors order IV therapy to:
Provide fluids and minerals when the person can not take fluids by mouth
Replace water and minerals lost during illness or injury
Provide sugar for energy
Provide drugs for treatment
Intravenous Solutions: are classified as nutrient solutions (Dextrose 5 %) used for energy, electrolyte solutions
(Ringer 0.9 %) providing fluids and minerals, and blood volume expanders (dextran, plasma, serum) used to
replace blood in cases of severe acute blood-loss.
IV sites are divided into peripheral sites (usually veins of the hand, forearm and arm in adults, and scalp or
feet in children); nurses place the needle and the catheters and set up the infusion for peripheral veins and
central veins (subclavian and internal jugular veins). The doctor places the catheter in the central veins. IV
therapy is given in hospital, out-patient, long term care, and home settings. RNs are responsible for IV therapy.
They start and maintain the infusion according to the doctor‟s orders. State laws vary regarding the role of
patient care technicians in IV therapy. Patient care technicians do not regulate the flow rate of the perfusion
or change the IV solution containers. Patient Care technicians never give IV drugs. Patient care
technicians help meet the hygiene and the active needs of a person with an IV.
g. Surgical Patient and Wound Care
The roles of Patient Care technician in surgical patient care is to ease the patient‟s fear and anxiety and prepare
the patient before the surgery by following the doctor orders. Patient care technicians also take care of the
patients during the post-operative period.
Preoperative Skin Care: The process of cleaning and shaving of the surgical field is called “Skin prep”. In
most hospitals, the skin prep is performed the night before or the morning of the surgery. The nurse will tell you
which area to clean and shave, determined by the type of surgery and doctor‟s orders.
Post-operative Patient Care: The post-operative period is the time after the surgery that begins when the
patient is transported from the OR to the recovery room. The patient remains in the recovery room until the vital
signs are stable and the patient is fairly alert. The general post-operative care involves measuring the vital signs
every 15 minutes for the first hour, and thereafter is based on the nurse‟s orders. It involves assisting the patient
with elimination needs, recording of the first voiding or elimination after surgery, providing liquids when
permitted, checking the urinary catheter drainage and checking the wound drainage etc.
Assisting with patient’s Blood Circulation: are exercises and special devices used to prevent blood clots. A
blood clot inside a vessel is called a thrombus. A clot travelling through the blood stream is called embolus.
The methods used to prevent clotting in a post-operative patient are:
a. Anti-embolitic stocking are elastic stocks placed on the lower limbs that continuously squeeze the
superficial veins and promote the blood return into the heart.

20
b. Intermittent Pneumatic Compression Device is an inflatable cuff wrapped around the legs that are
periodically inflated and de-inflated by a pump compressing the superficial and deep veins and
promoting blood circulation.
c. Leg exercises passive or active movements of the legs stimulate the circulation by making the muscles
squeeze the veins and promote circulation and maintain the normal function of the articulations. Flexion
and extension exercises could be performed by the patients themselves or with the help of the patient
care technicians.
Wound Care: A wound is a break in the skin or mucous membranes. Wounds are of significant importance
because they can cause pain, need special care and may spread infection. The following are some types of
wounds:
1. Surgical wounds: openings of the skin and mucosa made to reach deep structures during a surgical
procedure
2. Traumatic wounds: these are injuries to the skin caused by trauma or accident.
3. Circulatory ulcers (vascular ulcers): these damages that appear in areas where there is a decrease in
blood supply.
4. Pressure ulcers (Decubitus): these result from poor skin care, low blood supply caused by unrelieved
pressure. Constant pressure, friction, and shearing cause the skin to break down and may result in
ulcers.
5. Document and report all your patient observations and care. Report if the patient is not eating or
drinking, if they are not getting out of bed and if you see a red area on the patient's skin.
Wound drainage: During wound healing, fluids and cells may ooze out of the tissues and depending on the
size and location of the wound; the drainage may be small or large. This fluid collection if it is not drained will
cause an excessive pressure on the wound margins delaying their closure and if infected will cause serious
problems to the wound and the patient. To prevent these serious complications doctors apply different types of
procedures to prevent or drain these fluid accumulations. The following are the different types of wound
drainage.
Serous drainage is clear and watery and does not contain blood cells.
Sanguineous drainage is bloody drainage. A bright color signifies fresh bleeding while dark bleeding
would be old.
Serosanguineous drainage is blood-tinged thin, watery drainage.
Purulent drainage is thick greenish, yellowish or brownish drainage.
The patient care technician will assist the doctor or the nurse in changing of the wounds and in the special skin
care involved. You should always follow universal precautions during these procedures. Record the findings or
notify the doctor or the nurse if the drainage fluid is changed.
1. Anatomy of the heart
A. External Heart Anatomy
The heart is a hollow muscular organ located in the thoracic cavity between the lungs (mediastenum), just
behind the sternum. One third of the heart is located on the right side and two thirds are located on the left. The
apex of the heart is located in the cross lines of left midclavicular and fifth intercostal space. The heart is
usually the size of the person‟s fist. The heart has two sides, right side that circulated deoxygenated blood
returned from the veins to the lungs (pulmonary circulation) and left side that circulated oxygenated blood from
the heart to the tissues via arteries. Cardiovascular system has arteries, capillaries and veins. Arteries are
defined as vessels coming outside the heart that deliver oxygenated blood to the tissues. Arteries have a thick
muscular wall, and they have pulse and blood pressure. Capillaries are microscopic blood vessels that connect
arteries with veins and feed the tissues with oxygen and glucose, and remove the toxins created by metabolism
(Co2). Capillaries have only an endothelial layer of cells. Capillaries have pores (small holes in their walls)

21
used for diffusion and cell movement outside the capillaries. Blood is mixed in tissue and pulmonary capillaries.
Veins are defined as vessels going back into the heart; they return the deoxygenated blood from the tissues.
Veins have a thin muscular layer, they have valves and a large lumen (hallow vessel space) to store the blood.
The largest veins returning blood into the heart are Vena Cava Superior and Inferior and Pulmonary Veins
(the only veins that transport oxygenated blood into the heart from the lungs). The largest arteries leaving the
heart are Aorta and Pulmonary Trunk (that divides into two pulmonary arteries). Pulmonary Trunk and
Pulmonary Arteries are the only arteries that transport deoxygenated blood into the lungs.
Internal Heart Structure
Layers of the heart
Endocardium - the innermost layer of the heart. It is a thin layer of epithelium very similar to
vessels‟ endothelium, which covers the inside part of the heart. It forms the lining and folds back
onto itself to form the heart valves and also covers the papillary muscles that anchor chordae
tendinae, strings of connective tissue that keep in place the AV valves. The function of endocardium
is to prevent blood cell destruction and clotting. The endocardium is also the layer in which the
heart‟s conduction system is embedded.
Myocardium - the middle and contractile layer of the heart. It is made up of special striated muscle
fibers with strong connection with each other (intercalated disks) and branches that ensure a unified
and simultaneous contraction of all the muscle fibers. There is a high concentration of calcium ions
in the space between the muscle fibers (interstitial space), which influences the force of the muscle
contraction.
“Heart Skeleton”- is made up of four rings of thick connective tissue. These rings which surround
the base of the heart and large vessels, create the cardiac septum, and provide a solid connection
between the heart chambers and a strong attachment for the heart valves.
Pericardium – is the outermost layer of the heart. Pericardium is attached with ligaments to the
spinal column and diaphragm fixing the heart in its position. Pericardium is built by two layers of
connective tissue. The outside layer is called parietal pericardium and the inner layer is called
visceral pericardium or epicardium. Two layers of pericardium are separated by a thin layer of fluid
to prevent friction. These layers and the fluid between them are referred to as the pericardial sac.
The Heart Chambers
A structure in the middle of the heart called the septum, divides the heart into two sides. The right side
pumps deoxygenated blood with low pressure from the veins into the lungs (pulmonary circulation) and
left side, that pumps oxygenated blood with high pressure (blood pressure) toward the tissues through
arteries (systemic circulation). The heart has four chambers: they are the right and left atria (smaller,
thin-walled chambers that are situated on top of the ventricles and receive blood from the lungs and
veins) and the right and left ventricles (larger, more muscular chambers that eject blood out to the
systemic circulation and to the two lungs).
Right Atrium receives deoxygenated blood returning to the heart from the body via the superior vena cava
which carries blood from the upper body and the inferior vena cava which carries blood from the lower
body. Right Atrium (RA) receives blood from the coronary sinus; the largest vein that drains the heart
muscle‟s deoxygenated blood.
Right Ventricle receives deoxygenated blood from the right atrium which it pumps to the lungs for
oxygenation through the pulmonary trunk and then to the pulmonary arteries.

22
The pulmonary arteries -- are the only arteries in the body that carry deoxygenated blood (because they are
going away from the heart).
Left atrium receives oxygenated blood returning from the lungs via the right and left pulmonary veins.
The pulmonary veins are the only veins in the body that carry oxygenated blood (because they are going
towards the heart).
Left ventricle receives the oxygenated blood from the left atrium and pumps it to the body through the aorta,
the largest artery of the body.
The chambers pump simultaneously – both atria contract together then the two ventricles.
Figure 2: Conduction System of the Heart *****
HEART STRUCTURE AND FUNCTION – ANATOMY OF THE HEART
The Heart Valves
The purpose of the heart valves is to prevent backflow of blood thereby assuring
uni-directional flow thru the heart.
A. The atrioventricular valves (AV): are located between the atria and ventricles. AV cusped valves
characteristics are:
They have tough fibrous rings
Long and strong leaflets (cuspids)
They have accessory organs, such as papillary muscles and chordae tendinae.
a.) Tricuspid valve is located between the right atrium and the right ventricle. As the name connotes, it
has three cusps (or leaflets).

23
b.) Bicuspid Mitral valve is located between the left atrium and the left ventricle. It has two cusps (or
leaflets) and it also called the mitral valve.
B. The semilunar valves: called semilunar because they have half-moon shaped leaflets, with the following
characteristics:
Three leaflets
Shallow in depth
They have no accessory organs
a.) Pulmonic valve – located between the right ventricle and the pulmonary trunk.
b.) Aortic valve - located between the left ventricle and aorta
Coronary Circulation
The right and left coronary arteries are the first branches coming out of Aorta and supply the heart with
oxygenated blood. The blood runs through these arteries during diastole. Coronary arteries are located
on the epicardium.
The left coronary artery has two branches Left Anterior Descending (LAD) artery and Left Circumflex
(LCX) artery. There is only one main artery that supplies the right side of the heart RCA (Right
Coronary Artery) artery.
Heart Physiology
Cardiac Cycle
Systole is the period of contractions of both Arial and Ventricles
Diastole is the period of relaxation and filling of all cardiac chambers.
Heart Sounds
Heart sounds are caused by the closure of the heart valves
S1 first heart sound (Lubb) occurs during ventricle contraction and the closure of AV valves.
S2 second heart sound (Dupp) occurs during ventricular relaxation when SL valves
(Pulmonary and Aortic valves) close. Murmurs are caused by diseases of the valves or other structural
abnormalities.
Heart Rate is the number of heart contractions per minute. The normal heart rate is 60 to 100 bpm (beat
per minute). HR is controlled by Chemo-receptors (chemical sensors) and Baro-receptors (pressure
receptors) located in Aortic Arch and Carotid arteries. The heart is under the influence by the autonomic
nervous system (ANS) which is subdivided into the sympathetic and parasympathetic nervous systems.
Parasympathetic (Vagus Nerve) generally has an inhibitory effect via the neurotransmitter
Acetylcholine which may cause the following to happen:
Slows SA pacemaker and HR
Slows the conduction of electricity in AV node
Decreases the strength of atrial and ventricular contraction

24
Sympathetic via the neurotransmitter Norepinephrine results:
Increases the HR
Increases the force of contraction
Increases the blood pressure
Via dopaminergic receptors increases the diameter of the visceral blood vessels and consequently
the visceral blood flow.
Heart as a Pump
The blood volume ejected outside the heart is equal to the blood volume returning back I into the heart.
Stroke Volume (Preload) is the blood volume ejected outside the ventricle after each contraction. The
stroke volume depends on
The volume of blood returning into the heart.
The force of the myocardium contraction
Vascular resistance (After Load)
Starling Law: “The greater the volume of blood inside the heart during diastole, the stronger the
heart contraction force during the systole. (Stroke Volume).
The other main factor influencing the stroke volume is vascular resistance (after load). The lower the
resistance in the vessels, the more easily blood can be ejected outside the heart through the circulation.
Cardiac Output:: The amount of blood ejected outside the heart per minute.
Cardiac Output = (Stroke volume) x (HR per/min)
Peripheral Vascular Resistance: Is the force exerted against the blood flow and is determined by the
diameter of the vessel. The lower the vascular resistance the less force is needed to eject the blood out of
the heart during systole.
Blood Pressure: The force exerted by circulating blood volume on the walls of the artery during
circulation.
BP = (Cardiac Output) x (Vascular Resistance)
Higher Cardiac output will result in a higher BP
High vascular resistance will also result in a higher BP.
Therefore, lower cardiac output OR lower vascular resistance will result in a lower BP.
Basic Electrophysiology
EKG = graphical presentation of heart electricity (voltage) over time. This electricity is created by specialized
cells called pacemaker cells. These cells generate electrical impulses spontaneously (without outside influence)
and rhythmically (automaticity). The electricity is created by passing of ions (charged particles) through the cell
membrane. The electricity is than conducted, transmitted to other specialized cells that together with the
pacemaker cells create the conductive system of the heart, the necessary wires and switches to stimulate cardiac
muscle fibers for a synchronized contraction.

25
Cardiac Cell properties:
Automaticity: the ability to spontaneously trigger electrical impulses without being stimulated by
another source.
Excitability: (also called irritability) the ability to respond and react to a stimulus
Conductivity: the ability to receive and transmit electrical impulses to adjacent cells.
Contractility: a myocardial cell‟s ability to shorten (or contract) in response to a stimulus.
Depolarization occurs when positively charged ions (such as sodium and calcium) rapidly move from outside
the myocardial cell membrane to the inside, changing the overall charge from negative to positive. This process
results in a “chain reaction” that spreads from cell to cell very rapidly. This electrical event is expected to result
in contraction. Depolarization flows from the endocardium to the myocardium to the epicardium (or from the
innermost layer to the outermost).
Repolarization occurs immediately after depolarization and is the movement of positively charged ions back to
the outside of the cell, returning the cell back to its original polarized state. A cell must repolarize before it can
depolarize again. Whereas depolarization results in myocardial contraction, repolarization does not result in
any actual muscle movement…it is strictly an electrochemical event.
Absolute Refractory Period: is the 1
st
phase of repolarization in which a myocardial cell is unable to react to
any electrical stimulus. This period falls during the depolarization and contraction of the ventricles, thus
protecting the heart from any abnormal electrical stimulus that might result in loss of rhythmic contractions.
Relative Refractory Period: is the 2
nd
phase of repolarization during which time a strong enough electrical
stimulus might cause new depolarization and contraction. This could result in a chaotic, possibly lethal rhythm
disturbance.
Conduction System of the Heart
Conduction system of the heart is the system that generates and delivers (conducts) the electricity to all the
muscle fibers of the heart resulting in a smooth, complete contraction of the cardiac muscle fibers, which
forcefully ejects the blood outside the heart. This electrical delivery system consists of two nodes (which
generate and control the rhythmic impulses) and conduction pathways that connect the nodes and deliver the
electrical impulses to the myocardium.
The Conduction system of the heart consists of:
SA Node (Sino-Atrial Node or Sinus Node) Found in the upper posterior portion of the right atrial wall just
below the opening of the superior vena cava. It is the primary pacemaker of the heart and has a normal firing
rate of 60-100 beats per minute (BPM).
Internodal Pathways: Consists of anterior, middle and posterior divisions that distribute electrical impulses
generated by the SA node throughout the right and left atria to the atrio-ventricular (AV) node.
AV Junction (AV node): This node is located at the posterior septal wall of the right atrium just above the
tricuspid valve. There is normally a .12 - .20 second delay of electrical activity at this level to allow blood to
flow from the atria and fill the ventricles with blood. The AV node also functions as the backup pacemaker (at a
slower heart rate) if the Sinus Node fails to fire. Its intrinsic firing rate is between 40-60 beats per minute.

26
Bundle of His: Found at the superior portion of the interventricular septum, it is the pathway that leads out of
the AV node and connects to the Bundle Branches. It has an ability to initiate electrical impulses with an
intrinsic firing rate of 40-60 beats per minute.
Bundle branches: Located at the interventricular septum, the Bundle of His divides into the right and left
bundle branches, the function of which is to conduct the electrical impulse to the Purkinje fibers throughout the
ventricles.
Purkinje fibers: Found within the ventricular endocardium, it consists of a network of small conduction fibers
that deliver the electrical impulses from the Bundle Branches to the ventricular myocardium. This network has
the ability to initiate electrical impulses and act as a pacemaker if the higher level pacemakers fail. The intrinsic
firing rate is 20-40 beats per minute.
Fundamentals of Electrocardiogram
EKG is a galvanometer that measures the heart electricity traveling through the conductive system and an
important tool for patient‟s diagnosis and evaluation as:
1. Monitoring patient‟s HR
2. Evaluates injuries to the heart muscle
3. Evaluates the pacemakers and conductive system function
4. Evaluate the response toward medication
5. Provides a baseline record for medical procedures
EKG Basic Concepts:
Electrode: is a paper, plastic or metal sensor placed on the patient‟s skin on a specific location and
transmits it to the cable.
Cable is a wire that connects the electrode to the EKG machine (cardiac monitor)

27
Lead is a recorded tracing of the heart electricity from one or two electrodes that provides a specific
view of the heart.
EKG Lead Types:
1. Standard Bipolar Limb Leads: Record electrical activity in the frontal plane. Electrodes are
applied to the left arm (LA), the right arm (RA) and the left leg (LL). These leads record the difference
in electricity between two electrodes.
Lead I = the left arm is positive and the right arm is negative. (LA – RA)
Lead II = the left leg is positive and the right arm is negative. (LL – RA)
Lead III = the left leg is positive and the left arm is negative. (LL – LA)
During the 12 lead recording, the EKG machine automatically changes the polarity of electrodes in order
to record multiple leads, or views, simultaneously.
The Right leg electrode is used as a ground electrode.
2. Augmented Unipolar-also records electrical activity in the frontal plane.
Augmented Unipolar Leads record the heart electricity from one limb and compare it with a zero
voltage lead in the center of the heart. The EKG machine uses a midpoint between the two other limbs
as a negative reference point. These leads augment (magnify) the voltage up to 50% compared to the
standard leads. AV stands for augmented voltage; R stands for Right Arm (RA), L stands for Left
Arm (LA) and F stands for Left Leg (LL).
Lead aVR = the right arm is positive and the other limbs are negative.
Lead aVL = the left arm is positive and the other limbs are negative.
Lead aVF = the left leg (or foot) is positive and the other limbs are negative.
3. Precordial Chest Unipolar Leads: All these electrodes are positive and record the heart electricity in
the horizontal plane. They include leads: V1, V2, V3, V4, V5, and V6.
V1 : Fourth intercostal space, right sternal border.
V2 : Fourth intercostal space, left sternal border.
V3 : Equidistant between V2 and V4.
V4 : Fifth intercostal space, left midclavicular line
V5 : Fifth intercostal space, anterior axillary line
V6 : Fifth intercostal space, midaxillary line
Figure 3: Precordial Leads

28
The usual routine EKG consists of placing 10 electrodes on the patient producing 12 Leads: I, II, III,
aVR, aVL, aVF; V1-V6.
Definition of Waves, Segments and Intervals
Waveform: refers to movement away from the isoelectric line with either upward (positive)
deflection or downward (negative) deflection.
Segment: line between two waveforms.
Interval: waveform plus a segment.
Complex: several waveforms
The Normal EKG Waves and Complexes
1. Atrial Depolarization:
a. P wave: is the first deflection after the diastole, produced by atrial depolarization.
It is a smooth, round, not more than 2.5 mm high and no more than 0.11 sec
Positive in I,II, and V2 to V6
The normal P wave in standard, limb, and precordial leads does not exceed 0.11s in duration or 2.5mm
in height.
b. There is no wave for atrial repolarization, because is obscured by the larger QRS complex
2. Ventricular Depolarization:
a. QRS complex
Represents ventricular depolarization (activation).
The ventricle is depolarized from the endocardium to the myocardium, to the epicardium.
Normal duration is no more than 0.1 sec (otherwise stated as “less than .12 sec”).
b. Q (q) wave: the initial negative deflection produced by ventricular depolarization.
c. R (r) wave: the first positive deflection produced by ventricular depolarization.
c. S (s) wave: the first negative deflection produced by the ventricular depolarization that follows the first
positive deflection, (R) wave.
3.Ventricular Repolarization:
a. T wave: The first wave after the QRS complex has the following characteristics
The deflection produced by ventricular repolarization.
It is slightly asymmetric
No more than 5 mm in height
b. U wave: Is the deflection seen following the T wave but preceding the diastole.
Represents repolarization of Purkinje fibers
Round and symmetric less than 1.5 mm in height
A prominent U wave is due to hypokalemia (low potassium, blood level).
29
The Normal EKG Segments, Intervals and Junctions
1. Normal EKG Segments: Segments: are lines between waveforms.
a. PR segment this segment is measured from the end of the P wave to the beginning of the QRS complex.
Represents depolarization of AV node and its delay and depolarization of the Bundle of His and the
Bundle Branches.
b. ST segment This segment represents the time of ventricular contraction and the beginning of
repolarization of both ventricles. It is measured from end of QRS to the beginning of the T wave. The
point where QRS complex and the ST segment meet is called “the junction” or “J point”. ST segment is
the most sensitive part of EKG changed by cardiac ischemia.
2. Normal Interval and Junctions: By definition an interval is a segment plus a waveform.
a. PR Interval Is defined as P wave and PR segment and is measured from the beginning of P wave to
the beginning of QRS complex. The normal interval is 0.12 – 0.2 sec.
b. QT Interval It represents the total ventricular activity (ventricular depolarization PLUS ventricular
repolarization), and it is measured from the beginning of QRS to the end of T wave.
The normal duration of this interval depends on the age and the HR.
c. RR Interval. It is important to determine the HR and its regularity..
RR interval: this is the interval between two R waves.
d. J (RST) junction: point at which QRS complex ends and ST segment begins.
e. ST segment: from J point to the onset of the T wave. This segment is compared to the PR segment to
help identify myocardial ischemia or injury.
Analyzing the EKG Strip involves the following steps
To analyze the EKG strip for its quality and to identify any emergency pathology you can follow the
following guidelines:
1. Assesses the HR
1. 6 second Method: The number of QRS complexes between 6 sec marks on the EKG paper is multiplied
by 10. Used generally for estimating slow or irregular rhythms.
2. Large Boxes Method: count the number of large boxes between two consecutive RR (one RR interval)
and divide into 300 for the ventricular rate; and count large boxes between two consecutive P waves for
the atrial rate. Used mainly in regular rhythms.
3. Small Boxes: One minute has 1500 small boxes (0.04 sec). Count the number of small boxes between
an RR interval and divide into 1500.This method is more accurate and is used for regular rhythms only.
4. Sequence Method: Select the R that falls on a dark vertical line. Number the next consecutive dark line
as 300, 150, 100, 75, 60, and 50. Note where the next R wave falls in relation to the dark lines. That is
the heart rate.

30
2. Assess Rhythm/ Regularity
The HR is considered regular if all the RR or PP intervals on the EKG leads are equal. If there are changes in
their durations the rhythm is irregular.
3. Identify and examine the P waves: Identify the P waves, PP interval and measure the size of the P wave in
different leads.
4. Assess intervals (PR, QRS, QT): Measure each of these intervals and determine if they are normal.
5. Evaluate ST segments and T waves. ST segment elevation or depression and/or T wave abnormalities can
suggest the presence of myocardial ischemia or injury.
6. General Evaluation and Conclusion: Notify the doctor for any abnormality that you can find on the EKG
strip.
EKG Interpretation and Pathology Recordings
Cardiac arrhythmias are due to the following mechanisms:
Arrhythmias of sinus origin - where electrical flow follows the usual conduction pathway but is
too fast, too slow, or irregular. Normal sinus rate is 60-100 beats per minute. If the rate goes
beyond 100 per minute, it is called sinus tachycardia. If the rate goes below 60 per minute, it is
referred to as sinus bradycardia.
Ectopic rhythms - electrical impulses originate from somewhere else other than the sinus node.
Conduction blocks - electrical impulses go down the usual pathway but encounter blocks and
delays.
Pre-excitation syndromes - the electrical impulses bypass the normal pathway and, instead, go
down an accessory shortcut
A. Sinus Rhythm
1. Normal Sinus Rhythm
Fig. 5. Normal Sinus rhythm. Notice that all PQRST waves are equal and present. Diastolic
period can be easily identified.
The rhythm originated from the SA has the following characteristics
a. HR 60 – 100 bpm
b. Similar P in all the leads in front of all QRS (0.1 sec)
c. A constant PR (0.12 to 0.2) sec interval in all the leads, regular rhythm

31
2. Sinus Bradycardia
Fig. 6. Sinus Bradycardia. Notice all the waves are present and in normal size. A very long
diastolic period can be easily seen in all the leads.
a. HR less than 60 bpm
b. Normal equal P and QRS in all the leads, as well as normal PR intervals
c. Diastolic pause is longer (main graphic characteristic).
d. Bradycardia decreases the blood flow in the brain and other body tissues
3. Sinus Tachycardia
Fig 7. Sinus Tachycardia. The diastolic period cannot be seen well, P and T waves are very
close to each other.
a. HR over 100 bpm
b. Normal equal P and QRS in all the leads, as well as normal PR intervals
c. Diastolic pause is very small or nonexistent (main graphic Characteristic)
d. Tachycardia reduces the blood supply to the cardiac muscle.
4. Sinus Arrhythmia:
Fig. 8. Sinus Arrhythmia. Notice that the PQRST waves are equal and normal in size, but
diastolic periods are different after each heart systole.
a. HR 60 to 100 bpm
b. Normal equal P and QRS in all the leads, as well as normal PR intervals

32
c. Different diastolic pause after each systole. If there are changes with the respiration is named
Respiratory Sinus Arrhythmia, otherwise is called Nonrespiratory Arrhythmia
B. Important Atrial Rhythms
1. Supraventricular Tachycardias.
Fig. 10. Supraventricular Tachycardia
Atrial Tachycardia (AT) it is caused by an irritable focus in the atria that fires electrical
impulses after the normal firing of the SA node pacemaker. HR is regular between 100
and 150 bpm.
AV Reentry Tachycardia is caused when the electrical impulse passes through a
passage other than AV node. Cardiac rhythm is regular but up to 250 bpm. P waves are
often hidden by the QRS complexes or the QRS complexes that follow a P wave are
different and with different PR interval (AV Nodal Reentry Tachycardia AVNRT).
In cases with AV Reentry Tachycardia (AVRT) QRS complexes are greater than 0.12
sec with a slurred up strike (delta wave) seen in one or more leads.
It is an EMERGENCY. NOTIFY THE DOCTOR.
2. Atrial Flutter
Fig. 11. Atrial Flutter: Notice that there are no more “P” waves, instead a typical saw-
tooth-like wave, called “F” wave is seen in the above recording.
a. Atrial Flutter is characterized by rapid depolarization of a single atrial focus at a rate of
250-350 bpm.
b. Because the AV node cannot transmit every impulse at excessive rates, there is typically
a slower ventricular rate (often appearing as a 2:1, 3:1, 4:1, etc. conduction ratio).
c. Typical saw-toothed waves, named “F” waves, followed by almost normal QRS
complexes with a slower rate are seen in all the leads.
It is an EMERGENCY. NOTIFY THE DOCTOR.

33
3. Atrial Fibrillation
Fig 12. Atrial Fibrilation. There are no more “P” waves, instead they are substituted by
small trembling waves, while QRST complex are almost normal and fired with a
different rate.
a. Atrial fibrillation is caused by multiple irritable sites all over the atria firing at a rate exceeding
350 bpm. These rapid impulses cause quivering (fibrillation) of the muscular fibers, which
results in a drastic decrease in the cardiac output, blood stagnation and the formation of a clot.
b. No identifiable P waves can be seen, fibrillatory erratic “f” waves are seen in all the leads.
Ventricular rhythm is very irregular, with a much slower rate than the atria. This is seen in all
leads.
c. Controlled atrial fibrillation: Average ventricular rate is less than 100 bpm.
d. Uncontrolled atrial fibrillation: Average ventricular rate is over 100 bpm.
It is an EMERGENCY. NOTIFY THE DOCTOR.
C. Ventricular Rhythms
1. (PVC) Premature Ventricular Complex:
Fig. 13. PVC. Observe the difference between the normal QRS complexes and the wide
inverted abnormal QRS of the PVC and the full compensatory pause.
A premature ventricular complex arises from an irritable site within the ventricles.
The QRS of PVC is typically greater than 0.12 sec because the ventricular
depolarization is abnormal or aberrant.
T waves are usually in opposite direction of the QRS complex
A full compensatory pause usually follows a PVC
2. Ventricular Tachycardia (VT):
Fig. 14. Notice the evident characteristics of this pathological rhythm, there are no more
“P” wave, but wide, bizarre QRS complexes at a rate over 100 bpm.

34
Ventricular Tachycardia (V-Tach) is characterized by 3 or more PVC‟s in a row at a rate over
100 bpm. If V-Tach occurs for more than 30 sec is called sustained Ventricular Tachycardia.
The main characteristics of this rhythm are:
Regular fast rhythm 100 to 250 bpm
No P waves
Wide, bizarre QRS complexes with T waves pointing in opposite direction from main QRS
direction (T waves may be difficult to identify). If QRS complexes are different in size it is
called Polymorphic V-Tach or “Torsades de Pointes”.
It is an EMERGENCY. NOTIFY THE DOCTOR.
3. Ventricular Fibrillation (VF):
Fig. 15. Notice the quivering erratic waves that do not resemble any of the normal
waves or QRS complexes.
It is produced by multiple electrical sites firing electrical impulses at the same time resulting in
quivering of the ventricles myocardial muscle fibers, but not a uniform contraction.
The rhythm is a chaotic deflection of different waves that vary in size, shape and duration.
There are no normal visible waves. There is no contraction, there is no blood ejected in the blood
vessels, so the blood can clot. This is a medical emergency, which requires defibrillation and
CPR.
It is an EMERGENCY. NOTIFY THE DOCTOR.
3. Asystole (Cardiac Arrest, Standstill):
Fig. 16. There is just an isoelectric line, no waves are seen, and there is no more electric
activity from the heart.
It is a total absence of ventricular electrical activity. It is a straight isolelectric line. The patient
is clinically dead and CPR is imperative.
It is an EMERGENCY. NOTIFY THE DOCTOR.

35
D. Atrio-Ventricular Blocks (AV Blocks)
AV blocks are defined as a delay or interruption of the electric impulse conduction beyond the
AV node. It is evaluated by measuring the PR interval in EKG traces. The PR interval is the key
of differentiation and classification of the AV blocks.
1. Type I First Degree AV block. It is characterized by a delay of impulses at the level of AV
node. . PR interval is prolonged and is greater than 0.2 sec
Fig. 17. Notice the prolonged PR interval after each “P” wave in the recording. This is the
main feature of the First degree Av Block. Other than the PR prolongation, the EKG may
otherwise appear normal.
2. Type II Second Degree AV blocks. Some of the atrial impulses, but not all, are blocked at the
AV node level. Because SA node fires regular rhythmic impulses, each P wave occurs in a
regular interval across the EKG strip, but not all P waves will be followed by a QRS complex
a. Type I second Degree AV Block (Wenckebach, Mobitz I)
PR interval lengthens in each interval until one QRS disappears
Fig. 18. Notice the gradual increase in the PR interval, and then a sudden disappearance of
a QRS complex. In a Type I, there is occasionally an extra P wave, not always.
b. Type II Second Degree AV Block (Mobitz II)
It is a more serious pathology.
Conducted P waves have a constant PR interval; but there are always non-conducted P waves between cardiac cycles, usually producing a
“conduction ratio” between atria and ventricles (i.e. 2 P waves for each QRS, or 3 P waves for each QRS)
Fig 19. In this strip, there are 2 P waves per QRS; indicating a sudden loss of a QRS every
other cardiac cycle.

36
3. Third Degree AV Block. This type of AV block is also called a Complete Heart Block, or CHB,
because impulses generated by the SA node are completely blocked before reaching the ventricular
muscle fibers. The atria and ventricles beat independently from each other. Second degree blocks
can progress in third degree blocks, especially after an inferior MI (myocardial Infarction). The third
degree block‟s characteristics are:
Atrial rate is greater than ventricular rate
P waves are normal, there are no measurable PR intervals
The atrial rhythm (P waves) is regular; AND the ventricular rhythm is regular (QRS
complexes).
There is no relationship between P waves and QRS complexes
If the escape rhythm is junctional, the QRS complexes may appear normal in width and
the ventricular rate may be slightly higher
If the escape rhythm is ventricular, the QRS complexes will be abnormally wide with a
slower ventricular rate.
E. Myocardial Ischemia and Infarction
Ischemia is defined as insufficient blood supply to the myocardium. Atherosclerosis of the coronary
arteries is the most common cause of the blood supply reduction.
Myocardial Infarction MI is defined as sudden death of the myocardial tissue due to an abrupt
cessation of the blood flow. Clotting and total obstruction of a coronary artery are frequently
superimposed on an already narrowed vessel from atherosclerosis.
There is always an area of ischemia surrounding the infarction (dead muscle) zone and it is the
combination and gravity of these two zones that gives a unique pattern in the EKG traces.
Ischemic EKG characteristics are as follows:
Subendocardial ischemic injury is manifested by ST segment depression in the leads recording in
front of the ischemic site.
Subepicardial and transmural injury is manifested by ST segment elevation in the leads recording
in front of the lesion.
Myocardial Infarction EKG characteristics follow the pathological events occurring during the heart
attack (MI).
In the early stages of the MI ischemic lesion predominates, manifested as ST depression and T wave
inversion in the leads facing the myocardial lesion. Some times T waves increase in amplitude and
width.
Fig. 20. Notice the ST segment depression in aVL leads on the trace, an evident sign of
acute myocardial ischemia.
Marked ST elevation with hyperacute T waves reflect complete muscular wall damage.
In later stages (sub-acute MI) deep Q waves are seen on the leads facing the lesion
manifesting necrosis.
Pathological Q waves and inverted T waves are signs of fibrosis and scar tissue formation.

37
It is an EMERGENCY. NOTIFY THE DOCTOR.
Fig. 221. Changes in ST segments and T wave inversion are the early signs of
myocardial infarction.
The World Health Organization (WHO) criteria for the diagnosis of myocardial infarction are the
presence of at least two of the following:
- Clinical history of ischemic-type of chest discomfort
- Changes on serial EKG tracings
- Rise and fall in serum cardiac markers demonstrating cardiac tissue damage.
F. EKG Artifacts
Artifact is an unwanted interference or jitter on the EKG recording. This makes the EKG reading
difficult or impossible, as well as can lead to a misdiagnosis.
Somatic Tremor, it is a jittery pattern caused by the patient‟s shivering or by shaking wires. Help the
patient relax, cover the patient, make sure that the wires are correctly placed, or try the examination two
more times. Redo the EKG until the tracing is more readable.
Fig 22. Notice the jittering pattern on the aVR and aVL leads
Wandering Baseline, it is when the baseline moves up and down on the EKG paper. It is often caused
by lotion or sweat on the skin interfering with the signal transmitted to the machine. Cleaning the site of
the electrode and properly placing it resolves the interference.

38
Fig. 23. The iso-electric line moved up and down the strip.
60-cycle Interference: Caused by improperly grounded electrical equipment that is directly or
indirectly in contact with the patient. Cellular phones and pagers may also interfere with the EKG trace.
Disconnect and remove all the electric objects from the patient or near by the machine.
Fig. 24. 60-cycle Interference: The spikes over the P, Q, S and T waves are beating 60 per
sec.
Broken Recording can be caused by a damaged wire or loose electrodes. If the probes are placed
properly, the cause is originating from a broken or damaged wire. Use a different EKG machine or
replace the wires. Never use a damaged or malfunctioning machine.
Fig. 25. The V2 electrode is detached from the patient
G. Other EKG Related Tests
1. Stress Testing
Stress testing is a noninvasive diagnostic procedure to determine indirectly, the presence and severity of
coronary artery disease and the heart muscle lack of blood supply. The test is performed through
exercise (by having the patient walk on a treadmill or by pedaling on a bicycle), or pharmacologically

39
(by administration of medication that causes increase in heart rate), while hooked up to an EKG monitor.
The limb leads are applied to the torso of the patient rather than on the extremities themselves. A rhythm
strip is run continuously throughout the test and a complete 12-lead EKG is recorded usually every 90
seconds during exercise and every minute in the recovery period post-exercise. The most common
indication for a stress test is chest pain during exercise or physical effort (Angina Pectoris).
Some indications for stress testing are:
Exercise stress test
This test is performed until at least 85% of the target heart rate is reached or symptoms or EKG changes
develop which requires the test to be terminated. Target heart rate is: 220 minus patient‟s age. For
example, the target heart rate for a 40 year old patient is 180 (220 – 40). 85% of 180 or 153 is required
for the test to be valid for interpretation.
Pharmacologic stress test
This test is appropriate for patients with physical limitation, e.g. amputees, or those who could not
exercise to reach the target heart rate, e.g. elderly. Medications such as adenosine, dipyridamole, or
dobutamine are given intravenously through an IV line to cause the heart rate to climb to the target level
or the same symptoms and EKG changes as the exercise test develop. The test is concluded after 85% of
the target heart rate is achieved.
2. Ambulatory EKG Monitoring
Ambulatory EKG monitoring is mainly, but not only, used for diagnosis of cardiac dysrhythmias
(disorders of the heart rhythm). It also can evaluate the heart rate, rhythm and function during daily
activities.
Holter Monitor: This is an ambulatory EKG done to rule out intermittent arrhythmias or
ischemia that could be missed on a routine EKG. This may be done as an in-patient or outpatient
procedure. The patient is hooked-up to a Holter monitor and EKG signals are recorded on a
magnetic tape or digital flash media. After the prescribed duration, the patient returns the
monitor to the facility and the data is entered into a computer and scanned for abnormalities.
Five electrodes are attached to the patient’s trunk instead of the arms and leg to prevent
muscle artifact. The skin is especially prepped by abrading a thin layer of skin and then the
electrodes are taped to the skin so it will adhere better and prevent from dislodging since the
entire procedure will be on for 24 hours or longer. Before the ambulatory recording starts, EKG
tracings are taken with the patient lying, sitting, and standing in order to be able to identify these
positional changes which can bring about substantial variation in QRST morphology upon
playback of the tape.
Typical electrode placement for Holter monitoring:
Two exploring electrodes are placed over bone (to minimize motion artifact) near the V1 (over the 4
th
or
5
th
rib to the right of the sternum) and V5 (over the 5
th
rib at the left midaxillary line).
Two indifferent electrodes placed over the sternal head.
One ground electrode placed over the 9
th
or 10
th
rib at the right midaxillary line

40
Artifacts of Ambulatory EKG Recording
Recording artifacts can result from the following:
With an analog system: Incomplete tape erasure - this can result in EKG tracings belonging to two
different patients confounding both the scanner and the interpreter.
With an analog system: Tape drag within the apparatus - this will result in recording of spuriously rapid
cardiac rhythms. A narrowing of all EKG complexes and intervals should give clue to this situation.
Battery depletion - this may result in varying QRS amplitude
Loose connection - intermittently loose connection in the insertion of the electrodes into the recording
apparatus can result in the absence of all EKG signals which may mimic bradycardia-tachycardia
syndrome. Clue to this artifact is the attenuated QRST morphology of the complexes beginning and
ending the pause in rhythm.
Movement of electrodes - this may occur during scratching the chest near the electrodes and can
produce tracings that look like malignant ventricular arrhythmias. However, the underlying rhythm and
rate remain undisturbed and should give clue to this artifact.
Event Monitoring Some patients have symptoms very infrequently that a Holter monitor yields little
useful data. These patients are best suited for an event recorder, a hand held device carried in the
patient‟s pocket or purse which is switched only when the patient is actually experiencing the symptom.
The EKG is recorded from the anterior chest wall on magnetic tape or computer chip which is scanned
later the same way as that of the Holter monitor or it can be transmitted by telephone to a receiving
station for immediate attention. Since the event recorder is used only when symptoms occur, multiple
recordings can be made over the course of a prolonged period of time.
Commonly Used Cardiovascular Drugs:
1. Oxygen: Given to all patients with angina pectoris (acute severe chest pain). Causes
vasodilatation and protects the tissues from hypoxia. It can be administered through a cannula or a
facial mask.
2. Epinephrine: A sympathetic drug used to manage cardiac arrest, because increases heart
contractibility.
3. Isoproterenol (Isuprel): Isoproterenol produces an overall increase in heart rate and myocardial
contractility, but newer agents have replaced it in most clinical settings.
4. Dopamine (Intropin): This drug is indicated and is used in cases with hypotension (systolic blood
pressure is less than 90 mmHg). It causes vasoconstriction (narrowing of the blood vessel). It should
be used at the lowest dose that produces adequate perfusion of vital organs.
5. Beta Blockers (Propranolol, Metoprolol, Atenolol, and Esmolol): Beta blockers reduce heart rate,
blood pressure, myocardial contractility, and myocardial oxygen consumption which make them
effective in the treatment of angina pectoris and hypertension. They are also useful in preventing
atrial fibrillation, atrial flutter, and paroxysmal supra-ventricular tachycardia. Adverse effects of
beta blockers are hypotension, congestive heart failure and broncho-spasm.
6. Lidocaine: Lidocaine is the drug of choice for the suppression of ventricular ectopy (a beat located
outside the conductive system) contractions (PVC), including ventricular tachycardia and ventricular
flutter. Excessive doses can produce neurological changes, such as drowsiness, disorientation,
decreased hearing ability, paresthesia, muscle twitching, and eventual seizures. In large doses it
causes
myocardial depression, and circulatory depression.
7. Verapamil: Verapamil is used in the treatment of paroxysmal supraventricular tachycardia (PSVT),
effective in terminating more than 90% of episodes of PVST in adults and infants. Verapamil is also
useful in slowing ventricular response to atrial flutter and fibrillation. Vigilant monitoring of blood
pressure is recommended due to hypotension that could occur.
41
8. Digitalis: Digitalis increases the force of cardiac contraction as well as cardiac output.. Digitalis is a
drug with high toxicity, therefore patients require constant monitoring for signs and symptoms of
toxicity such as: yellow vision, nausea, vomiting, and drowsiness.
9. Morphine Sulfate: It is the traditional drug of choice for the pain and anxiety associated with acute
myocardial infarction. In high doses, morphine sulfate may cause respiratory depression. It is a
controlled substance and has a tendency for abuse and addiction.
10. Nitroglycerin: Nitroglycerin is a powerful smooth muscle relaxant effective in relieving angina
pectoris. Headache is a common consequence following the administration of this drug. Hypotension
may occur and patients should be instructed to sit or lie down while taking nitroglycerin.
1. Phlebotomy Profession, duties and responsibilities- The medical laboratory
The hospital laboratory in which the phlebotomist works is part of a large organization. The laboratory
consists of a team of many health care professionals and performs a variety of tests on blood and other body
specimens. The laboratory obtains, handles, studies, and analyzes the specimens. Departments within a clinical
laboratory are:
o Chemistry department is the largest department and performs many tests such as, blood lips
(cholesterol and triglycerides), electrolytes (sodium, potassium), creatinine, blood urea nitrogen
(BUN), liver and cardiac enzymes, bilirubin, blood specific proteins and etc. The most
automated section in the laboratory.
o Electrophoresis is the chemical analysis of the blood proteins, based on their electrical charges
and size while moving on a gel film. Toxicology analyzes plasma levels of drugs and poisons.
Immunochemistry uses techniques such as radio immunoassay (RIA) and enzyme
immunoassay to detect and measure substances such as hormones, enzymes, and drugs.
o Hematology department conducts laboratory analysis testing of blood and blood forming
tissues. The Complete Blood Count (CBC) conducted by this department includes: Red Blood
Cell count (RBC); White Blood Cell count (WBC); Hematocrit (ct) blood concentration;
Hemoglobin percentage (Hgb or Hb); Platelets count (Thrombocytes); Differential WBC
(diff) the ratio between different types of white blood cells in a blood unit (1 millimeter cubic).
Other hematological analyses are Erythrocyte Sedimentation Rate (ESR), fibrinogen, Partial
Thromboplastin Time (PTT), Prothrombin Time (PT), coagulation studies, and Reticulocyte
studies (young erythrocytes).
o Microbiology analyzes specimens for the presence of infectious micro-organisms. A culture of
the specimen is performed (growing microorganisms in an artificial environment) and the
sensitivity test will determine which antibiotic would be effective. This is also called C & S test.
Cultures are examined for almost every body fluid, including feces. Blood cultures
(hemoculture) are used to diagnose patients‟ fever of unknown origin (FUO).
o Immunology and Serology: this department runs tests on serum (the blood fluid part after
coagulation) to determine the antigen-antibody specific reactions for infectious diseases (HIV,
syphilis) and auto-immune diseases (rheumatoid arthritis).
o Blood Bank department: conducts tests on RBC and serum including blood typing and
compatibility tests. Blood taken from donors is carefully tested and analyzed before it is
administered to patients who need a blood transfusion. Blood collected may be separated into
components: packed cells, platelets, fresh frozen plasma, and cryoprecipitate.
o Urinalysis may be performed within several departments, depending on the laboratory. Urine is
examined for its physical properties (color, clearance, and concentration), chemical

42
composition (electrolytes), and microscopic sediment properties (different cells of the urinary
system, crystal and microorganisms).
o Surgical and Anatomical Pathology department examines body tissues and cells provided
during an autopsy or biopsy examinations.
Quality Control is defined as a program that guarantees quality patient care by tracking the outcomes through
scheduled audits in which areas of the hospital look at the appropriateness, applicability, and timeliness of
patient care. A quality control program is a continuous program, established by the healthcare facility, which
will provide guidelines, protocols and continuing education for their employees. The Laboratory/Phlebotomy
Specimen Collection Procedures Manual has established these guidelines.
Analytical Errors
Before Collection:
During Collection:
After Collection:
Patient misidentification
Extended tourniquet time
Failure to separate serum
from cell
Improper Time of
Collection
Hemolysis
Improper use of serum
separator
Wrong Tube
Wrong order of draw
Processing delays
Inadequate fast
Failure to invert tubes
Exposure to light
Exercise
Faulty technique
Improper storage conditions
Patient posture
Under filling tubes
Rimming clots
Poor coordination with
other treatments
Improper site preparation
Medication interference
2. Infection Control in Phlebotomy
During phlebotomy procedures, the patient care technician should be aware of infections from blood borne
pathogens and must be protected, inoculating infectious agents into the blood stream, and sample
contamination.
The most common blood borne pathogens are HIV and HBV. The most serious of these infections is HIV
infection that is a deadly infection. The most dangerous route of transmission for HIV infection is through
needle sharing or transfusions. For this reason all the medical personnel at risk should be vaccinated for
hepatitis B virus and should know the procedure in place for prevention and treatment in cases of needle stick
injuries.
Prevention of infection and handling needle stick injuries:
Wash hands before and after the wearing gloves for the procedure for more than two 2 minutes
Follow universal precautions and wear PPE when needed
Always wear gloves during the procedure
Single use needles and syringes
Be vaccinated for HBV
In cases of accidents wash the site with running water and use an anti-viral treatment
Introducing pathogens in the tissues under the skin or into the blood stream could be life-threatening in
chronically ill and immuno-depressed patients. Prevention of parietal infection transmission and sample
contamination is achieved by:
Proper disinfection, the most commonly used is 70% Alcohol (Bacteriostatic)

43
Betadine (Iodine) and Phenols are used to sterilize the phlebotomy field, especially in cases when
blood culture is required or when alcohol can not be used.
Sterile or single-use tools are always used over the phlebotomy field.
3. Anatomy and Physiology: Blood and blood vessels
I. Blood: The average adult has 5 to 6 liters of blood. Blood is a connective tissue with cells called formed
elements and fluid as matrix called plasma.
A. Plasma comprises 55% of the circulating blood and it contains water (92%), proteins, amino acids, gases,
electrolytes, sugars, hormones, minerals, and vitamins. It also contains waste products such as urea that are
destined for excretion. Hematocrit is defined as the ratio (percentage) of the packet red blood cells found in a
unit volume of whole blood. Hematocrit is measured as the height of the RBC column versus the whole blood
column. Hematocrit (Htc) = RBC volume/ whole blood volume (RBC + Plasma).
B. The formed elements constitute the remaining 45% of the blood. They are erythrocytes (red blood cells),
which comprise 99% of the formed elements, the leukocytes (white blood cells) and the thrombocytes
(platelets). All blood cells normally originate from stem cells in the bone marrow.
1. The red blood cells (erythrocytes) function is the transportation of oxygen to the tissues. They are disc
shaped cells with no nucleus. Four molecules of a round protein (hemoglobin) incorporate iron carry the
oxygen. Young and immature erythrocytes, called Reticulocytes, have a nucleus are seen in blood in cases of
sudden and severe blood loss. There are 4.2 to 6.2 million RBC‟s per micro liter of blood. The normal life span
of an RBC is 120 days.
2. The white blood cells WBC (leukocytes) function is to provide protection against infection. The normal
amount of WBC‟s (white blood cells) for an adult is 5,000 to 10,000 per micro liter. Leukocytosis (increase in
WBCs), is seen in cases of infection and leukemia. Leukopenia (decrease in WBcs), is seen with viral
infection or chemotherapy.
There are five types of WBCs in the blood. A differential count determines the percentage of each type:
o Neutrophils are the most numerous, comprise about 40% to 60% of WBC population. They are
phagocytes, meaning they engulf and digest bacteria. Their number increases in acute bacterial
infection, and often the first one on the scene. If the number of young neutrophils is increased in blood
(shift to the left) and this is a sign of acute bacterial infection.
o Lymphocytes are the second most numerous, comprising about 20% to 40% of the WBC population.
Lymphocytes protect us against some chronic bacterial infections and against viral infections. They
carry the immunity memory that protects the body from repeated infections. Lymphocytes produce
specific antibodies. Their number increases in acute viral infection.
o Basophils account for 0% to 1% of WBCs in the blood. They carry histamine, which is released in
allergic reactions. Their numbers increase in allergic reactions.
Hemostasis is the process that stops the bleeding. It is also the process by which blood vessels are repaired after
injury. It occurs in four stages:
First Stage/Vascular Stage: Is predominantly a vasoconstriction the vessel reduces the blood flow and
the blood loss, by reducing its cross-section.
Second Stage/ Platelet Stage: Is characterized by a platelet aggregation forming a platelet wall that
seals the vessel gap and totally stops the blood loss. Vascular phase and platelet phase comprise the
primary hemostasis. Bleeding time test is used to evaluate primary hemostasis.
Third Stage/ Coagulation Phase: This involves a cascade of interactions of coagulation proteins
(factors) that converts the temporary platelet plug to a stable fibrin clot by enlodging the platelets with a
strong protein called Fibrin. The coagulation cascade involves an intrinsic system and extrinsic system,

44
which ultimately come together in a common pathway and produce Fibrine. Activated partial
thomboplastin time (APTT) test used to evaluate the intrinsic pathway. This is also used to monitor
heparin therapy. Prothrombin time (PT) test used to evaluate the extrinsic pathway. This is also used to
monitor Coumadin therapy.
Fourth Stage/ Fibrinolysis: Is characterized by melting of the thrombus and total repair of the blood
vessel. As tissue repair starts, plasmin (an enzyme) starts breaking down the fibrin in the clot. Fibrin
degradation products (FDPs) measurement is used to monitor the rate of fibrinolysis.
II. Anatomy of the region, neurovascular structures, and vein selection
The most common site for phlebotomy is antecubital fossa, because there are many large and superficial veins
in this area called antecubital veins. The antecubital fossa is located in the front of the elbow, below the biceps
muscle. Antecubital fossa is created as a groove between biceps on top and two group muscles of the forearm.
On the side are the extension muscles and on the medial side close to the body is flexor group. The skin layer on
this area is thin and with a very little subcutaneous tissue under, therefore the blood leaked during a procedure
can easily spread in this area and cause hematoma (a mass of clotted blood). Strips of connective tissue anchor
the vein and fat into the dermal layer, so by stretching the skin over the vein, the vein is immobilized and can
not move during the needle insertion.
The most important antecubital veins are:
Median antecubital vein, the most frequent vein used for phlebotomy.
Cephalic vein is the second choice for venipuncture, because it is harder to palpate but is well
anchored. It is often the only palpable vein in obese patients.
Basilic vein is the third choice for phlebotomy, it is large and palpable, but is not well anchored and
rolls and bruises easily.
Other important anatomical landmarks of the forearm are radial and ulnar regions. The area of the wrist
located close to the thumb is the radial region. Radial artery is palpated here. The area of the wrist
located close to the fifth finger is the ulnar region. A small artery with the same name is located her,
too.
Note: Do not draw blood from an arm with IV fluids running into it. The fluid will alter the test results.
Do not draw blood from an artificial a-v fistula site, such as those surgically implanted in dialysis
patients. In both cases select another vein on the opposite arm.
4. Phlebotomy Equipment
The first step in performing a phlebotomy procedure is to have the necessary supplies and/or equipment
organized for proper collection of the specimen and to ensure the patient‟s safety and comfort. The
recommended supplies are as follows:
1. Laboratory requisition slip and pen.
2. Gloves must always be worn when collecting blood specimen.
3. Antiseptics solutions and disinfectants:
4. Vacutainer needles: These are disposable and are used only once both for single-tube draw and
multidraw (more than one tube).Needle sizes differ both in length and gauge. 1-inch and 1.5-inch long
are routinely used. The diameter of the bore of the needle is referred to as the gauge. The smaller the
gauge the bigger the diameter of the needle; the bigger the gauge the smaller the diameter of the needle
(i.e. 16 gauge is large bore and 23 gauge is small bore). Needles smaller than 23 gauge are not used for
drawing blood because they can cause hemolysis (destruction of the erythrocytes).
Never recap a needle without a safety device.
5. Needle adapters are also called the tube holder. One end has a small opening that connects the needle,
and the other end has a wide opening to hold the collection tube
6. Winged infusion sets or butterfly needles are used to puncture on small veins such as those in the
hand. They are also used for elderly and pediatric patients. The most common size is 23 gauge, ½ to ¾
inch long.
45
7. Sterile syringes and needles: 10-20 ml syringe is used when the Vacutainer method cannot be used.
8. Tourniquets prevent the venous outflow of blood from the arm causing the veins to bulge thereby
making it easier to locate the veins. The most common tourniquet used is the latex strip. (Be sure to
check for latex allergy). Tourniquets with Velcro and buckle closures are also available. Blood
pressure cuffs may also be used as tourniquets. The cuff is inflated to a pressure above the diastolic but
below the systolic.
9. Chux is an impermeable pad used to protect the patient‟s clothing and bedding.
10. Specimen labels will be placed on each tube collected after the venipuncture.
11. Needle disposal container must be a clearly marked puncture-resistant biohazard disposal container.
12. VacutainerTubes: Color-coded for specific tests and available in adult and pediatric sizes. The top part
of the tube defines the additive inside the vatutainer tube that can prevent or speed up the clotting
process, and is selected based on the type of blood analysis is ordered by the doctor.
a. Lavender Top Tube: Additive is an Anticoagulant, ethylenediaminetetraacetic acid (EDTA).
EDTA inhibits coagulation by binding to calcium present in the specimen. The tubes must be filled at
least two-thirds and inverted eight times
Common tests: CBC (Complete Blood Count); Includes: RBC count, WBC count and Platelet count;
WBC differential count; Hemoglobin and Hematocrit determinations; ESR (Erythrocyte Sedimentation
Rate); Sickle Cell Screening.
b. Light-Blue Top Tube: Additive is an Anticoagulant, Sodium Citrate, which also prevents
coagulation by binding to calcium in the specimen. Sodium citrate is the anticoagulant used to
coagulation studies because it preserves the coagulation factors. The tube must be filled completely to
maintain the ratio of nine parts blood to one part sodium citrate, and should be inverted three to four
times.Common tests: Coagulation Studies, such as Prothrombin Time (PT), which evaluates the
extrinsic system of the coagulation cascade and monitors Coumadin therapy; Activated Partial
Thromboplastin Time (APTT, PTT), which evaluates the intrinsic system of the coagulation cascade
and monitors Heparin therapy. It is used also to evaluate Fibrinogen Degradation Products (FDP);
Thrombin Time (TT); Factor assays, Bleeding Time (BT).
c. Green Top Tube: Additive is an Anticoagulant, Heparin that is usually combined with sodium,
lithium, or ammonium ion. Heparin works by inhibiting thrombin in the coagulation cascade. It is not
used for hematology because heparin interferes with the Wright‟s stained blood smear. This tube should
be inverted eight times.
Common tests: Chemistry tests: performed on plasma such as Ammonia, carboxyhemoglobin & STAT
electrolytes.
d. Gray Top Tube: Additives of this tube are a glucose preservative (antiglycolytic agent): sodium
fluoride preserves glucose for 3 days; and/or lithium iodoacetate-preserves glucose for 24 hours. May
also contain the anticoagulant potassium oxalate, which prevents clotting by binding calcium. This
tube should be inverted eight times.
Common tests: Fasting blood sugar (FBS); Glucose tolerance test (GTT); Blood alcohol levels;
Lactic acid measurement
e. Red/Gray (Speckled) Top Tube: Additive is a Serum Separator a gel that fastens the coagulation
process. It is also called tiger-top tube and serum separator tubes (SST) tube. Contains clot activators:
glass particles, silica and celite which fastens clot formation, and thixotropic gel, a serum separator
which when centrifuged forms a barrier between the serum and the cells preventing contamination of the
serum with cellular elements. Tubes must be inverted five times.
Common tests: Most chemistry tests.

46
f. Red Top Tube: Additive none; is also called plain vacuum tube, because contains no additives. The
blood sample inside this tube clots by normal coagulation process in 30 minutes. There is no need to
invert the tube after collection.
Common tests: Serum chemistry tests; Serology tests; Blood bank
g. Yellow Top Tube: Additive is an Anticoagulant: Sodium Polyanetholesulfonate (SPS).
Common Tests: Used for Hemoculture or blood microbiological studies. SPS aid in the recovery of
microorganisms by inhibiting the actions of complement, phagocytes, and certain antibiotics. These
tubes should be inverted eight times.
5. Phlebotomy procedure
A. Factors to Consider Prior to Performing the Procedure
Fasting: some tests such as those for glucose, cholesterol, and triglycerides require that the patient
abstain from eating for at least 12 hours. The phlebotomist must ascertain that the patient is indeed in a
fasting state prior to the testing.
Edema is the accumulation of fluid between the tissues. Collection from edematous tissue alters test
results.
Fistula is the permanent surgical connection between an artery and a vein. Fistulas are used for dialysis
procedures and must never be used for venipunctures due to the possibility of infection.
Skin Infection and Allergies can introduce infections to the vein and surrounding tissues and have a
defective hemostasis (stop the bleeding)
B. Phlebotomy Method/ Steps
Following are the steps used prior to and during a phlebotomy procedure:
1) Verify the requisition for the tests.
2) Identify the patient: check the patient’s ID number and have him/her state his/her name.
3) Identify yourself to the patient, explain the procedure, and secure his/her consent.
4) Establish the chain of Custody for blood samples drawn for drug purposes.
5) Properly position the patient for the test
6) Select the vein and than palpate it in the antecubital fossa using your index finger.
7) Gather and place in order of use the necessary equipment.
8) Wash hands; put on gloves.
9) Tie on the tourniquet; it should be applied 3-4 inches above the site where the venipuncture will be
made. Ask the patient to make a fist or open and close his/her hand to help engorge vein. Other
methods to make the vein visible are tap over the vein with to fingers, warm compresses over the site,
and some phlebotomists use small flashlights to make the vein under the skin visible.
10) Palpate the vein while looking for the straightest point. Cleanse the area with an antiseptic using a
circular motion starting at the inside of the venipuncture site.
11) Assemble the needle and tube holder while the alcohol is drying. Uncap the needle and examine it
for defects such as blunted or barbed point.
12) Hold the patient’s skin taut with the non-dominant hand by placing four fingers below the
antecubital area slightly pulling the skin back to anchor the vein.
13) With the bevel facing upward, insert the needle at an angle of 15-30 degrees.
14) Once the needle is inside the vein (you will feel a “give” as the vein is entered), push the collection
tube into the holder, to puncture the tube stopper with the back-end of the needle, and collect the
blood sample.
15) Release the tourniquet once blood flow has begun. The tourniquet should not be left on for more
than one 1 minute in order to prevent hemoconcentration.
16) Fill the needed tubes, according to the order of draw.
17) Pull out collection tube form the holder.
47
18) Place folded gauze over the venipuncture site and withdraw the needle. Then apply pressure until
bleeding stops. This is done to prevent hematoma. Do not ask the patient to bend the arm as it does
not offer enough pressure.
19) Discard needle into the biohazards sharp container.
20) Label each collected specimen, writing the patient‟s name and ID number, the time and date of
collection, and your initials.
21) Place labeled tubes inside the biohazards transport bag.
22) Before leaving, check the venipuncture site. If it is still bleeding, apply pressure for another 2
minutes. If after this time, it is still bleeding, continue to apply pressure for another 3 minutes. If
bleeding persists after a total 8 minutes of applying pressure, call for help.
23) At any point when the bleeding stops, an adhesive bandage is applied over a folded gauze square.
The patient should be instructed to remove the bandage within an hour.
24) Clean up everything and dispose of waste properly.
25) Leave the patient’s call light within his/her reach.
26) Remove the gloves, wash your hands, say good-bye to the patient and inform him/her that his/her
physician will deliver the results.
Do not label the tubes prior to the venipuncture.
Do not leave the patient‟s room before labeling the tubes.
Do not dismiss an outpatient before labeling the tubes.
Do not label tubes using a pencil; black ink should be used.
Do not leave the patient until you checked and ensure that the bleeding has stopped.
C. Order of Draw of Multiple Samples
Often requests are for more than one test to be performed; and as such, more than one collection tube needs to
be drawn. The correct order of draw is:
1. Blood Cultures
2. Light Blue top tubes
3. Serum or non-additive tube (Red or Red/Gray top tubes)
4. Green top tubes
5. Lavender top tubes
6. Gray top tubes
7. Documentation and Specimen handling
A. Documentation
B. Special Specimen Handling
1. Cold Agglutinins are antibodies produced in response to Mycoplasma Pneumoniae infection (atypical
pneumonia). The antibodies formed may attach to red blood cells at temperatures below body
temperature, and as such, the specimen must be kept warm until the serum is separated from the cells.
Blood is collected in red-topped tubes pre-warmed in the incubator at 37 degrees Celsius for 30 minutes.
2. Chilled specimens: Some tests require that the specimen collected be chilled immediately after
collection in crushed ice or ice and water mixture. Likewise, the specimen must be immediately
transported to the laboratory for processing. Some of the tests that require chilled specimen are: arterial
blood gases, ammonia, lactic acid, pyruvate, ACTH, gastrin, and parathyroid hormone.
3. Light-sensitive specimens: These are specimens that should be protected from light by wrapping the
tubes in aluminum foil immediately after they are drawn. Exposure to light could alter the test results
for: bilirubin, beta-carotene, vitamins A & B6, and porphyrins.

48
8. Special Phlebotomy Procedures
Some venipunctures are done using special collecting or handling procedures specific to the test being
requested. Some require patient preparation such as fasting, while some need to be collected at a specific time.
Still, others may need special handling such as protection from light.
Fasting Specimens: This requires collection of blood while the patient is in the basal state, that is, the patient
has fasted and refrained from strenuous exercise for 12 hours prior to the drawing. It is the phlebotomist‟s
responsibility to verify if the patient indeed, has been fasting for the required time.
Timed Specimens: They are often used to monitor the level of a specific substance or condition in the patient.
Blood is drawn at specific times for different reasons. Their uses are:
To measure blood levels of substances exhibiting daily variation (e.g. cortisol hormone).
To determine blood levels of medications, which are toxic and need accurate monitoring of their plasma
levels (e.g. digoxin for cardiovascular disease).
To monitor changes in a patient‟s condition (e.g. steady decrease in hemoglobin level).
Two-hour Postprandial Test: This test is used to evaluate diabetes mellitus. Fasting glucose level is
compared with the level 2 hours after eating a full meal or ingesting a measured amount of glucose.
Oral Glucose Tolerance Test (OGTT): This test is used to diagnose diabetes mellitus and evaluate patients
with frequent low blood sugar. 3-hour OGTT is used to test hyperglycemia (abnormally high blood sugar level)
and diagnose diabetes mellitus. 5-hour OGTT is used to evaluate hypoglycemia (abnormally low blood sugar
level) for disorders of carbohydrate metabolism. OGTT are scheduled to begin between 0700 and 0900.
Therapeutic Drug Monitoring: This test is used to monitor the blood levels of certain medication to ensure
patient safety and also maintain a plasma level. Blood is drawn to coincide with the trough (lowest blood level)
or the peak level (highest blood level). Trough levels are collected 30 minutes before the scheduled dose. Time
for collecting peak level will vary depending on the medication, patient‟s metabolism, and the route of
administration (I.V., I.M., or oral).
Blood Cultures (BC)/Hemoculture: They are ordered to detect the presence of microorganisms in the patient‟s
blood. The patient will usually have chills and fever of unknown origin (FUO), indicating the possible
presence of pathogenic microorganisms in the blood (septicemia). Blood cultures are usually ordered STAT or
as timed specimen, and collection requires strict aseptic technique.
PKU: This test is ordered for infants to detect phenylketonuria, a genetic disease that causes mental
retardation and brain damage. The test is performed on blood from a newborn‟s heel or urine.
9. Phlebotomy complications and Failure to Obtain Blood
A. Phlebotomy Complications
1. Hematoma is the most common complication of phlebotomy procedure. This indicates that blood has
accumulated in the tissue surrounding the vein. The two most common causes are the needle going
through the vein, and/or a failure to apply enough pressure on the site after needle withdrawal.
2. Hemoconcentration is the increase in proportion of formed elements to plasma caused by the
tourniquet being left on too long (more than two (2) minutes).
3. Phlebitis is the inflammation of a vein as a result of repeated venipuncture on it.
4. Petechiae are capillary rupture hemorrhages, tiny non-raised red spots that appear on the skin due to the
prolonged and very tight application tourniquet.
5. Thrombus is a blood clot inside the blood vessel that in cases of phlebotomy is usually a consequence
of insufficient pressure applied after the withdrawal of the needle.
6. Septicemia is considering as soiling of the blood by pathogenic microorganisms and their toxins. It is
usually due to improper disinfection of the phlebotomy area and seen frequently in immuno-suppressed
patients (AIDs), elderly and infants.
7. Trauma to the underlying tissues caused and neurovascular structures by probing of the needle and
inserting it too deep.

49
B. Failure to Obtain Blood
The following are some of the common causes:
The tube has lost its vacuum: This may be due to a manufacturing defect, expired tube or a crack in
the tube. The negative pressure inside the vacutainer diminishes with time.
Improperly positioned needle: In many instances, slight movement of the needle can correct this.
a. The bevel of the needle is resting against the wall of the vein. Slightly rotate the needle.
b. The needle is not fully in the vein. Slowly advance the needle.
c. The needle has passed through the vein. Slowly pull back on the vein.
d. The vein was missed completely. With a gloved finger, gently determine the positions of the vein and the
needle, and redirect the needle.
Collapsed vein. This may be due to excessive pull from the vacuum tube; use of a smaller vacuum tube
may remedy the situation. If it does not, remove the tourniquet, withdraw the needle, and select another
vein preferably using either a syringe or butterfly.
10. Capillary blood collections / Dermal Puncture
When venipuncture is inadvisable and impossible, it is possible to perform a majority of laboratory tests on
micro samples obtained by dermal (skin) puncture; with the exception of ESR, blood cultures and other tests
that require a large amount of serum. Dermal puncture may be done on both pediatric and adult patients.
Punctures should never be performed with a surgical blade or hypodermic needle because they can be difficult
to control. Deep penetration into the skin can cause serious injury such as osteomyelitis (inflammation of the
bone and bone marrow). A lancet should be used, which delivers a pre-determined depth that can range from
0.85mm for infants to 3.0mm for adults.
Dermal Puncture in Infants: The heel is used for dermal punctures on infants less than 1 year of age. Areas
recommended are the medial and lateral areas of the planter surface of the foot. These are determined by
drawing imaginary lines medially extending from the middle of the great toe to the heel and laterally from the
middle of the fourth and fifth toes to the heel. The American Academy Site selection for dermal puncture of
Pediatrics recommends that heel punctures for infants not exceed 2.0mm.
Observe the following precautions when performing dermal puncture:
do not puncture deeper than 2.0mm
do not perform dermal punctures on previous puncture sites
do not use the back of the heel or arch of the foot
use the medial and lateral areas of the planter surface of the heel
Dermal Puncture in Older Children and Adults: The distal segment of the third or fourth finger of the non-
dominant hand is the recommended site. Puncture is made in the fleshy portion of the finger slightly to the side
of the center perpendicular to the lines of the fingerprint.
Dermal Puncture Equipment: Lancets are short flat blades with a rubber coat that prevents the blade to go
deeper than 2.4 mm. Unopette Blood Dilution System is a short capillary tube ending with an overflow
chamber, a reservoir for collecting the blood sample and a pipe shield. Other tools are sterile gauze, alcohol or a
disinfection pads, a band aide and blood smear slides.
Dermal Puncture Procedure:
1. Identify the patient
2. Assemble equipment warm the site: this is an essential part of the procedure when collecting specimens
for pH or blood gases. Warming the site can increase the blood flow up to seven times the normal
amount. The specimen is referred to as arterialized specimen because of the increase arterial flow to the

50
area. This is accomplished by warming the site for a minimum of three minutes with a warm moistened
towel (no greater than 108 F), or with a commercial warming device.
3. Clean the site: Use 70% isopropyl alcohol. Allow the site to dry for maximum antiseptic action.
Alcohol residue can cause hemolysis of the red blood cells and may interfere with glucose testing.
Povidone-iodine (Betadine) is not used for cleaning the site because it interferes with several tests like
bilirubin, uric acid, phosphorus, and potassium.
4. Prepare the puncture device
5. Perform the dermal puncture
6. Identify the patient
7. Assemble equipment
8. Warm the site: this is an essential part of the procedure when collecting specimens for pH or blood
gases. Warming the site can increase the blood flow up to seven times the normal amount. The
specimen is referred to as arterialized specimen because of the increase arterial flow to the area. This is
accomplished by warming the site for a minimum of three minutes with a warm moistened towel (no
greater than 108 F), or with a commercial warming device.
9. Assemble equipment
10. Warm the site: this is an essential part of the procedure when collecting specimens for pH or blood
gases. Warming the site can increase the blood flow up to seven times the normal amount. The
specimen is referred to as arterialized specimen because of the increase arterial flow to the area. This is
accomplished by warming the site for a minimum of three minutes with a warm moistened towel (no
greater than 108 F), or with a commercial warming device.
11. Clean the site: Use 70% isopropyl alcohol. Allow the site to dry for maximum antiseptic action.
Alcohol residue can cause hemolysis of the red blood cells and may interfere with glucose testing.
Povidone-iodine (Betadine) is not used for cleaning the site because it interferes with several tests like
bilirubin, uric acid, phosphorus, and potassium.
12. Prepare the puncture device
13. Perform the dermal puncture
Dermal Puncture Order of Draw of Specimens:
1. Lavender tube
2. Tubes with other additives
3. Tubes without additives
Micro-samples are labeled with the same information required for venipuncture specimens of draw.
Blood Smear Procedure:
1. Select two slides that are clean and free of chipped edges.
2. Place a drop of blood in 1 to 2mm in diameter on one of the slides. The drop should in the center line
approximately ¼ inch from the frosted edge of the slide (Holding and labeling end).
3. Rest the end of the spreader slide over the drop of blood slide at a 45–degree angle. Make sure that
blood is spread over the all width of the slide, first draw the spread slider back and than push the
spreader slide rapidly across the stationary slide (blood drop slide) with one even stroke avoiding jerky
movements.
4. Allow the slide with the blood smear to dry, check for acceptability (feathered edge) and label the
slide.
End of Study Guide for CPCT
See Practice Exam in Next Section
Practice Exam questions are important to review as well.
PRACTICE EXAM QUESTIONS

51
The following question content may be found on the exams. This information may not be
covered in the study guide itself, rather here where you can ponder the question – and the
possible answers – to test your knowledge. Please be sure to complete this entire practice exam
in addition to reviewing the study guide and/or review classes online.
1.
Bleach solutions for disinfecting work surfaces is:
a
5%
b
10%
c
15%
d
20%
2.
The first step toward stopping the bleeding at the phlebotomy site is to:
a.
Apply pressure to the site
b.
Apply a tourniquet
c.
Call for help
d.
Panic
3.
The slanted part of the needle is called:
a.
Lumen
b.
Bevel
c.
Shaft
d.
Hub
4.
When taking a blood pressure, you should all of the following except:
a.
Apply the cuff to a bare upper arm
b.
Take the blood pressure in the arm with an IV infusion
c.
Turn off the radio and TV
d.
Locate the brachial artery
5.
What is the least accurate measurement of body temperature?
a.
Axillary
b.
Tympanic
c.
Oral
d.
Rectal

52
6.
The Patient Above is in which position?
a.
Prone position
b.
Supine position
c.
Semi-Fowlers position
d.
Trendelenburg position
7.
The following describe normal respirations except:
a.
There are 12 to 20 per minute
b.
They are quiet and effortless
c.
Noises occur on inhalation
d.
They are regular with both sides of the chest rising and falling equally
8.
A mask:
a.
Can be reused
b.
Is contaminated when moist
c.
Is clean on the inside
d.
Should fit loosely for breathing
9.
These statements are about surgical asepsis. Which is not true?
a.
Wet items are held up
b.
A sterile item can touch only another sterile item
c.
If you cannot see an item, it is contaminated
d.
Sterile items are kept above the waist
10.
Which one of the following does not prevent nosocomial infections?
a.
Hand hygiene before and after giving care
b.
Sterilizing all care items
c.
Surgical asepsis
d.
Standard Precautions

53
11.
The muscular portion of the heart is called the:
a.
Pericardium
b.
Endocardium
c.
Myocardium
d.
Dyscardium
12.
The heart muscle contracts during:
a.
Diastole
b.
Fibrillation
c.
Systole
d.
Conduction
13.
The standard ECG involves:
a.
3 leads
b.
6 leads
c.
12 leads
d.
Unipolar leads
14.
The chest leads are also called:
a.
Precordial leads
b.
Limb leads
c.
Augmented limb leads
d.
Bipolar leads
15.
A person develops chest pains during an ECG. What should you do?
a.
Call for the nurse at once
b.
Take the person‟s vital signs
c.
Use telemetry
d.
Continue taking the ECG
16.
A 24-hour urine specimen involves:
a.
Collecting a random specimen every hour for 24 hours
b.
Collecting all urine voided during a 24 hour period
c.
Measuring output every hour for 24 hours
d.
Testing urine and sugar ketones every day
17.
A hematoma is:
a.
A blood test
b.
A device to control bleeding
c.
A swelling that contains blood
d.
A short, disposable blade

54
18.
A vein for a venipuncture site should:
a.
Be narrow
b.
Be sclerosed
c.
Roll easily
d.
Rebound after palpating it
19.
The needle and syringe method is used to obtain a blood specimen. Which is true?
a.
The needle and syringe are sent to the lab
b.
The syringe is capped and sent to the lab
c.
Blood is transferred from the syringe to a vacuum tube
d.
Blood is collected in vacutainers
20.
You perform a skin puncture. The first drop of blood is:
a.
Saved
b.
Tested in case you cannot get another drop
c.
Wiped off with a cotton ball
d.
Rinsed off with water
21.
You inspect a skin puncture site. You can use a site that:
a.
Has intact skin
b.
Is callused
c.
Is swollen or bruised
d.
Is scarred
22.
You will assist with a patient‟s exam. Which is false?
a.
Hand hygiene is practiced before and after the exam
b.
You leave the room when the patient is being examined
c.
Instruments are placed near the examiner
d.
Provide for privacy by screening, closing the door and proper draping.
23.
What does this symbol represent?
a.
Biologic Hazard
b.
Chemical Hazard
c.
Sharp‟s Hazard
d.
Radioactive Hazard

55
24.
The purpose of fecal occult blood test is to help determine:
a.
Presence of GI bleeding not seen with the naked eye
b.
Presence of drugs and their levels
c.
Presence of diabetes, not otherwise found
d.
Presence of eye disease not seen with naked eye
25.
The strip above reflects a “lead error” Which of the following is correct?
a.
V1 and V3 chest electrodes are interchanged
b.
V4 and V6 chest electrodes are interchanged
c.
V3 and V7 chest electrodes are interchanged
d.
V8 and V9 chest electrodes are interchanged
26.
When a patient is catheterized the drainage bag should never:
a.
Be hanging higher than the bladder
b.
Be monitored for intake and output
c.
Be emptied every 20 minutes
d.
Hanging lower than the bladder
27.
You were not able to obtain blood from an elderly patient. This may be caused by:
a.
The tourniquet was on too tight
b.
An excessive pull from the vacuum tube causing a collapsed vein
c.
Patient‟s posture
d.
Improper site prep
28.
Neonatal blood screening is used to identify all of the following except:
a.
Spina bifida
b
Congenital hypothyroidism
c.
Cystic fibrosis
d
PKU ( phenylketonuria)
29.
Which of the following evacuated tubes is preferred for the collection of a blood

56
culture specimen?
a.
Green-topped evacuated tube
b.
Light blue-topped evacuated tube
c.
Yellow-topped evacuated tube
d.
Red-topped evacuated tube
30.
What type of urine specimen is needed to detect an infection?
a.
Clean catch
b.
Random
c.
Routine
d.
24-hour
31.
The liquid portion of an anticoagulated blood specimen is called:
a.
Plasma
b.
Serum
c.
Cellular components
d.
Oxygenated blood
32.
Which legal concept refers to the voluntary permission by a patient to allow touching,
examination, and/or treatment by health care providers?
a.
Implied consent
b.
Assault and battery
c.
Battery
d.
Informed consent
33.
A surgical bed is kept in the:
a.
Fowler‟s position
b.
In the lowest position
c.
In the highest position
d.
In the supine position
34.
The logrolling procedure:
a.
Is used after spinal cord injuries or surgery
b.
Requires a transfer belt
c.
Requires a mechanical lift
d.
Involves a stretcher and a lift sheet
35.
Which is not a portal of exit?

57
a.
Respiratory tract
b.
Blood
c.
Reproductive system
d.
Intact skin
36.
Standard Precautions:
a.
Are used for all persons
b.
Keep pathogens in a certain area
c.
Require gowns, masks, gloves and eyewear
d.
Involve medical and surgical asepsis
37.
These statements are about personal protective equipment (PPE). Which is false?
a.
Wash disposable gloves for reuse
b.
Remove PPE before leaving the work area
c.
Discard cracked or torn utility gloves
d.
Wear gloves when touching contaminated items or surfaces
38.
A person is agitated or aggressive. You should do all of the following except:
a.
Stand away from the person
b.
Stand close to the door
c.
Use touch to show you care
d.
Talk to the person without raising your voice
39.
You gave a patient the wrong care. What should you do?
a.
Report the error at the end of the shift
b.
Take action only if the patient was injured
c.
You should report yourself as guilty of negligence
d.
You must complete an incident report
40.
Which part of the heart pumps blood to the body?
a.
Right atrium
b.
Right ventricle
c.
Left atrium
d.
Left ventricle
41.
Which carry blood away from the heart?
a.
Capillaries
b.
Veins
c.
Venules
d.
Arteries
42.
Urine passes from the body through:
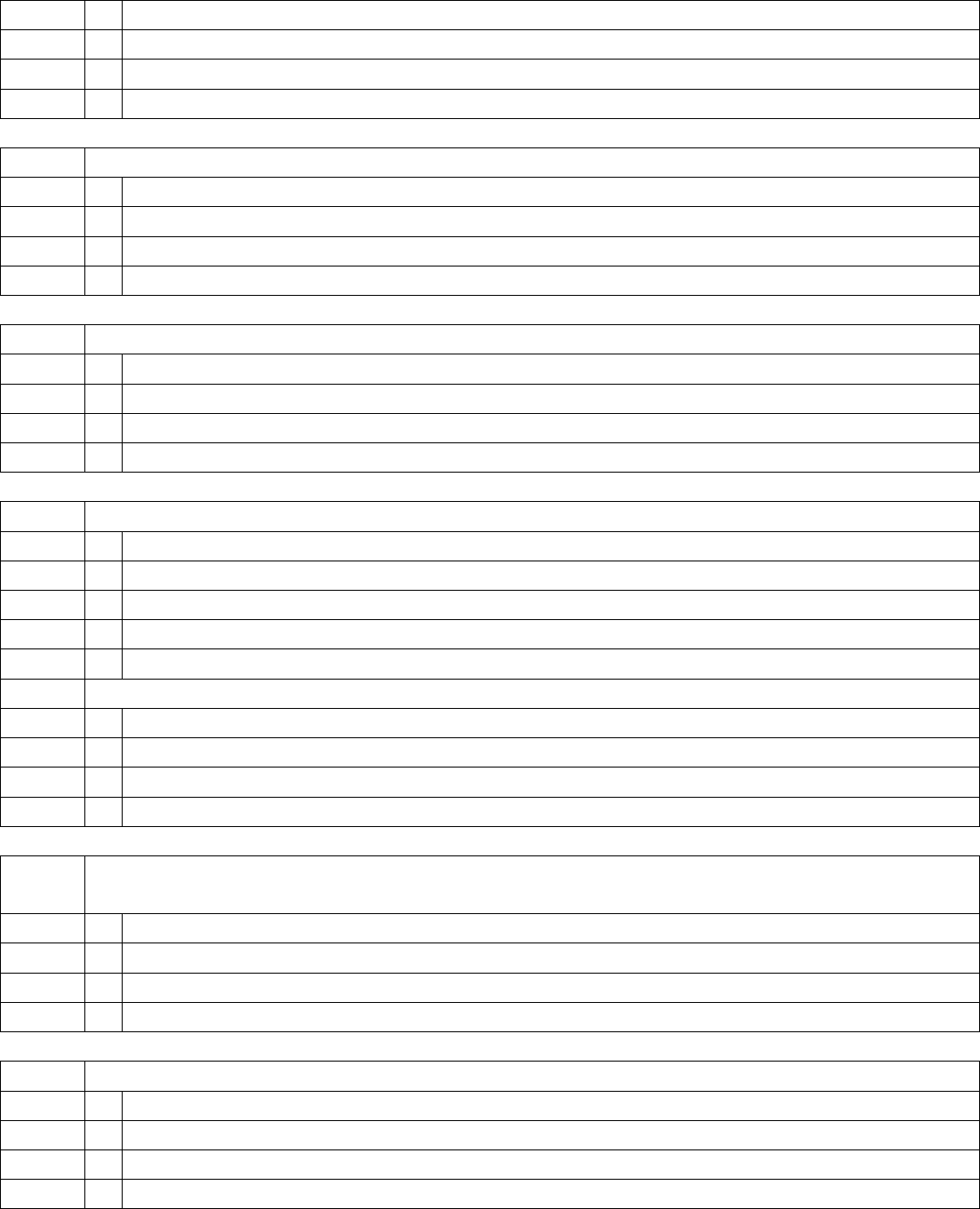
58
a.
The ureters
b.
The urethra
c.
The anus
d.
Nephrons
43.
Which is a sign?
a.
Nausea
b.
Headache
c.
Dizziness
d.
Dry skin
44.
Which is a symptom?
a.
Redness
b.
Vomiting
c.
Pain
d.
Pulse rate of 78
45.
The nursing care plan:
a.
Is written by the doctor
b.
Has actions the nursing team takes to help a person
c.
Is the same for all persons
d.
Is also called the Kardex
46.
In the evening the clock shows 9:30. In military time this is written:
a.
2130
b.
1930
c.
0930
d.
1130
47.
A co-worker is often late for work. This means extra work for you. To resolve the
conflict you should do the following except:
a.
Explain the problem to your supervisor
b.
Discuss the matter during the end-of-shift report
c.
Give facts and specific behaviors
d.
Suggest ways to solve the problem
48.
A person is weighed daily. The measurement is recorded on the:
a.
Admission sheet
b.
Graphic sheet
c.
Flow sheet
d.
Progress sheet

59
49.
The intentional attempt or threat to touch a person‟s body without the person‟s consent
is:
a.
Assault
b.
Battery
c.
Defamation
d.
False imprisonment
50.
Ethical standards
a.
Are federal laws
b.
Are state laws
c.
Are about right conduct and wrong conduct
d.
Are rules stating what you can and cannot do
END OF PRACTICE EXAM
WRITTEN REVIEW GUIDE

60
ANSWERS TO PRACTICE EXAM
TO ACCOMPANY CPCT WRITTEN
REVIEW GUIDE
1
B
2
A
3
B
4
B
5
A
6
C
7
C
8
B
9
A
10
B
11
C
12
C
13
C
14
A
15
A
16
B
17
C
18
D
19
C
20
C
21
A
22
B
23
A
24
A
25
A
26
A
27
B
28
A
29
C
30
A
31
A
32
D
33
C
34
A
35
D
36
A
37
A
38
C
39
D
40
D
41
D
42
B
43
D
44
C

2
45
B
46
A
47
B
48
B
49
A
50
C
